The population prevalence of attention-deficit hyperactivity disorder (ADHD) is estimated to be 7.2% worldwide and has been relatively stable over the past 40 years.Reference Thomas, Sanders, Doust, Beller and Glasziou1 ADHD is a neurodevelopmental disorder with symptoms including hyperactivity, impulsivity and inattention. ADHD has a childhood onset but symptoms of ADHD and impairments often persist into adolescence and adulthoodReference Riglin, Collishaw, Thapar, Dalsgaard, Langley and Smith2 and have been associated with lower educational levels, greater risk of criminal activities,Reference Dalsgaard, Mortensen, Frydenberg and Thomsen3 and early and violent death.Reference Dalsgaard, Ostergaard, Leckman, Mortensen and Pedersen4 Some population-based studies have noted a higher rate of suicidal behaviour, including suicide attempts and death by suicide, among people diagnosed with or treated for ADHD, when compared with persons without ADHD.Reference Ljung, Chen, Lichtenstein and Larsson5 It is not completely clear which mechanisms might account for this higher rate, but given that persons with ADHD also have an increased risk of developing comorbid psychiatric disorders,Reference Ottosen C, Faraone, Chen, Hartman, Larsson and Petersen6 it has been suggested that such comorbidities might act as mediating factors for suicidal outcomes.Reference James, Lai and Dahl7 To date, the relative impact of a comorbid diagnosis on the risk of suicidal behaviour has only been examined in small study samples of patients with ADHD.Reference Yoshimasu, Barbaresi, Colligan, Voigt, Killian and Weaver8 Studies with larger samples and more rigorous analyses (i.e. adjustment for relevant social covariates, such as cohabitational, educational and socioeconomic status) are needed.
In this study, we aimed to investigate whether persons diagnosed with ADHD were more likely to present with suicidal behaviour than persons without ADHD, as well as whether the association might be mediated by psychiatric comorbidity. To our knowledge, this is the first nationwide study to examine the role of psychiatric comorbid disorders in the association between ADHD and suicidality.
Method
A cohort design was applied to nationwide register data. The Danish Civil Registration System was implemented in 1968, whereby every person living in Denmark was given a unique identification number. From then onward, the identification number was given upon live birth or immigration into the country. The Civil Registration System stores information on every person in Denmark and is considered to have a high reliability.Reference Pedersen9 For this study, the identification number facilitated individual-level linkage to the following administrative registers: the Psychiatric Central Research Register (PCRR), the National Hospital Register (NHR), the Cause of Death Registry (CDR), the Populations Education Register, the Register on Criminal Statistics and the Income Statistics Register.
Study population
The study population comprised all persons aged 10 years or above who were recorded as living in Denmark between 1 January 1995 and 31 December 2014. Persons would enter the cohort at baseline, on their 10-year birthday or date of immigration into the country during the study period and the follow-up ended upon date of death, emigration or 31 December 2014, whichever came first. To minimise unmeasured bias among migrants related to potential traumatic events not recorded in the Danish registries, only persons for whom records of their parents being born in Denmark existed were included. This method has been used in previous studies,Reference Ottosen, Petersen, Larsen and Dalsgaard10 and resulted in an exclusion of approximately 16% of the Danish population, where data was found to be insufficient.
Assessment of psychiatric disorder
Information on psychiatric diagnoses was obtained from the PCRR. From 1969 onward, all psychiatric in-patient admissions have been registered in the PCRR, and from 1995, emergency room and out-patient visits were also included. Diagnoses were recorded according to the ICD-811 and ICD-1012. ICD-9 was never implemented in Denmark.
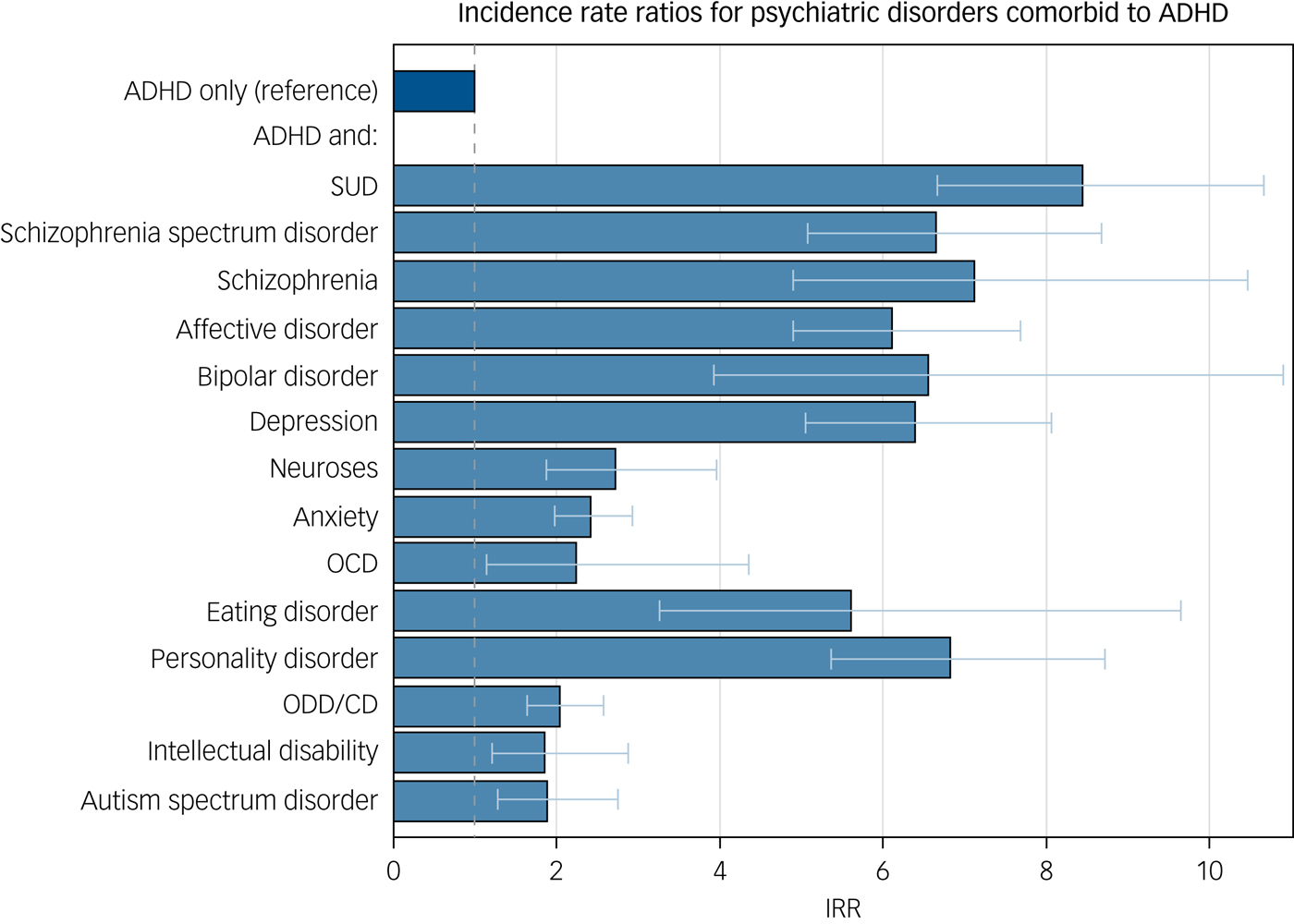
Fig. 1 The relative rates of suicidal behaviour of persons with ADHD and the specified comorbid disorder compared to persons with ADHD only
Every person who had ever received a diagnosis of ADHD (ICD-8: 308.01; ICD-10: F90, F98.8) was considered as exposed from that date onward. In addition, other psychiatric diagnoses of substance use disorder (SUD); schizophrenia; schizophrenia spectrum disorders; affective disorders; bipolar disorder; depression, anxiety, dissociative, stress-related and somatoform disorders; anxiety; obsessive–compulsive disorder; post-traumatic stress disorder; eating disorders; personality disorders; intellectual disability; autism spectrum disorders (ASD) and oppositional defiant disorder/conduct disorder (ODD/CD) were identified. Detailed specifications of the ICD codes are listed in Supplementary Table 1 available at https://doi.org/10.1192/bjp.2019.128.
Outcomes
The outcome of suicidal behaviour was defined as having had a hospital contact for suicide attempt or death by suicide. In the NHR and PCRR, a diagnosis of suicidal behaivour (ICD-8: 950–959; ICD-10: X60–X84) or a reason for contact of ‘suicide attempt’ were considered as indicative of a suicide attempt. Records on cause of death from the CDR were assessed and persons with an ICD-code of suicidal behaivour (see above) or where suicide was recorded as the manner of death were considered as having died by suicide.
Statistical analyses
We calculated incidence rates based on number of events and person-days in each stratum. Poisson regression was used to calculate incidence rate ratios (IRRs) between those with ADHD and those without ADHD. Multivariate regression models were adjusted for gender (male, female), age (in years: 10–14, 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, ≥60) and calendar year (1995–2004, 2005–2014). A sensitivity analysis was conducted, further adjusting for cohabitational status (single adult household, cohabiting household), level of education (vocational/none, high school, university degree), socioeconomic status (within the workforce, including children and students; unemployed), as well as parents’ suicide attempts (no parent, one parent, both parents) to estimate figures without the social implications associated with ADHD and the parental factors known to contribute to suicidal behaviour. All of these were treated as time-dependent variables. Interaction analyses were performed by comparing the following groups: group 1, persons with no diagnosis; group 2, persons with ADHD as their only psychiatric diagnosis; group 3, persons diagnosed with psychiatric disorders other than ADHD and group 4, persons diagnosed with one or more other psychiatric disorders comorbid to ADHD. Group 2 was chosen to include only those with no comorbid disorders to avoid comparing the effect of different comorbid disorders. The IRRs were reported with 95% CIs. The same analyses were performed with suicide as the outcome where a minimum of five suicides were observed in each category of the examined predictor. Analyses were conducted by SAS version 9.4 statistical software for Windows (SAS Institute, Inc.).
This study was approved by the Danish Data Protection Agency. In Denmark, informed consent is neither feasible nor required for register-based studies.
Results
The total study population comprised 2 924 780 persons (including 1 402 113 females) who were observed over 46 million person-years. During the 20 years of observation, 37 705 suicidal events (4 930 suicide deaths, 32 775 suicide attempts) were observed within the total cohort (see Supplementary Table 2). In all, 32 540 persons (including 10 019 females) with an ADHD diagnosis were followed until a mean age of 21.5 (s.d. 9.6), accounting for 164 113 person-years and 697 suicidal events (35 suicide deaths, 662 suicide attempts). The incidence rates of suicidal behaviour in the total cohort and those with ADHD were 75.5 and 415.6 per 100 000 person-years, respectively.
Main analysis
Compared with persons with no ADHD diagnosis, a 4.7-fold higher rate of suicidal behaviour (95% CI, 4.34–5.06) was noted among those with ADHD (see Table 1). Males with ADHD were found to have a 3.4-fold higher rate (95% CI, 3.04–3.76), whereas a 9.1-fold higher rate was noted for females (95% CI, 8.12–10.12) when compared with males without ADHD. When stratifying by age groups, we found an excess IRR among people with ADHD for all age groups, which was particularly pronounced for those with ADHD aged 20–29 years who had an IRR of 10.07 (95% CI, 8.81–11.51) compared with those without ADHD. Persons with ADHD who had been convicted of a crime had a three-fold higher rate compared with those with ADHD who were not convicted (IRR: 14.07; 95% CI, 12.27–16.15 v. IRR: 4.86; 95% CI, 4.44–5.33, respectively).
Table 1 Incidence rate ratios for suicidal behaviour

ADHD, attention-deficit hyperactivity disorder; IRR, incidence rate ratio.
a. Adjusted for age, gender and calendar year.
***P < 0.001.
The sensitivity analysis resulted in a 2.6-fold higher rate of suicidal behaviour (95% CI, 2.43–2.84) among those with ADHD (see Table 2). For all analyses the resulting IRRs were smaller but significant in the same direction as the main analysis.
Table 2 Sensitivity analyses with incidence rate ratios for suicidal behaviour and for death by suicide, with additional adjustments

ADHD, attention-deficit hyperactivity disorder; IRR, incidence rate ratio; SES, socioeconomic status.
a. Adjusted for age, gender, year, cohabitational status, SES, educational level and parents’ suicide attempts.
b. Adjusted for age, gender, year, cohabitational status, SES and educational level.
* P < 0.05, **P < 0.01, ***P < 0.001.
Parental factors
Parental psychiatric disorders or suicidal behaviour affected the rate of suicidal behaviour in children. Persons with ADHD and parents with no psychiatric disorders had an IRR of suicidal behaviour of 4.85 (95% CI, 4.40–5.35). In comparison, among those with ADHD where at least one parent had a psychiatric disorder, an IRR of 7.32 (95% CI, 6.49–8.25) was noted. Having ADHD and a parent with suicidal behaviour was associated with an IRR of 3.87 (95% CI, 3.19–4.68), whereas those whose parents did not have suicidal behaviour had an IRR of 2.99 (95% CI, 2.75–3.25) compared with those without ADHD.
Psychiatric comorbidity
Individuals who had only been diagnosed with ADHD had an IRR of 4.09 (95% CI, 3.53–4.73), whereas those diagnosed with additional psychiatric disorders had an IRR of 10.43 (95% CI, 9.53–11.41) when compared with those without ADHD (see Supplementary Table 3). The IRR was highest among persons with psychiatric disorders other than ADHD (IRR: 14.84; 95% CI, 14.52–15.17). The largest difference was noted for SUD: those who only had ADHD had an IRR of 2.90 (95% CI, 2.51–3.36), whereas those with ADHD and SUD had an IRR of 21.55 (95% CI, 17.98–25.83), which was comparable with those with SUD but without ADHD (IRR: 25.12; 95% CI, 24.32–25.95). A comorbid diagnosis of ASD was associated with a two-fold higher rate of suicidal behaviour, from an IRR of 2.63 (95% CI, 2.27–3.05) for people with ADHD to 4.65 (95% CI, 3.25–6.66) among those with both disorders; those with autism alone had an IRR of 2.31 (95% CI, 1.98–2.71).
Having an increasing number of different comorbid disorders was linked to increasing rates of suicidal behaviour. Having one, two and three or more comorbid disorders resulted in IRRs of 4.76 (95% CI, 3.88–5.84), 4.41 (95% CI, 3.47–5.61) and 8.20 (95% CI, 7.36–9.13) when compared with those without ADHD.
Death by suicide
With regard to death by suicide, persons with ADHD had an IRR of 3.20 (95% CI, 2.29–4.47) (see Table 3). Males with ADHD had an IRR of 2.98 (95% CI, 2.06–4.30), but the estimate for females failed to reach significance (IRR 1.47; 95% CI, 0.66–3.27). Persons with ADHD who were aged 30–39 years had a higher suicide rate (IRR: 3.01; 95% CI, 1.66–5.44) than age-matched persons without ADHD.
Table 3 Incidence rate ratios for death by suicide

ADHD, attention-deficit hyperactivity disorder; IRR, incidence rate ratio.
a. Adjusted for age, gender and calendar year.
* P < 0.05, **P < 0.01, ***P < 0.001.
Discussion
Our analysis confirmed that persons diagnosed with ADHD have higher rates of suicidal behaviour, including death by suicide, when compared with those without ADHD. Specific risk factors for suicidal behaviour in persons with ADHD suggested by this study were female gender, young age, psychiatric comorbidity, previous suicidal behaviour, a criminal record and parental history of psychiatric disorder. This is the first study to give a comprehensive overview of the relation between ADHD, suicidal behaviour and comorbid psychiatric disorders, and we noted a significantly higher rate among those with comorbidity, which was comparable with that of the comorbid disorder.
In line with previous studies,Reference Dalsgaard, Ostergaard, Leckman, Mortensen and Pedersen4,Reference Ljung, Chen, Lichtenstein and Larsson5 we found an excess rate of suicidal behaviour among people with ADHD. Our findings suggest that this association cannot be fully explained by parental psychiatric disorders. Children with ADHD without parental psychiatric disorders also had a substantially higher frequency of suicidal behaviour. There are several possible explanations for the observed association. First, impulsivity, a recognised trait of ADHD, has also been linked genetically to suicidal behaviour,Reference Hawton and van Heeringen13 and so it is possible that some of the association might be thus explained.Reference Ljung, Chen, Lichtenstein and Larsson5 Second, other characteristics of ADHD, such as impaired decision-making,Reference Miller, Sheridan, Cardoos and Hinshaw14 low peer preferenceReference Meza, Owens and Hinshaw15 and high risk-willingness,Reference Humphreys and Lee16 have been suggested to contribute to the increased rate. Finally, low educational attainmentReference Barry, Lyman and Klinger17 and high levels of stressReference Lackschewitz, Hüther and Kröner-Herwig18 have been noted as risk factors for suicidal behaviour.Reference Jablonska, Lindblad, Ostberg, Lindberg, Rasmussen and Hjern19 Our sensitivity analysis confirmed that ADHD was associated with suicidal behaviour also when adjusting for several relevant covariates that might act as confounders.
Although an association with suicidal behaviour was confirmed for both males and females separately, the hazard for females was found to be twice that of males, supporting previous findings.Reference Ljung, Chen, Lichtenstein and Larsson5 ADHD has also been found to have a more pronounced effect in females on a number of other adverse outcomes,Reference Dalsgaard, Ostergaard, Leckman, Mortensen and Pedersen4,Reference Ottosen, Petersen, Larsen and Dalsgaard10,Reference Dalsgaard, Mortensen, Frydenberg and Thomsen20 which might indicate that the social implications of having ADHD are more extensive for females, who are traditionally expected to be calmer and less physical than males. It has, to our knowledge, not previously been shown that ADHD might have a more pronounced impact on suicidal behaviour in younger persons. This could be related to attenuation of social effects especially important in this age group, such as starting a family or adjusting to the educational system. The higher rate related to having parents with a psychiatric disorder might indicate an increased emotional vulnerability in persons exposed to a more turbulent childhood, but could also be explained through genetically transmitted vulnerability.Reference Ljung, Chen, Lichtenstein and Larsson5 Having a parent with suicidal behaviour did not result in a significantly higher IRR for persons with ADHD as it did for persons without ADHD. This suggests that a parent's suicidal behaviour is not relevant for the outcome of their child if they are also affected by an ADHD diagnosis. This might be owing to the already elevated distress that seems to be present in these individuals. It has been suggested that persons with ADHD are more likely to carry out criminal activities,Reference Dalsgaard, Mortensen, Frydenberg and Thomsen3 and criminal behaviour has been linked to suicidal behaviour.Reference Webb, Qin, Stevens, Mortensen, Appleby and Shaw21 It is therefore highly relevant to explore the mechanisms making persons with ADHD at risk for criminal activities.
Psychiatric comorbidity
Although the association was particularly strong for SUD, schizophrenia spectrum disorders and affective disorders, almost all comorbid diagnoses resulted in an increased rate of suicidal behaviour for persons with ADHD, suggesting that the association is partly mediated by comorbid psychiatric disorders. Nevertheless, a 2.5- to 3.0-fold higher rate was noted among persons with ADHD only across all analyses, clearly showing the unexplained effect of the diagnosis. The excess ratio associated with a comorbid disorder was generally of the same magnitude as in persons diagnosed only with the other disorder, suggesting that ADHD does not further increase risk in persons who are already at high risk via their other diagnosis. This contrasts with previous findings related to comorbid bipolar disorder, albeit from a smaller sample size.Reference Lan, Bai, Hsu, Huang, Su and Li22 The importance of addressing comorbid SUD is well known and yet particularly relevant.Reference Ottosen, Petersen, Larsen and Dalsgaard10 For persons with anxiety, an additional ADHD diagnosis seemed to have a protective effect, possibly because persons with both disorders might represent a select group. A similar finding was observed for overall comorbid diagnoses. Further analyses would be needed to elucidate these findings. ASD stood out with an elevated rate for persons with comorbid ADHD compared with those without, which could suggest that the increased risk of suicidality in individuals with ASDReference Culpin, Mars, Pearson, Golding, Heron and Bubak23 may be partly mediated through ADHD. This would, however, need further examination. A higher rate of suicidal behaviour in relation to higher numbers of comorbid disorders is well established.Reference Qin and Nordentoft24
Strengths and limitations
The strengths of this study are related to the use of longitudinal data from highly reliable nationwide registers with very little missing data. The large sample includes all persons diagnosed with ADHD and has virtually no loss to follow-up and a low risk of mortality and selection bias. Furthermore, it was possible to examine associations with a wide spectrum of comorbid disorders. As Danish registers allow for linkage of family members, it was possible to adjust for predisposing factors related to parents’ mental health, with an almost complete coverage for people born after 1952. The long study period was yet another strength of this study.
We also acknowledge several limitations of this study. Although the registration of suicide deaths is evaluated to be reliable in Denmark, suicide attempts might be under-recorded by as much as 30%.Reference Helweg-Larsen, Kjøller, Juel, Sundaram, Laursen and Kruse25 It is possible that a small fraction of individuals with ADHD might only be diagnosed by psychiatrists in private practices and so are not identified by the registers and not included in our ADHD population. Furthermore, misclassification might have occurred, particularly in early years; however, these circumstances would likely render our estimates as conservative. Indeed, those diagnosed at hospital clinics may represent more severe cases, which means that our findings might not generalise to the broad ADHD spectrum. This limitation also applies to other psychiatric disorders analysed. Furthermore, as only few events of death by suicide were observed for some psychiatric diagnoses, the main outcome was chosen to be a combination of attempted suicide and death by suicide. The results may therefore only be partially representative of the relation between ADHD and suicide deaths. Also, by excluding children whose parents were not born in Denmark, our findings might not be fully representative of the entire nation.
Clinical implications
Given that ADHD is correlated with an increased risk of developing other and often more disabling psychiatric disorders later in life,Reference Dalsgaard, Mortensen, Frydenberg and Thomsen20 the findings of this study underscores the importance of diagnosis and treatment of ADHD. An awareness regarding suicidality among persons with ADHD, especially among those with comorbid disorders, is needed. Long-term effects of ADHD might persist into adulthood, and there is a need for preventive measures and interventions throughout a patient's lifetime, to reduce the risk of suicides and suicide attempts.
To our knowledge, no interventions have specifically targeted suicide in persons with ADHD. General interventions addressing suicide among children and adolescents have been implemented in many countries, but the evidence base is limited.Reference Hawton, Witt, Taylor Salisbury, Arensman, Gunnell and Townsend26 However, previous cohort studies suggest that pharmacotherapy for ADHD may have beneficial effects on the risk of suicidal behaviour.Reference Ljung, Chen, Lichtenstein and Larsson5,Reference Chen, Sjolander, Runeson, D'Onofrio, Lichtenstein and Larsson27 In addition, our findings suggest that interventions focused on comorbid disorders, particularly on SUD, schizophrenia spectrum disorders and affective disorders, might be indicated. When assessing risk of suicidal behaviour, clinicians might consider other risk factors, such as juvenile delinquency and/or a history of psychiatric disorders or suicidal behaviour in parents. Also, clinicians could provide increased clinical attention for females with ADHD,Reference Dalsgaard, Ostergaard, Leckman, Mortensen and Pedersen4,Reference Ottosen, Petersen, Larsen and Dalsgaard10 including assessing for risk of suicidal behaviour.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2019.128.
Funding
The study was supported by a research trainee grant from the Danish Lundbeck Foundation. Dr. Dalsgaard's research is supported by grants from Aarhus University Research Foundation (AUFF-E-2015-FLS-8-61), The Lundbeck Foundation (iPSYCH grants R102-A9118 and R155-2014-1724), National Institute of Health (R01 grant ES026993), Novo Nordisk Foundation (grant 22018) and the European Commission (Horizon 2020, grant 667302).






eLetters
No eLetters have been published for this article.