Introduction
This paper focuses on the practice of low-intensity cognitive behavioural therapy (LICBT), by evaluating adaptations to the therapeutic strategies and techniques that focus on managing anxiety and depression for autistic adults. It additionally provides patient feedback that specifies examples of adaptations to session content, structure, and environment. This paper contributes to an emerging body of research into the efficacy and best practice of adapting CBT for autistic people and adds to limited available research regarding low-intensity techniques. This has the potential to increase psychological wellbeing practitioners’ (and CBT therapists’) confidence in adapting for this patient group. Furthermore, it may influence an introduction to a universal offer of adapted low-intensity provisions for autistic adults within NHS Talking Therapies Services (NHS-TTS).
Autism and mental health
Autism is a neurodevelopmental condition, and its diagnosis is determined by the presence and interaction of social communication and interaction difficulties, and restrictive patterns of behaviour and sensory integration differences (Baker and Jeste, Reference Baker and Jeste2015; Centers for Disease Control and Prevention, 2022). It is termed a spectrum condition because every autistic individual presents differently; this is not necessarily a linear, high-to-low spectrum, but where every autistic person has varying traits, resulting in different strengths and challenges (Jack, Reference Jack2022; Stark et al., Reference Stark, Ali, Ayre, Schneider, Parveen, Marais, Holmes and Pender2021b). Autism and mental health conditions often co-exist, with eight in ten autistic adults experiencing mental health problems in their lifetime, with anxiety and depression being most common (All Party Parliamentary Group on Autism, 2019; National Autistic Society, 2021). Additionally, it was reported that three in ten autistic adults fell into the severe depression category, and more than half fell into the severe anxiety category when examining psychometric measures (National Autistic Society, 2021). This demonstrates that these conditions are often experienced at high severity.
Anxiety disorders have the highest prevalence within the autism community at 20%, compared with 7.2% within the general public (Stark et al., Reference Stark, Ali, Ayre, Schneider, Parveen, Marais, Holmes and Pender2021b). The reason for this is complex and multifaceted; for instance, Stark et al. (Reference Stark, Ali, Ayre, Schneider, Parveen, Marais, Holmes and Pender2021b) suggest it could be contributed to by factors like alexithymia (difficulties recognising and regulating emotions), masking, double-empathy problems with neurotypicals and executive functioning differences. Additionally, Oakley et al. (Reference Oakley, Loth and Murphy2021) argue that autism lived experiences, such as bullying due to social-communication differences, increases vulnerability to chronic stress and mental health conditions. The increased anxiety and depression which autistic individuals experience has detrimental impacts, as autistic people were found to be 7.5 times more likely to die by suicide compared with the general population (Hirvikoski et al., Reference Hirvikoski, Mittendorfer-Rutz, Boman, Larsson, Lichtenstein and Bölte2016). Thus, it is imperative that autistic people are able to access and receive effective psychological treatment.
Organisational issues
A stepped care approach is used within NHS-TTS (previously known as Improving Access to Psychological Therapies, ‘IAPT’), so clients face the least intrusive treatment first (Thieme, Reference Thieme2021). Initial treatment involves LICBT, also called ‘guided self-help’, and is commonly offered to those with depression or anxiety disorders (National Collaborating Centre for Mental Health, 2023). It consists of short-term skills-based support, focusing on a single mental health problem, and can be delivered online, in groups or one-to-one (Bennett-Levy, Reference Bennett-Levy2006; Papworth, Reference Papworth2018; National Collaborating Centre for Mental Health, 2023). High-intensity support offers longer term CBT or counselling for those with social anxiety, post-traumatic disorder, more severe presentations, or where further support following LICBT is required (Bennett-Levy, Reference Bennett-Levy2006; Papworth, Reference Papworth2018; National Collaborating Centre for Mental Health, 2023).
The number of autistic adult referrals to talking therapy is expected to be high nationally. However, many autistic adults experience challenges in accessing an NHS-TTS, which is the predominant provider of cognitive behavioural therapy (CBT) in England (National Collaborating Centre for Mental Health, 2023). El Baou et al. (Reference El Baou, Bell, Saunders, Buckman, Mandy, Dagnan, O’Nions, Pender, Clements, Pilling, Richards, John and Stott2023) examined 8593 autistic patients that accessed an IAPT treatment between 2012 and 2019 and found depression and anxiety scores decreased for most, although were less likely to meet recovery and reliability criteria and had lower rates of treatment retention to adults without identified autism. They also found autistic adults were more likely to receive high-intensity CBT and be identified as unsuitable for IAPT; however, it was undetermined whether the received treatment was adapted.
Reliance on self-referral, rigid completion of screening tools, professionals lacking autism awareness, misattribution of symptoms and non-adapted therapy are some reasons why treatment retention and access rates are low for autistic adults within NHS-TTS (All Party Parliamentary Group on Autism, 2019; National Autistic Society, 2021). Yet, the Autism Act (2009), National Institute for Health and Care Excellence (2021) and NHS (2019) state that adaptations are required in mental health settings to ensure that autistic adults have equal access to treatment. Therefore, it is imperative that clinicians are willing to adapt their practice to increase effectiveness of CBT for this client group. However, adaptations are rarely available as practitioners lack training due to limited research in the field, reducing confidence to adapt (Brice et al., Reference Brice, Rodgers, Ingham, Mason, Wilson, Freeston, Le Couteur and Parr2021; Cooper et al., Reference Cooper, Loades and Russell2018).
Adaptations
Providing prior information to minimise uncertainty, autism awareness training, a sensory friendly environment, using direct and concrete language with written and verbal aids, and linking with autism specialist services and other caregivers, are adaptations all healthcare settings can make to improve access for autistic people (National Autistic Society, 2021; National Institute for Health and Care Excellence, 2021; Petty et al., Reference Petty, Bergenheim, Mahoney and Chamberlain2021). Additional adaptations for CBT include flexible session structure, incorporating special interests, emphasising on changing behaviours, providing emotional literacy, and incorporating psychoeducation on autism, such as the overlap with symptoms and completing sensory profiles (Russell et al., Reference Russell, Jassi and Johnston2019; Stark et al., Reference Stark, Ali, Ayre, Schneider, Parveen, Marais, Holmes and Pender2021b).
A meta-analysis by Weston et al. (Reference Weston, Hodgekins and Langdon2016) found a small to medium effect size of CBT for adults with autism and affective disorders; however, it is unclear whether autism adaptations were made. Additionally, a systematic review conducted by Spain et al. (Reference Spain, Sin, Chalder, Murphy and Happé2015) found adapted CBT was moderately effective for autistic adults with co-occurring anxiety and depression. Yet, limitations included small sample sizes, widely varied adaptations, and validity of self-report psychometric measures with autistic people have been widely debated. Research on adapting CBT for autistic adults is limited as existing research largely focuses on child populations; thus, suggested adaptations may be unsuitable for adults as they have greater autonomy and awareness (Kerns et al., Reference Kerns, Roux, Connell and Shattuck2016). Petty et al. (Reference Petty, Bergenheim, Mahoney and Chamberlain2021) also highlighted a lack of qualitative research involving the autistic community. Hence, further exploration into the effectiveness of adapted CBT for autistic adults is required, along with their perspectives into what specific adaptations are most useful.
Much of current literature focuses on adapting CBT in line with what is offered at high-intensity CBT, and there has been limited research into adapting LICBT for autistic adults. Nonetheless, the pilot randomised control trial (RCT) of Russell et al. (Reference Russell, Gaunt, Cooper, Barton, Horwood, Kessler, Metcalfe, Ensum, Ingham, Parr, Rai and Wiles2020) investigated the feasibility of adapting LICBT within NHS-TTS across two regions for 70 autistic adults with depression. The treatment included autism-trained practitioners, increased session time and frequency, and autism psychoeducation. The depression and anxiety mean scores for the adapted treatment group had minimal reduction at 24-week follow-up, but the study was not powered to detect differences between the treatment groups. However, they found the adapted treatment group had greater retention to those receiving treatment as usual. The qualitative findings of Horwood et al. (Reference Horwood, Cooper, Harvey, Davies and Russell2021) indicated that previous negative experience of non-adapted treatment may have limited retention and recruitment of the study; however, there was a preference for the adapted treatment, as participants appreciated practitioners’ increased awareness of autism. Therefore, further investigation into adapted LICBT for adults with autism and co-occurring affective disorders is needed to determine whether adaptations improve outcomes.
Aims of the present study
It is of great concern that autism and mental health conditions have a high co-morbidity rate, impacting not only physical and mental wellbeing, but also mortality. Therefore, it is necessary that autistic people can access and receive effective psychological treatment. However, research in this field is currently lacking, especially regarding LICBT. Hence, further research is required to investigate clinical outcomes and experiences of LICBT for autistic people with co-occurring anxiety and depression, as this could improve accessibility and treatment quality this client group receives across NHS-TTS. Therefore, the focus of this study is to evaluate adapted LICBT treatment pathways offered within Plymouth’s NHS-TTS and Autism Service.
This study aims to investigate whether anxiety and depression severity was lowered for autistic adults who completed either of the adapted LICBT interventions (group or one-to-one) by comparing routine outcome measures (ROMs) at the start and end of treatment. ROMs are hypothesised to show lower scores on completion across both interventions. Co-production with service users was deemed important as it fosters, as far as possible, an environment whereby research is conducted ‘with’ the community, rather than ‘about’ them, thus helping them feel empowered, enabled, and advocated for (Stark et al., Reference Stark, Ali, Ayre, Schneider, Parveen, Marais, Holmes and Pender2021a). Therefore, an additional objective was to explore autistic service users’ perspectives on the treatments to understand which aspects and adaptations are deemed favourable, and what further improvements can be made from their recommendations.
Method
Service evaluation overview
This study uses a mixed-method design to evaluate treatment pathways between two services based in the Southwest of England, Plymouth Autism Spectrum Service (PASS), and Plymouth NHS-TTS (Plymouth Options). PASS is a specialist autism service offering adult autism assessments, advice, and training and consultation (Livewell Southwest, n.d.-b). The advice service offers post-diagnostic signposting support to adults with autism and their families and works collaboratively with local services to improve support provided to autistic people. Plymouth Options is a part of a network of NHS-TTS found across England. They provide evidence-based psychological treatments like CBT to clients with common mental health problems, such as anxiety and depression (Livewell Southwest, n.d.-a). Three psychological wellbeing practitioners (PWPs) employed by Plymouth Options were appointed and trained as neurodiversity champions to facilitate sharing of information, training, and referrals between the services. They also delivered adapted LICBT provisions including a co-created psychoeducational group, and one-to-one guided self-help.
The psychoeducational group focused on providing learning on anxiety and autism, and CBT skills to support symptom management. The group consisted of six weekly sessions of two hours long, had a maximum of ten clients face-to-face, and delivered within PASS’s facilities. Each session focused on an aspect of the CBT cycle and LICBT techniques, with additional content on communication and lifestyle. The session is supplemented with a specifically designed PowerPoint presentation and printed workbook. Psychoeducation on autism characteristics runs throughout; for example, information on sensory integration differences. Sessions are slow paced, highly interactive, and use clear and plain language.
The one-to-one guided self-help similarly supports anxiety and depression management, by working through a single LICBT technique (such as behavioural activation). An average of six sessions were completed, ranging from 35 to 60 minutes long, held within either services facilities or virtually. Each session focused on a step of the LICBT technique and its associated home practice task; for example, completing a session of behavioural activation may have focused on an activity diary worksheet. The CEDAR LICBT workbooks by Farrand et al. (Reference Farrand, McGahey and Woodford2022) were commonly used materials supplementing this treatment; however, other resources, such as videos/apps, may have been used. Practitioners integrated psychoeducation on autism within sessions when appropriate and adapted their practice differently depending on clients’ individual needs; some examples include flexible verbal and written communication, such as direct language and simple worksheets. A flexible session structure was offered, and discussions took place on creating a sensory-friendly environment within treatment.
Participants
A homogeneous and purposive sampling strategy was employed, because it enabled participants to be selected based on if they had completed the evaluated treatments. All participants were patients of PASS and met their criteria (formally diagnosed with autism and 18+ years old). All PASS patients identified as having co-existing mental health difficulties were able to opt into attending the psychoeducational course. PASS also referred patients to Plymouth Options who met the NHS-TTS criteria (mild to moderate levels of anxiety and depression with no active risk) who had a preference for one-to-one treatment, or if it was clinically indicated as more appropriate to the group. The one-to-one participants were patients of PASS and Plymouth Options and underwent an assessment with a neurodiversity champion (PWP) to ensure symptomology was eligible for step 2 intervention, before commencing treatment.
Table 1 provides the gender, age, ethnicity, and session distribution collected from health records at data collection. ROMs from initial and final treatment sessions were collected. This is pre-existing data and was collected from PASS and Plymouth Options databases from September 2020 to July 2023. Service users are informed at time of entering PASS and Plymouth Options that ROMs are used for service auditing and evaluation, and no participants opted out. Eighty-five participants (56 in one-to-one and 29 in group treatments) were excluded from data collection due to not completing the treatment protocol or being ineligible. Ten participants completed both treatments, which was deemed an insignificant number to analyse, but to reduce bias, their second treatment scores have been excluded to ensure independence between treatment groups.
Table 1. Demographic distribution of the quantitative participants

The 84 participants were sent an information sheet via their preferred mode of contact inviting them to participate in an interview. Six participants were recruited as they positively responded and were available in the data collection time frame. Table 2 presents their demographic information. The participants experienced different practitioners, and treatments at differing times and locations. Due to autistic service user involvement, accessibility to participate was considered; therefore, at expression of interest, a support form was offered to be completed with the researcher to reduce participant burden and recruitment barriers.
Table 2. Demographics of the qualitative participants (n=6)

Materials and procedure
The ROMs consist of two standardised published questionnaires. The Patient Health Questionnaire (PHQ-9) is a reliable 9-item measure of depression severity (Kroenke et al., Reference Kroenke, Spitzer and Williams2001). Similarly, the Generalized Anxiety Disorder Questionnaire (GAD-7) is a valid 7-item measure to assess severity of general anxiety (Spitzer et al., Reference Spitzer, Kroenke, Williams and Löwe2006). Both questionnaires ask, ‘Over the last two weeks, how often have you been bothered by any of the following problems?’, and list items which require a selection of one number (0=‘not at all’, 1=‘several days’, 2=‘more than half the days’ or 3=‘nearly every day’). The PHQ-9 items consists of statements like ‘Little interest or pleasure in doing things?’, ‘Feeling down, depressed, or hopeless?’, ‘Feeling tired or having little energy?’. The GAD-7 items consists of statements like ‘Feeling nervous, anxious or on edge?’, ‘Not being able to stop or control worry?’, ‘Feeling afraid as if something awful is going to happen?’. Item scores are added with the total score falling into either a minimal (0–4), mild (5–9), moderate (10–14), moderately severe for PHQ-9 (15–19) and severe for PHQ-9 (10–17) and GAD-7 (15–21).
ROMs are self-administered via a webform or on paper, although participants were able to request support with completing questionnaires from a clinician within sessions. Individuals who access an NHS-TTS routinely complete ROMs in treatment sessions which are stored so their progress can be tracked, which allows effectiveness of psychological interventions like LICBT to be investigated (National Collaborating Centre for Mental Health, 2023). The PHQ-9 and GAD-7 are well-validated measures for detecting and monitoring depression and anxiety within the general public (Kroenke et al., Reference Kroenke, Spitzer, Williams and Löwe2010). However, Cassidy et al. (Reference Cassidy, Bradley, Bowen, Wigham and Rodgers2018) argue that these measures less accurately predict clinical diagnosis in those with autism as their factor structure may not be sensitive to autistic patients’ unique experiences; hence, internal consistency may be lower. The PHQ-9 nonetheless was found to have strong internal consistency and convergent validity within an autism sample, as a bi-factor analysis identified the presence of an overall depression factor (Arnold et al., Reference Arnold, Uljarević, Hwang, Richdale, Trollor and Lawson2020). However, the GAD-7 has not yet been validated for use within an autistic sample (El Baou et al., Reference El Baou, Bell, Saunders, Buckman, Mandy, Dagnan, O’Nions, Pender, Clements, Pilling, Richards, John and Stott2023).
Interviews lasted for 60 minutes, were audio recorded, and used a semi-structured format. Topic questions were designed based on existing knowledge of the treatment pathway and from literature on adapting CBT for autistic people. Questions included how participants found the preparation for treatment, environment, structure, therapeutic relationship, content, and materials (see supplementary material for topic guide). This method generated rich data on experiences of adapted LICBT and helped inform what further improvements can be made (Braun and Clarke, Reference Braun and Clarke2013). Participants were made aware of the interview structure, aims and types of questions before arranging the interview. Information gathered from the support form enabled interviews to be tailored to participants, such as including breaks, having shorter interviews over two meetings, and enabling a flexible venue for the interview either at PASS or online via Microsoft Teams. Further verbal instruction on what to expect was provided, demographic information was gathered, and informed consent was confirmed before commencing interview recording.
Analysis
Qualitative interviews were transcribed using the Microsoft Word transcribe feature and followed an orthographic transcription style, in which all verbal utterances and vernacular terms are recorded (Braun and Clarke, Reference Braun and Clarke2013). Researcher H.T. conducted a thematic analysis using Braun and Clarke’s (Reference Braun and Clarke2021) framework. This included ensuring that data were familiar by re-reading the transcriptions. Initial codes were generated by taking transcriptions at face value, and semantically coded by labelling relevant information using a phrase to capture its meaning. In line with the aims of this research, quotes were selected when positive and negative experiences of treatment, along with recommended improvements, were identified. Codes were then clustered into themes and reviewed and defined before being reported. This process was overseen by the two other researchers (S.H. and S.W.) to minimise bias, by discussing emerging themes, subthemes and codes, with a joint agreement of the final structure of themes and the thematic map.
Collected data (ROMs) was processed within R (R Core Team, 2021). A factorial ANOVA was completed for each psychometric measure using the afex package (Singmann et al., Reference Singmann, Bolker, Westfall, Aust and Ben-Shachar2022). The two-level between-subject variable is treatment (group or one-to-one); the two-level within-subject variable is time (pre- and post-treatment scores). Post-treatment scores were predicted to be lower than pre-treatment scores for both treatment conditions; thus, a main effect of time was expected. Furthermore, an interaction between treatment and time was explored to determine whether one treatment had different ROM scores than the other. A power analysis was also completed in R and G*Power (Faul et al., Reference Faul, Erdfelder, Buchner and Lang2009).
Results
The quantitative data present findings from a 2×2 mixed factorial ANOVA for both PHQ-9 and GAD-7 psychometric measures. This is followed by reporting of qualitative data, presented through a thematic analysis where four themes and nine subthemes emerged.
Quantitative findings
Statistical results revealed lower scores in anxiety and depression symptoms on completion of both interventions; Figs. 1 and 2 display a greater distribution of people within the negative range. They also show that the GAD-7 and one-to-one treatment had a higher distribution within the negative range, indicating a larger difference in questionnaire scores over time compared with the PHQ-9 and group treatment condition.

Figure 1. Density plot of difference for GAD-7.

Figure 2. Density plot of difference for PHQ-9.
Main effect of time
The two-factor within-subject variables differentiated between time questionnaire scores were taken as either pre- or post-treatment. Figure 3 illustrates differing averages for GAD-7, with a 12.85 average for pre-treatment scores and 8.68 for post-treatment. Figure 4 shows differing averages for the PHQ-9, with an average of 14 for pre-treatment and 10.71 for post-treatment scores. Time had a significant main effect on symptoms, as F 1,82=92.34, p=<.001, η2=.134 for GAD-7, and F 1,82=39.86, p=<.001, η2=.060 for PHQ-9. A post-hoc power analysis for the t-tests showed a power of .99 (both measures) for n=84 and d=0.75 (GAD-7) and d=0.48 (PHQ-9; i.e. for detection of small-medium effects).

Figure 3. GAD-7 mean difference between 4 factors.

Figure 4. PHQ-9 mean difference between 4 factors.
Main effect of treatment type
The two-factor between-subject variables differentiated between treatment type, as either one-to-one or group conditions. Averages between these conditions differed slightly across both psychometric measures. The GAD-7 had a 10.61 average for the one-to-one condition, and a 10.92 for group (Fig. 3). The PHQ-9 had a 12.01 average for the one-to-one, and 12.7 for the group (Fig. 4). However, there were no significant differences for either GAD-7, F 1,82=0.08, p=.776, or the PHQ-9, F 1,82=0.26, p=.614. This indicates no evidence of a main effect of treatment type alone on symptoms. A post-hoc power analysis for the t-tests showed a power of .05 (GAD-7) and .07 (PHQ-9) for n=40 and d=0.05 (GAD-7) and d=0.10 (PHQ-9; i.e. for detection of negligible effects).
Interaction between time and treatment type
The difference of differences between the within-subject variables (pre- and post-treatment scores) and between-subject variables (one-to-one, group) for GAD-7 was 3.22, and 2.98 for PHQ-9 (Figs 3 and 4). The lines in the graphs cross, suggesting an interaction between time and treatment on symptoms. This was supported by a significant interaction for GAD-7, F 1,82=13.78, p=<.001, η2=.023, and PHQ-9, F 1,82=8.46, p=.005, η2=.013. A post-hoc power analysis for the f-tests showed a power of 1.0 (both measures) for n=84 and f=.41 (GAD-7) and f=.32 (PHQ-9; i.e. for detection of medium to high effects).
Qualitative findings
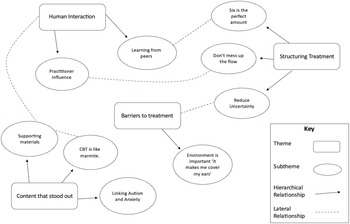
The following themes focus on different aspects of treatment that people favoured and recommendations on areas for improvement (Table 3 and Fig. 5).
Table 3. Table exploring thematic themes of autistic service users’ experiences of adapted low-intensity CBT


Figure 5. Thematic analysis map.
Human Interaction
Interacting with others was an important function for treatment; for instance, the social interaction required when attending a group was daunting, yet listening to one another gave participants confidence to express themselves openly.
‘As there were conversations it almost inspired me to offer my own opinion, managed to step out of my shell because other people also were kind of had the courage to do it themselves, so after they did it, it was more along the lines of following suit’ (Henry, p 4).
There were different factors that helped elicit human interaction, such as running the group face-to-face: ‘I enjoyed the face to face because it made the group discussions very personable, and it was … nice to come into a session every week and see the same people and kind of hear their experiences in person’ (Jack, p 14). Supporting conversations between people about their lives and the content on anxiety helped participants trust others within the group and open up: ‘just hearing about other people’s lives, like, just generally not necessarily just like ohh my anxiety this … I remember the dude that had the bike and it was just kind of like, ok these are nice people’ (Tish, p 9). Icebreakers also supported this: ‘introducing bit was very interesting to me because I’ve got to like … know some positive facts about different people’ (John, p 2), although they need to be adapted for autistic people within the group, as Tish said, ‘it was one of the best icebreakers that I’ve been a part of because there was like an answer, you know, so like rather than just share a fun fact’ (p 19). This highlights that icebreakers need to be specific in what they are asking and only require direct answers to avoid putting people on the spot.
A casual atmosphere within the group helped create a safe space for people to express themselves: ‘the casual atmosphere actually made it easier to be more upfront and thorough with my explanations’ (Henry, p 13). Henry also explained how the casual atmosphere came about: ‘chairs positioned however you want them and people just in their casual clothing no particular formal attire required and even the presenters of it in their own casual attire being relaxed’ (p 14). This quote demonstrated that clients’ freedom to wear what they like, and the facilitators being in casual clothes rather than uniform, helped make the space feel relaxed, making conversation easier. Having the ability to ask questions within the group when they arose, rather than at specific points, also supported a casual atmosphere, as Jack stated:
‘People were encouraged … to just shout it out if you need to or raise your hand however you need to … It kind of lent itself to that very free flow nature … there would be points where we would say right we’re gonna have a group discussion now but I think that the really important ones are the ones that just came up naturally through questions’ (p 9).
Having a free-flow nature to group discussions should, however, not impede on people having a space to talk without interruptions: ‘I want to have like my turn to speak … I need to say make sure I don’t get any interruptions’ (John, p 11).
The facilitators giving ideas and demonstrating answers to questions was another way to illicit interaction:
‘I like the fact that like when we did icebreakers or just generally ask questions the presenters would give their thoughts on it as well. So you’d be like ohh ok they’re like human’ (Tish, p 9).
Tish’s use of the word ‘human’ indicates that they welcomed facilitators joining in with icebreakers rather than non-disclosure, which is commonly required of psychological practitioners. The next subtheme ‘Practitioner Influence’ explores the great influence practitioners have on direction of interaction within treatment.
Practitioner Influence
There are positive and negative influences practitioners have on interactions within treatment. Active listening skills and non-judgemental attitudes were some of the main influences participants highlighted in supporting a safe space for people to share: ‘If I was to talk about some problems, whether they can do anything about it or not all that’s important is that they’re always able to listen to you properly’ (John, p 10). Tish also explains how practitioners can express non-judgement when clients ask for clarification:
‘you don’t feel judged when … I’m like sorry my brain forgot to process any of that you’ve just said so they just repeated it and then like added a little bit on or like slowed it down and asked if I was still with it more often and that helped’ (Tish, p 13).
How to approach clients that experience challenges, such as not completing home practice tasks, was also emphasised: ‘if you didn’t manage to get it done this week because it was too much or whatever, it was we can fix it I wasn’t like scolded’ (Tish, p 11). This supports the stance that practitioners that have open curiosity with clients, rather than jumping to conclusions, will have effective interactions. Practitioners understanding autism traits, like communication differences may assist in them adapting their communication to ensure all parties are understood and listened too. For instance, Barry points out: ‘Several people in the first session where … going into the zone, very much hyper fixating on their own specialist interests and how that related to the course material … I could see that [name of facilitator] wasn’t aware’ (p 8).
However, not all participants experienced positive facilitation within group treatment. Barry said, ‘it felt like [name of practitioner] may have been experiencing more anxiety than we were, it was very … other members noticed as well and that was a big thing’ (p 2). Managing the pace of content, time and group dynamics can be difficult as practitioners need to ensure that the group finishes on time, content is covered, whilst ensuring everyone feels heard and has an opportunity to participate. Practitioners with less experience may lack confidence and common factor skills needed to effectively manage this:
‘there was three very chatty people in the group, which meant that we didn’t actually cover all the material that was in the course and then after that from then onwards, every week was very stressed as far as like time management was concerned so it’s more like being able to have a strong leader who can maintain those “No seriously guys, we need to keep this on track”’ (Barry, p 6).
When there is focus from the practitioner to complete treatment on time, it can detract them from being fully engaged with clients, ‘It felt like their time and energy was focused on trying to hold everything together and to finish the course as opposed to fully integrating us into that process’ (Barry, p 8). On the other hand, Tish highlighted an experience where this was managed well within a one-to-one session:
‘I think it was like a 10, 15 minute warning being like by the way not stopping you talking but we’ve only got this amount of time left, so we might have to either do this next bit next session or carry this on next session because we are getting short on time now and having that choice … was nice because I was like ok well they do still want to know about it it’s just that the time’s not there’ (p 13).
It was suggested that practitioners need to consider clients’ lived experience: ‘people coming in with just with some qualifications, but they’re not willing to reconcile with the lived experience in the group’ (Barry, p. 9). This implies there can be a conflict between practitioner being expert of the therapeutic intervention, and the client being expert of lived experience. Therefore, for both of these expertise to be recognised, it is important clients have their experiences heard within sessions.
Learning from peers
Having a group exclusively for autistic people to attend enabled participants to open up and feel more comfortable in interacting: ‘We all felt very safe with each other even though we were all sharing stuff … which they wouldn’t necessarily feel comfortable sharing in a room with neurotypical people’ (Barry, p. 14). A conversation with John also highlighted that he felt confident opening up around neurodiverse peers because he believed they were more understanding of him:
‘you know if I tell them about, why I find it difficult to talk to … ladies about anything, then they would be more understanding. Hope: So, it sounds like from what you’re saying that, being in a room full of other people who have autism made you feel more comfortable to talk about some of your worries? John: Correct, yes’ (p 6).
John’s experience of feeling safer to express himself within a group of autistic individuals could be because of feeling misunderstood when involved in previous groups open to the public. Barry highlights this by explaining autistic people face different challenges to neurotypical people, thus require different solutions:
‘Prefer the idea of it being all neurodivergent, if you’ve got a room full of neurotypical people and neurodivergent people. It can become very confusing as … we could come up with neurotypical solutions or could, because I know that there’s a lot of neurotypical solutions that just don’t work for me’ (Barry, p 13).
Hearing from one another about problems faced, and how each other got on with the interventions also supported learning: ‘it was nice hearing how people remembered what to do in situations rather than just being told what to do’ (Tish, p 1). The group treatment also supported socialisation and meeting new people: ‘definitely meeting other people felt like a really important experience for me to have’ (John, p 2).
Structuring Treatment
This theme contains three subthemes describing factors around preparing, developing, and pacing treatment.
Six is the perfect number
Most participants identified ‘six is a good number’ (Barry, p 5) for the number of people within the group treatment. It is important to get the amount of people within the group right because it ensures a breadth of knowledge is shared, whilst allowing enough time for everyone to talk: ‘you don’t want too many people so that people don’t feel like they are being heard but on the other side of that, the more people involved, the more voices and more experiences you’re going to hear’ (Jack, p 9). Having six people in the group supported this balance:
‘It’s a good number because it wasn’t too little that you knew every single detail of someone’s life, but it was also not too large so that you couldn’t remember who was who, it gave you just enough time to be able to talk about what you wanted to talk about for each person’ (Tish, p 10).
Therefore, this links to the subtheme, ‘Learning from peers’, as having this number of people supported socialisation, and learning from experiences within the group.
Having six sessions within the group treatment was also expressed as being satisfactory: ‘Once a week was appropriate and like six sessions was a reasonable commitment’ (Jack, p 8). However, the one-to-one sessions were identified as being too short in duration and frequency as some identified wanting longer term support: ‘For the one-to-one ones … would have been better being a bit longer because I was still going through a difficult time at that time’ (Freya, p 7). This could be because the group ran for two hours over six weeks, meaning a substantial amount of content was covered, whereas the one-to-one was shorter and focused on one LICBT technique with a lack of opportunity for open discussions or additional topics. Nonetheless, there was a general consensus between participants that follow-ups after completion of treatment would be beneficial: ‘I think you could potentially look at a follow up, like … refreshers for people like a one day overview so people can stay up to date on those skills’ (Jack, p 13). A follow-up would also support continued socialisation: ‘it gives people the opportunity to kind of stay connected to carry on, because the journey continues’ (Barry, p 15).
Don’t mess up the flow
There needs to be a balance between fitting in content within treatment sessions whilst not rushing, as the pace needs to allow participants time to be able to process information. Not having a fixed ending time was given as a recommendation to help manage this: ‘If the time was a little bit more loosened … then some of the sessions wouldn’t need to end up having to be kind of tapered on to the next and get this odd cascading effect’ (Henry, p 5). On the other hand, trying to finish all content within the allocated session time can result in it feeling rushed without enough time to process information:
‘after about five to ten seconds of being asked a question, it was like, right, let’s go on to the next thing and sometimes my brain needs to catch up a little bit so giving more time for people to think … may have been useful’ (Barry, p 10).
This links with subtheme ‘Practitioner Influence’ because if practitioners are anxious, they may rush and not stick to agendas, disrupting the session’s pace.
Trying to get the pace right within treatment sessions is difficult because it is subjective; for one client it may be too fast and for another to slow. For instance, John says: ‘I kind of preferring it to be a little more slower, if I’m honest, because … if the pace was too quick then, I probably wouldn’t have recovered from my anxieties’ (p 8); whereas Tish explained the pace as just right: ‘If the pace had been any slower I think I definitely would have just lost it and like daydreamed, but I think if the pace was any faster I wouldn’t have been able to like retain the information’ (p 8). Therefore, it is important for practitioners to collectively agree with clients the speed of delivery that suits all, which is more difficult within a group.
A recommendation for managing the pace was including breaks: ‘I was very grateful that there was a break in between the two hours because by the time there was a break I was getting like antsy’ (Tish, p 7). However, opinions on their duration differed as some wanted ‘10 to like 15 minutes’ (Barry, p 6), whereas others wanted longer, ‘I would have liked longer like twenty minutes to process information that was talked about’ (Freya, p 9). Jack identifies that there should not be a hard rule for the length of a break; however, a decision should be made between practitioner and client(s): ‘I think it’s down to the facilitators more than anything to gage the room on the day’ (p. 9). Thus, it is important practitioners do not interrupt the flow of their sessions as they need to ensure content is covered, but not at the disadvantage of session content and learning being processed. Breaks are an effective strategy to help manage this.
Reduce uncertainty
When preparing for treatment it is important practitioners set clear expectations beforehand. For instance, providing an agenda, practitioner profiles and ground rules:
‘beforehand … a breakdown of the sessions of what’s going to be covered, so that if there’s any pre questions people are able to do that. A bit of information on the facilitators so that people can kind of meet in advance and also house rules and how the sessions are gonna be handled’ (Jack, p 4).
Having the opportunity to orientate to the environment with a caregiver also helped reduce uncertainty and anxiety for participants: ‘me and mum went in beforehand and had a look at the place so that I knew different ways to get there’ (Tish, p 3). Starting treatment on time was also important: ‘I do find it frustrating when we start five, ten minutes after the course. Time management, making sure we start on time is an important one for me, definitely’ (Barry, p 10). Therefore, any delays in starting treatment, or changes to agendas need to be communicated early and clearly.
Increasing predictability for clients within sessions was favourable: ‘I liked how it had the same structure … you knew what to expect like the break was at the same point every time as well’ (Tish, p 10). Tish also highlights that knowing the layout of the room prior helps reduce uncertainty: ‘I like knowing what the room’s gonna be like, if it’s like a complicated room it’s not clear where you’re supposed to sit … I just wait until someone tells me’ (p 6). This suggests that maintaining the same room/layout throughout treatment would help increase predictability, thus supporting the client to focus on the content of the sessions rather than the environment. Clients not knowing what to expect can be a barrier to them engaging in treatment, linking it to the subtheme ‘Barriers to treatment’. Therefore, it is important to reduce as much uncertainty as possible.
Content that stood out
Participants left treatment feeling like they gained something from it and remembered aspects that affected their anxiety and low mood symptoms. For instance, Tish remembered the mindfulness techniques as being helpful: ‘I remember learning all about the different coping mechanisms like the sushi train and the wave thing’ (p 1). By contrast, others remembered and took on board the LICBT interventions. Barry, for example, completed the exposure and habituation technique one-to-one:
‘I have exposed myself around on the bus and also to a lot of other passengers … the sessions at the time improved more my independent like bus journeys … I feel very relieved … that my bus journey experience is like going back to normal’ (pp 1, 3 and 13).
For others, the specific autism content stood out more:
‘I really loved learning about all of the sensory section … especially like interoceptive the vestibular senses all of that. Going deeper on that and understanding not just what they are but how they affect me personally and my own sensory profile’ (Jack, p 8).
Overall, participants found the treatment helpful, although opinions on what made it helpful differed. The following subthemes will explore and interpret these varying opinions.
Linking Autism and Anxiety
Opinions differed on whether sessions were autism-informed, especially within the group sessions. Jack identified that the group sessions helped provide a greater understanding on the link between autism and anxiety: ‘it honed in on a focus around autism … I looked at the two in isolation before but hadn’t considered to that extent the influence that they have over each other’ (p 1). However, others felt the course was not specifically focused on autism at all: ‘It didn’t feel to me that it was specifically, catered for people who are neurodivergent’ (Barry, p 1). This difference in experience could be because participants attended different groups, thus experienced different facilitator approaches.
Opinions may have differed because participants may have different understandings of their autism diagnosis and how it affects them. For example, Tish demonstrates a high level of awareness of how their anxiety and autism interact:
‘I know personally that when I’m having a high anxiety day, my autism symptoms go through the roof and like sensory issues become like kind of supercharged, kind of get a bit more hypervigilant of everything and if I’m having like high autism day, kind of already aware of my toes say and then that kind of spikes up my anxiety as well because I’m like ohh I’m acting more autistic than normal and stuff like that in public. So, the two very closely link like if one’s high the other’s high. But if one becomes high because of like a meltdown or something, then it shoots the other right back up as well’ (p 15).
If clients already have a good understanding of their mental health symptoms and how their autism relates, they may not find the adapted LICBT as useful:
‘I did feel like they understood autism. I was kind of surprised that it wasn’t necessarily more autism directed, so like the anxiety was like kind of general anxiety and it did relate to back to autism in a couple of the sessions I was just surprised that it came up so little’ (Tish, p 14).
Tish’s comment highlights a desire for there to have been more autism-specific content within treatment sessions, although this may not have been possible within LICBT, which is short-term support.
Supporting clients to discuss or write down how the autism content applies to them could improve its integration: ‘taking the knowledge and applying it to myself and starting that journey in the course would have been really beneficial’ (Jack, p 8). Another recommendation was practitioners having an autistic frame of mind. Tish identified when working through the cognitive restructuring technique that it conflicted with their understanding of masking: ‘The whole mindreading situation like ohh these people think your weird then it would be like yeah that’s probably because you know you’re masking’ (p 15). Therefore, it is important for practitioners to consider whether CBT techniques conflict with characteristics of autism and get feedback from clients on whether the techniques sound applicable, and if adaptations are needed.
CBT is like Marmite
Some participants expressed a dislike for CBT which discouraged them from engaging in treatment: ‘If I’d known it was gonna be CBT it might have put me off but if it could have been described in a way which says it is tools of CBT as opposed to the process of CBT’ (Barry, p 2). Although people expressed a negative attitude towards CBT, many identified finding it helpful on completion, suggesting that people may hold negative perceptions of CBT. Thus, it is important to consider language used to explain LICBT as it could make a difference in them engaging. Jack points out, ‘I like CBT when it is incorporated into other things and it’s not full on CBT I guess’ (p 10). This indicates that some people may not have a clear understanding of what autism adapted LICBT is and how it differs from non-adapted treatment, high-intensity CBT or other third wave CBT. Thus, using language like ‘not full-on CBT’ or ‘CBT tools’, may be a more accessible way to explain LICBT.
Negative perceptions of CBT could be down to previous unsuccessful experiences. For example, Jack discussed his experience of previous CBT compared with the autism and anxiety course:
‘it wasn’t this is page one three eight this technique of CBT that we’re going to be practising today you’re gonna go away and do your homework for seven days and then you’re gonna feedback how that technique was and then move onto the next one. This was autism and anxiety is the focus’ (p 11).
Jack’s experience of CBT improved when it was within a group setting, but more so when it was adapted for autism. Some are more open to CBT than others. Thus it is important to consider the language being used to explain LICBT, clients’ previous experience of treatment, modality preference and adaptations, before choosing treatment.
Supporting Materials
This theme discusses how supporting materials either helped or hindered the treatment. Most people held the opinion that the booklets given within sessions were not helpful: ‘for me personally … those types of resources are superfluous’ (Jack, p 13). Many others did not even realise additional paper resources were provided, although Tish (quoted in Table 3) found the booklets helpful, did not complete them, but aided in remembering the content. The PowerPoint presentations on the other hand were found to be supportive as it provided ‘a springboard for good group discussions, you can’t have one without the other’ (Jack, p 9). Henry further illustrates how the PowerPoint supported peer interaction compared with the booklet: ‘I preferred the presentation format because that was much more engaging than the piece of paper as it helped discussions between the people presenting the presentation and the people who attended’ (p 14). This links to the subtheme ‘Human Interaction’ as materials used within sessions can be a factor in aiding discussion.
Further recommendations for materials included: layout being clear, use of simple language, free from grammatical errors and examples being relevant to autistic adults and providing a file for materials, either as an online system to store electronic files or folders for paper resources. Improving materials on CBT content was also suggested: ‘some links to like websites and stuff so if you did want to go back and do your own research just because that might be easier than hyperfixating on it for four hours’ (Tish, p 16). Providing additional reading may be an effective way to provide adequate support to those within treatment who already have a sound understanding of their symptoms, thus providing them with a breadth and depth of knowledge that is otherwise not available. Barry also highlighted: ‘Potentially testimonials from people who are autistic, who have actually responded well to CBT could be useful’ (p 10). This suggests that autistic clients may believe that CBT is not effective for them, and thus providing testimonials may increase confidence in the intervention. Hence, linking to the subtheme ‘CBT is like Marmite’, as it indicates that additional resources could aid in improving autistic adults’ experiences and perceptions of LICBT.
Barriers to Treatment
Participants experienced many barriers when trying to access support. A common barrier was feeling misunderstood or dismissed due to a lack of autism understanding from others in authority: ‘when I’ve like brought up feelings and stuff before to like teachers or other people in power it’s just been kind of dismissed … especially because of the autism’ (Tish, p 3). This advocates a need for all practitioners to have autism training, which neurodiversity champions within NHS-TTS could facilitate. A potential consequence of practitioners not understanding autism is misattribution of symptoms, causing autistic people to feel a burden when asking for treatment: ‘I don’t want to … like waste time because there’s plenty of other people that need help’ (John, p 3). Another potential barrier is clients lacking independence. For example, Tish highlights that her mother was unavailable to take her to sessions, thus she had to practise coming alone: ‘it’s like important for me to go in and do it by myself because she didn’t have many Wednesdays off’ (p 4). Thus, a flexible attendance policy is a reasonable adaptation for autistic clients who rely on caregivers.
Going into treatment often means clients are faced with lots of uncertainty, as identified in the subtheme ‘Reducing Uncertainty’; however, even when measures are put in place there is still a level of anxiety, which can act as barrier to seeking support: ‘Regardless of how much prep I did it was a new place with new people … there was always going to be some anxiety there’ (Tish, p 4). Tish additionally describes a situation of being singled out at school which left them avoidant of being in situations involving groups of strangers: ‘I join your group and they’d be like … sorry we’re full, so I have a kind of an aversion to group tasks’ (Tish, p 8). This suggests that for autistic clients, group treatment could be more difficult to engage with than one-to-one, due to an anxiety and avoidance of being around groups of strangers, because of previous negative experiences.
Environment is important: ‘it makes me cover my ears’
The sensory environment of both the waiting and treatment rooms are important to consider:
‘I remember it being … bit too hot, but um we opened the window and it soon cooled down and … the lighting was fairly good … I remember asking the blinds to be shut once because there was too much like light refraction off of the other windows and then there was um like there was hardly any smell … for me the sudden heat change and really strong smells can set off my Tourette’s’ (Tish, p 7)
Therefore, light, noise, smell, and temperature levels must be considered within the environment and be possible to adjust accordingly to individuals’ needs to reduce distraction and overstimulation. Other suggestions to improve the environment within the service was to acquire more comfortable chairs and to ensure that waiting rooms are not crowded, as this can increase noise levels and anxiety.
Discussion
This study investigated whether anxiety and depression ROMs differed in severity for autistic adults who completed either a group or one-to-one adapted LICBT. As hypothesised, there was a significant main effect of time, showing that anxiety and depression ROMs were lower on completion of both treatments. However, it is important to recognise limitations in terms of validity and the inability of our study design to determine causality (see ‘Limitations and recommendations’ section below).
Nonetheless, the qualitative findings provide information on which adaptations participants favoured; this feedback may help explain what factors influenced improvement in clinical outcomes. For instance, participants found it beneficial that the group was dedicated to autistic people, face-to-face and limited capacity. Similarly, incorporation of autism psychoeducation, practitioner profiles, and adapting the sensory environment, were also noted as helpful and already recommended within literature (National Autistic Society, 2021; National Institute for Health and Care Excellence, 2021; Petty et al., Reference Petty, Bergenheim, Mahoney and Chamberlain2021; Russell et al., Reference Russell, Jassi and Johnston2019; Stark et al., Reference Stark, Ali, Ayre, Schneider, Parveen, Marais, Holmes and Pender2021b).
Adaptations can result in deviation from standard practice; therefore, service leads may conduct cost-benefit analyses when considering adaptations. Staff admininstration time, for example, may increase when creating suitable materials, and treatment frequency and length may increase to cover additional information, which could impact waiting lists. Nonetheless, adapting for this patient group is a legal requirement of the NHS; thus, it is important to factor additional costs and resources into services’ budgeting and planning.
A significant interaction was found between treatment type and time, with one-to-one treatment showing a greater difference in anxiety and depression ROMs on completion. The qualitative data pointed out that practitioners sometimes facilitated the group poorly due to anxiety, causing difficulties with managing group dynamics and time. Brice et al. (Reference Brice, Rodgers, Ingham, Mason, Wilson, Freeston, Le Couteur and Parr2021) and Cooper et al. (Reference Cooper, Loades and Russell2018) suggested that practitioners can lack training and subsequent confidence when adapting for autistic clients. This could explain why some participants felt the group was rushed, and not autism-informed. In contrast, one-to-one treatment provides the opportunity for practitioners to tailor the information and pace delivered to individuals, indicating why the group’s effectiveness came second to one-to-one.
There was a stronger interaction for the GAD-7 than PHQ-9, suggesting larger changes in anxiety than depression scores. This may reflect autistic adults having a higher prevalence of co-occurring anxiety to depression (National Autistic Society, 2021; Stark et al., Reference Stark, Ali, Ayre, Schneider, Parveen, Marais, Holmes and Pender2021a, Reference Stark, Ali, Ayre, Schneider, Parveen, Marais, Holmes and Pender2021b). Thus, interventions for anxiety may be more common; for example, the group was focused on anxiety for autistic adults. Throughout the qualitative data, participants also mentioned aspects of treatment that hindered or supported their anxiety, yet there was no explicit mention of depression. For instance, the subtheme ‘Linking Autism and Anxiety’ highlighted that content which incorporated both conditions was particularly helpful, although ways to improve this were identified. This puts into context a potential reason for the greater reduction in GAD-7 scores.
Co-producing this research was important because it supports self-advocacy for improvement to healthcare by those who receive it (Stark et al., Reference Stark, Ali, Ayre, Schneider, Parveen, Marais, Holmes and Pender2021a). This study therefore recommends LICBT adaptations for autistic adults, by them. The key recommendations that were specified include providing therapist profiles, session agendas with the same structure, prior notice to agenda changes, the same room layout, orientation sessions with option for caregivers to join, follow-ups on completion of treatment, reduced group capacity, breaks, clear and relatable materials without errors, additional reading/testimonials on autism and CBT, flexible attendance policy, sensory-friendly environment and autism psychoeducation in sessions whilst making it applicable to individuals. These recommendations either support or supplement those already cited by the National Autistic Society (2021), National Institute for Health and Care Excellence (2021), and Stark et al. (Reference Stark, Ali, Ayre, Schneider, Parveen, Marais, Holmes and Pender2021b).
Limitations and recommendations
This study had large heterogeneity in the within- and between-subject factors, as identified within Figs 3 and 4, indicating a wide variance of scores. This may suggest why there was a non-significant difference between the treatment conditions. The wide range of views seen within the qualitative data could be explained because all participants experienced different treatments with varied practitioners, at different locations and times. This meant that participants were not explicitly reviewing the same treatments, which could help explain the variance in scores. This, however, led to a wide range of experiences being explored within the current study and gave context to which specific adaptations were helpful for different participants.
In addition, it is important to recognise that the validity of ROMs with autistic adults has been debated (Spain et al., Reference Spain, Sin, Chalder, Murphy and Happé2015). Future research could include measures that have been validated within autistic samples, such as the Anxiety Scale for Autistic-Adults (Rodgers et al., Reference Rodgers, Farquhar, Mason, Brice, Wigham, Ingham and Parr2020) and the Beck Depression Inventory-II (Williams et al., Reference Williams, Everaert and Gotham2021).
Furthermore, the study’s design prevented us from investigating causality. We are thus unable to conclude whether the treatments caused the changes over time in participants’ anxiety and depression scores. Future research would benefit from experimental designs, such as a full scale RCT as recommended by Russell et al. (Reference Russell, Gaunt, Cooper, Barton, Horwood, Kessler, Metcalfe, Ensum, Ingham, Parr, Rai and Wiles2020), as this enables investigating whether the psychological benefits are due to the adapted treatments.
The main effect of treatment type was not significant and had low statistical power, indicating that averages between treatments did not significantly differ. Participants were not perfectly randomised between treatment conditions due to interventions being allocated based on individual need and available resource. Therefore, there was a wide variance in baseline scores, which may have influenced no effect being found. The study had a limited sample size, was restricted to a single locality, and was not demographically diverse, with the majority being 18- to 34-year-old white British males, and is therefore limited in its generalisability. Thus, future research would benefit from recruiting participants across NHS-TTS nationally as well as international services, to increase statistical power, generalisability and applicability.
A further limitation is the concern of poor internal validity as the researcher was known to participants, which may have caused them to respond to interview questions untruthfully. This effect was mitigated by providing transparency of the researcher’s involvement from initial provision of information. Participants were also asked to provide honest feedback with no concern of offence being taken, as the aim of the study was to improve the treatments being evaluated. Conversely, the participants knowing the researcher, and trusting the organisations involved, may have increased interest in participation and intersubjectivity. Confirmation bias is an additional concern, as the first author (H.T.) was closely involved in the interventions that have been evaluated and conducted the analysis (Klayman, Reference Klayman, Busemeyer, Hastie and Medin1995). Dowling (Reference Dowling and Hay2005) states that qualitative research typically involves interpersonal relationships, and therefore researchers need to be critically reflexive. Hence, as there were no external raters the researcher (H.T.) pursued a balanced perspective when analysing data, in addition to the input from the other two researchers. Nevertheless, Sargeant (Reference Sargeant2012) identified an increased potential for coercion when researchers and participants are explicitly known to one another. Therefore, to increase objectivity, a future study should use external researchers to investigate LICBT interventions being delivered within the NHS, or other health services, as it would address concerns of partiality.
Implications
A key implication of this study is that it found adapted LICBT in the format of both group and one-to-one was associated with lower anxiety and depression ROMs for autistic adults. This study adds to limited research in the field as a pilot RCT was the only study found to explore the effectiveness of adapted LICBT for autistic clients (Russell et al., Reference Russell, Gaunt, Cooper, Barton, Horwood, Kessler, Metcalfe, Ensum, Ingham, Parr, Rai and Wiles2020). Such results are therefore essential in the reinforcement of further research, which is significant because empirical research informs evidence-based practice within NHS-TTS (National Collaborating Centre for Mental Health, 2023). For instance, the NHS (2019) set out a focus for long-term health conditions within NHS-TTS following evidence that physical health conditions can improve on treatment of mental health. This increased resources such as training provisions across services. Thus, this study could have implications for the implementation of adapted LICBT interventions for autistic adults across NHS-TTS nationally.
Another implication of this study was that the qualitative results provided a perspective into how to effectively adapt LICBT. This has the potential to inspire other practitioners and NHS-TTS to adapt their practice based on suggestions provided by autistic clients. These recommendations also have implications for improving the evaluated interventions, as changes such as adding follow-ups on completion of treatment will be made to the current provisions. However, it is important to note that some recommendations may be unfeasible due to resource limitations, conflicts with commissioning requirements, or the IAPT manual, which sets policy and procedure on treatment and service delivery (National Collaborating Centre for Mental Health, 2023).
Conclusion
Despite limitations, the study supported that adapted LICBT was associated with lower anxiety and depression symptoms for autistic adults as observed by ROMs. Additionally, the study provided recommendations from autistic adults on how to adapt treatment effectively. Many adaptations were highlighted within literature, although further details on how to implement them were added (National Autistic Society, 2021; National Institute for Health and Care Excellence, 2021; Stark et al., Reference Stark, Ali, Ayre, Schneider, Parveen, Marais, Holmes and Pender2021b). The study found greater changes in the anxiety measure and for one-to-one treatment. Future studies should take a experimental approach to determine causality in the reduction of ROMs. To conclude, improvements to the provisions being delivered within Plymouth’s NHS-TTS and autism services can be implemented from this study, but there is also potential for it to improve the quality and accessibility of LICBT for autistic adults within NHS-TTS nationally and in international health services.
Key practice points
-
(1) Low-intensity CBT can effectively be adapted and used to help with common mental health difficulties like anxiety and depression for autistic people.
-
(2) Clinicians should consider autistic patient feedback to identify barriers they experience accessing effective treatment to aid change.
-
(3) Services and practitioners to consider implementing adapted provisions for autistic adults, for instance through increasing autism awareness, appointing neurodiversity/autism champions, and facilitating co-production with experts by experience.
-
(4) Adaptations to the treatment preparation, content, structure, interaction, and environment can be made.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1754470X24000230
Data availability statement
The data that support the findings of this study are available on request from the corresponding author, H.T. The data are not publicly available to protect the privacy of research participants, and as the participants have not agreed to have their data publicly shared.
Acknowledgements
We thank Plymouth Autism Spectrum Disorder and Plymouth NHS Talking Therapies Service for sharing data for analysis and publication, and for clinical support.
Author contributions
Hope Trimmer: Conceptualization (equal), Data curation (lead), Formal analysis (lead), Investigation (lead), Methodology (lead), Resources (lead), Visualization (lead), Writing – original draft (lead), Writing – review & editing (supporting); Sonja Heintz: Conceptualization (supporting), Data curation (supporting), Formal analysis (supporting), Investigation (supporting), Methodology (supporting), Resources (supporting), Supervision (lead), Validation (lead), Visualization (supporting), Writing – review & editing (lead); Sarah Williams: Conceptualization (equal), Methodology (supporting), Project administration (supporting), Resources (supporting), Supervision (lead), Visualization (supporting).
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interests
H.T. is employed at Plymouth NHS Talking Therapies Service and Plymouth Autism Spectrum Disorder (Livewell Southwest). S.W. is employed at Plymouth Autism Spectrum Disorder (Livewell Southwest).
Ethical standards
Due to the nature of the study and the vulnerability of this sample, the researcher closely followed the British Psychological Society (BPS) code of Human Research Ethics (Oates et al., Reference Oates, Carpenter, Fisher, Goodson, Hannah, Kwiatkowski, Prutton, Reeves and Wainwright2021) and the code of conduct by the British Association for Behavioural and Cognitive Psychotherapies (BABCP). It highlights the importance of respecting participant autonomy, privacy, confidentiality, and ensuring capacity for informed consent and withdrawal, which is in line with NHS guidance for ethical research (Research Ethics Service, n.d.). The interviews were conducted by the first author (H.T.), who helped develop and deliver the treatments that are being evaluated, and was known by the participants. Nonetheless, this study did not bring harm to any participants or influenced their treatment/care with the services they were accessing. Ethical implications were considered and mitigated by providing participants with an information sheet with the researcher’s picture and details and asked to sign a consent form prior to interview. Before proceeding with audio recording, the researcher confirmed participants’ understanding, and signed to approve capacity for informed consent. On completion, a debrief form was discussed and provided to participants, reminding them of their right to withdraw, data protection and signposted them to further support and supervisor contact details. If answers in the interview raised concerns of participant wellbeing or safety, the clinical team lead at PASS was notified as stated in the information sheet. All data were anonymised and stored securely to protect participants’ confidentiality. The Faculty of Health of the University of Plymouth and Livewell Southwest granted ethical approval (number 438).










Comments
No Comments have been published for this article.