Electroconvulsive therapy (ECT) has a long and controversial history in medicine and in the public consciousness.Reference Sadowsky 1 Before the 1960s, ECT was considered a crude and frightening procedure that was administered without standardization or the benefit of anesthesia, muscle relaxants, or emergency equipment.Reference Lebensohn 2 However, with the institution of ethical principles and important advances in ECT methods and procedures, ECT has become a safe, accepted form of treatment for mental disorders and is now used in every continent in the world.Reference Leiknes, Schweder and Høie 3 - Reference Weiner and Coffey 5 ECT is now recognized through numerous rigorous clinical trials to be a robust and effective treatment for severe psychiatric conditions such as major depression and schizophrenia. 6 - Reference Petrides, Fink and Husain 10 Among patients with treatment-resistant depression, ECT has demonstrated a 60% to 80% response rate and a 50% to 60% remission rate.Reference Husain, Rush and Fink 8 , Reference Petrides, Fink and Husain 10 , Reference Kho, van Vreeswijk, Simpson and Zwinderman 11 Despite its demonstrated effectiveness and advancements in procedures, ECT is utilized in less than 0.5% of individuals with major depression in the United States, with utilization rates decreasing over time.Reference Case, Bertollo and Laska 12 - Reference Sackeim 14 Underutilization of ECT may be due to increased regulations around ECT; bureaucratic rules on reimbursement; lack of available hospital resources and trained personnel; increased use of transcranial magnetic stimulation and ketamine; and negative perceptions and inaccurate knowledge about ECT.Reference Case, Bertollo and Laska 12 , Reference Wilkinson, Agbese, Leslie and Rosenheck 13 , Reference Livingston, Wu, Mu and Coffey 15 - Reference Abbasi 21
While there is stigma associated with ECT treatment in the United States, studies have shown that privately insured patients are more likely to receive ECT than poor, publicly insured, or uninsured patients, suggesting vulnerable populations may actually have more limited access to ECT.Reference Case, Bertollo and Laska 12 Thus, there may be socioeconomic disparities in ECT use, and it may be important to understand availability and utilization of ECT among homeless and unstably housed (HUH) populations. ECT is also a treatment which requires multiple sessions, follow-up care, and arrangements for transportation and other healthcare needs, so there may be barriers to ECT use, and providers may be reluctant to offer ECT to HUH populations. There has been virtually no research on ECT use among homeless adults despite the high prevalence of severe mental illness found in homeless populations, including veterans.Reference Tsai and Rosenheck 22 - Reference Fazel, Kholsa, Doll and Geddes 25 The U.S. Department of Veterans Affairs (VA) operates the largest healthcare system in the country serving hundreds of thousands of HUH veterans annually. HUH adults typically face various barriers to care such as uninsurance, brokered healthcare services, difficulties in accessing a regular source of care, and receiving services from underfunded organizations.Reference Kushel, Vittinghoff and Haas 26 - Reference Kim, Swanson, Swartz, Bradford, Mustillo and Elbogen 28 The VA presents a unique opportunity to examine ECT use in an integrated healthcare system where there are fewer barriers to care than other public and private healthcare systems, serving as a national safety net for millions of veterans who are eligible for comprehensive coverage and an array of medical, mental health, and social services.Reference Wilson and Kizer 29
We conducted a descriptive study using VA administrative data from 2000 to 2019 to: 1) compare ECT utilization between HUH and domiciled veterans with mental illness and 2) track changes in ECT utilization among both groups over time. We followed trends between and within both groups over two decades. The results may enhance our understanding of how use of ECT has changed and evolved in a national healthcare system for HUH and general mental health service users.
Methods
Administrative data from all veterans with mental illness who used VA healthcare services from 2000 to 2019 were extracted from VA’s Corporate Data Warehouse (CDW). Mental illness was operationalized using ICD-9 codes starting with 290 to 319 and ICD-10 codes starting with F. ECT sessions were identified using CPT codes (4066F, 90870, and 90871) as well as both ICD-9 (94.26 and 94.27) and ICD-10 (GZB0ZZZ, GZB1ZZZ, GZB2ZZZ, and GZB3ZZZ) procedure codes. In addition, the analyses included not only ECT administered by VA providers, but also ECT administered by approved providers in the community (ie, fee basis claims). These coding procedures were based on previous studies which comprehensively examined ECT in the VA.Reference Tsai, Peltzman, Watts and Shiner 30 , Reference Peltzman, Gottlieb, Shiner, Riblet and Watts 31
HUH veterans were identified using the following methods: 1) ICD-9 (V60.0) and ICD-10 (Z59.0) diagnostic codes for homelessness in inpatient and outpatient records; 2) outpatient stop codes (for HCHV, GPD, and HUD-VASH); 3) inpatient specialty codes (for DCHV and CWT/TR); 4) positive responses to the Homelessness Screener Clinical Reminder; 5) homeless program utilization reported in the Homeless Operations Management and Evaluation System; and 6) Supportive Services for Veteran Families utilization reported by community providers. Veterans with no indication of HUH were presumed to be domiciled. This project was not human subjects research, did not involve contact with any participants, and was conducted as a program evaluation initiative of the VA National Center on Homelessness among Veterans.
First, for each year from 2000 to 2019, analyses determined the total number of patients with any mental health diagnoses, the number of such patients receiving ECT, and the number of ECT sessions, thereby computing ECT use per 1000 veterans and the average number of ECT sessions per ECT patient. Chi-squares were used to compare ECT use rates between homeless and domiciled veterans in each year, and analyses of variance (ANOVAs) were used to compare the average number of ECT sessions per HUH and domiciled veteran each year.
In addition to assessing annual numbers, data from 2000 to 2019 were also compared by Veterans Integrated Service Networks (VISNs) which cover different regions of the country. Because VISNs had been reorganized several times during the observational period of the study, we based all comparisons between VISNs based on their fiscal year 2017 designation. A two-way ANOVA was used to compare changes in number of persons per 100 000 receiving ECT between domiciled and homeless veterans from 2000 to 2019, with time, housing status, and a time by housing status interaction term entered in the model.
As a supplementary analysis, we conducted a logistic regression analysis to examine the association between HUH status on ECT use, adjusting for demographic characteristics, VA service-connection, psychiatric diagnoses, and other clinical variables including the Elixhauser Comorbidity IndexReference Moore, White, Washington, Coenen and Elixhauser 32 extracted from the CDW. We used 1 year of data from 2019 to use recent data but avoid historical confounds of the COVID-19 pandemic in 2020; our sample consisted of all HUH veterans with mental illness in 2019 along with a 10% random sample of domiciled veterans with mental illness in that year as a comparison group.
Results
As shown in Table 1, rates of ECT use among domiciled veterans with mental illness have remained relatively consistent from 2000 to 2019 with 9 to 14 veterans receiving ECT per 1000 veterans. Rates of ECT use among HUH veterans with mental illness have been consistently higher from 2000 to 2019 compared with their domiciled counterparts with 58 to 104 HUH veterans receiving ECT per 1000 veterans. In addition, there has been greater variability in ECT use among HUH veterans than domiciled veterans over time, with an upward trend in ECT use observed among HUH veterans (62 per 1000 veterans in 2000 compared with 85 per 1000 veterans in 2010, which is a 37.1% increase). As shown in Figure 1, there was no visual pattern of synchronous increases or decrease in ECT use between HUH and domiciled veterans over time. Among ECT recipients, both HUH and domiciled veterans attended 5 to 9 sessions of ECT on average across years. There was no significant difference in the number of ECT sessions received per person between domiciled and HUH veterans, except for the years 2008 and 2017 in which domiciled veterans received significantly more ECT sessions than HUH veterans (Table 1).
Table 1. Use of Electroconvulsive Therapy (ECT) Among Domiciled and Homeless Veterans with Mental Illness from 2000 to 2019.

* P < .05.
** P < .01.
*** P < .001.

Figure 1. Trends in rates of electroconvulsive therapy (ECT) use among veterans with mental illness from 2000 to 2019.
Table 2 describes ECT use by VISNs which represent different geographic areas in 2000 and 2019 (mapped in the Supplementary Figure). There was considerable variability in ECT use by VISNs in both years. In 2019, ECT utilization among veterans with mental illness overall was highest in VISNs 1, 20, 9, and 8 (Northeast, Northwest, Midwest, and Southeast regions, respectively). The VISNs with the higher rates of ECT utilization differed between domiciled and HUH veterans. Among domiciled veterans, ECT use among different VISNs ranged from 1.02 to 20.04 per 1000 veterans in 2000 to 2.85 to 15.90 per 1000 in 2019. Among HUH veterans, ECT use ranged from 0.00 to 84.33 per 1000 HUH veterans in 2000 to 3.04 to 132.21 per 1000 in 2019. Thus, there was greater variability in ECT use among HUH veterans compared with domiciled between VISNs in 2000, but the variability in ECT use was similar between HUH and domiciled veterans in 2019. The total denominator and counts of domiciled and homeless veterans who received ECT by VISN are provided in the Supplementary Table.
Table 2. Use of Electroconvulsive Therapy (ECT) by Veterans Integrated Service Networks (VISNs) Among Domiciled and Homeless Veterans with Mental Illness in 2000 and 2019.
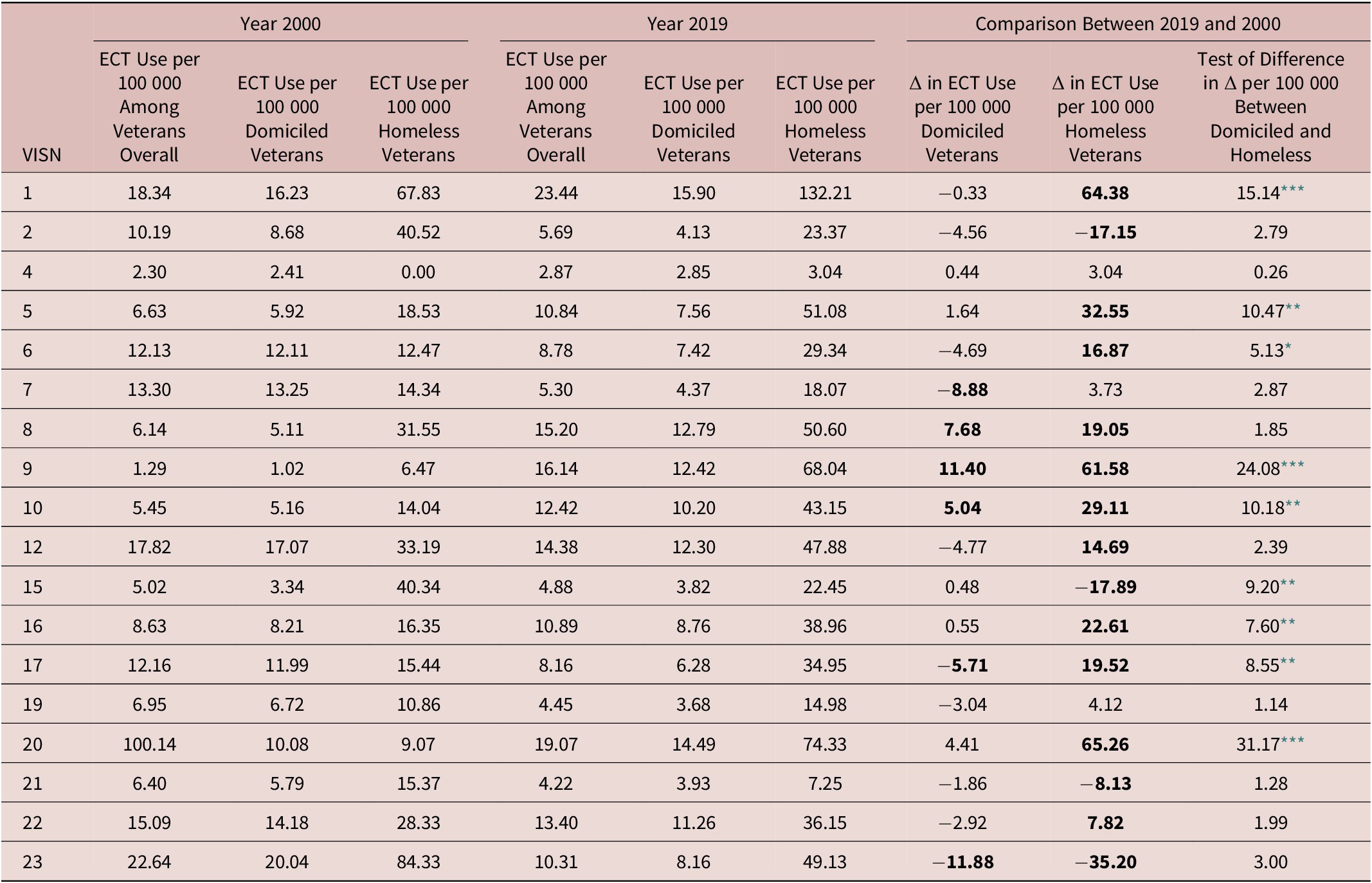
Note: Bolded are Δ > 5.0 per 100 000.
* P < .05.
** P < .01.
*** P < .001.
In addition, there has been greater change and variability in change in ECT use within VISNs between 2000 and 2019 among HUH veterans than domiciled veterans. Among HUH veterans, changes in ECT use between VISNs ranged from −35.20 to 65.26 per 100 000; the greatest increases in ECT use were observed in VISNs 20, 1, and 9, representing the Northwest, the New England Area, and a southern portion of the Midwest (most of Tennessee and Kentucky), respectively. Among domiciled veterans, changes in ECT use between VISNs ranged from −11.88 to 11.40 per 100 000; the greatest increase in ECT use was observed in VISN 9 with a similar magnitude decrease observed in VISN 23 (representing the upper Midwest, including most of North and South Dakota, Iowa, Minnesota, and Nebraska).
There has been an overall greater increase in ECT use among HUH veterans compared with domiciled veterans over time; this greater increase in ECT use for HUH versus domiciled veterans was statistically significant in 7 VISNs (ie, VISNs 1, 5, 9, 10, 16, 17, and 20). It is worth noting that a significant decrease in ECT use among HUH veterans was observed in VISN 15 (representing a southern portion of the Midwest, including most of Kansas and Missouri) while rate of ECT use among domiciled veterans in that VISN was essentially unchanged. Change in ECT use at the VISN level between domiciled and HUH veterans was significantly and moderately correlated, as the Spearman correlation was .56, P = .014.
A supplementary logistic regression analysis of veteran characteristics associated with ECT use in 2019 among domiciled and HUH veterans with mental illness revealed that major depressive disorder and bipolar disorder were most strongly associated with ECT use (Table 3). After controlling for psychiatric diagnoses along with other background characteristics, HUH status was associated with an 86% increased odds of receiving ECT compared with domiciled veterans.
Table 3. Logistic Regression of Sociodemographic and Clinical Characteristics Associated with ECT Use Among Domiciled and Homeless Veterans with Mental Illness in 2019 (n = 100 786)

Note: The sample consisted of all homeless veterans with mental illness and a 10% random sample of domiciled veterans with mental illness.
Discussion
This study described rates and trends in ECT utilization among HUH and domiciled veterans with mental illness in the VA healthcare system from 2000 to 2019. Surprisingly, there was consistently higher ECT utilization among HUH veterans than domiciled veterans across years over the past two decades with a trend toward increasing ECT use among HUH veterans, whereas ECT use among domiciled veterans has remained the same. These findings accounted for the growing population of HUH veterans served by VA during the past two decadesReference Tsai, Pietrzak and Szymkowiak 33 , Reference Rosenheck, Sorkin and Stefanovics 34 , and our analysis of recent data found that HUH status was associated with ECT use even after controlling for other sociodemographic and clinical variables, which makes these findings particularly noteworthy.
While we do not know for certain the reasons for the high ECT utilization among HUH veterans which may not be observed among other HUH adults, we theorize that it may be due to high rates of severe mental illness among HUH veterans, the comprehensive VA healthcare system, and the considerable resources and services available to HUH veterans. The VA’s federal priority to prevent and end veteran homelessnessReference Tsai, Pietrzak and Szymkowiak 33 , 35 may have made it comparatively easier for HUH veterans to access ECT compared with HUH patients who are not veterans, although this needs to be explored in further research. Importantly, we found that, on average, most HUH and domiciled veterans attended 5 to 9 sessions of ECT, which is within general recommendations and guidelines that typically suggest for 6 to 12 sessions but also allow for some clients who may respond to fewer than 6 sessions. 36 , Reference Sackeim, Aaronson and Bunker 37 Thus, we found that many HUH veterans were able to engage with a typical course of ECT treatment which is notable, because many HUH adults experience difficulties with medication adherence.Reference Hunter, Palepu, Farrell, Gogosis, O’Brien and Hwang 38 Since HUH veterans are more likely to use VA-funded residential care than domiciled veterans, use of residential care may have facilitated greater use of ECT among HUH veterans, and this possibility is worth further exploring. The HUH population is known to often require costly acute healthcare servicesReference Tsai, Syzmkowiak and Kertesz 39 , Reference Moore and Rosenheck 40 , and ECT has been found to be a cost-effective treatment for treatment-resistant depression, so ECT may represent an important way to reduce service costs for HUH populations.Reference Ross, Zivin and Maixner 41 Since ECT is often accompanied by ancillary support services, arrangements for transportation, healthcare needs, and follow-up care, it may be that these other services help keep HUH veterans engaged with ECT treatment.
Geographic variability in ECT utilization of veterans with mental illness overall in 2019 somewhat mirrored that observed in non-VA healthcare systems, with higher rates found in the Northeast and Midwest among both HUH and domiciled veterans.Reference Wilkinson, Kitay, Harper, Rhee, Sint, Ghosh, Lopez, Saenz and Tsai 20 Notably, VISN 17 which encompasses Northern California (including an area where ECT was briefly banned during the 1980s) had relatively low levels of ECT use in both domiciled and HUH veterans despite having relatively high levels of homelessness. This finding may reflect variations in culture or stigma that may make it more challenging for patients to receive ECT. The relatively strong correlation in rates of ECT use between HUH and domiciled veterans suggests that local factors (ie, ECT champions, administrators who facilitate ECT) may account for a large portion of the geographic variation between regions.
Findings of the study have clinical and public health implications. Our results confirm those of another study that ECT can be safely and commonly used in HUH adults experiencing mental illness.Reference Wilkinson, Rhee and Tsai 42 This is an important finding, as HUH adults generally have higher rates of psychiatric illness than their domiciled counterpartsReference Edens, Kasprow, Tsai and Rosenheck 43 , Reference Tsai 44 and may be in situations that require a more rapid treatment response. Future work is warranted to assess the effect of ECT on a full range of health outcomes in this specific population. If ECT is effective and feasible to administer in this population, the treatment might warrant consideration as a part of a comprehensive approach to treating HUH individuals with mental illness. A taskforce report of the American Psychiatric Association has indicated that ECT should be considered for individuals with major depression, mania, and schizophrenia, 6 although it remains greatly underused.Reference Sackeim 14 Given that ECT is often initiated when patients are hospitalizedReference Rhee, Olfson, Sint and Wilkinson 45 and that ECT can act relatively rapidly to reduce symptoms of mood and psychotic disorders,Reference Kellner, Husain and Knapp 46 - Reference Petrides, Malur and Braga 48 ECT may be an important part of treatment of complex patients who experience homelessness.
Several limitations of this study require comment. First, changes in how HUH has been identified and captured may have affected the results. For instance, the population of HUH veterans identified has increased over time likely due to increased screening and funding of homeless programs. Second, we relied on coding of ECT in VA medical records using a combination of indicators to be comprehensive, but some ECT visits may not have been documented or included in our indicators. Third, there were relatively small samples of ECT recipients which affected the stability of estimates on ECT utilization rate, especially comparing rates between VISNs. Finally, our analyses based on administrative databases were not able to include important moderating or mediating factors, such as social support, symptom severity, financial issues, and side effects of ECT. Additional studies using alternative approaches are required to improve our understanding of the effects of these clinical and social issues on both ECT use and homelessness.
Conclusion
National administrative data in the VA healthcare system show that HUH veterans commonly and safely receive ECT at higher rates than domiciled veterans over a 20-year period. Large geographic variability in ECT use suggests that there are local barriers to care that need to be overcome to increase access to this treatment for HUH veterans. have access to this treatment. Further work is also needed to understand the specific benefits of this treatment on health outcomes of HUH veterans, ways to reduce barriers to ECT, and optimal ways to maximize treatment gains in this population.
Acknowledgments
The work was supported by the VA National Center on Homelessness among Veterans. The views presented are of the authors alone and do not represent those of any federal agency.
Funding Statement
There was no specific funding for this work.
Disclosures
None of the authors have any disclosures to report, and all authors report no conflicts of interest with this work.
Supplementary Materials
To view supplementary material for this article, please visit http://doi.org/10.1017/S1092852921001061.






