Introduction
“Advance care planning (ACP) is a process that explores personal values, life goals, and preferences of individuals about their future medical care” (Diegelmann et al. Reference Diegelmann, Bidmon and Terlutter2022; Sudore et al. Reference Sudore, Lum and You2017). It might have a role in reducing costs associated with unhelpful treatment at end of life (Kolarik et al. Reference Kolarik, Arnold and Fischer2002). Most patients with end-stage kidney disease (ESKD) and their families in low and low-middle income countries seldom have discussions with their families and health care providers regarding their preferences on admission to intensive care, referral to renal supportive care services, discontinuing dialysis, resuscitation, and preferred place for end-of-life care (O’Halloran et al. Reference O’Halloran, Noble and Norwood2018). In patients with ESKD, ACP might be beneficial during transition points of illness trajectory like initiating, withholding, or stopping dialysis, and may shift focus to psychological and spiritual aspects of care (Davison and Torgunrud Reference Davison and Torgunrud2007; Holley Reference Holley2012). Family can be an integral part of ACP discussions as patients often rely on their families for health decision-making (Davison et al. Reference Davison, Levin and Moss2015; Davison and Torgunrud Reference Davison and Torgunrud2007). The essential aspects of ACP include information provision by the health care provider in a language and manner understood by the patient; appropriate and honest information related to diagnosis and prognosis and anticipated outcome of treatment and its impact on quality of life (Davison Reference Davison2006).
In many countries, ACP and advance medical directive are a legally valid living will (Rietjens et al. Reference Rietjens, Sudore and Connolly2017). ACP documents must be part of patients’ medical records and should be accessible and activated when required by treating team, especially when a person is seriously ill and cannot communicate choices. It can be modified or rejected based on the patient’s diagnosis, change in health status, purpose of hospitalization, or decision (Conroy et al. Reference Conroy, Fade and Fraser2009; Rietjens et al. Reference Rietjens, Sudore and Connolly2017).
The Renal Physician’s Association and the American Society of Nephrology in their guideline have recommended step wise approach in shared decision-making and ACP in the ESKD population (Galla Reference Galla2000). It focuses on patient preferences, future illness course, and enables decision-making regarding appropriateness of continuation of dialysis therapy alongside symptom control measures (Davison and Torgunrud Reference Davison and Torgunrud2007).There is evidence to support ACP use in routine care of ESKD patients. However, they are from high-income countries (Combs Reference Combs2016; Deodhar et al. Reference Deodhar, Prasad Nagaraju and Kirpalani2021; Song et al. Reference Song, Ward and Fine2015). ACP has become a globally recognized standard of care and clinicians implement it in various forms (Mullick et al. Reference Mullick, Martin and Sallnow2013). However, their acceptability in developing countries like Indian setting is not known (Deodhar et al. Reference Deodhar, Prasad Nagaraju and Kirpalani2021). It might be due to a lack of awareness among the patient, families, and the nephrology team (Goff et al. Reference Goff, Unruh and Klingensmith2019). Before integrating ACP into routine clinical practice, information must be provided to the ESKD patients, their families, and the nephrology team to better awareness and acceptability (O’Halloran et al. Reference O’Halloran, Noble and Norwood2018). The findings of a systematically constructed review showed that training of health care professionals must include addressing concerns, improving communication skills, appropriate clarification of processes, thorough documentation, individualized and culturally appropriate approach, and involving surrogates in decision-making. These strategies might lead to more effective implementation of ACP in the clinical setting (O’Halloran et al. Reference O’Halloran, Noble and Norwood2018).
A scoping review of literature showed that ACP questionnaire for ESKD patients and their family caregivers in an Indian setting was unavailable. The use of a validated culturally context-specific scale might be beneficial for exploring the awareness and acceptance of ACP in clinical practice. The aim of this study was to develop and validate a bilingual questionnaire to evaluate awareness and knowledge of ACP among ESKD patients, caregivers, and health care providers.
Methods
Study setting
This study was conducted between August 2021 and July 2022 in the department of nephrology in a tertiary academic hospital in South India. Ethical approval was obtained from the institutional ethics committee (IEC: 214/2021).
Development of the ACP questionnaire (see Supplementary material)
The ACP questionnaire was developed from the findings of scoping literature search with concerning awareness and preference regarding ACP (Deodhar et al. Reference Deodhar, Prasad Nagaraju and Kirpalani2021; Ghoshal et al. Reference Ghoshal, Salins and Damani2019; Lai et al. Reference Lai, Mohd Mudri and Chinna2016; Ng et al. Reference Ng, Kuah and Loo2017). The initial questionnaire developed in English was translated into Kannada using forward–backward method. The questionnaire had three domains that focused on illness, treatment preferences, ACP awareness, and its acceptability. The questionnaire consisted of 50 questions, 16 questions each for patients with ESKD and their family caregivers and 18 questions for the nephrology team. An expert panel consisting of nephrologists, palliative medicine physicians, ESKD patients, and their family caregivers participated in the content validity of the questionnaire using the Delphi process. A facilitator reviewed the answers and suggestions made by the expert panel. After two rounds of questions, the group consensus was reached that these questions satisfactorily covered various aspects pertaining to ACP process.
Patient questions
The patient questions explored knowledge about illness and decision-making preferences. The first part of patient questions sought patient preferences on knowing disease progression and its severity, treatment options and their side effects, future illness-related complications, and its management and expected length of survival. The second part of patient questions explored patient’s decisions regarding future health care and documenting it as an advance care plan.
Family caregiver questions
The caregiver questions were same as patient questions. However, we surveyed the family caregivers’ views on patient knowing about the disease process and ACP decision-making.
Nephrology team questions
The nephrology team questions were designed to know the team members’ knowledge of ESKD patient’s goals of care, initiating and facilitating ACP discussions, and identifying barriers to ACP and its documentation. The nephrology team members included nephrologist, nurses, and technical staff involved in renal replacement therapy.
Content validity
Content validation was done by a team of five nephrologists, five palliative care physicians, three ESKD patients, and two caregivers using Delphi method. Individual experts were asked for a level of agreement and relevance. Quantitatively experts’ suggestions were measured using Content Validation Ratio formula “{CVR = (Ne − N/2)/(N/2)}.” Each item of the questionnaire scored from 0 to 2, stating “Not relevant,” “Somewhat relevant”, and “Relevant.” CVR was higher than 0.49 for items of instrument indicating acceptable agreement (Ghoshal et al. Reference Ghoshal, Salins and Damani2019; Ng et al. Reference Ng, Kuah and Loo2017; Nunnaly Reference Nunnaly1978). Based on their suggestion, some questions were reframed and finalized in coordination with experts.
Most of our ESKD patients and caregivers had difficulty understanding English, as their preferred language was Kannada; hence, the English version of the questionnaire was translated by two independent translators fluent in English and Kannada. Third independent person reconciled two translated versions. The final Kannada version was back-translated into English and compared with the original English version. The Kannada version of patient and caregiver questionnaire was pilot tested for five patients and five family caregivers to assess the feasibility of its use.
Participants
In our study, three groups included patients, caregivers, and nephrology team.
Participant eligibility criteria
Patients
Adults (18 years and above) with ESKD and consenting to participate in the study.
Family caregivers
Adult family caregivers (18 years and above) who had cared for a patient with ESKD for at least 6 months and consenting to participate in the study.
Nephrology team
Renal physicians and nurses, technical staff involved in renal replacement therapy working with ESKD patients for at least 12 months.
Sample size
30 ESKD patients, 30 family caregivers, and 10 nephrology team members were selected using convenience sampling.
Procedure
Eligible participants were recruited after obtaining informed consent. The content validated ACP questionnaire was administered to the participants in person. The retest was carried out after 1 week.
Statistical methods
Descriptive analysis was used for demographic variables. The intraclass correlation coefficient (ICC) and Cronbach’s alpha were used to determine the test–retest reliability and internal consistency respectively. The Statistical Package for the Social Sciences (SPSS version 15) was used for analysis.
Reliability
The Cronbach’s α was used to evaluate for internal consistency of each item and domain in the ACP questionnaire and a value ranged from 0.70 to 0.90 suggested satisfactory internal consistency (Abd Elhafeez et al. Reference Abd Elhafeez, Sallam and Gad2012; Hilton and Skrutkowski Reference Hilton and Skrutkowski2002; Nunnaly Reference Nunnaly1978). The test–retest reliability was evaluated based on the ICC value.
Results
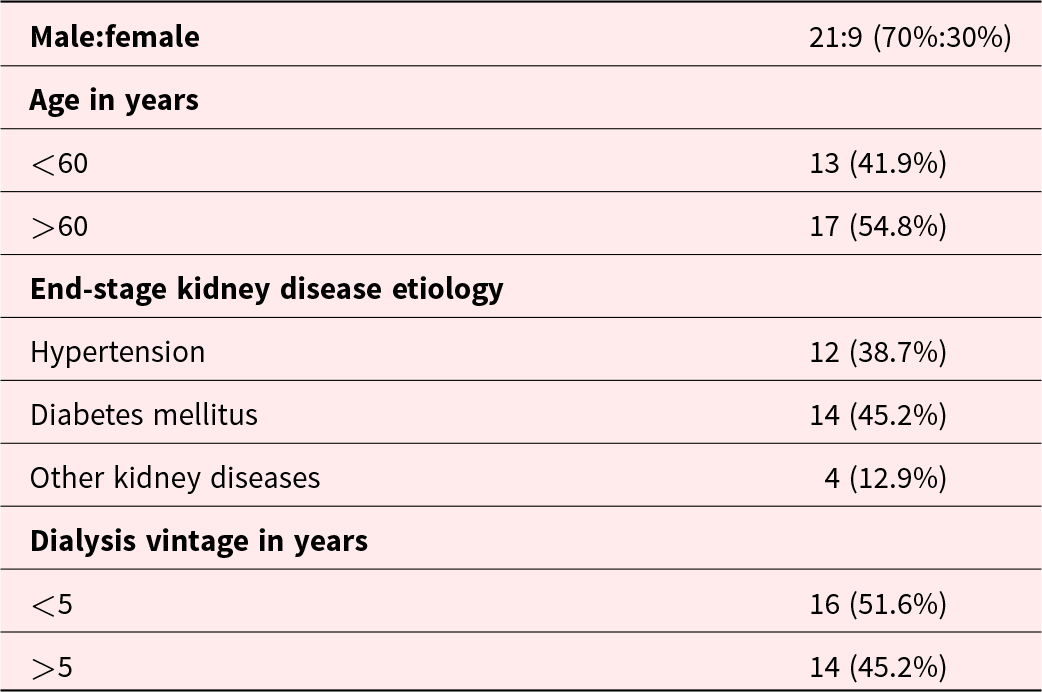
The final version of the ACP questionnaire had three domains with total 50 items. The demographic data of ESKD patients are shown in Table 1. The ESKD patients’ mean age was 56.50 ± 10.23 years and dialysis vintage were 5.71 ± 3.92 years.
Table 1. Demographic details of ESKD patients
Patient questions
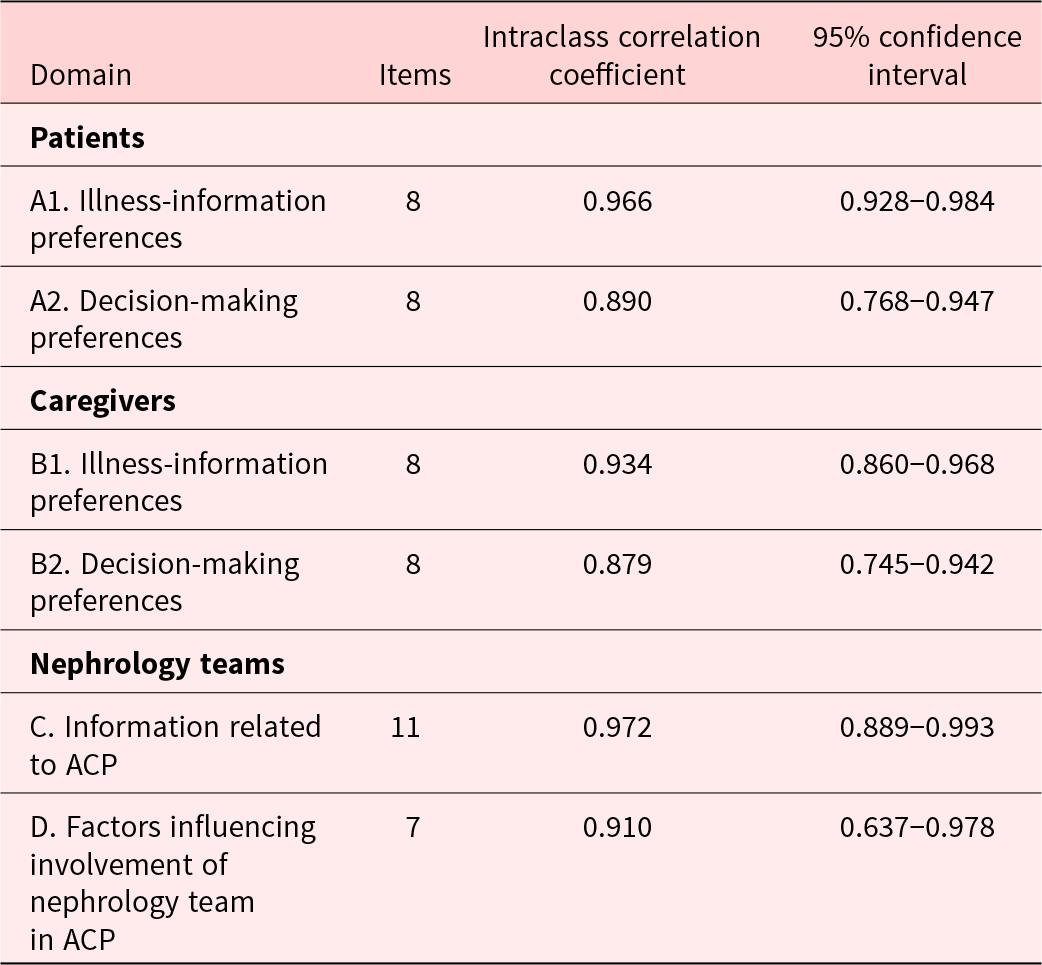
ESKD patient’s questions explored patient views on illness-information preferences and decision-making preferences. The initial section on illness-information preferences consisted of eight questions concerning disease-related information and knowledge preferences. The content validity ratio of these questions ranged from 0.6 to 1, and reliability as assessed by Cronbach’s α was 0.954 and ICC was 0.966 (95% CI 0.928–0.984). The latter section on decision-making preferences consisted of eight questions concerning future goals of care and ACP preferences. The content validity ratio of these questions was 1, reliability as assessed by Cronbach’s α was 0.79, and ICC was 0.890 (95% CI 0.768–0.947).
Family caregiver questions
The family caregiver questions explored family views on illness-information preferences and decision-making preferences. The initial section concerning illness-information preferences, consisted of 8 questions on family caregiver preferences on patient knowing disease-related information. The content validity ratio of these questions ranged from 0.6 to 1, and reliability as assessed by Cronbach’s α was 0.896 and ICC was 0.934 (95% CI 0.860–0.968). The latter section of the caregiver questionnaire concerning decision-making preferences consisted of eight questions on family caregiver views on their patients participating in future goals of care discussion and ACP preferences. The content validity ratio of these questions was 1, and reliability assessed by Cronbach’s α was 0.69, and ICC was 0.879 (95% CI 0.745–0.942).
Nephrology team questions
The nephrology team questions explored information related to ACP and factors influencing their involvement in the ACP process. The initial section consisted of 11 questions assessing knowledge of ACP. The content validity ratio of these questions was 1, Cronbach’s α evaluated reliability was 0.714, and ICC was 0.972 (95% CI 0.889–0.993). The latter section consisted of seven questions concerning facilitators and barriers for ACP discussion. The content validity ratio of these questions was 1, reliability assessed by Cronbach’s α was 0.834, and ICC was 0.910 (95% CI 0.637–0.978).
Reliability analysis for this questionnaire was performed for each item. Cronbach’s α of each domain ranged from 0.693 to 0.952, and details of each domain are shown in Table 2. The test–retest reliability ICC values ranged from 0.879 to 0.972 (Table 3).
Table 2. The mean ± SD and Cronbach’s α values of the ACP questionnaire among ESKD patients, care givers (family), and nephrology team
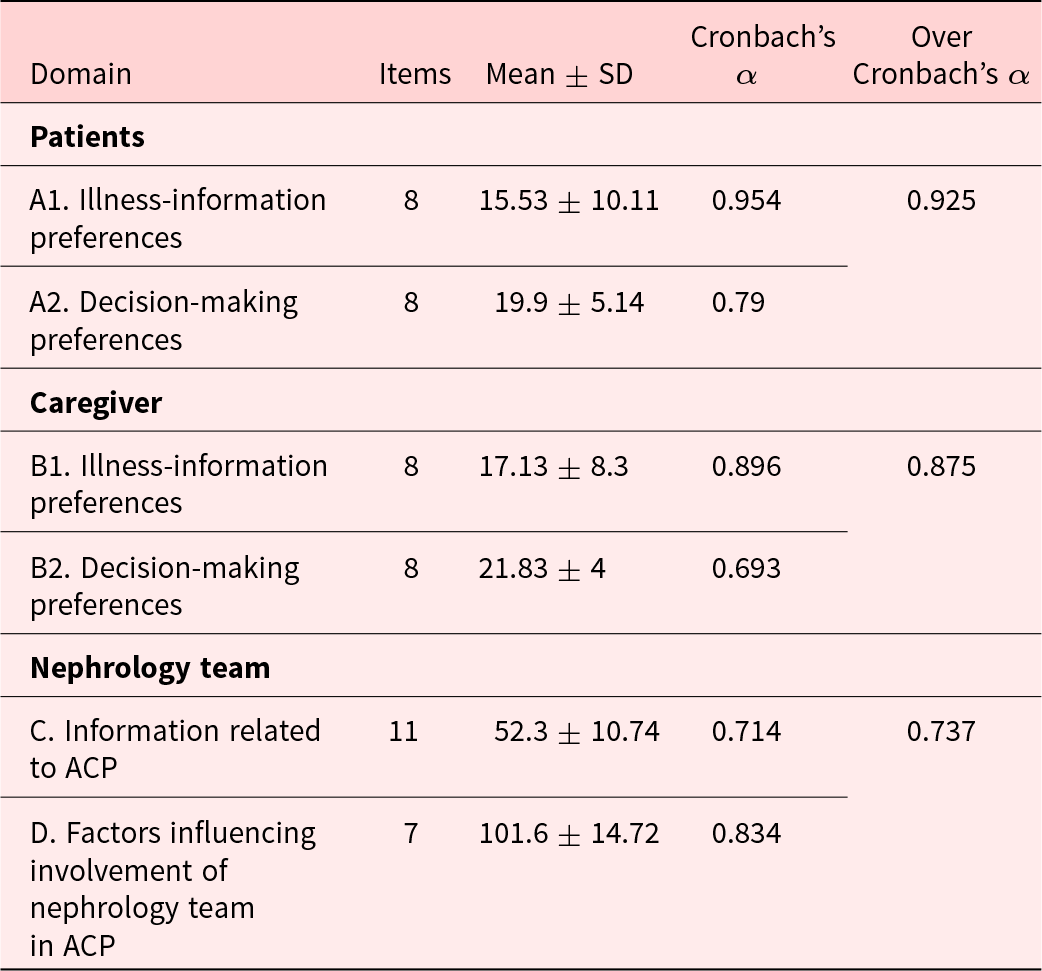
Table 3. The test–retest values of ACP questionnaire among ESKD patients, care givers (family), and nephrology team
Discussion
In this study, a questionnaire was developed to explore ESKD patients, their caregivers and health professionals’ preferences and knowledge of illness trajectory, future course, and forward planning as it might facilitate acceptance of ACP and end-of-life care.
Most high-income countries have implemented ACP as a routine practice (Combs Reference Combs2016; Deodhar et al. Reference Deodhar, Prasad Nagaraju and Kirpalani2021; Song et al. Reference Song, Ward and Fine2015). It is the first study developing and validating a questionnaire exploring ACP preferences in an ESKD setting in India.
In this study, CVR value for each item in questionnaire ranged from 0.6 to 1, which suggests that questionnaire has good content validity. CVR was higher than 0.49 for items of instrument indicating acceptable agreement (Davis Reference Davis1992; Gutiérrez-Sánchez et al. Reference Gutiérrez-Sánchez, Leiva-Santos and Sánchez-Hernández2016; Zamanzadeh et al. Reference Zamanzadeh, Ghahramanian and Rassouli2015). In our study found that questionnaire has an excellent internal agreement and is valid for assessing ACP preferences, knowledge, and acceptance in ESKD patients, their caretakers and kidney care providers.
In low and low-middle income countries, most of the decisions are made by family members in addition to patient themselves (Martina et al. Reference Martina, Lin and Kristanti2021). Therefore, we focused on both, the patient and the family caregivers to know their preferences regarding illness information, ACP decision-making process and documentation.
Along with nephrologists, we involved other nephrology team members who are part of ACP process for an overall better outcome of kidney supportive care. A similar finding was noted in other studies done previously (Davison Reference Davison2006; Weisbord et al. Reference Weisbord, Carmody and Bruns2003). Therefore, a validated ACP questionnaire can be used in kidney supportive care clinics and may be a trigger for initiation and implementation of ACP for ESKD patients in a developing country setting.
Limitations
The development and validation of the questionnaire was a pilot study and convergent validity could not be conducted because this is the first questionnaire developed and validated in the Indian context and is a single-center study.
Conclusion
Both English and Kannada versions of the questionnaire developed in this study are reliable and valid methods for evaluating the preferences and knowledge of ACP in ESKD patients, their family caregivers, and the treating nephrology team. This will help in clarifying and establishing patient and caregiver preferences and goals of care in ESKD patients.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1478951523001797.
Competing interests
None declared.






