Racially and ethnically marginalized people experience morally unacceptable serious illness care inequities, including poorer pain-related outcomes, less hospice care, lower rates of advance care planning, greater financial burden, and higher mortality rates across several conditions (Bailey et al. Reference Bailey, Feldman and Bassett2021; Meghani et al. Reference Meghani, Byun and Gallagher2012; Suntai et al. Reference Suntai, Noh and Jeong2022). The existential questions that serious illness may raise related to suffering, legacy, and meaning are difficult to disentangle from the toxic stress of racism. Dismantling racist structures requires empathic, tailored communication to engage and support people of color with care that is physically, psychologically, and culturally safe and goal-concordant (Bailey et al. Reference Bailey, Feldman and Bassett2021; Sanders et al. Reference Sanders, Curtis and Tulsky2018, Reference Sanders, Durieux and Cannady2022a). Although targeted palliative and end-of-life interventions for racially and ethnically marginalized people may improve some related outcomes, their overall effectiveness is unclear (Jones et al. Reference Jones, Luth and Lin2021). Serious illness communication (SIC) that acknowledges and validates racism’s historical and current context, and recognizes and responds to the uniqueness of intersectional identities, is essential to advancing socially responsible care and research.
SIC and health equity
Serious illnesses are those conditions that either (1) carry high mortality risk, negatively impact the quality of life and function, and/or carry significant symptom, treatment, or caregiver stress burdens or (2) are not advanced but carry a high degree of clinical uncertainty (Kelley Reference Kelley2014). SIC involves a clinician’s use of relatable language to create and foster interpersonal safety; elicit patients’ values, goals, and concerns; iteratively explore patient and surrogate decision-making roles; and recommend individualized care options throughout the course of serious illness and at the end of life, among other person- and family-centered steps (Jacobsen et al. Reference Jacobsen, Bernacki and Paladino2022). Patients’ experiences with racism may strongly influence the ability of SIC to achieve health equity in the serious illness context. When considering Jones’ definition of health equity – “assurance of the conditions for optimal health for all people … valuing all individuals and populations equally, recognizing and rectifying historical injustices, and providing resources according to need” – SIC becomes an interpersonal tool to address the root of health injustices and to tackle the “social determinants of equity” (Jones Reference Jones2014, S74).
Why race-conscious SIC?
Health care is commonly influenced by hierarchical power imbalances (e.g., patient–physician) and racialized differences (e.g., Black–white). Evidence shows people of color frequently experience biased care provision and discriminatory behaviors during clinical encounters and while accessing health services more broadly (Akinade et al. Reference Akinade, Kheyfets and Piverger2023; Ben et al. Reference Ben, Cormack and Harris2017; Lorié et al. Reference Lorié, Reinero and Phillips2017). Interactions viewed as unsafe or racist by the care recipient may understandably curtail transparency and prohibit honest communication. Patients’ fears and worries about serious illness may only not be related to a given illness but also racially motivated mistreatment as they lose agency or functional independence. In addition, community engagement in decision-making may vary across cultures in ways the health system does not accommodate. For instance, some Black communities value church ministries as a source of support at the end of life (Sloan et al. Reference Sloan, Gray and Harris2021). Clinicians who do not recognize the role of or actively partner with these communities risk perpetuating white supremacist culture and racist norms that may isolate and harm patients (Okun Reference Okun2006).
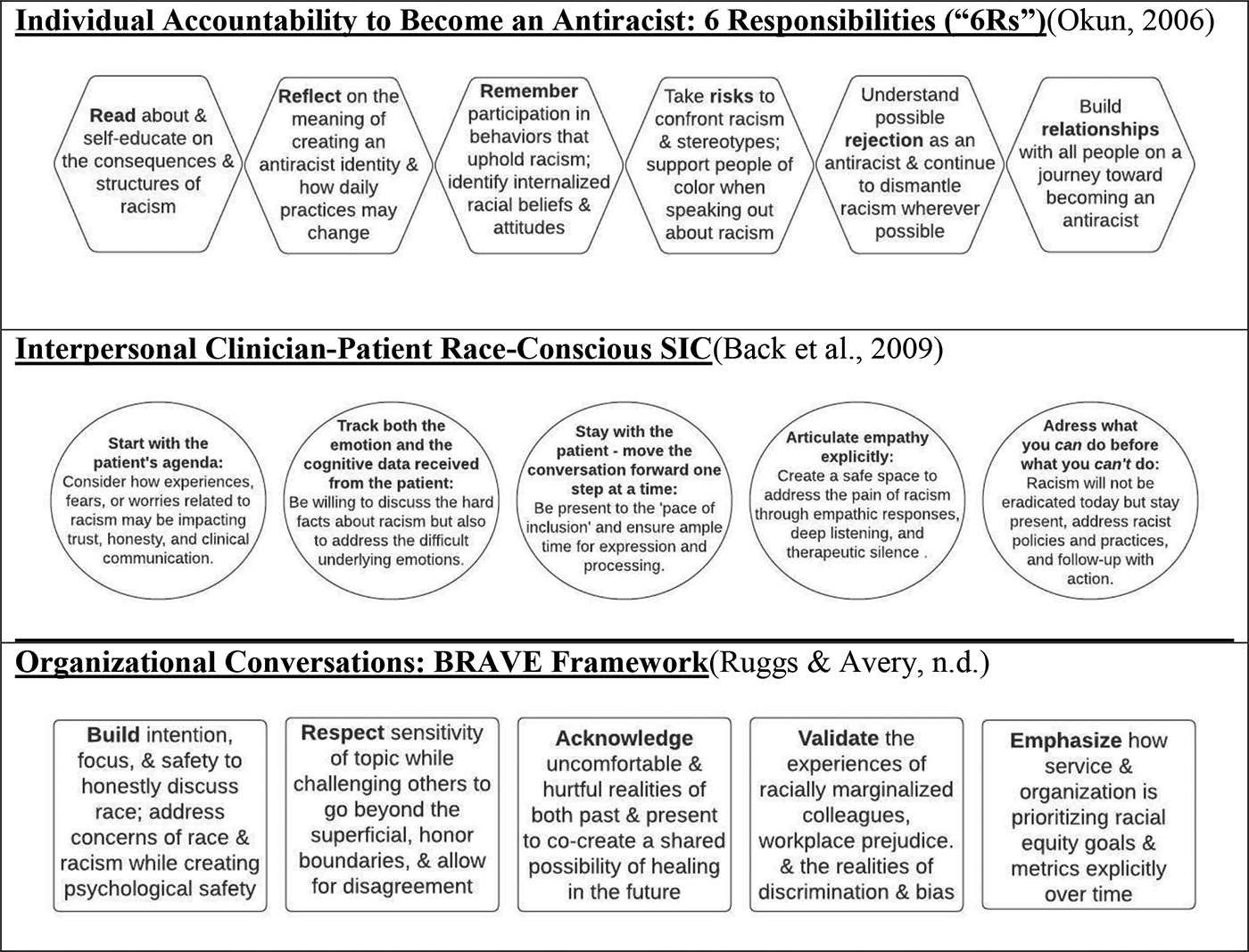
Fig. 1. Inclusive practices to support race-conscious serious illness communication at individual, interpersonal, and organizational levels (adapted Back et al. Reference Back, Arnold and Tulsky2009; Okun Reference Okun2006; Ruggs and Avery Reference Ruggs and Avery2020).
A race-conscious approach to SIC requires acknowledgment of the racial dynamics during the clinical encounter (Needham et al. Reference Needham, Ali and Allgood2022; Stangl et al. Reference Stangl, Earnshaw and Logie2019). Many current SIC tools do not explicitly create space for a patient’s open and honest lived experiences of racism (Back et al. Reference Back, Tulsky and Arnold2020; Bernacki et al. Reference Bernacki, Hutchings and Vick2015; Bernacki and Block Reference Bernacki and Block2014; Childers et al. Reference Childers, Back and Tulsky2017; Chung et al. Reference Chung, Oczkowski and Hanvey2016). These shortcomings may lead to avoidance, denial, and even reactiveness or aggression from the clinician who feels threatened by the narrative or does not accept its validity. Such a situation requires the clinician to (1) recognize their own social location when communicating with the patient, (2) acknowledge that myriad levels of racism exist and impact decision-making, and (3) address how biased policies disrupt cultural safety, promote distress, and negatively affect the therapeutic alliance (Bailey et al. Reference Bailey, Feldman and Bassett2021). SIC ideally strengthens trust and supports person-centered decision-making (Jacobsen et al. Reference Jacobsen, Bernacki and Paladino2022). But unless SIC is adapted to authentically welcome the painful truths of racism, clinicians and researchers may inadvertently violate principles of nonmaleficence and justice while disenfranchising individuals with racialized trauma. They may also unconsciously demonstrate outward biased behaviors or language despite intent (Okun Reference Okun2006). Race-conscious SIC can assist to ethically engage people of color using narrative approaches (Daryazadeh Reference Daryazadeh2019) (e.g., through moral reflection, witnessing patient story, and responding empathically) and gain a life course perspective that more accurately gauges the multilevel social factors that have informed a patient’s lived experience with racism (Green et al. Reference Green, Doherty and Bugbee2022). Inclusive approaches must be iteratively integrated throughout serious illness care in myriad ways, including organizational conversations to safely address racism among colleagues, individual clinician–researcher commitments to becoming an antiracist, and demonstrating race-conscious clinician–patient SIC (see Figure 1) (Back et al. Reference Back, Arnold and Tulsky2009; Okun Reference Okun2006; Ruggs and Avery Reference Ruggs and Avery2020).
Consider Tanya – a Black transgender woman experiencing houselessness. Tanya is navigating multiple stressors related to interlocking, minoritized identities and confronts barriers to medication and service access, as well as safe opioid stewardship options in the setting of severe cancer pain (Crenshaw Reference Crenshaw2017). Not only would the highest quality, holistic care call on the clinician to integrate structural and social factors into planning but also remain conscious and sensitive to Tanya’s social realities and serious illness needs. Current SIC research and tools are severely inadequate to account for or safely address Tanya’s values and goals, particularly in the setting of being unhoused. Both a framework and an approach are needed to ensure Tanya’s dignity and personhood are prioritized in the face of systematic marginalization.
Public Health Critical Race Praxis
The Public Health Critical Race Praxis (PHCRP) is a framework based on Critical Race Theory that may broaden scientific inquiry in serious illness while improving race- and racism-related outcomes and providing key implications for SIC (Brown et al. Reference Brown, Curtis and Doll2022; Ford and Airhihenbuwa Reference Ford and Airhihenbuwa2010a, Reference Ford and Airhihenbuwa2010b). The PHCRP – guided by 4 focus areas and accompanying principles (Table 1) – posits that racism is contextualized in each society and among each race (Ford and Airhihenbuwa Reference Ford and Airhihenbuwa2010a, Reference Ford and Airhihenbuwa2010b). The PHCRP can aid the development and adaptation of SIC tools to address racism and poor communication in both research and clinical practice (Table 2) (Brown et al. Reference Brown, Curtis and Doll2022). The principle of race consciousness extends throughout all focus areas, giving explicit attention to racial dynamics in one’s social and personal world, including in health-care spaces.
Table 1. Public Health Critical Race Praxis principles, focus areas, and definitions
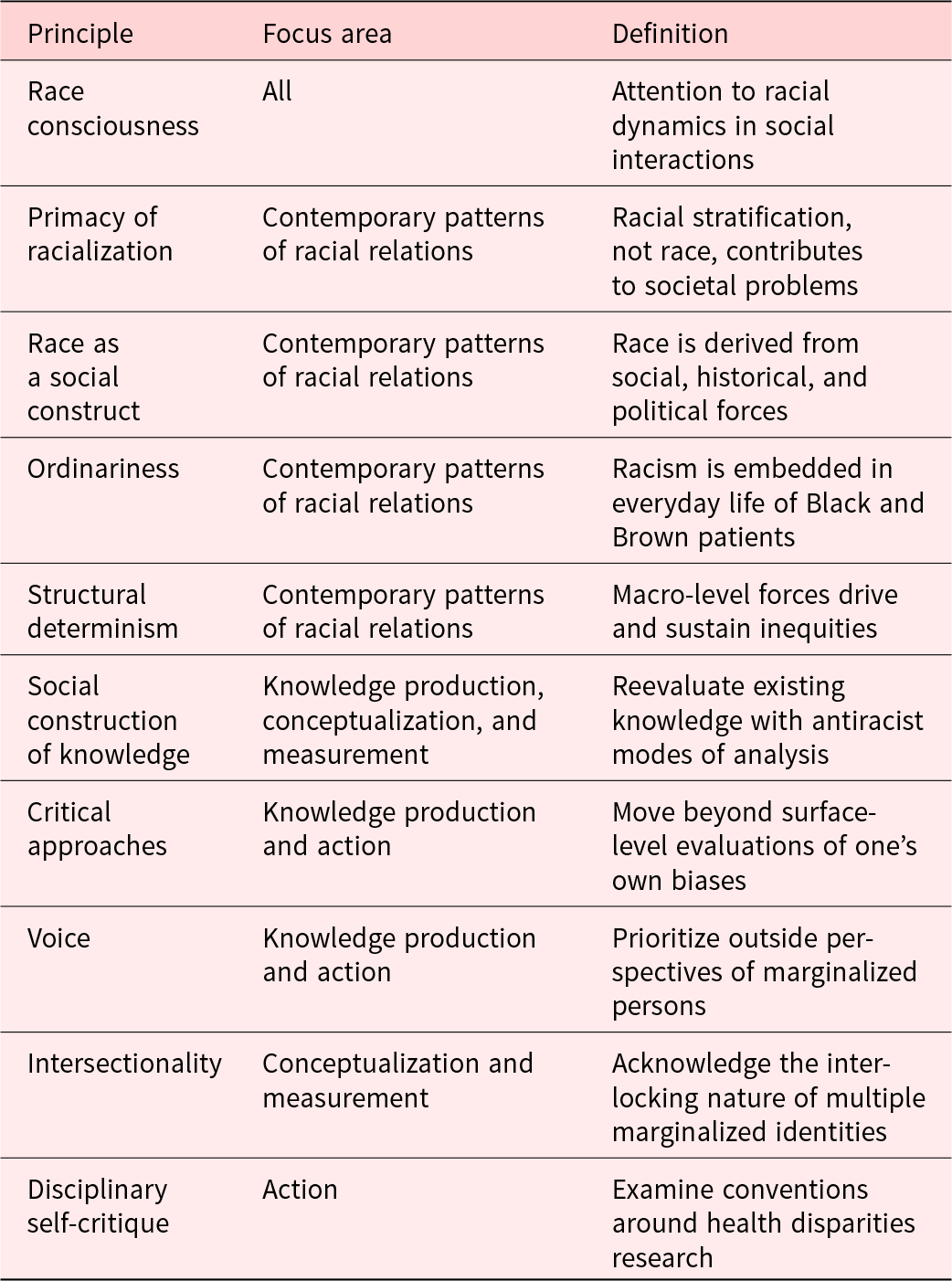
Table 2. Using the Public Health Critical Race Praxis to shape serious illness communication tools for racially marginalized patients


Fig. 2. Empathic opportunities, definitions, and examples related to serious illness and racism (adapted Pehrson et al. Reference Pehrson, Banerjee and Manna2016).
PHRCP Focus 1: contemporary patterns of racial relations
Racially marginalized patients are affected by racism in everyday life. Well-meaning clinicians engage in personal interactions with racially traumatized individuals in a health-care structure that perpetuates inequities (Bailey et al. Reference Bailey, Feldman and Bassett2021; Needham et al. Reference Needham, Ali and Allgood2022; Stangl et al. Reference Stangl, Earnshaw and Logie2019). It is important for researchers and clinicians to take into consideration current events that disproportionately and negatively impact Black and Brown people (e.g., racialized violence and economic strain). Considering these factors allows researchers to account for how these additional stressors – in conjunction with serious illness – shape how patients perceive clinicians and systems, make decisions, and prioritize goals of care.
PHRCP Focus 2: knowledge production
How have disciplinary conventions around research and a lack of race consciousness shaped SIC knowledge? Although SIC literature attempts to better understand communication disparities, there must be greater transparency on how racialization has biased research, reinforced negative beliefs and stereotypes about racially marginalized groups, and informed the development of SIC tools. Improving SIC communication for racially marginalized patients requires researchers to account for researcher positionality in white-predominant spaces, including research institutions and health-care systems. “Centering the margins” requires prioritizing patient and researcher perspectives that have typically been excluded from research processes, and including racially marginalized researchers beyond ornamental engagement (Rhodes et al. Reference Rhodes, Barrett and Ejem2022; Sanders et al. Reference Sanders, Gray and Sihlongonyane2022b).
PHRCP Focus 3: conceptualization and measurement
Although SIC research and tools aim to improve communication, a patient’s racialized experience is often unassessed or treated as simply another variable in statistical modeling (Needham et al. Reference Needham, Ali and Allgood2022; Stangl et al. Reference Stangl, Earnshaw and Logie2019). A race-conscious approach to SIC tool development and improvement includes an examination of race-related constructs, their hypothesized relationships to outcomes, and whether such measures can capture the sequelae of racism. Importantly, patients often have more than one marginalized identity and it will be important that SIC can create space for patients and providers to acknowledge how intersectionality shapes these narratives (Crenshaw Reference Crenshaw2017).
The need for community-based participatory research (CBPR) approaches in serious illness cannot be overstated. CBPR actively engages communities as equal partners and serves as a social justice mechanism to ensure that research endeavors are community-guided (Elk et al. Reference Elk, Emanuel and Hauser2020). Importantly, CBPR strives to ensure that scientific findings and implications will be contextually relevant to the study population.
PHRCP Focus 4: action
Existing health disparities research fails to identify a tangible plan for eliminating racist practices or forging sustainable commitments to racially minoritized communities. It is not enough to simply document that Black–white SIC disparities exist – work must be done to eradicate them starting with how we engage during the communication that connects us. Of significant importance is the need for clinicians to take accountability for their personal practices that perpetuate inequities and their conscious and unconscious justification of proliferating white supremacist ideas in health care, academia, and interpersonal engagement (Okun Reference Okun2006). Such actions call for teaching and implementing antiracist SIC frameworks in research to ultimately shift knowledge, improve clinical outcomes, and enhance the quality of clinician–patient relationships informed by race-conscious SIC (Brown et al. Reference Brown, Curtis and Doll2022; Rosa et al. Reference Rosa, Gray and Chambers2022; Sanders et al. Reference Sanders, Gray and Sihlongonyane2022b).
Practical changes in SIC require action. Take, for example, an evidence-based approach to empathic communication (Pehrson et al. Reference Pehrson, Banerjee and Manna2016). There are clear opportunities to integrate race-conscious SIC into the encounters among patients, families, and clinicians in ways that promote relationship-building. Table 3 provides strategies, skills, and potential talking point examples of race-conscious SIC. We acknowledge that these are incredibly high-stakes questions for many patients and that the clinician may not receive an honest response or may be rejected altogether if they are not perceived as safe or genuine. Additionally, clinician–patient race discordance may be a barrier to transparency in some cases. Clinicians must take advantage of empathic opportunities to deepen trust with patients and families, even while risking rejection (Figure 2). The very premise of goal-concordant care requires a restructuring of how clinicians understand the communication process, the patient experience, and shared decision-making. Thus, one solution is to more inclusively engage surrogates and community supports – as well as considerations of racism and exclusionary policies and practices – to ensure care is aligned with patient goals and the grieving process for caregivers is intentionally supported (Johnson Reference Johnson2022; Sanders et al. Reference Sanders, Curtis and Tulsky2018).
Table 3. Race-conscious communication: strategies, skills, and examples of talking points (adapted Pehrson et al. Reference Pehrson, Banerjee and Manna2016)

Conclusion
As clinicians and researchers partner with marginalized communities to dismantle barriers to health equity, it is imperative that how we listen and respond to patients, their families, and their communities reflects a commitment to whole-system awareness. Developing race-conscious SIC competencies may allow for hard truths to be safely spoken so that we may more effectively prevent avoidable suffering for people like Tanya, for all Black and Brown persons with serious illness, and for the families and communities that support them.
Acknowledgments
The authors thank Tamryn Gray, PhD, RN, and Khaliah Johnson, MD, for their expert review and insights during the writing of this manuscript.
Conflicts of interest
These authors have no conflicts of interest to disclose. W.E.R. has completed disclosure and conflict of interest statements on behalf of J.R.C.








