Recent meta-analysis has shown that only 13.5% of patients with schizophrenia achieve recovery and outcome has not improved over the years.Reference Jääskeläinen, Juola, Hirvonen, McGrath, Saha and Isohanni1 Despite active research, not many potentially modifiable predictors of outcomes have been identified. The duration of untreated psychosis (DUP) has been one of the most commonly studied predictors of the outcome of schizophrenia.Reference Marshall, Lewis, Lockwood, Drake, Jones and Croudace2,Reference Perkins, Gu, Boteva and Lieberman3 The correlation between long DUP and poor outcome in the first years of illness has been systematically shown.Reference Marshall, Lewis, Lockwood, Drake, Jones and Croudace2,Reference Perkins, Gu, Boteva and Lieberman3 The evidence for sustainable improvements in outcome by shortening DUP is inconclusive and methodically challenging. Follow-up studies of at least 5 years have shown that the beneficial effects of early intervention may not persist in the long term.Reference Bertelsen, Jeppesen, Petersen, Thorup, Øhlenschlaeger and le Quach4,Reference Gafoor, Nitsch, McCrone, Craig, Garety and Power5 In one study with a follow-up of 10 years, early detection of psychosis was associated with higher recovery rates and employment but also with higher levels of excitative symptoms.Reference Hegelstad, Larsen, Auestad, Evensen, Haahr and Joa6 The long-term consequences of prolonged untreated psychosis are unclear,Reference Penttilä, Miettunen, Koponen, Kyllönen, Veijola and Isohanni7-Reference Dassa, Boyer, Benoit, Bourcet, Raymondet and Bottai9 with no previous systematic meta-analysis with a wide perspective of outcomes focusing also on the length of follow-up. Our aim was to analyse the associations between length of DUP and long-term outcomes of schizophrenia. Our hypothesis was that long DUP associates with poor long-term clinical and social outcomes. In addition, we aimed to explore the effects of the proportion of male participants, the age at illness onset, the length of DUP, proportion of cases of schizophrenia, withdrawal percentage, length of follow-up and income level of the country on correlation between DUP and outcome.
Method
We applied the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines for systematic reviews and meta-analyses of observational studies.Reference Stroup, Berlin, Morton, Olkin, Williamson and Rennie10 With the help of an information scientist (N.H.) relevant literature was searched from Scopus, PubMed, Science Direct, ISI Web of Knowledge, PsycINFO (Ovid), CINAHL (EBSCO) and Academic Search Premier (EBSCO) databases in May 2013, using the following search strategy: (”duration of untreated psychosis” OR “delay in treatment” OR “treatment delay” OR “initiation of treatment” OR “duration of untreated illness”) AND (psychosis OR “psychotic disorders” OR schizophrenia OR schizoaffective OR schizophreniform) (online Appendix DS1). No language, publication date or publication status restriction was imposed and the search was directed to all fields. Non-English articles were translated if necessary. Articles found through citations, reviews and meta-analyses were included in our meta-analysis.Reference Jääskeläinen, Juola, Hirvonen, McGrath, Saha and Isohanni1 Authors of included samples were contacted for unpublished data. All abstracts were analysed by one author (M.P.). The excluded abstracts were then reviewed by another author (E.J.) and problematic cases were assessed by three authors (M.P., E.J. and J.M.). For studies that met inclusion criteria, a second investigator (E.J. or J.M.) checked the data accuracy. When a disagreement occurred related to data extraction, this was resolved by consensus. In keeping with related systematic reviews of schizophrenia epidemiology,Reference Jääskeläinen, Juola, Hirvonen, McGrath, Saha and Isohanni1,Reference McGrath, Saha, Welham, El Saadi, MacCauley and Chant11 we evaluated the quality and characteristics of the included studies (online Appendix DS2). Information on the data collected from the included studies is presented in online Table DS1.
Study selection
The articles included in the analyses were required to meet the following criteria:
(a) the sample included at least 50% of individuals with schizophrenia and at least 75% of individuals were diagnosed with schizophrenia, schizophreniform, schizoaffective or delusional disorder (i.e. broadly defined schizophrenia);
(b) structured diagnostic system criteria were used;
(c) the sample size was 20 or more;
(d) the study assessed the association between DUP and at least one of clinical or social outcomes (defined later) or quality of life with minimum length of follow-up of 2 years;
(e) the definition of DUP was clear and comparable with other studies (the definition used was time between the onset of first-episode psychosis and first treatment, specifically antipsychotic medication, psychosocial treatment, contact with treatment services or first hospital admission after the onset of psychosis).
Prospective, cross-sectional and retrospective study designs were included, including register-based studies and observational clinical samples. Randomised controlled trials were excluded because of their specific inclusion criteria which limit the representativeness of these samples. Where several papers were available on the same or overlapping cohorts, we selected the results from the studies that had longest follow-up when there was no major difference in withdrawal rate. If a study had less than the required percentage of participants with schizophrenia but the results for this subgroup were presented, the subgroup results were included. Authors of excluded studies were contacted for unpublished data if inclusion was considered possible. Details of the excluded studies are available from the authors on request, and some examples are presented in online Appendix DS3. Online Appendix DS4 lists the references for the included studies.
Outcome
Outcome was categorised into nine groups: general symptomatic outcome, positive symptoms, negative symptoms, clinical remission, social functioning, employment, global outcome, quality of life and hospital treatment. The outcome categories were chosen to describe different dimensions of the outcome in schizophrenia.Reference Menezes, Arenovich and Zipursky12,Reference Shrivastava, Johnston, Shah and Bureau13 Factors such as suicidality, insight, excitement and depression were not included in the meta-analysis as they were reported in only a few studies.Reference Penttilä, Miettunen, Koponen, Kyllönen, Veijola and Isohanni7,Reference Parellada, Boada, Fraguas, Reig, Castro-Fornieles and Moreno14,Reference Nielssen, Malhi, McGorry and Large15 General symptomatic outcome describes all of the symptoms, for example as total symptoms, unspecified symptomatic remission or recovery, or score on the Clinical Global Impression (CGI) scale. Specific symptom dimensions analysed in the meta-analysis were positive and negative symptoms (Table DS1). We studied clinical remission separately using the definition of Andreasen et al,Reference Andreasen, Carpenter, Kane, Lasser, Marder and Weinberger16 which is a structured, widely used and accepted definition of remission in schizophrenia. Other measurements of relapse or recovery were included in the general symptomatic outcome category. Nowadays, recovery in schizophrenia is commonly defined as remission of symptoms and improvement of social functioning.Reference Faerden, Nesvåg and Marder17 When the definition of recovery was not clearly described in the original studies, we assumed that recovery indicated diminished symptoms.Reference Jääskeläinen, Juola, Hirvonen, McGrath, Saha and Isohanni1,Reference Faerden, Nesvåg and Marder17
Hospital treatments were defined as the estimated number of hospital admissions and/or days in hospital to describe the utilisation of psychiatric services, in contrast to general symptomatic outcome. Hospital admission may be a proxy measure of severity of illness, for example relapse, but other factors (related to the patient, healthcare staff, method of treatment, organisation and family) may also account for its use. Social functioning was included when studies reported occupational and social functioning using measures such as the Social and Occupational Functioning Assessment Scale (SOFAS). Specific definitions of social functioning and social activities such as hobbies and social support were also included. Employment was included when the level of work or education or the receipt of disability pension was recorded, using information from registers, interviews or questionnaires. This category describes the actual work or study that can be measured as days or percentage of time. The assessed employment and disability pension can be affected by ability of work, general employment in society and level of social security.
Global outcome included combinations of outcome variables estimating both clinical and social aspects or a single global outcome measure such as the Global Assessment of Functioning (GAF) scale. Quality of life was included from studies that had estimated the correlation between DUP and various quality of life scales. This category was created to describe participants’ subjective assessment of satisfaction.
Statistical analysis
Based on the expected heterogeneity of the associations between DUP and outcomes, we used random effects models to pool overall estimates of effect sizes. In the random effects analysis each study was weighted by the inverse of its variance and the between-studies variance. Results from unadjusted analyses were included if they were given in the original studies. The effect of DUP was estimated using correlation coefficients with 95% confidence intervals. If original studies presented other effect measures these were transformed to correlations using formulas presented by Rosenthal and colleagues.Reference Rosenthal, Cooper and Hedges18,Reference Rosenthal, Rosnow and Rubin19 If the studies presented more than one effect measure for the same outcome group in the same sample, the average of these correlations was used in the meta-analysis. Correlation coefficients can be interpreted as effect sizes that are small (0.10), moderate (0.30) or large (0.50).Reference Cohen20 In our study negative correlation indicates that long DUP associates with poorer outcome, for example more severe symptoms and decreased functionality.
We studied the heterogeneity of the studies (i.e. how much the studies were assessing the same effect size) using the I 2 statistic. The statistical significance in heterogeneity was tested using the chi-squared test.21 Values of I 2 range from 0% to 100%, reflecting the proportion of the total variation across studies beyond chance: 25% is low, 50% moderate and 75% high heterogeneity or major excessive variation across studies.Reference Higgins, Thompson, Deeks and Altman22 In additional analyses we used meta-regression to estimate the effect of possible confounders on the correlations in different outcome groups.Reference Sterne23 Included potential confounders were gender distribution (proportion of male participants), mean age at onset, mean length of DUP, proportion of participants diagnosed with schizophrenia, percentage withdrawing, study design, mean follow-up length and income level of the country (economic index of the country based on per capita income World Bank statistics for 1988; data.worldbank.org): low-income (US$1005 or less), lower-middle income ($1006-3975), upper-middle income ($3976-12 275) and high-income economies ($12 276 or more).
We also made an influence analysis in which the meta-analysis estimates were computed omitting one study at a time. Possible publication bias was studied using the Begg’s test for small-study effects.Reference Sterne23 An alpha level of 0.05 was used for all statistical tests. Stata version 11 for Windows21 was used in all analyses.
Results
The search produced 4495 results and, after the removal of duplicates, 3493 publications were identified. Based on the information on abstracts, 193 articles were selected for comprehensive evaluation and 56 articles were found from other sources, leading to a total of 249 articles that were evaluated. Thirty-nine articles analysing 33 different samples met our inclusion criteria and were included in the meta-analysis (Fig. 1). Main reasons for exclusion were that the study did not analyse DUP (52 studies) or its association with long-term outcome (53 studies), or the outcome studied did not meet the inclusion criteria (e.g. cognition: 50 studies).
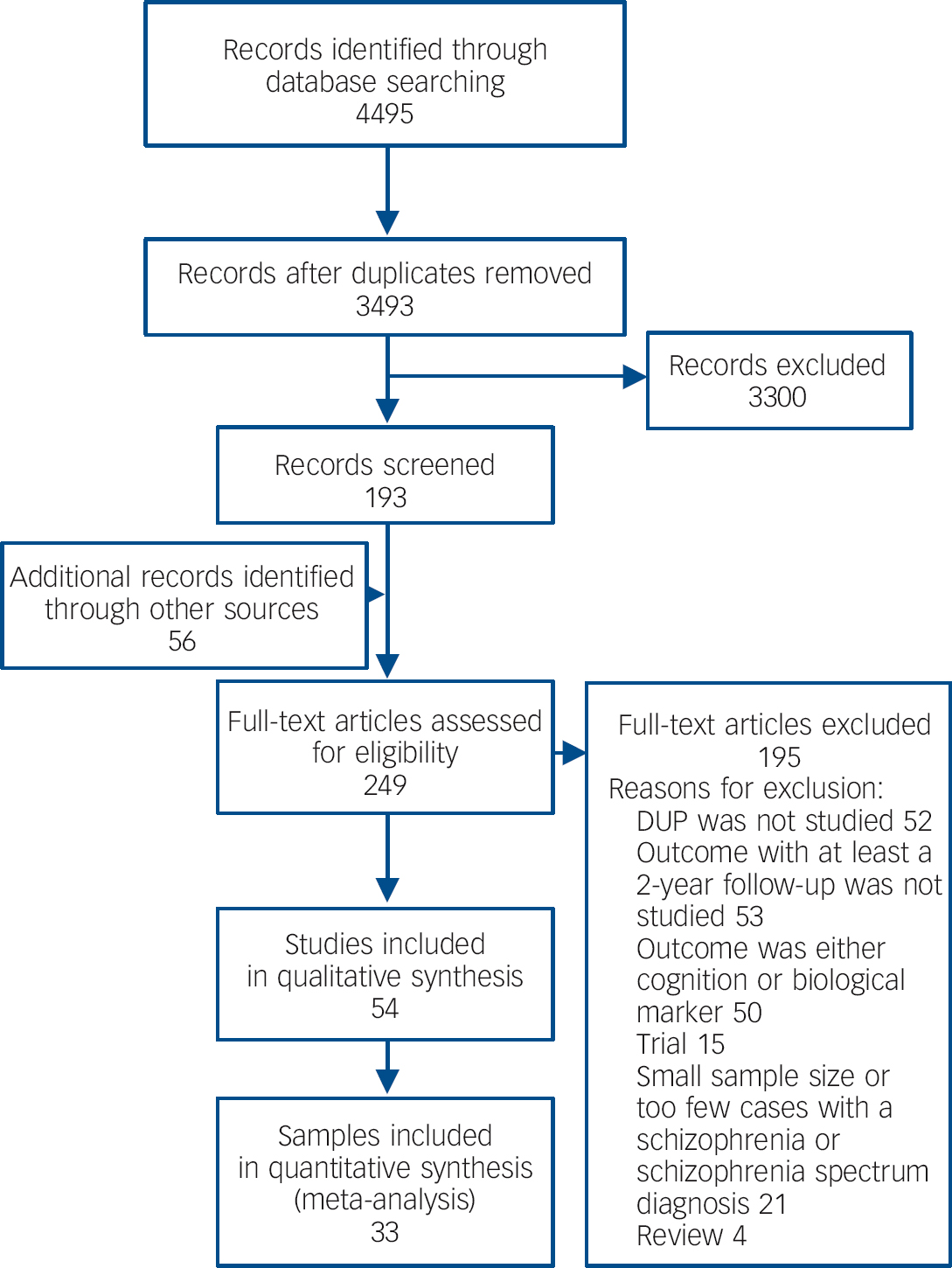
Fig. 1 Literature search and selection of the studies (adapted from the PRISMA flowchart, www.prisma-statement.org DUP, duration of untreated psychosis.
Study characteristics and quality
Table DS1 reports the main characteristics of studies included in the meta-analysis. In these studies mean age at onset was 24.4 years (range 12.2-31.5), mean length of follow-up was 8.1 years (range 2-28), mean length of DUP was 61.3 weeks (range 10.4-213.2) and, on average, 50.5% (range 29.8-77.3) of the samples were male. Withdrawal percentages were 4-71%, and exceeded 50% in five samples; for two studies information on number of participants leaving the study was not available. Included studies did not use any statistical method to take attrition into account in analyses. Sample sizes at the end of the follow-up period varied between 23 and 776. Study populations were mostly clinical samples drawn from people with first-episode psychosis from both out-patient and in-patient care; 13 samples were drawn from one type of care only. This information was not available for two samples. Diagnoses were classified mainly based on DSM-III-R (5 studies), DSM-IV (18 studies), ICD-9 (4 studies) and ICD-10 (4 studies). The percentage of participants with a diagnosis of schizophrenia was 60-100%. Duration of psychosis was mostly defined using interviews; the method used for its definition was not reported for 10 samples. Outcomes were most frequently defined using validated scales, but in some studies the scale or its use were not clearly reported. Interrater reliability was rarely estimated for the definition of DUP or outcomes (Table DS2).
The number of studies in different outcome categories varied from 7 to 19. The correlations between length of DUP and outcomes of original studies are presented in Table DS3. The majority of correlations were unadjusted, with only one study having only adjusted correlations available.Reference Röpcke and Eggers24 Three studies presented one of the several correlations between DUP and outcome only as adjusted.Reference Górna, Jaracz, Rybakowski and Rybakowski25-Reference Hill, Crumlish, Clarke, Whitty, Owens and Renwick27 Details of the results and which of them were transformed into correlations, as well as the covariates used in the original studies, are outlined in Table DS3. When the analyses presented below were done with only unadjusted correlations, the results did not change.
Association between DUP and outcome categories
General symptomatic outcome and its correlation with DUP were available for 15 samples; DUP and both positive and negative symptoms were studied in 18 samples, and remission and its correlation with DUP were obtained from 10 samples. Long DUP associated with more severe outcome in all these categories (general symptomatic outcome: r = –0.15, 95% CI –0.22 to –0.09; positive symptoms: r = –0.14, 95% CI –0.22 to –0.07; negative symptoms: r = –0.13, 95% CI –0.21 to –0.05; remission: r = –0.14, 95% CI –0.23 to –0.06). The estimated correlation between DUP and hospital treatment from 11 samples was small and not statistically significant (r = –0.09, 95% CI –0.22 to 0.04). Long DUP correlated with poor social functioning (14 samples, r = –0.18, 95% CI –0.27 to –0.09). There was no correlation between DUP and employment (7 samples, r = –0.05, 95% CI –0.16 to 0.06). Long DUP correlated with poor global outcome (19 samples, r = –0.17, 95% CI –0.26 to –0.07). A small but statistically non-significant correlation between DUP and quality of life was found (7 samples, r = –0.10, 95% CI –0.22 to 0.01). Forest plots including correlations (with 95% CIs) in individual studies in the different outcome categories are presented in online Figs DS1-DS9. The overall correlations in different outcome categories are summarised in Fig. 2.
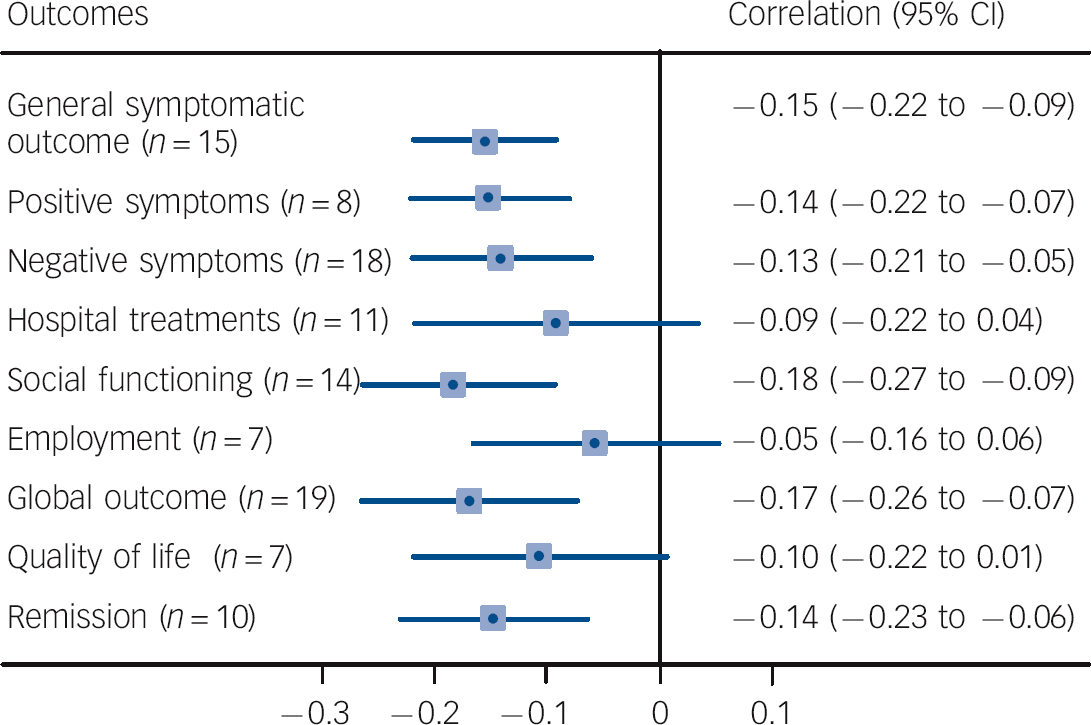
Fig. 2 Correlations between duration of untreated psychosis (DUP) and clinical outcomes, hospital treatment and social functioning. Negative correlation indicates that long DUP is associated with poor outcome (n, number of studies).
Heterogeneity
Categories of positive symptoms (I 2 = 56.1%, P = 0.002), negative symptoms (I 2 = 66.1%, P<0.001) and remission (I 2 = 54.7%, P = 0.019) as well as general symptomatic outcome were statistically significantly and moderately heterogeneous (I 2 = 38.9%, P = 0.061). There was high and significant heterogeneity between studies of DUP and hospital treatment (I 2 = 75.8%, P<0.001). Studies of social functioning (I 2 = 68.2%, P<0.001), employment (I 2 = 55.1%, P = 0.038), global outcome (I 2 = 73.8%, P<0.001) and quality of life (I 2 = 55.0%, P = 0.038) were all moderately heterogeneous.
Covariates in meta-regression
In additional analyses several study characteristics were used as potential confounders in meta-regression. Gender distribution, onset age, length of DUP, the proportion of participants with schizophrenia, withdrawal percentage and study design did not affect the correlation between DUP and outcomes. Longer follow-up resulted in stronger associations between DUP and negative symptoms (P = 0.035), hospital treatment (P = 0.046) and global outcome (P = 0.035). Higher national income level resulted in stronger correlation between DUP and general symptomatic outcome (P = 0.008) and positive symptoms (P = 0.016) (online Table DS4).
Influence analysis and publication bias
In the influence study correlations were not affected statistically significantly when one study was excluded at a time. In the analyses of publication bias, statistically significant bias was not found in Begg’s test for small-study effects.
Discussion
We found a significant association between long DUP and poor general symptomatic outcome, more severe positive and negative symptoms and failure to achieve remission, as well as decreased social functioning and global outcome. There was no significant correlation between DUP and employment, quality of life or hospital treatment. Few of the correlations tended to be stronger in studies with longer follow-up and in countries with higher level of income. The relatively high withdrawal rate in the original studies and variation in the methods of defining DUP and outcomes increased the risk of selection and information bias.
Comparison with earlier studies
Previous systematic reviews and meta-analyses of DUP and outcome of schizophrenia have mainly focused on the short-term outcome. The general conclusion of previous reviews was that short DUP seemed to be related to better outcome, whereas long DUP was related to poorer clinical and functional outcome and quality of life.Reference Marshall, Lewis, Lockwood, Drake, Jones and Croudace2,Reference Perkins, Gu, Boteva and Lieberman3 The small correlations between long DUP and poor clinical outcome are similar to earlier meta-analyses.Reference Marshall, Lewis, Lockwood, Drake, Jones and Croudace2,Reference Perkins, Gu, Boteva and Lieberman3 Boonstra et al found that over an 8-year follow-up period the correlation between long DUP and negative symptoms increased from r = 0.12 at baseline to r = 0.20,Reference Boonstra, Klaassen, Sytema, Marshall, De Haan and Wunderink28 which is in line with our finding that the correlation between DUP and negative symptoms was stronger when follow-up was longer. The correlations between DUP and remission (as defined by Andreasen et al Reference Andreasen, Carpenter, Kane, Lasser, Marder and Weinberger16) and hospital treatment have not previously been subjected to meta-analysis. The correlation between long DUP and a decline in social functioning seems to be small, but significant also in the long term. We were the first to study DUP and employment in meta-analysis, and found no significant association.
In meta-regression the length of follow-up had a statistically significant effect on the correlation between DUP and negative symptoms, hospital treatment and global outcome. Interestingly, the correlation between long DUP and poor outcome was stronger in longer follow-up periods. This does not prove that long DUP causes poor outcome,Reference McGlashan29 but may indicate that participants with longer DUP have a different type of illness or different coping mechanisms for the symptoms, as well as different cognitive performance from some participants with short DUP. For example, it is possible that more severe negative symptoms, as part of an insidious mode of onset, are one reason for longer DUP,Reference Compton, Chien, Leiner, Goulding and Weiss30,Reference Compton, Gordon, Weiss and Walker31 and this type of disorder relates to poor prognosis. This association could remain during the course of illness. It is debatable whether shortening the DUP would decrease negative symptoms, as current treatment options do not generally greatly improve the outcome of such symptoms.Reference Tandon32
A previous review suggested that the correlation between DUP and outcome in developing countries was somewhat contradictory as the DUP tended to be longer but remission rates were higher, despite some correlation between long DUP and poor outcome.Reference Chiliza, Asmal and Emsley33 Our meta-analysis gives only limited information on differences between countries based on the level of income. There was no study from a low-income country and only a few (from none to four) studies from countries with lower- or higher-middle level of income in each of the outcome categories. However, the correlations between DUP and general symptomatic outcome and positive symptoms seemed to be smaller in countries with a lower income level.
Methodological discussion and risk of bias
Varying degrees of heterogeneity were found between studies in different outcome categories. This possibly reflects the heterogeneity of DUP and the measures of outcome used. The heterogeneity between studies indicates methodological differences and differences in clinical protocols between countries’ treatment units. Both of these could affect not only the estimation of DUP and outcomes, but may also have confounding effects on both of them. The definition of DUP is challenging and the comparison between participants and samples based on the length of DUP is not always exact. The reasons behind the prolonged periods of untreated psychosis may vary. It might be due to poor insight and more severe types of disorder, but equally in some individuals it could reflect good coping abilities and levels of support, allowing people with psychotic symptoms to live without resorting to mental healthcare and without an accurate diagnosis. The characteristics of local health services may also affect the length of DUP.Reference Tandon32
Defining DUP in a standardised fashion could be one way to decrease variability between studies. The use of a proposed definition of DUP, which takes into account not only the duration of symptoms but also their severity, could be a more accurate means of measuring the potential harmful effects of DUP and reducing the levels of heterogeneity found in our study.Reference Compton, Gordon, Weiss and Walker31 Unfortunately detailed assessment of DUP in many of the included studies was not possible owing to limited information given on the methods of defining DUP and their reliability. A number of studies did use structured interviews with more than one source of information, which can be considered reliable, and studies that did not clearly define and separate DUP from (for example) duration of untreated illness were excluded.
Different aspects of possible bias need to be considered. Selection bias may have been present in the original studies as participants with better or worse outcomes might have been left out during the several years of follow-up, and perhaps more probably patients with long DUP might have been more difficult to engage during the study. Some of these issues could be minimised in future studies with more synchronised study designs and systematic measurements of exposure and outcome. In observational designs, investigations are at risk of confounding. The DUP most probably affects treatment in a way that might confound the association between DUP and outcomes. Some confounders, such as personal characteristics of temperament, may affect both DUP and treatment adherence.Reference Dassa, Boyer, Benoit, Bourcet, Raymondet and Bottai9 Mode of onset is another possible confounding factor.Reference Moncrieff34 However, this was taken into account in four of the original samples without significant effect on the correlation between DUP and outcome.Reference Penttilä, Miettunen, Koponen, Kyllönen, Veijola and Isohanni7,Reference Ichinose, Nakane, Nakane, Kinoshita, Ohta and Honda35-Reference Chang, Tang, Hui, Lam, Wong and Chan37 Norman et al found no significant correlation between DUP and mode of onset and found significant correlation with outcome and both of them in only two of eight outcome variables,Reference Norman, Manchanda, Windell, Harricharan, Northcott and Hassall38 whereas Selten et al found significant association (P<0.001) between mode of onset and poor outcome, but no clear association with DUP and poor outcome (P = 0.08).Reference Selten, Veen, Hoek, Laan, Schols and van der Tweel39 However, in forthcoming studies mode of onset or other markers of severity of the early phase of illness should be taken into account.
Owing to the methodological variation between original studies we were unable to analyse systematically the effect of all possible confounders, but using meta-regression variables such as gender and age at onset seemed to have no major confounding effect. The method of meta-regression used is not the most efficient way to study possible confounders, but as original studies rarely studied confounders, this was our only option. Additionally, the possibility of multiple testing and low number of studies in some of the outcome categories should be noted. Therefore, the possible confounding bias should be considered when interpreting the results of this meta-analysis.
Another methodological challenge was the possible correlation between different outcome categories. Owing to our definition of general symptomatic outcome, results from PANSS scores could have been included in both general symptomatic outcome and positive and negative symptoms. This should also be considered when interpreting the results. As the original studies did not study the correlations between different outcomes, it was not possible to analyse the effect of these correlations in our meta-analysis.
Positive study findings are more likely to be reported than negative findings, which may bias the results of meta-analysis of observational studies. The negative finding regarding publication bias needs to be assessed with caution because the method used (Begg’s test) is not very powerful in detecting bias with a small number of included studies. The observed heterogeneity between studies also presents a challenge in synthesising their results. Our approach, using random effects models, can be considered reliable for studying this sort of data. Sample sizes of included studies varied from 23 to 776, with the majority of studies having relatively small samples. Most of the studies had quite high rates of withdrawal during the follow-up period, which increases the risk of selection bias. The possibility of outcome reporting bias was reduced by contacting authors for their unpublished results and data.
Strengths and limitations
The literature search for the meta-analysis was done using several databases. Articles published in languages other than English were included and were translated by professionals. We also used criteria requiring the majority of participants to have been diagnosed with schizophrenia and at least three out of four with schizophrenia spectrum disorder, which is somewhat stricter than the criteria used in previous meta-analyses.Reference Perkins, Gu, Boteva and Lieberman3 Some studies with remarkably different definitions of DUP were excluded from the meta-analysis.Reference Compton, Gordon, Weiss and Walker31 We were not able to include some of the earliest studies of delayed treatment and long-term outcome in schizophrenia,Reference Moncrieff34-Reference Bottlender, Sato, Jager, Wegener, Wittmann and Strauss36 owing to variations in definitions of diagnosis and DUP. Most of the studies published before the 1990s defined DUP as the duration of symptoms prior to treatment and no information was provided as to whether these symptoms were positive or negative and what threshold was defined for their onset.Reference Rupp and Fletcher40,Reference Achte41 The end of DUP had also been defined as the beginning of antipsychotic treatment in one sample, in which participants had their first episode of psychosis in the pre-antipsychotics era, leading to DUPs of over 10 years.Reference Scully, Coakley, Kinsella and Waddington42 However, the results of these studies were similar to our findings: Rupp & Fletcher found that duration of symptoms (especially if more than 2 years) before treatment decreased the probability of the improvement of outcome,Reference Rupp and Fletcher40 and Scully et al concluded that more severe negative symptoms were predicted by longer DUP.Reference Scully, Coakley, Kinsella and Waddington42 The exclusion of randomised controlled trials, most notably the OPUS trial, should not cause an underestimation of the correlation between DUP and outcome in this meta-analysis.Reference Jeppesen, Petersen, Thorup, Abel, Øhlenschlaeger and Christensen43,Reference Petersen, Thorup, Øqhlenschlaeger, Christensen, Jeppesen and Krarup44
There are limitations in this study’s design. Possible differences in the original samples may have affected our results and conclusions. There were only 7 to 19 samples in the different outcome categories. The studies also differed largely in terms of the research methods used. As the original studies presented their results with various effect size measures, we were forced to convert them to correlations using previously presented equations.Reference Rosenthal, Cooper and Hedges18,Reference Rosenthal, Rosnow and Rubin19 These conversions can create inaccuracy, as the equations for the conversions are based on normal distribution.Reference Rosenthal, Cooper and Hedges18,Reference Rosenthal, Rosnow and Rubin19 However, the use of random weights is an advantage and reduces the risk of such inaccuracies. Most of the studies had analysed the association between DUP and symptoms or global outcome. Owing to the small number of studies definitive conclusions should not be made regarding the longitudinal effects of DUP on, for example, employment and quality of life.
Implications
When developing new treatments for schizophrenia it is important to have a broad knowledge of the effects of current treatment options and periods when the illness has not been treated. Possible differences in the lifestyles of patients with long DUP, compared with those with short DUP, could provide new information for use in the treatment of schizophrenia. It has previously been shown that more severe negative and depressive symptoms correlated with decreased quality of life in schizophrenia,Reference Tomotake45 and early intervention might not be able to improve the quality of life in this disorder.Reference Thorup, Petersen, Jeppesen and Nordentoft46 Therefore, the factors behind our finding that people with long DUP might have as good a quality of life as those with shorter DUP should be studied further. Future studies of DUP and outcome should use more standardised methods for defining both DUP and outcomes. It would also help the generalisation of results in clinical practice if potential confounders were approached more systematically in studies.
The small correlation between long DUP and poor long-term outcome indicates that early intervention and care in psychosis might have some positive effects on the long-term outcome on schizophrenia. However, drawing evidence-based clinical conclusions from analyses using natural experiments and observational designs is problematic as it is neither possible nor ethical to randomise people to different conditions regarding DUP. It is likely that in the long term other factors (such as individual characteristics, social support and treatment factors) are more influential than DUP in determining outcomes. However, the constant, subtle correlation between long DUP and poor outcome dictates that periods of untreated psychosis should be shortened whenever possible.
Funding
This work was supported by Oulu University Hospital, University of Oulu, the Academy of Finland; the Sigrid Jusélius Foundation; National Alliance for Research in Schizophrenia and Affective Disorders (NARSAD): The Brain and Behavior Research Fund (Dr Mortimer D. Sackler Developmental Psychobiology Research Program); the Oulu University Pharmacy Foundation; H. Lundbeck; the Northern Finland Health Care Support Foundation; and the Jalmari and Rauha Ahokas Foundation.
Acknowledgements
We thank Dr David Cowling for proofreading the manuscript. We acknowledge the contribution of all contacted authors who responded and especially Drs Robert Boden, Svein Friis, Ingrid Melle and Ghada Hassan for providing unpublished results or data for the analyses in this meta-analysis.





eLetters
No eLetters have been published for this article.