Introduction
Worldwide, chronic obstructive pulmonary disease (COPD) affects millions of people (Mannino and Buist, Reference Mannino and Buist2007) and places a significant demand on health resources (Price et al., Reference Price, Lowe, Hosker, Anstey, Pearson and Roberts2006). There is limited data on the prevalence of COPD in South Africa, but the Burden of Obstructive Lung Disease Initiative found that almost a quarter of participants sampled in communities in Cape Town had some degree of airways obstruction, with more advanced stages of disease being strikingly more prevalent than in the other 11 countries sampled (Buist et al., Reference Buist, McBurnie, Vollmer, Gillespie, Burney, Mannino, Menezes, Sullivan, Lee, Weiss, Jensen, Marks, Gulsvik and Nizankowska-Mogilnicka2007). Smoking, occupational exposure and tuberculosis are important probable causes of chronic lung disease in South Africa (Ehrlich and Jithoo, Reference Ehrlich and Jithoo2005).
Multidisciplinary care in patients with COPD has enjoyed much attention in the last decade, with promising outcomes in symptomatology, exercise tolerance, quality of life and cost of care (Man et al., Reference Man, Polkey, Donaldson, Gray and Moxham2001; Moullec and Ninot, Reference Moullec and Ninot2010; Kruis AL et al., Reference Kruis, Smidt, Assendelft, Gussekloo, Boland, Rutten-van Mölken and Chavannes2011; Puhan et al., Reference Reda, Kotz, Kocks, Wesseling and van Schayck2011; Van Wetering et al., 2010). However, literature mainly stems from developed countries and there remains a lack of research on this approach in poorer countries and communities, especially in Africa.
Avian Park is a low socio-economic community located outside the town of Worcester in the Western Cape of South Africa. Twenty-seven per cent of the population is functionally illiterate, and 24% live below the poverty line and experience food insecurity (Heinecken et al., Reference Heinecken, Vorster and du Plessis2011). A primary healthcare site supported by Stellenbosch University’s Rural Clinical School offered a platform to mobilise a student-run healthcare team to provide a multidisciplinary, home-based intervention.
Methods
This was a prospective, quasi-experimental before-and-after intervention that took place over three months.
Recruitment
Patient records at Avian Park Service Learning Centre were hand searched to identify adult community members known with COPD. Patients were excluded if they had moved outside of Avian Park or lived in areas inaccessible or regarded as unsafe for home-based interventions; if they were wheelchair or bedbound, or had severe mental disabilities.
Twelve patients met the inclusion criteria and all initially consented to participate in the programme.
Intervention
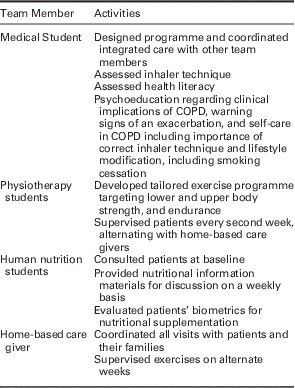
Patients were visited at their homes on a weekly basis by one or more members of a team consisting of a home-based caregiver, a medical student, a physiotherapy or a human nutrition student. The content of the programme is shown in Table 1. Qualified practitioners supervised all student activities.
Table 1 Roles and responsibilities of the multidisciplinary, home based team
Outcome measures
Primary outcome measures
Physiological and quality of life metrics were measured at week 0, week 6 and week 12. The percentage forced expiratory volume in one second (FEV1%) was measured by means of a mobile spirometry device (Alcomed SP10 Digital, Alcomed, Cape Town, South Africa); exercise tolerance was evaluated by the 6-min walk test (6-MWT), and disease specific quality of life was measured using a validated Clinical COPD Questionnaire (CCQ) (Reda et al., 2010). The Body mass index, airflow Obstruction, Dyspnoea and Exercise capacity (BODE) prognostic index was calculated using a combination of FEV1%, 6-MWT, Modified Medical Research Council Scale for Dyspnoea, and body mass index (BMI) (Celli et al., Reference Celli, Cote and Marin2004).
Secondary outcome measures
Inhaler technique and patient disease-specific insight were assessed at week 0, week 6 and week 12. Inhaler technique was assessed using a standardised stepwise approach with video demonstration of how to use a metered-dose inhaler (UTAH Asthma Program, Reference Van Wetering, Hoogendoorn and Broekhuizen2011). Patients were divided into three groups to grade their level of disease-specific insight, namely informed, poorly informed and uninformed. Patients were considered ‘informed’ if they could identify their diagnosis as COPD and showed some insight into the aetiology and principles of self-care, ie, the rationale of using metered dose inhalers and prevention of exacerbations. Patients were considered ‘poorly informed’ if they could identify their diagnosis as COPD, but lacked further insight. Those who could not identify their diagnosis as COPD and lacked general insight, were considered to be ‘uninformed’.
Data analysis
Data were recorded on a paper data sheet that was transferred to an Excel spreadsheet. Differences in the paired before-and-after observations from participants were analysed using the paired t-test and an on-line statistical calculator (Statgraph). Statistical significance was set at P⩽0.05.
Ethics approval was granted by Stellenbosch University’s Human Research Ethics Committee.
Results
At baseline 12 patients, nine female and three male, took part in the programme, but five subsequently withdrew at an early stage. When questioned about the reason for withdrawal, most reported that they found the exercises challenging and thought they might be harmful.
Of the seven patients who completed the programme, six were female and one male. Ages ranged between 31 and 71, with a mean age of 57. Four patients were former smokers and three were current smokers. Two patients had contracted pulmonary tuberculosis (PTB) once before and one had contracted PTB four times previously. BMI measurements at baseline indicated that one patient was underweight (BMI=17.6), one patient morbidly obese (BMI=56.3) and five patients were within a normal range.
The baseline FEV1% and 6MWT for patient 7 were lost and so results from the CCQ, inhaler technique and COPD knowledge only were used for this patient.
Primary outcomes
Week 0 versus week 6
By week 6 there was no significant improvement in the FEV1%, 6MWT or BODE index. The quality of life (CCQ) assessment showed improvement in the symptom score only (P=0.03).
Week 0 versus week 12
Paired before-and-after observations at baseline and at 12 weeks are shown for the participants who continued the programme in Table 2. A statistically significant improvement in the FEV1% of mean 8% was seen, together with a significant mean improvement in the quality of life scores. One patient developed claudication symptoms in the course of the three-month intervention and had a deterioration in walking distance while respiratory parameters improved. The mean increase in the 6 min walking distance was not statistically significant for the group as a whole. The improvement in the BODE prognostic index also failed to reach statistical significance.
Table 2 Baseline and 12 week results for the seven patients remaining in the study
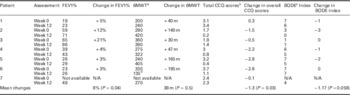
a 6MWT=six minute walk test.
b CCQ=clinical COPD questionnaire. A lower score indicates an improved quality of life score.
c BODE=a multidimensional prognostic index. A lower score indicates an improved prognosis.
d Patient 6 developed claudication symptoms during the course of the intervention.
Secondary outcomes
Five of seven patients at baseline demonstrated an inappropriate inhaler technique. At week 6, three of seven patients continued to use their inhalers incorrectly. At week 12, two patients were still using their inhaler incorrectly.
When insight regarding COPD was assessed at baseline, five patients reported that they had no knowledge of COPD and two reported that they only knew the term of their diagnosis and lacked further insight. At week 12, five patients demonstrated adequate insight about COPD and two patients still reported that they were only familiar with the term ‘COPD’.
Discussion
There has been growing recognition that muscle wasting, exercise avoidance and poor participation in daily activities contribute to a poor quality of life in patients with COPD (McCarthy et al., Reference McCarthy, Casey, Devane, Murphy, Murphy and Lacasse2015). The addition of tailored therapies that include exercise training and patient education is increasingly referred to as ‘pulmonary rehabilitation’, and a recent Cochrane report concluded that pulmonary rehabilitation improves quality of life, while noting that there is still uncertainty over how best to deliver it (McCarthy et al., Reference McCarthy, Casey, Devane, Murphy, Murphy and Lacasse2015).
Although the numbers in this pilot project were small, a home-based multidisciplinary team of students and home-based caregivers working in a low income peri-urban community was able to produce measureable and statistically significant improvements in the FEV1%, and the disease specific quality-of-life scores in those patients who completed a three-month programme.
However, potentially important constraints on the provision of community-based multidisciplinary care in this context were also identified. Five of 12 patients withdrew from the study at an early stage, and had we decided to analyse these results on an ‘intention to treat’ basis, we could not have concluded that the programme resulted in health gains. While the relatively high proportion of withdrawals limits the conclusions that can be drawn, feedback from these patients provided interesting insight into patient motivation and attitudes around exercise in this community. It was clear that several patients thought that exercise was harmful to them because it caused fatigue and they could not be persuaded otherwise. These attitudes may be worth exploring in future studies. Although one patient was underweight and qualified for therapeutic nutritional supplementation, supplements could not be provided as a result of lack of stock and the prioritising of other medical conditions. In a population experiencing a quadruple burden of disease, where older adults are often malnourished (Charlton and Rose, Reference Charlton and Rose2001; Marais et al., Reference Marais, Marais and Labadarios2007), widening access to adult nutritional interventions may result in health service cost savings in the long term and this is an argument that needs to be made at policy level.
These findings also demonstrate how students can contribute to clinical care in low-income communities. ‘Service learning’ is growing in importance as several African countries, including South Africa, are in the process of a substantial scale-up of health professions training – a scale up that exceeds the capacity of traditional tertiary teaching platforms (Mullan et al., Reference Mullan, Frehywot, Omaswa, Buch, Chen and Greysen2011; Bateman, Reference Bateman2013). If clinical training is to be accommodated on a decentralised teaching platform, students need to find ways to add value to health services as they learn. We found that health literacy was low and most patients were not using their inhalers correctly; together with a tailored exercise programme and nutritional advice, this COPD intervention had measureable benefits to those participants who completed the programme, and could safely and appropriately be delivered by supervised students working in a team with home-based caregivers at minimal cost to state funded health services. In addition to improving chronic disease control, there are also potential educational advantages as this type of intervention offers an opportunity for students to learn about collaborative healthcare, the delivery of primary healthcare at community level, and the reality of everyday life for many of their future patients.
Conclusion
A home-based, multidisciplinary student team approach showed positive results in improving the functional status and quality of life of those patients living with COPD in a low-income setting in South Africa who were willing to complete a three-month pulmonary rehabilitation programme. However, the high dropout rate limits the conclusions that can be drawn from this self-selected, more motivated group. Exercise avoidance limits the potential efficacy of this type of programme.
Acknowledgements
The authors would like to acknowledge the contributions of Postia Makhele and the Home Based Care Team at Avian Park Service Learning Centre; Jana Muller (Physiotherapy lecturer at the Rural Clinical School); Elria Joubert (Human Nutrition lecturer at the Rural Clinical School), and Francois Coetzee (Family Physician at the Rural Clinical School).
Financial Support
This study was supported by the Stellenbosch University Rural Medical Education Partnership Initiative (SURMEPI), which is supported by the President’s Emergency Plan for AIDS relief (PEPFAR) [T84HA21652].
Conflicts of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.





