Worldwide, endometrial cancer is the sixth most common cancer in women, being more frequent in high-income countries(1). The majority of risk factors are related to oestrogenic exposure, where oestrogen-stimulated endometrial cell proliferation increases risk if not counterbalanced sufficiently by progesterone(Reference Kaaks, Lukanova and Kurzer2). It is biologically plausible that dietary phyto-oestrogens may protect against hormone-dependent cancers(Reference Adlercreutz3). In Nordic countries, plant lignans contribute to the largest phyto-oestrogen concentration(Reference Peeters, Slimani and van der Schouw4). Lignans are ubiquitously found in plants, predominantly in the fibre layers, and rich sources include seeds, whole-grain cereals, legumes, vegetables and fruits(Reference Mazur5). Plant lignans are converted to enterolignans by microbial fermentation in the colon, and the concentration is primarily determined by the intake of plant lignans and the capacity of the intestinal microflora(Reference Adlercreutz3).
Owing to their chemical similarities with oestrogens, enterolactone may compete with oestrogens for binding to oestrogen receptors and thereby disrupt oestrogen signalling, an effect that could vary according to the level of endogenous oestrogen. Thus, enterolactone might reduce a woman's lifetime exposure to bioavailable oestrogens and thereby decrease risk of endometrial cancer. Furthermore, enterolactone may decrease endometrial cancer risk by stimulating the synthesis of sex hormone-binding globulin, inhibiting aromatase and 17-β-hydroxysteroid dehydrogenase, as well as exerting antioxidative effects, inducing apoptosis and inhibiting cancer cell growth(Reference Adlercreutz, Mousavi and Clark6).
Due to its oestrogenic potential, enterolactone has been evaluated in relation to several hormone-dependent cancers with inconsistent findings(Reference Adlercreutz3). To our knowledge, however, only one currently published study has investigated the association between circulating levels of enterolactone and incidence of endometrial cancer(Reference Zeleniuch-Jacquotte, Lundin and Micheli7). This nested case–control study did not find an association when evaluating enterolactone using ordered categorical variables in a population with a relatively low concentration and variation of circulating enterolactone. Two other case–control studies have estimated intake of plant lignans in relation to endometrial cancer(Reference Horn-Ross, John and Canchola8, Reference Bandera, Williams and Sima9), where one found a protective effect(Reference Horn-Ross, John and Canchola8).
The aim of the present study was to evaluate whether plasma enterolactone concentrations were associated with the incidence of endometrial cancer among Danish middle-aged women in a case–cohort study nested within a large prospective cohort. Furthermore, we evaluated if the association between enterolactone and endometrial cancer differed in different hormonal environments. This was done by testing for potential effect modification by menopausal status, use of hormone replacement therapy (HRT) and BMI.
Materials and methods
Cohort
The ‘Diet, Cancer and Health’ study is a prospective cohort study established with the primary aim of evaluating the aetiological role of diet in cancer development(Reference Tjonneland, Olsen and Boll10). Between December 1993 and May 1997, 79 729 Danish women living in greater Copenhagen and Aarhus were invited to participate, the inclusion criteria being age 50–64 years, born in Denmark and not registered with a previous cancer diagnosis in the Danish Cancer Registry. Subjects were identified by a unique ten-digit personal identification number assigned to all citizens from the Civil Registration System. A total of 29 875 women were enrolled in the study corresponding to approximately 37 % of those invited. The present study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by the Ethical Committees on Human Studies in Copenhagen and Aarhus. All cohort participants provided written informed consent.
All participants attended one of the two study centres and filled in a validated 192-item FFQ(Reference Tjonneland, Overvad and Haraldsdottir11) and a life-style questionnaire. Information on parity, menopausal status, use of HRT and smoking was obtained from the life-style questionnaire. Anthropometric measurements were taken by professional staff from where information on BMI was gained. A total of 30 ml blood was drawn in a non-fasting state and samples were spun and divided into 1 ml tubes (citrated and plain Venojects) of plasma, serum, erythrocytes and buffy coat. All samples were processed and frozen within 2 h at − 20°C and stored in liquid N2 vapour with a maximum temperature of − 150°C at the end of the day.
Definition of study group
Of the initial 29 875 women, we excluded 335 who were later reported to the Danish Cancer Registry with a diagnosis of cancer before study entry. Furthermore, another 1291 women with no or incomplete blood samples were excluded, leaving 28 249 women for the study. These were linked to the Central Population Registry to obtain information on vital status and migration.
Each woman was followed from baseline (i.e. date of visit at a study centre) until diagnosis of any cancer (except non-melanoma skin cancer), hysterectomy, death, emigration or end of follow-up (i.e. 27 April 2006), whichever came first. Information on endometrial cancer occurrence was obtained through record linkage to the Danish Cancer Registry (ICD7 172.0-172.2, 472.0, 872.0) and to the Danish Pathology Databank (T84000 and M8-9). Furthermore, the women were linked to the Hospital Discharge Registry to gain information on hysterectomy.
A total of 188 women were diagnosed with endometrial cancer during follow-up, and a random subcohort sample of 188 women was chosen, corresponding to a case–cohort design. Coincidentally, none of the subcohort members were cases. One woman was excluded due to suspected registry error, as were two cases concurrently diagnosed with endometrial and cervical cancer. Furthermore, ten cases and four subcohort members without enterolactone measurements and one case with an unrealistic enterolactone concentration (i.e. above 1100 nmol/l) were excluded. One subcohort member not handing in the life-style questionnaire, three cases and four subcohort members with missing information on potential confounders and thirty-one subcohort members with a hysterectomy before baseline were excluded. A total of 149 women were ultimately included as subcohort members and 173 women as cases in the final statistical analyses.
Biological analysis
The standard analytical procedure for time-resolved fluoroimmunoassay was used for determinations of plasma enterolactone concentrations(Reference Adlercreutz, Wang and Lapcík12, Reference Stumpf, Uehara and Nurmi13). The principle of the analysis relies on a method where goat anti-rabbit IgG-coated wells bind rabbit anti-enterolactone IgG (Labmaster Limited). Fluorescence was read in the DELFIA Victor multilabel counter (Wallac Oy). Duplicate internal control plasma samples were included in each batch and placed at the beginning and end of the plates. The plasma concentrations of enterolactone in the controls were 9·3 and 37·6 nmol/l, respectively, and the intra- and inter-assay CV were 13·5 and 15·0 %, respectively, at the low concentration and 8·1 and 9·2 %, respectively, at the high concentration. We have previously found the assay CV to be virtually independent of the concentration of enterolactone in plasma in the range 0–140 nmol/l (KEB Knudsen, unpublished results).
Statistical methods
Baseline descriptive characteristics for the included women are presented as median values (5th and 95th percentiles) for continuous variables, while categorical variables are presented as fractions (%).
The statistical analyses were performed according to the principles described by Prentice(Reference Prentice14) and suggested by Barlow et al. (Reference Barlow, Ichikawa and Rosner15), where a modified Cox proportional hazards model was used to evaluate the association between enterolactone concentration and endometrial cancer incidence. Age was used as the underlying time scale. Two-sided 95 % CI for incidence rate ratio (IRR) was calculated based on Wald's test of the Cox regression parameter, i.e. on the log rate ratio scale for testing the null hypothesis. All P values were two-sided, and the statistical significance level was set to 0·05.
The associations were evaluated with and without adjustment for baseline values of potential confounders, they being established risk factors for endometrial cancer and obtainable from the questionnaires: parity (yes or no), number of births (n, continuous), age at first birth (continuous), menopausal status (premenopausal or postmenopausal), use of HRT (current, former or never), type of HRT among users (unopposed oestrogen, combination or other), smoking (current, former or never) and BMI (kg/m2, continuous).
The association between enterolactone and endometrial cancer is presented as IRR associated with a 20 nmol/l increment in enterolactone concentration. The continuous analyses were supplemented with categorical analyses, where women were categorised into quartiles based on the distribution of enterolactone among subcohort members.
Possible interactions between enterolactone and the potential effect modifiers, menopausal status, use of HRT and BMI, were investigated. We tested whether the slopes for enterolactone at each level of the potential effect modifiers differed significantly from a single common slope using the likelihood ratio test.
All quantitative variables were entered linearly into the models, as this is biologically more reasonable than the step function corresponding to categorisation and furthermore increases the statistical power of the analyses(Reference Greenland16, Reference Greenland17).
Administration of antibiotics reduces the intestinal microflora and thereby the plasma concentration of enterolactone(Reference Kilkkinen, Pietinen and Klaukka18). Women with a relatively low enterolactone concentration may therefore comprise a heterogeneous group of women with a long-term low-enterolactone concentration and women with a short-term low-enterolactone concentration due to recent use of antibiotics. Thus, the second quartile was used as a reference group. A possible deviation from a linear association was evaluated with linear splines, with one boundary placed at the quartile 1 border based on the distribution among the subcohort. When including all women, a significant deviation from linearity (P =0·001) was present, which, however, disappeared when excluding women in the lowest quartile (P =0·37).
SAS version 9.1 (SAS Institute, Inc.) on a TextPad/Unix platform was used for statistical analyses.
Results
The median time from baseline to endometrial cancer diagnosis was 5·5 years, with a range from 0 to 11·8 years. The baseline characteristics of subcohort members and cases are presented separately in Table 1 for plasma enterolactone concentration and selected potential and established risk factors for endometrial cancer. The concentration of enterolactone was slightly lower among cases than among women in the subcohort, while cases were moderately older. Number of births and age at first birth among parous women did not differ, while a larger fraction of cases was nulliparous than subcohort members. More cases were postmenopausal and a greater proportion was present or former users of HRT than subcohort members, and among present users of HRT, a slightly higher fraction of cases used unopposed oestrogen. Furthermore, cases had a moderately higher BMI and fewer were present smokers at baseline than subcohort members. The distribution of risk factors among the included and excluded cases was rather similar, with the exception of smoking, where a lower proportion of the excluded cases was smokers at baseline (results not shown).
Table 1 Baseline characteristics of endometrial cancer cases and subcohort members nested within the ‘Diet, Cancer and Health’ cohort (Medians and 5th and 95th percentiles; percentages)

HRT, hormone replacement therapy.
* Among parous women.
† Among users.
The baseline characteristics of all women are presented in Table 2 according to the enterolactone levels among the subcohort members. The risk factors for endometrial cancer do not seem to differ systematically according to the levels of enterolactone.
Table 2 Baseline characteristics of women within the ‘Diet, Cancer and Health’ cohort according to the enterolactone levels among the subcohort members (Medians and 5th and 95th percentiles; percentages)
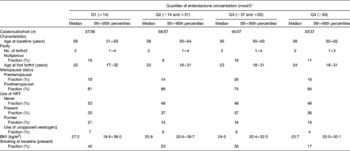
HRT, hormone replacement therapy.
* Cut-point quartiles (nmol/l) based on distribution among subcohort.
† Among parous women.
‡ Among users.
When evaluated linearly, a 20 nmol/l higher level of enterolactone was associated with a statistical borderline lower incidence of endometrial cancer (IRR 0·93, 95 % CI 0·85, 1·01). Adjustment for potential confounders did not change the IRR, but the CI became slightly wider (IRR 0·93, 95 % CI 0·84, 1·04) (Table 3).
Table 3 Endometrial cancer incidence per every 20 nmol/l increment in plasma concentration of enterolactone and when comparing women across quartiles in the ‘Diet, Cancer and Health’ cohort (Incidence rate ratios (IRR) and 95 % confidence intervals)

HRT, hormone replacement therapy.
* Adjusted for baseline values of menopausal status (post or pre), use of HRT (never, former or present), type of HRT (unopposed oestrogen, combination or other), parity (number of births, age at first pregnancy or nulliparity), BMI (kg/m2) and smoking (present, former or never).
† Including all women.
‡ Including all women. Cut-point quartiles (nmol/l) based on distribution among subcohort.
§ Including women with enterolactone >14·3 nmol/l.
Women in quartile 2 were used as a reference when evaluating enterolactone categorically, but none of the point estimates differed statistically significantly from the reference. When excluding women in the lowest quartile, every 20 nmol/l increase in plasma enterolactone concentration was associated with a 13 % lower risk of endometrial cancer when unadjusted (IRR 0·87, 95 % CI 0·77, 0·98). However, the association was no longer statistically significant after adjustment for potential confounders (IRR 0·90, 95 % CI 0·79, 1·02) (Table 3).
Potential effect modification by menopausal status (postmenopausal or premenopausal), use of HRT (never, former or present) and BMI ( ≤ 25, 25–30 or ≥ 30 kg/m2) on the association between plasma enterolactone concentration and endometrial cancer risk was evaluated after excluding women in quartile 1, but no modifications were observed (all P≥ 0·08) (Table 4).
Table 4 Endometrial cancer incidence per every 20 nmol/l increment in plasma concentration of enterolactone stratified by menopausal status, use of hormone replacement therapy (HRT) and BMI, respectively, in the ‘Diet, Cancer and Health’ cohort (Incidence rate ratios (IRR) and 95 % confidence intervals)

* Adjusted for baseline values of menopausal status (post or pre), use of HRT (never, former or present), type of HRT (unopposed oestrogen, combination or other), parity (number of births, age at first pregnancy or nulliparity), BMI (kg/m2) and smoking (present, former or never). Menopausal status, use of HRT and BMI were not adjusted for in the analyses stratified for these variables.
† Among postmenopausal women.
Discussion
In models adjusted for potential confounders, we found a non-significant lower risk of endometrial cancer associated with a higher concentration of plasma enterolactone (IRR 0·93, 95 % CI 0·84, 1·04 for every 20 nmol/l). After excluding the women with a low enterolactone level ( ≤ 14·3 nmol/l), the association became slightly stronger but remained non-significant (IRR 0·90, 95 % CI 0·79, 1·02 for every 20 nmol/l). The association between enterolactone and endometrial cancer did not differ between different categories of BMI, use of HRT or menopausal status.
The primary strengths of the present study include the prospective study design, the objective measure of and relatively large variation in exposure as well as detailed information on potential confounders. Selection bias, information bias and confounding were not considered problematic, as revealed by the prospective study design, a nearly complete follow-up (99·5 %) and the objective measure of exposure along with valid and complete registries for outcome measurement(Reference Storm, Michelsen and Clemmensen19). However, the present study is limited by the relatively small number of endometrial cancer cases, making it difficult to detect a small or moderate effect of enterolactone, if one exists. The study has 80 % power to detect a 40 % decrease in risk. This means that a true effect of a more moderate magnitude may be missed.
Enterolactone was measured in a single non-fasting baseline sample regarded to reflect long-term exposure, which might be reasonable due to a relatively slow elimination, precursors in many commonly consumed food items(Reference Milder, Kuijsten and Arts20) and enterohepatic circulation(Reference Adlercreutz21). Mean elimination half-life for enterolactone is 12·6 h, while mean residence time is 35·8 h for enterolactone(Reference Kuijsten, Arts and Vree22). However, studies disagree on the suitability of using a single non-fasting sample(Reference Hausner, Johnsen and Hallund23, Reference Zeleniuch-Jacquotte, Adlercreutz and Akhmedkhanov24), which might introduce exposure measurement error, potentially causing an attenuation of the association. Additionally, information on administration of antibiotics was not available, probably contributing further to exposure measurement errors. Quartile 2 was therefore used as a reference in the categorical analyses, and continuous analyses were presented both with and without women from quartile 1. Unexpectedly, the IRR of quartile 1 was of similar magnitude to the IRR of quartile 4. An IRR corresponding to a weighted average of quartiles 2, 3 and 4 would have been more biologically plausible.
Only one previous study has investigated circulating enterolactone concentrations in relation to risk of endometrial cancer(Reference Zeleniuch-Jacquotte, Lundin and Micheli7). The nested case–control study included 153 cases, aged 56–70 years, from cohorts in New York, Sweden and Italy. Enterolactone was not associated with a lower endometrial cancer incidence, neither when the full study population was evaluated nor after stratifying by menopausal status. The authors only presented results for a categorical evaluation of enterolactone, where risk is assumed to be the same within categories, which can be seen as a limitation. Risk estimates were only adjusted for BMI, as further adjustment did not affect the results, while type of HRT was not evaluated. The study evaluated effect modification by cohort and results were pooled even though the test was borderline significant (P =0·06). The relatively small number of cases might have limited the power to detect small or moderate effects in both the present and the previously published study. The median level (5–95 %) of enterolactone was lower in the previous case–control study (cases: 19 nmol/l (2–68), controls: 19 nmol/l (3–56)) than in the present study (Table 1), whereby it might have been more difficult to identify a potential association in the previous study due to a relatively homogeneous exposure level. Estimation of lignan intake by FFQ in the two American case–control studies(Reference Horn-Ross, John and Canchola8, Reference Bandera, Williams and Sima9), including 482 and 417 cases, respectively, is limited by intake measurement methodologies and problems associated with estimating the precise content of lignans in foods included in the FFQ(Reference Lampe25). When comparing studies using plant lignan intake as an exposure to studies using circulating enterolactone, it must be regarded that enterolactone quantifies a combination of plant lignan intake and microflora capacity.
The primary consideration in relation to generalisability in the present study is the limited selected age range as well as potential differences among participants and non-participants, where participants might be healthier in general, partly explained by a higher socio-economic status(Reference Tjonneland, Olsen and Boll10).
In conclusion, the findings from the present substudy provide some support for a possible inverse association between plasma enterolactone concentration and endometrial cancer incidence, although further studies with higher statistical power and information on antibiotic use are required to confirm the associations.
Acknowledgements
We gratefully acknowledge the contribution of Katja Boll and Jytte Fogh Larsen in the collection of data and Winnie Østergaard Thomsen for excellent technical assistance. The present work was supported by the Danish Cancer Society (DP06012) and NordForsk (the Nordic Center of Excellence HELGA (070015)). Neither of the funding agencies has had any influence on the design and conduct of the study; collection, management, analyses and interpretation of the data; or preparation, review or approval of the manuscript. A. T., K. O., A. O., C. K., E. W., K. E. B. K. and J. A. designed and conducted the research; J. C. and J. A. analysed the data; J. A., C. K., and A. O. wrote the paper with help from A. M. L. W., N. F. J., K. O., E. W., K. E. B. K. and M. K. K. E. B. K. was responsible for the biological analyses. All authors read and approved the final manuscript. The authors have no conflicts of interest to report.






