The Professor Leslie Michaels prize for the best presentation of the meeting was awarded jointly to Rebecca Harrison for ‘Maintaining your index of suspicion in unexplained facial palsy’ and Guled Jama for ‘An unexpected cause of neck swelling following total laryngectomy’.
The chairpersons and secretary have edited the proceedings of the meeting to reflect the discussion of each case by the expert panel and audience during the Semon Club meeting.
Introduction
Mucormycosis is classically an aggressive infection, with acute onset and high mortality. We present a 73-year-old immunocompromised gentleman with slow onset, minimally invasive mucormycosis and minimal symptoms.
Case report
A 73-year-old gentleman with chronic myelomonocytic leukaemia with bone marrow fibrosis, who was taking interferon and deferoxamine for iron chelation, was admitted to hospital with a red, swollen right eye. Following computed tomography (CT) imaging, he underwent functional endoscopic sinus surgery three weeks after admission, which revealed a black necrotic turbinate. Interestingly, the patient had no sinogenic symptoms.
Radiological findings
A CT scan of the head revealed right-sided pansinusitis, pre-septal cellulitis and paranasal soft tissue swelling. The scan was repeated following surgical treatment and did not show any improvement.
Histological findings
From the biopsy of the inferior turbinate, Dr Sandison highlighted the inflammatory infiltrate and the large branching fungal hyphae with no septae, characteristic of mucormycosis (Figure 1).
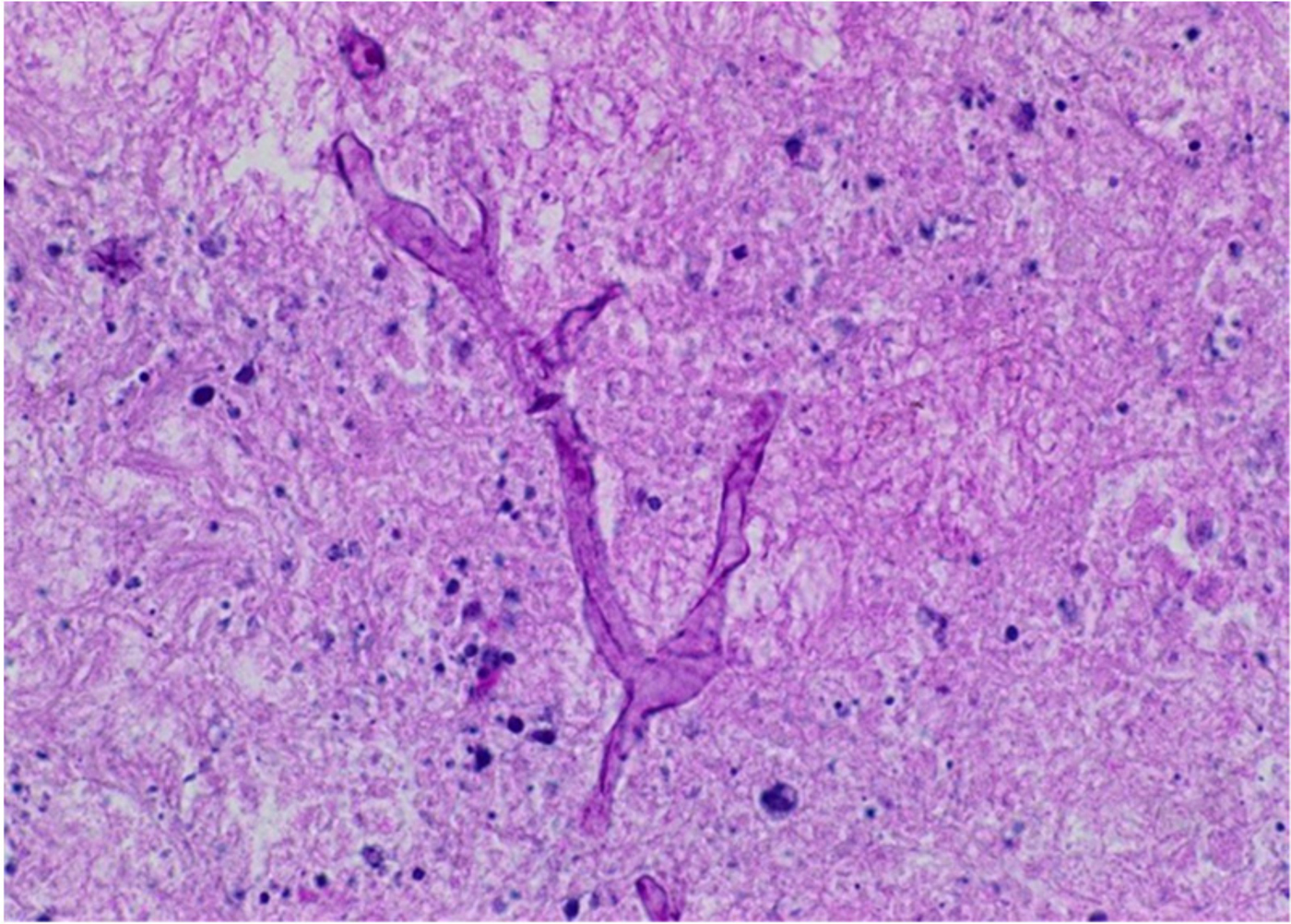
Fig. 1. Histology slide of inferior turbinate showing mucormycosis. (H&E; ×200)
Management
Extensive disease resection was performed. Two endoscopic operations were required, alongside intravenous antifungals and antibiotics. The patient was discharged on long-term antifungals and nasal douches.
Discussion
The patient did not have a culture positive result for mucormycosis. However, Dr Sandison explained that the characteristic histological finding of fungal hyphae is sufficient for diagnosis. Patients should be discharged on long-term antifungals, with interval scans being performed. Dr Connor advised that early magnetic resonance imaging was useful in suspected fungal disease, as minimal disease visible on a CT scan can hide catastrophic clinical disease. Miss Pai enquired as to the difference between fungal infections and mucormycosis on imaging. Dr Connor said that mucormycosis frequently involves soft tissues outside the sinus and causes bony erosion.
Conclusion
In cases of immunosuppression and sinusitis, fungal disease must be considered early. Mucormycosis can be highly invasive with a high mortality, but, as in this case, it can also have a more insidious onset.
Introduction
Phosphaturic mesenchymal tumours are rare head and neck neoplasms. However, they represent a common, often-missed diagnosis for tumour-induced osteomalacia. We report a case of an anterior skull base phosphaturic mesenchymal tumour with intra-orbital and intracranial extension.
Case report
A 70-year-old female presented with a 6-month history of left-sided nasal obstruction, watery eye and eye displacement. Biochemistry revealed hypophosphatemia, hyperphosphaturia and raised alkaline phosphatase. This led to the investigation of tumour-induced osteomalacia. Levels of fibrinogen growth factor 23 were elevated. Complete tumour excision resulted in paraneoplastic effect resolution.
Radiological findings
Dr Connor demonstrated a skull base lesion with left orbit extension and dural invasion on computed tomography (Figure 2). He said the areas of hyperdensity probably represented haemorrhage. The gadolinium enhanced fat suppression magnetic resonance imaging (MRI) images showed extension through the intracranial periosteum.
Fig. 2. Non-contrast computed tomography scan of the sinuses.
Histological findings
Dr Sandison demonstrated the characteristic features of spindle cells, calcification and fatty deposits (Figure 3). She commented on the extensive positive cluster of differentiation 56 staining suggestive of phosphaturic mesenchymal tumour, and explained that to reach a diagnosis, histology must be combined with clinical features.
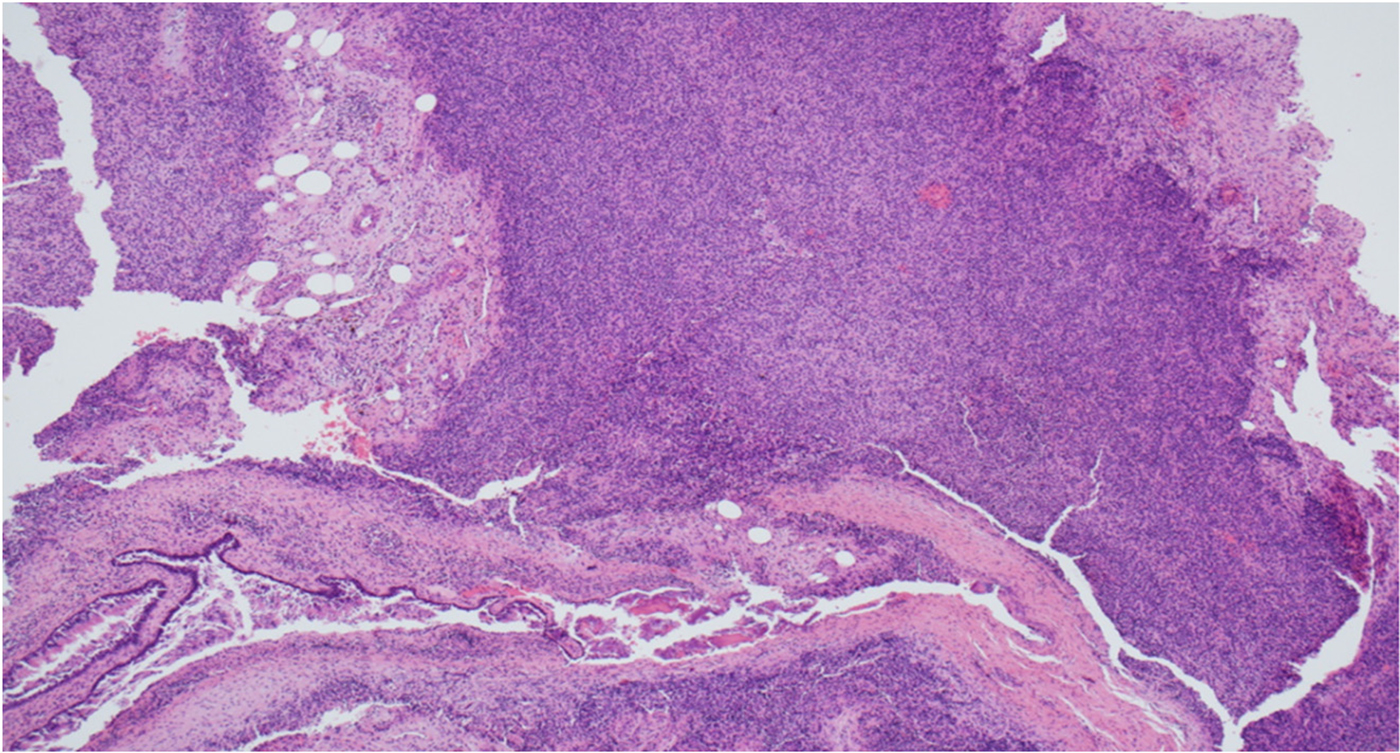
Fig. 3. Histology image. (H&E; ×100)
Management
Endoscopic craniofacial resection along with dura resection with reconstruction was performed. The multidisciplinary team (MDT) recommended clinical and radiological follow up and no adjuvant radiotherapy.
Surveillance MRI demonstrated left frontal lobe tumour cyst recurrence two years following surgery. The patient underwent Ommaya reservoir insertion and cyst aspiration, as per MDT discussion. The cyst re-accumulated twice requiring re-aspiration.
Discussion and conclusion
Cyst aspirate revealed no malignant cells. Dr Sandison recommended testing the cyst aspirate for fibrinogen growth factor 23 levels to support a diagnosis of tumour recurrence. Dr Sandison felt that these are slow-growing tumours and radiosensitivity has not been established, and therefore commented it is possible that radiotherapy could do more harm than good.
Introduction
A rare case of midline nasal destruction secondary to cocaine and the role of levamisole.
Case report
A 20-year-old male cocaine user presented with sepsis, central facial erythema, epistaxis and sinus discomfort following expulsion of nasal cartilage. Rhinoscopy demonstrated paucity of anatomy, subtotal septal perforation and an ulcerated mass. Debridement, wash-out and biopsy were undertaken, revealing destructive granulomatous tissue and a dehiscent skull base.
Vasculitis screen results were antineutrophil cytoplasmic antibody and proteinase 3 positive. Cocaine toxicology was positive, whilst levamisole contamination, reported in cases of granulomatosis polyangiitis secondary to cocaine use, was negative.
Radiological findings
Contrast computed tomography scanning of the head and neck demonstrated destruction of the anterior nasal septum and extensive soft tissue swelling (Figure 4).
Fig. 4. Computed tomography scan of the head and sinuses depicting absent anterior nasal septum and soft tissue swelling.
Management
Urgent endoscopic evaluation and extensive debridement of the nasal cavity was indicated, with intravenous antibiotics administered for superimposed infection (Figure 5).
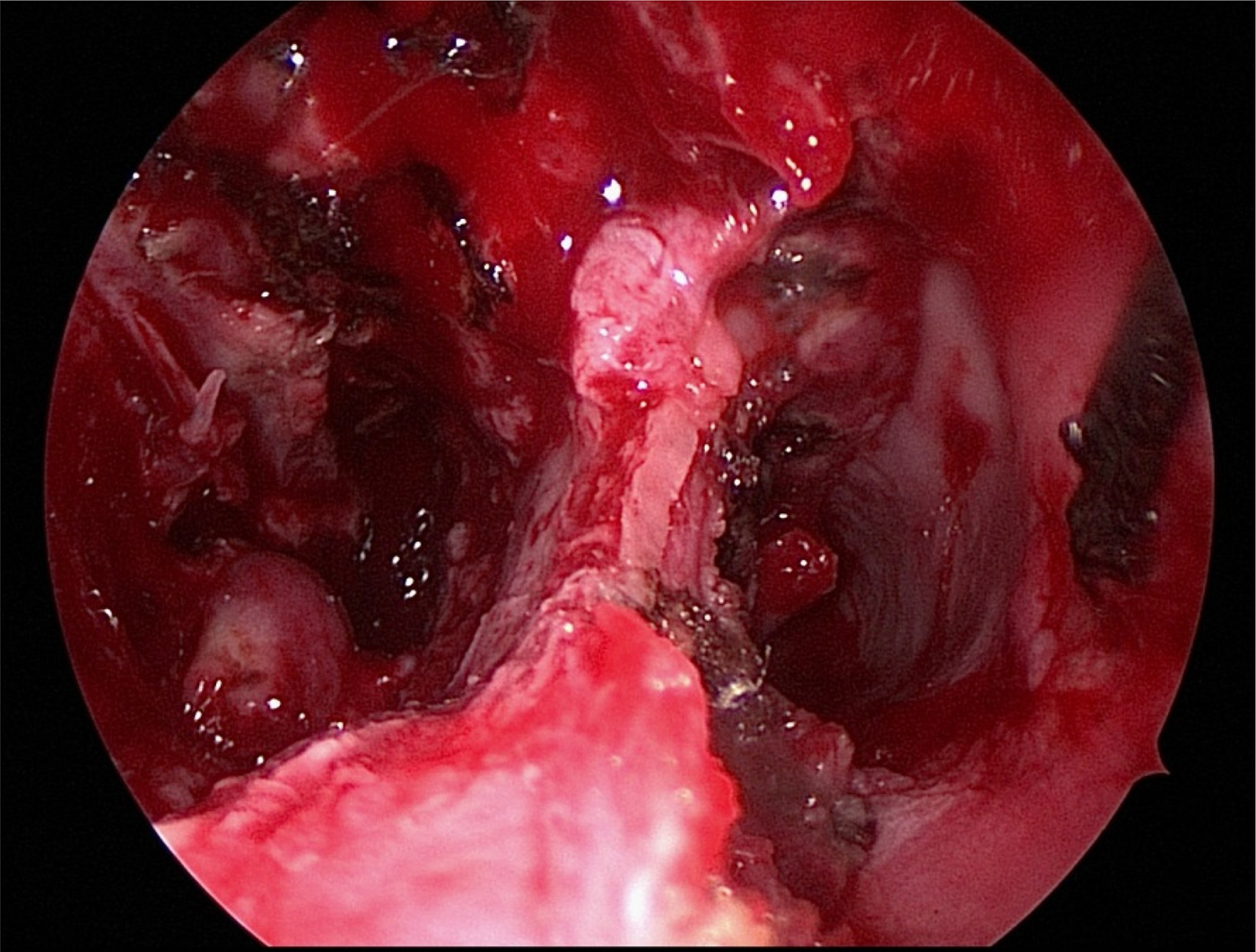
Fig. 5. Endoscopic view of granulomatous tissue and septal perforation.
A clear diagnosis should be ensured using serology, radiology, histology and multidisciplinary team review before implementing immunosuppressants. Cocaine abstinence has a large role to play in both cocaine-induced midline destructive lesion and levamisole-induced vasculitis.
Histological findings
Dr Sandison demonstrated a chronic inflammatory infiltrate with chondrocytes and reactive hyperplasia. This raised the possibility of a polychondritis, but this was excluded by the absence of granulomas. She also pointed out that the lack of vasculitis helped to exclude levamisole as an aetiological agent.
Discussion points
Time-critical plasma testing for levamisole with mass spectrometry has to be within a 5-day half-life, and is required alongside a vasculitis screen to obtain the correct diagnosis in order to prevent unnecessary side effects of immunosuppressants. Increasing awareness is required of levamisole in street cocaine, which is a growing public health issue and difficult to detect by conventional methods.
Introduction
The differential diagnosis for diplopia involves a range of pathologies including neoplastic, vascular, autoimmune and inflammatory conditions, and atypical infections at various levels including the central nervous system, cranial nerves, neuromuscular junction, and/or extraocular muscles. We present an unusual case posing diagnostic and treatment challenges.
Case report
A 67-year-old lawyer with hypertension and diabetes presented with a 5-day history of diplopia on right lateral gaze that was unresponsive to steroids. Clinical examination revealed isolated right abducens palsy with no systemic symptoms. Blood tests including inflammatory markers were normal.
Radiological findings
Dr Connor demonstrated on the computed tomography scan an erosive lesion centred around the clivus that extended into the sphenoid sinus and caused erosion of the basiocciput and basisphenoid (Figure 6). This was uniformly T1 hypointense/short tau inversion recovery (‘STIR’) hyperintense on magnetic resonance imaging, exhibiting strong enhancement post-gadolinium. The differential diagnoses included chordoma, chondrosarcoma and metastasis. Subsequent metabolic imaging revealed no distant pathology. Dr Connor commented on how lesions of the sphenoid are rarely neoplastic. Nevertheless, consideration of a nasopharyngeal carcinoma that had extended up to the skull base was important, as this diagnosis would make biopsy easier and the primary treatment would not be surgical. He stressed the importance of adequate biopsy in such cases.

Fig. 6. Computer tomography scan demonstrating a central skull base lesion originating from the right sphenoid sinus and eroding the clivus.
Histological findings
Histology was reported as submucosal haematoma with normal overlying sinonasal epithelium and no evidence of neoplasia. Some organising granulation tissue including a mild chronic inflammatory/plasma cell infiltrate was noted. Subsequent immunohistochemistry showed the plasma cells to abnormally express cluster of differentiation 56, cyclin D1 and a kappa light chain restriction (Figure 7). Dr Sandison explained that the monoclonal proliferation of plasma cells indicated either a multiple myeloma or a plasmacytoma.
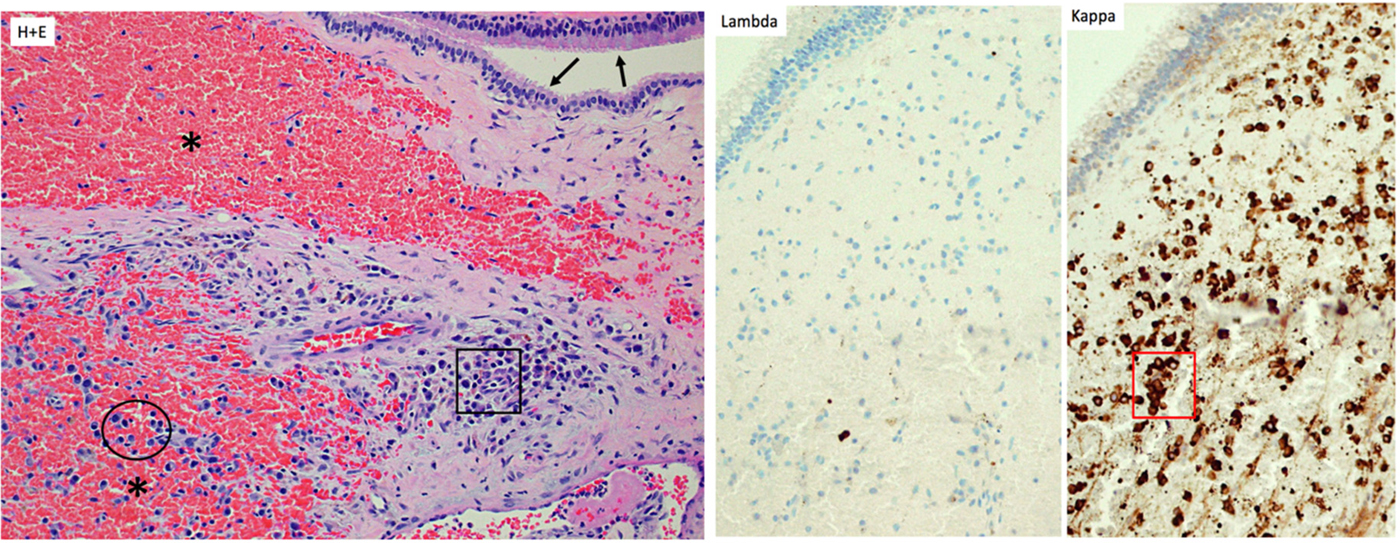
Fig. 7. Haematoxylin and eosin staining of the biopsy specimen. Fragments of sinonasal mucosa (arrows), beneath which an organising haematoma is visible (asterisks). In the submucosa, clusters (square) and scattered atypical plasma cells (circle) with nuclear pleomorphism are present (×100 magnification). The atypical plasma cells expressed Kappa (red square), but not Lambda, light chains (×100 magnification).
Management
Following endoscopic resection, the diplopia resolved. The patient was referred to the haematology department, which diagnosed a solitary extramedullary plasmacytoma following a normal bone marrow biopsy. Although these are radiosensitive tumours, the patient is asymptomatic and remains under surveillance.
Discussion
Dr Sandison advised that if an initial pathology report suggests a haematoma, the pathologists should be asked to review the slides or the slides should be discussed at a multidisciplinary team meeting.
Conclusion
For rare diseases, histology is subject to diagnostic uncertainty, and the threshold for second opinion and further immunostaining should be low.
Introduction
Erdheim–Chester disease is a rare infiltrative histiocytic disorder, with around 800 cases being reported worldwide. Patients most commonly present with skeletal pain, but it has been reported to affect multiple organs.
Case report
A 64-year-old ex-pilot, with a background of late-onset asthma, suffered from an asthma attack and sinusitis whilst abroad. On returning to England, he saw a number of physicians regarding his rhinitis and asthma. One year later, he presented with a week of progressive, right-sided visual loss associated with peri-orbital pain. Figure 8 shows the endoscopic appearance.
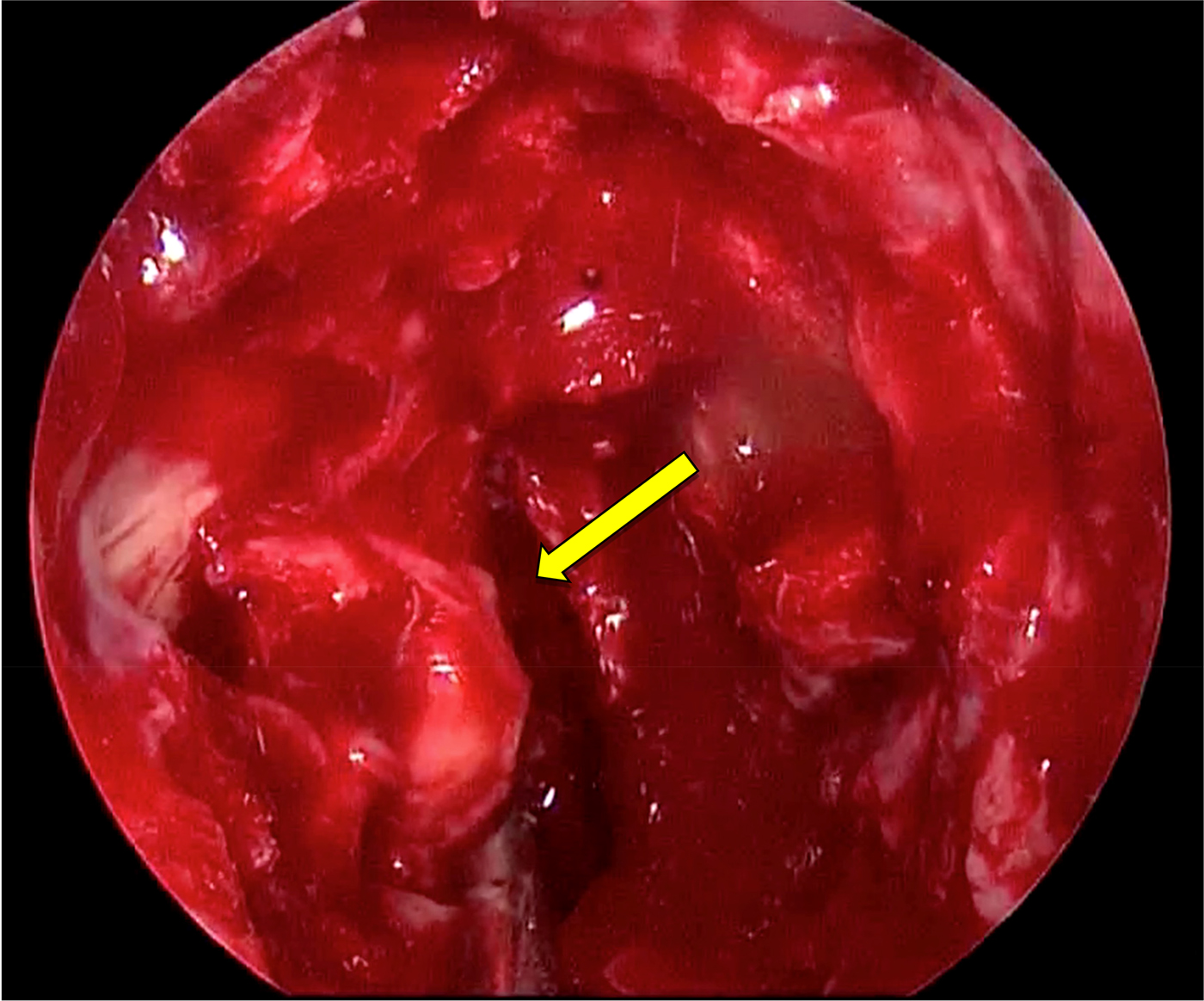
Fig. 8. Lesion identified on right endonasal approach, just medial to the orbit (arrow). The face of the sphenoid has been removed.
Radiological findings
A computerised tomography scan revealed a retro-orbital lesion, pan-sinus opacification, bony erosion of the superolateral wall of the sphenoid sinus, and a pneumatised anterior clinoid process (Figure 9).
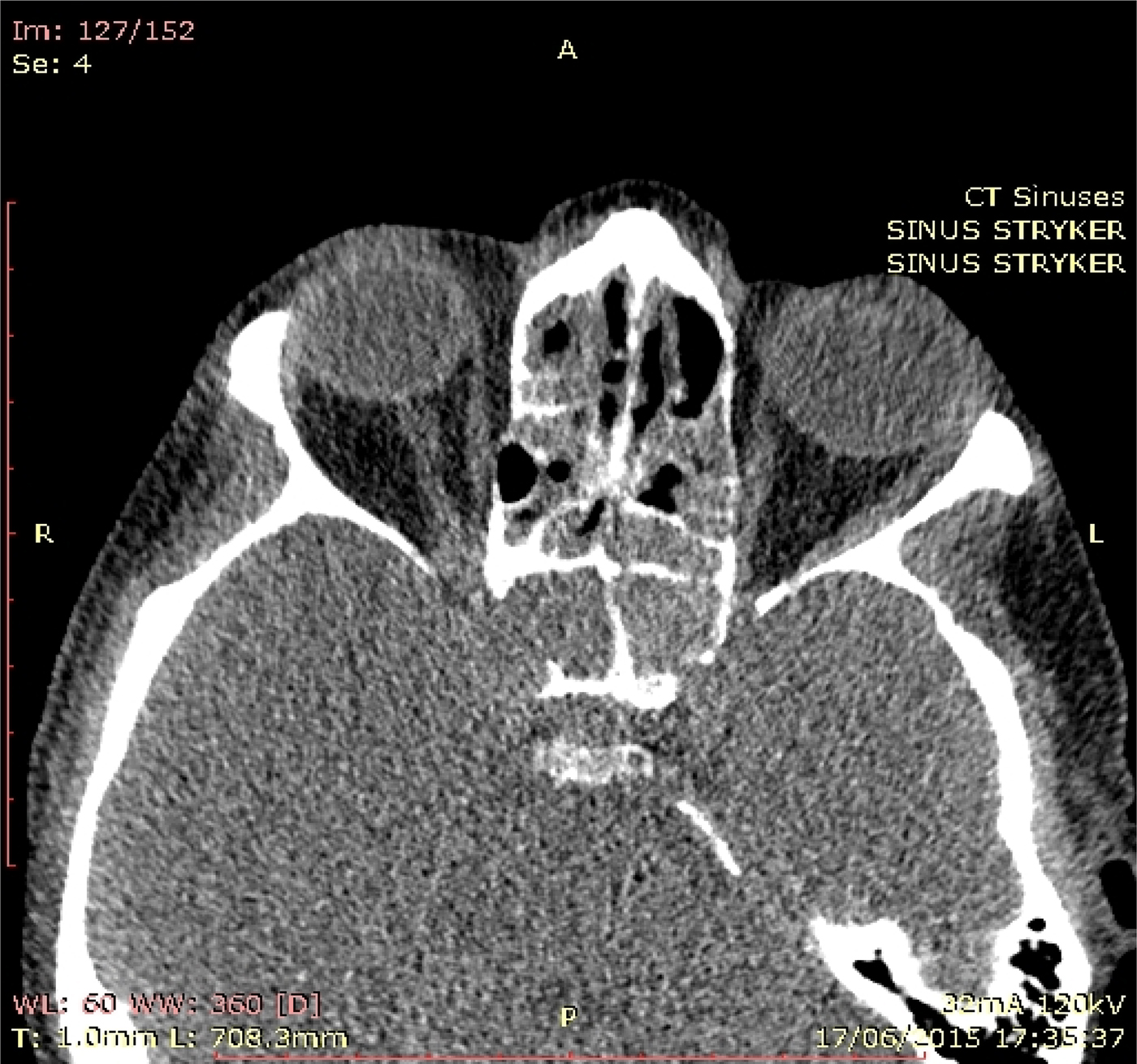
Fig. 9. Computed tomography scan of the head, showing bony erosion of the right superolateral wall of the sphenoid and a pneumatised anterior clinoid process.
Histological findings
Histology indicated late-stage eosinophilic angiocentric fibrosis affecting the paranasal sinuses. Polymerase chain reaction analysis of the BRAF gene revealed a mutation within codon 600. Histiocytes were positive for cluster of differentiation 68 PG-M1 and cluster of differentiation 68 KP-1, and negative for S-100 and cluster of differentiation 1a, confirming a non-Langerhans type histiocytosis.
Management
The patient underwent an emergency right-sided sphenoidotomy to decompress the optic nerve during the first admission. He subsequently received further sphenoid surgery for histological samples. He is currently being treated with oral and nasal steroids, after refusing interferon-α−2a therapy.
Discussion
Dr Sandison explained that non-X histiocytosis is a family of diseases, and pathology can only suggest this family of diseases as a possible aetiology without specifying the exact type.
Conclusion
Erdheim–Chester disease is a rare differential diagnosis for sinusitis and visual loss. Polymerase chain reaction analysis of BRAF V500 may be beneficial where immunostaining results are negative.
Introduction
Epiphora is a common symptom, usually secondary to nasolacrimal duct obstruction.
Case report
A 26-year-old lady presented with a 5-year history of nasal swelling, cheek lesions, loss of sense of smell and nose bleeds. She also described longstanding epiphora, with recurrent conjunctivitis. Examination findings showed mild cobble-stoning of the nasal mucosa. Her nasal bridge was widened, with multiple erythematous raised lesions (10–15 mm) around her nose
Radiological findings
Imaging revealed bilateral rhinosinusitis, along with bony erosion of the medial walls of both maxillary sinuses, and widening of the nasal septum and bridge (Figure 10).
Fig. 10. Axial CT scan of the paranasal sinuses, showing erosion of bony walls and thickened septum.
Histological findings
Histology of the nose revealed chronic rhinitis with collagenous scar tissue. Histology of the cheek showed a dense reticular lesion composed of a storiform pattern of fibrohistiocytic cells and collagen bundles. There was associated inflammatory cell infiltrate comprising plasma cells, eosinophils, neutrophils, lymphocytes and histiocytes. The results of special staining for mycobacteria, bacteria and fungi were negative. Immunoglobulin G (IgG) and IgG4 immunohistochemistry showed a proportion of around 33 per cent. Obliterative phlebitis was not seen (Figure 11).
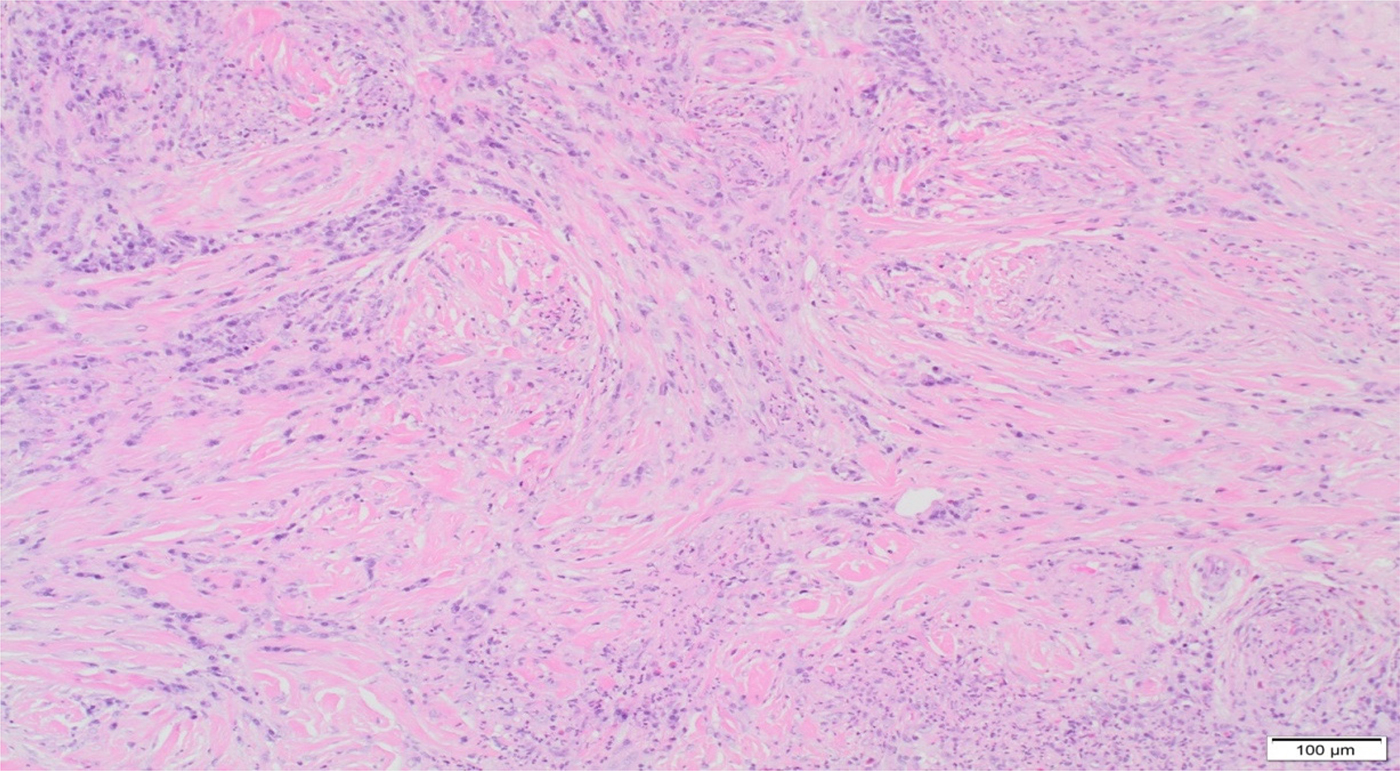
Fig. 11. Punch biopsy of skin histology image. Storiform fibrosis seen in deeper layers of skin. (H&E; ×100)
Management
This involved prednisolone followed by long-term azathioprine.
Discussion
Dr Sandison explained that the mixed inflammatory cell infiltrate was not diagnostic of IgG disease, and that the cheek lesion could be a granuloma faciale. It is possible that treatment may have changed the IgG4 ratio, leading to a difficulty in diagnosis. She suggested that an alternative diagnosis may be inflammatory pseudotumour.
Miss Pai enquired whether excision biopsy was an option, but Mr Ahmed explained that the lesion was very diffuse. He had injected triamcinolone into some of the lesions.
Miss Chevretton commented on possible aetiological factors for chronic inflammatory disease including a nose ring, or topical or inhaled agents.
Conclusion
It is difficult to diagnose IgG-related disease, especially after the acute phase. A multidisciplinary approach with repeat biopsies is the preferred option for such chronic inflammatory diseases.
Introduction
Adult-onset otitis media with effusion is uncommon, and may suggest the presence of skull base pathology. Radiographic investigation is not routinely recommended.
Case report
A 51-year-old woman presented a 7-month history of unilateral otitis media with effusion. Clinical examination revealed a unilateral middle-ear effusion and clear post-nasal space. Audiometry revealed right mixed hearing loss and a type B tympanogram.
Radiological findings
Computed tomography and magnetic resonance imaging showed a right parapharyngeal lesion measuring 5 × 4 × 3 cm, with remodelling of the maxillary antrum and extension into the middle cranial fossa and orbital apex.
Histological findings
Histology revealed respiratory type mucosa infiltrated by the tumour, comprising uniform spindle cells growing in intersecting short bundles, with focal storiform pattern, occasional whorl-like clusters and no necrotic cells. Histology and immunohistochemical analysis confirmed a fibrous meningioma.
Management
The patient refused surgical treatment. A right-sided grommet was inserted. She is currently asymptomatic and is being monitored by the skull base team.
Discussion and lessons learned
Mr Skilbeck highlighted the importance of ophthalmology input given the risk of optic nerve compression. Miss Pai noted the need for a lower threshold for imaging, especially in patients with no prior history of middle-ear disease.
Conclusion
Imaging is imperative in the presence of red flag signs or resistance to medical therapy.
Introduction
Tumours of the external auditory canal are unusual, and can be categorised according to the tissue from which they originate (bone, epithelium, gland) or by behaviour (malignant or benign). They are typically difficult to diagnose without histology because of difficulty in visualisation and a high incidence of concurrent infection.
Case report
A 31-year-old female presented with unilateral ear blockage and mild conductive hearing loss. Otoendoscopy was suggestive of ceruminous adenoma, revealing a smooth, skin-coloured mass with a cystic glandular appearance arising from the anterior wall of the canal (Figure 12).
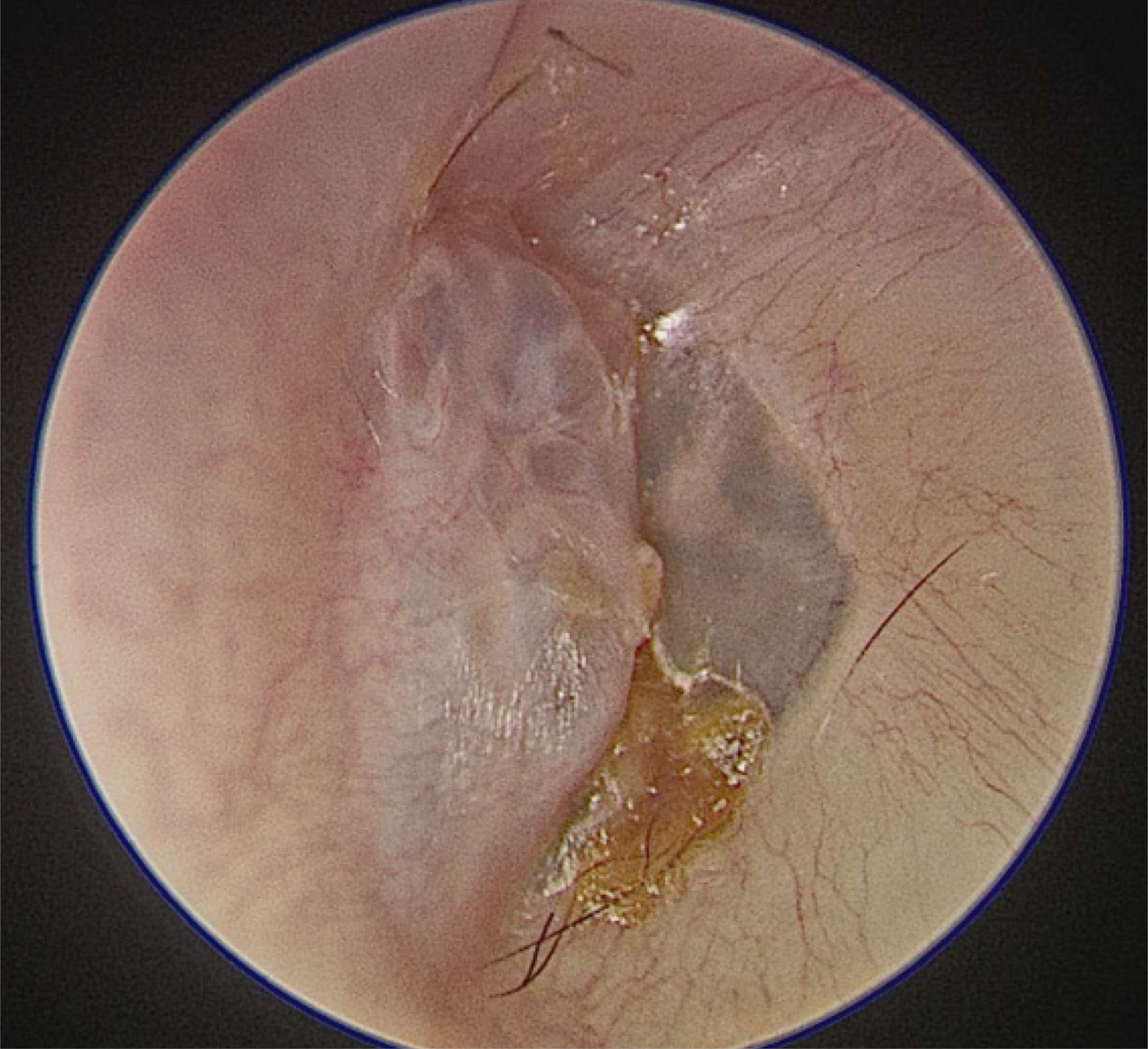
Fig. 12. Otoendoscopic view of left external auditory canal ceruminous adenoma.
Radiological findings
Computed tomography of the petrous bones showed an 8 mm soft tissue lesion abutting the tympanic membrane, with focal thinning of the adjacent tympanic bone.
Histological findings
Histology confirmed a ceruminous adenoma, revealing an unencapsulated tumour composed of cystic glandular spaces showing apical snouts (that produce cerumen) and apocrine sections. A region of lamellated keratin was also seen, suggesting concurrent cholesteatoma.
Management
Wide local excision was undertaken. The patient made a full recovery, with no evidence of recurrence at six months.
Discussion and lessons learned
The case illustrates how helpful good visualisation of external auditory canal lesions via otoendoscopy can be in the out-patient setting, although Mr Skilbeck lamented its cost which restricts its availability. Mr Haikel commented on the unusual location of the lesion close to the tympanic membrane, noting that ceruminous glands are normally present in the outer two-thirds of the external auditory canal. Dr Sandison felt that the lesion may have grown back from the outer part of the canal and may have produced the small amount of wax visible in the photograph (Figure 12).
Mr Haikel noted the presence of hair as well as wax on the tympanic membrane, and suggested maybe the patient had used cotton buds to push both onto the tympanic membrane. Miss Chevretton suggested possible implantation of the lesion deeper into the external auditory canal secondary to the use of cotton buds. The hyperkeratosis element may have arisen from the adenoma preventing normal skin migration.
Conclusion
Otoendoscopy allows excellent visualisation and documentation of external auditory canal lesions.
Introduction
We present the case of a lady with an unusual lesion in the left external auditory canal, found to be a probable anatomical defect.
Case report
A 63-year-old was referred to the otorhinolaryngology department with a lump in the external auditory canal noticed 3 months after an otitis externa. On examination, a spherical lesion was seen on the anterior wall of the external auditory canal, with no signs of infection. The lump moved as the patient opened and closed her jaw. Following investigations, it was found to be the temporomandibular joint (TMJ) protruding into the external auditory canal.
Radiological findings
Computed tomography (CT) confirmed a soft tissue lesion arising from the canal, with underlying bone destruction (Figure 13). Magnetic resonance imaging showed a normal TMJ and internal acoustic meatus.
Fig. 13. Computed tomography scan of the external auditory canal and temporomandibular joint.
Histopathology
An urgent biopsy was performed. The pathologist reported keratinising stratified squamous epithelium consistent with cholesteatoma.
Management
Clinically, there was no cholesteatoma. The head and neck multidisciplinary meeting concluded that the TMJ was protruding into the external auditory canal. The patient was completely asymptomatic; therefore, a repeat CT in six months was planned.
Discussion
This protrusion is likely the result of a patent foramen of Huschke, a congenital bony defect in the external auditory canal wall. When present, it is usually more medially located. The differential diagnosis included bony erosion due to previous otitis externa. However, there was a similar, less severe protrusion in the right ear, making a bilateral congenital defect more likely.
Introduction
The causes of facial palsy are varied and well known. Unusual presentations or unexpected symptoms mandate imaging to exclude tumours and deep-seated infection.
Case report
Tympanoplasty for subtotal perforation was delayed in a patient who developed breast cancer. During chemotherapy, she presented with otalgia and facial palsy, which was investigated initially with computed tomography (CT) and magnetic resonance imaging (MRI) scans. Symptoms resolved over six weeks. A second MRI scan was arranged after another six weeks for partial recurrence of palsy and temporal pain. After a further six weeks, a third MRI scan was performed for a subsequent dead ear and complete palsy. She required urgent surgery for histology. Whilst the frozen section findings were suggestive of lymphoma, formal histology demonstrated fungal infection.
Radiological findings
The CT scan identified facial canal dehiscence. Three MRI scans over four months showed subtle and then worsening high signal intensity in the otic capsule, and finally a rapidly expanding lesion in the internal auditory meatus, encroaching on the cochlea.
Histological findings
Dr Sandison demonstrated a necrotising fungal infection. The majority of the biopsy was dead tissue. There were basophilic septate fungi that were budding. Microbiology confirmed aspergillus as the causative fungus.
Management
Empirical treatment for skull base infection did not ease pain. There was rapid improvement of symptoms following debridement and antifungals, and once they were no longer immunocompromised. The treatment of symptoms included facial nerve graft, a Contralateral Routing Of Signals (‘CROS’) hearing aid and vestibular physiotherapy.
Discussion and lessons learned
Dr Sandison highlighted the importance of not committing to a diagnosis of lymphoma based on frozen section findings; formal histology slides are required for an accurate diagnosis. Mr Skilbeck discussed the extent of disease, which was along the length of the facial nerve from the middle ear to the brainstem. Dr Connor noted the unusual pattern of spread on imaging and suggested possible peri-neural spread along the facial nerve.
Conclusion
Imaging can be falsely reassuring; clinicians must maintain a high index of suspicion in patients with continued problems.
Introduction
Airway obstruction may occur at any point along the respiratory tract. When there is multi-site involvement, sometimes it can be difficult to discern which is responsible for the sudden airway deterioration. We describe a case of a venous malformation of the larynx causing acute airway compromise.
Case report
A five-year-old girl, with known severe life-threatening asthma, and significant but stable tracheobronchomalacia, presented with further acute airway compromise episodes. Flexible bronchoscopy identified a dynamic, compressible and prolapsing arytenoid mass with laryngeal outlet obstruction.
Radiological findings
Ultrasound revealed a lobulated heterogeneous lesion with multiple anechoic vascular channels, demonstrating low flow on Doppler. Computed tomography showed mild left main bronchus narrowing, without an obvious laryngeal mass lesion. Magnetic resonance imaging demonstrated a multi-lobulated, T2/short tau inversion recovery (‘STIR’) hyperintense, T1 isointense, patchily enhancing lesion, centred on the right aryepiglottic fold (12 × 12 mm in transverse and anteroposterior diameter), without a large arterial feeder.
Management
An interventional radiology-led attempt at sclerotherapy of the venous malformation was unsuccessful, under either direct vision or ultrasound-guided percutaneous approach. Serial operations involving microlaryngobronchoscopy under general anaesthesia with potassium titanyl phosphate (KTP) laser to debulk the laryngeal venous malformation have resulted in a visibly shrunken lesion, with better airway control.
Discussion and lessons learned
The panel agreed that laser therapy, rather than surgical resection, is the preferred management choice. Miss Chevretton commented that surgical resection risks potential arytenoid fixation with future associated problems.
Conclusion
Firstly, treat venous malformation when symptomatic. Secondly, laser is most helpful when venous malformations are not amenable to resection. Thirdly, KTP is the laser of choice owing to it being preferentially absorbed by oxyhaemoglobin.
Introduction
Foregut duplication cysts account for one-third of congenital gastrointestinal duplications, and can present with either respiratory or gastrointestinal symptoms.
Case report
An 18-month-old boy presented acutely with a choking episode and respiratory distress whilst eating grapes. Initial bronchoscopy findings were negative. He then developed persistent bi-phasic stridor following a tonsillitis episode, and was referred to the ENT department. A microlaryngo-tracheo-bronchoscopy revealed an 80 per cent narrowing at the mid-tracheal level secondary to external compression.
Radiological findings
Computed tomography revealed an obscuring subtle area of low density to the left of the trachea. Magnetic resonance imaging confirmed a complex cystic structure at the level of the thoracic inlet (Figures 14 and 15).
Fig. 14. Coronal, T2-weighted magnetic resonance imaging scan showing trachea on the right and hyperintense lesion on the left.
Fig. 15. Axial, T2-weighted magnetic resonance imaging scan showing: trachea on the right; oesophagus on the left; and bi-lobulated structure, with fluid level in the posterior component.
Management
The child underwent a bronchoscopy and excision of the cystic mass via a full deep neck incision. The patient made a full and uncomplicated recovery.
Histological findings
Histology revealed stratified squamous epithelium on the surface with underlying layers of muscle bundles arranged into distinct layers, with bundles of skeletal muscle fibres also present but no obvious epithelial lining. The overall appearances were consistent with a foregut duplication cyst.
Discussion
Dr Siddiqui highlighted the importance of considering chronic foreign body irritation as a differential radiological diagnosis. Dr Sandison agreed that despite the lack of epithelial cyst lining on histology, the diagnosis was correct. Mr Pepper also suggested that, in retrospect, it may have been possible to see the fullness of the posterior tracheal wall during the flexible bronchoscopy.
Conclusion
This case highlights the need to consider foregut duplication in cases of unusual presentation of choking and respiratory distress. This can pose diagnostic difficulties, particularly in the acute setting.
Introduction
We report a rare case of type II first branchial sinus presenting as an intra-parotid collection. Such rare anomalies can frequently lead to delayed diagnosis. A high index of suspicion is recommended. Complete excision is key.
Case report
A two-year-old boy with multiple co-morbidities, including chromosome 18p deletion, presented with chronic recurrent left submandibular infections with ipsilateral otorrhoea. Examination demonstrated a punctum opening in the neck, superolateral to the hyoid bone, coursing over the mandibular angle. No external auditory meatal abnormality was noted.
Radiological findings
Magnetic resonance imaging of the neck demonstrated a left parotid lesion with increased T1 and intermediate T2 signal, restricted diffusion and rim enhancement, with expansion of the gland. The lesion (1.5 × 1.3 cm) extended medial to the mandibular ramus. There was tracking of the T2 high signal extending to the left submandibular cutaneous surface, and a right parotid lesion (1.6 × 0.9 cm) of similar signal characteristics.
Histological findings
The tubular specimen (4.5 × 1 cm) demonstrated cartilage with overlying squamous mucosa and seromucinous glands. There was also granulation tissue formation with many multi-nucleated giant cells. Findings were consistent with a branchial cyst or sinus.
Management
The tract was excised en bloc, flush to the external auditory meatal, with an ellipse of submandibular skin.
Discussion and lessons learned
Bilateral first branchial anomalies are extremely rare. Chromosome 18p deletion is associated with numerous symptoms and signs, but not branchial anomaly. Magnetic resonance imaging is imperative to define the course of the facial nerve in such patients.
Conclusion
First branchial anomalies can present as a cyst, sinus or fistula between the external auditory meatal and submandibular area. They typically do not regress, with a propensity for recurrent infections. Surgery is the definitive treatment, but there is a risk to the facial nerve.
Introduction
We present the treatment challenge of a patient with profound hearing loss on a background of osteopetrosis. This case is of particular interest as we believe this is the first case of infantile osteopetrosis where cochlear implantation has been recommended. We discuss the unique challenges that infantile osteopetrosis poses in cochlear implantation.
Case report
A 14-year-old was referred to the paediatric implant programme with bilateral, profound, progressive, mixed hearing loss, in the setting of osteopetrosis, bilateral blindness, spinal stenosis and left-sided mandible osteomyelitis with a chronic mandibular fistula resulting from a dental extraction. Computed tomography and magnetic resonance imaging were performed, and the scans were reviewed at the unit's otology radiology multidisciplinary team (MDT) meeting. The best approach to cochlear implantation was debated.
Radiological findings
Diffuse sclerosis and thickening of the skull base and calvarium were noted, combined with ossific obliteration of the central mastoid tracts with no peripheral air cell formation on either side. There were markedly thickened mastoid bones. There was some reduction in the size of the middle ears, which were otherwise aerated. The otic capsules were normal. There was moderate narrowing of the cochlear apertures although they appeared patent, as well as narrowing of the facial canal.
Management
The MDT decided that the safest surgical approach would be a per-meatal round window approach via a front-to-back mastoidectomy and then a blind sac closure. The plan would be for sequential bilateral cochlear implantation. The right cochlea was the first to be operated because of concerns regarding implantation in the same side as the chronic mandible osteomyelitis.
Discussion
Miss Pai discussed the fact that there could be future challenges caused by ongoing narrowing of the internal auditory meatus, but that nonetheless cochlear implantation was the best current option to provide access to sound. It was agreed that cochlear implantation through a permeatal approach was the safest option available for this patient.
Introduction
We present a case of a 61-year-old, fit and well gentleman, who presented to the ENT clinic with a 1-month history of a slow-growing left submandibular lump.
Case report
He had no pain, dysphagia, weight loss or night sweats. The lump did not fluctuate in size. He had a non-tender, 2 cm, soft, left-sided submandibular lump with no skin changes. The rest of the upper aerodigestive tract examination revealed normal findings.
Radiological findings
An ultrasound scan showed two well-defined hypoechoic lesions (1.9 cm and 1 cm).
Histological findings
Histology of the core biopsy showed cytologically bland, bi-layered oncocytic epithelium, with partial cystic change. Histology of the excised submandibular gland confirmed cystic areas of varying sizes lined with bi-layered, cytologically bland oncocytic epithelium. There was no evidence of malignancy or a stromal lymphoid component.
Management
This involved an uncomplicated left submandibular gland excision.
Discussion and lessons learned
Following the core biopsy, differential diagnoses included an oncocytic cystadenoma or Warthin's tumour. Factors going against a diagnosis of Warthin's tumour included no stromal lymphoid component on histology, and Warthin's tumours are usually confined to the parotid. Dr Sandison explained that malignant change in an oncocytic cystadenoma is highly unlikely; thus, a conservative approach would be reasonable, especially if the patient was high risk for a general anaesthetic. Dr Sandison demonstrated how oncocytic cells appear under microscopy as bright pink cells with lots of mitochondria.
Conclusion
Oncocytic cystadenomas of the submandibular gland are rare and treatment entails surgical excision.
Introduction
Acute calcific tendinitis of longus colli is an uncommon manifestation of calcium hydroxyapatite deposition disease. The clinical presentation mimics that of a retropharyngeal abscess, and therefore prompt diagnosis is key in avoiding unnecessary antibiotic use or inappropriate attempts at surgical drainage.
Case report
A 60-year-old man presented to the emergency department with a 3-day history of worsening neck pain, restricted movement and mild odynophagia. On examination, he had marked torticollis; he was afebrile, had no cervical lymphadenopathy and his voice was normal. Blood tests revealed mildly elevated inflammatory markers. Flexible nasoendoscopy showed swelling of the posterior pharyngeal wall.
Radiological findings
A lateral X-ray of the neck showed swelling of the prevertebral soft tissues. Computed tomography (CT) with contrast confirmed retropharyngeal oedema. Magnetic resonance imaging (MRI) with contrast demonstrated enhancement of thin fluid dissecting into the longus colli (Figure 16). Detailed review of the CT images revealed an amorphous calcification anterior to C1/C2 (Figure 17), confirming the diagnosis of acute calcific tendinitis.
Fig. 16. T1-weighted, fat-saturated, axial magnetic resonance imaging scan with contrast, showing enhancing fluid dissecting into the left longus colli.
Fig. 17. Axial computed tomography with contrast, showing calcification anterior to C1/C2.
Management
The patient had initially been treated with intravenous antibiotics. Once the diagnosis was confirmed, the antibiotics were stopped, and his symptoms resolved with non-steroidal anti-inflammatories.
Discussion
Dr Siddiqui emphasised that calcium hydroxyapatite is not well visualised on MRI, and CT is crucial in making the diagnosis. Miss Pai highlighted the importance of discussion with the radiologist if the diagnosis remains unclear. Dr Sandison reminded the audience of the importance of checking biochemical markers of calcium metabolism in such cases.
Conclusion
In the absence of a septic clinical picture, calcific tendinitis should be considered as a differential diagnosis of acute neck pain and torticollis, which is best diagnosed using CT.
Introduction
Nasopharyngeal perforation is a rare event. The majority of cases reported in the literature have been associated with traumatic nasogastric tube insertion. Previous accounts have described intrathoracic complications, including pleural effusion and mediastinitis. To our knowledge, there are no other reported cases of nasopharyngeal perforation resulting in unilateral cervical subcutaneous emphysema as demonstrated in this case.
Case report
A 73-year-old man underwent total laryngectomy and right hemithyroidectomy for invasive squamous cell carcinoma of the glottis (tumour–node–metastasis staging of T4aN0M0). A standard, uncomplicated operation was performed. An 8 Fr polyurethane nasogastric tube was placed to facilitate enteral feeding post-operatively. On day 5, the patient reported a gradual onset swelling in the left side of his neck. Physical examination showed a soft, fluctuant, non-tender lump over the left submandibular area, with no associated skin erythema.
Radiological findings
A subsequent computed tomography scan of the neck demonstrated a sizeable air-filled cavity within the left submandibular and submental regions, with associated subcutaneous emphysema in the left parapharyngeal and parotid areas (Figure 18). An air leak arising from the left nasopharynx was identified (Figure 19).
Fig. 18. Computed tomography scan of the neck.
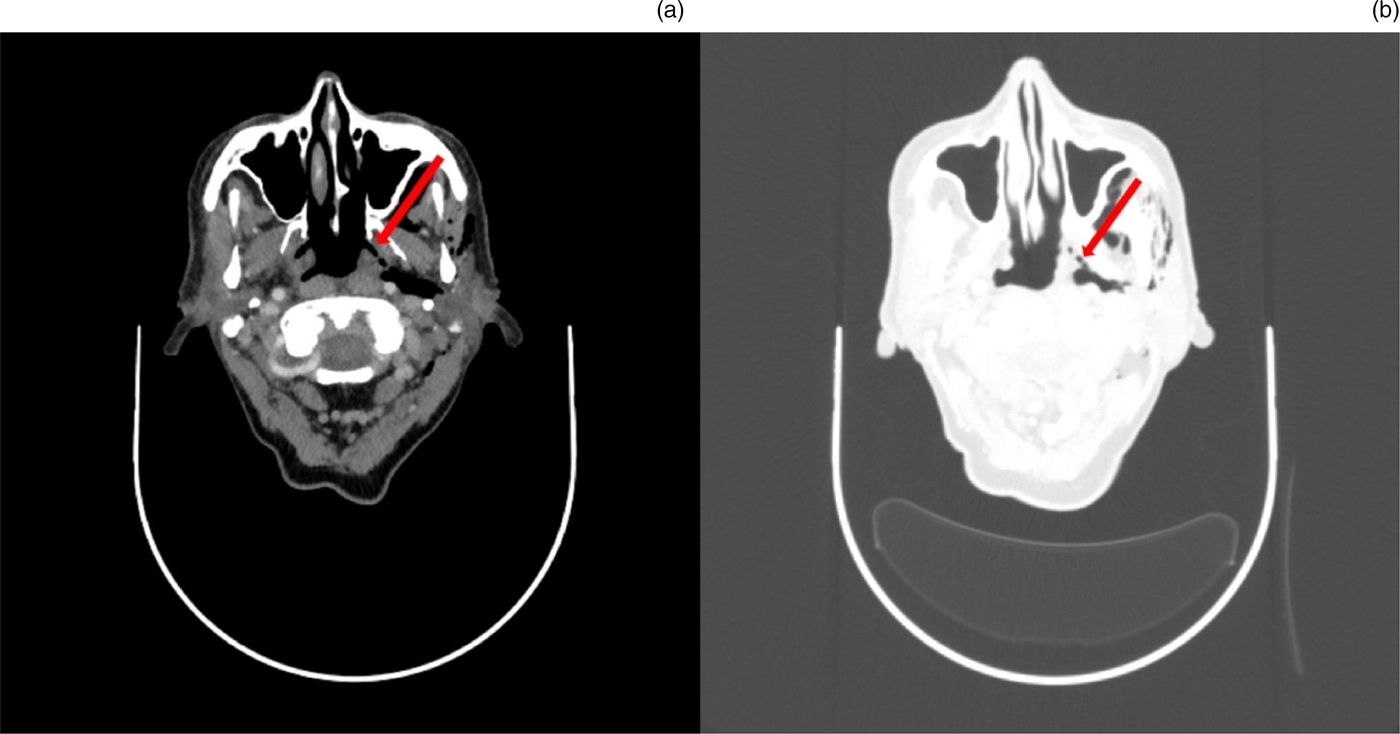
Fig. 19. Computed tomography scans of the neck.
Management
The patient was managed with fine needle aspiration of the lump and a pressure dressing. His post-operative recovery was otherwise uneventful. Endoscopic re-examination of his post-nasal space on day 20 showed healed nasopharyngeal mucosa.
Discussion
Nasopharyngeal perforation is a rare but recognised complication of nasogastric intubation. Miss Pitkin highlighted that the risk of iatrogenic injury is likely to be greater in the anaesthetised patient who is unable to co-operate.
Introduction
Tracheobronchopathia osteochondroplastica is a rare condition affecting the large airways. The presenting symptoms are varied, and include cough, haemoptysis, recurrent infections, or acute presentation with stridor. Investigatory findings are typical. Computed tomography (CT) or direct vision (by bronchoscopy or microlaryngoscopy) typically demonstrates exophytic calcification. Although more than half of cases do not progress after diagnosis, effective management includes inhaled (or injected) corticosteroids or laser excision. In extremis, tracheostomy may be required.
Case report
We present two cases referred to us. The first case was a 67-year-old male presenting with recurrent chest infections, chronic obstructive pulmonary disease, nasal mucopus and crusting, with CT-proven chronic sinusitis. Management included tracheostomy for respiratory failure and close monitoring. The second case was a 52-year-old female presenting with idiopathic stenosis requiring laryngotracheal reconstruction, repeat subglottic balloon dilatations and steroid injections. Both patients had examination findings consistent with tracheobronchopathia osteochondroplastica.
Radiological findings
The CT scans showed subglottic exophytic calcification with an irregular contour, and nodular submucosal calcification of the cartilaginous trachea extending down into the bronchi, with sparing of the posterior membranous trachea.
Histological findings
Histology showed granulation tissue and a fibrotic submucosa, with an active chronic lymphoplasmacytic inflammatory infiltrate and haemorrhage.
Management
Management entailed microlaryngoscopy, laser and steroid injections as required, with regular follow up. Both patients remain well. One patient has moved out of the country; the other remains on regular follow up with intermittent microlaryngoscopy and laser excision.
Discussion
The panel agreed that the diagnostic findings are pathognomonic for tracheobronchopathia osteochondroplastica. Miss Pitkin suggested that perhaps many of these cases are misdiagnosed as chronic obstructive pulmonary disease.
Conclusion
Computed tomography investigation for large airway disease will reveal characteristic findings of tracheobronchopathia osteochondroplastica. Correlation with microlaryngoscopy and histology confirms this unusual, but easily diagnosed, condition.
Introduction
Deep neck space abscesses are life-threatening presentations to ENT surgeons. We present a novel case of a palatine tonsillar low-flow lymphovenous malformation pre-disposing to multifocal deep neck space collections and resultant airway compromise.
Case report
A 37-year-old male presented with a sore throat and pyrexia. He then rapidly developed trismus, complete dysphagia and stridor. Examination identified fluctuant masses over the right parotid and in the neck at level IIa. Immediate management consisted of intravenous steroids, fluids and antibiotics, with the airway secured in an operating theatre using nasotracheal intubation prior to imaging.
Radiological findings
Contrast-enhanced computed tomography (CT) revealed two deep neck space collections: in the right parapharyngeal and masseteric space, and within the inferior aspect of the masseter muscle.
Management
After surgical tracheostomy, the abnormal tonsil was removed by bipolar dissection and pus was drained intraorally. Externally, the parapharyngeal space was opened, and blunt dissection was performed between the parotid gland and masseter where the final abscess was drained.
Histological findings
Histology revealed a tonsil lined with squamous epithelium and mucosal lymphoid tissue, but extending into the submucosa, which was a focus of dilated vascular (cluster of differentiation 31 and cluster of differentiation 34 positive) and lymphatic (D2-40 positive) tissue, without atypia, consistent with a cavernous lymphangioma.
Discussion
The panel noted that this is a rare pathology. Mr Pepper mentioned that, in his experience, these malformations spread across multiple fascial planes. Dr Siddiqui advised that magnetic resonance imaging be performed to exclude any further extension of this malformation which would not be detected with the current CT imaging.
Conclusion
Tonsillar low-flow lymphovenous malformations are rare in adults, and lymphatic stasis can predispose to secondary deep neck space infection. Management centres on the basic principles of airway management and formal drainage.
Introduction
Although bilateral recurrent laryngeal nerve (RLN) palsy is a known complication of total thyroidectomy, we present a unique case following hemithyroidectomy.
Case report
A 36-year-old woman with a 1-year history of a neck lump opted for hemithyroidectomy, despite the lesion's benign appearance on ultrasound. The procedure was uneventful and the left RLN was stimulated successfully.
Post-operatively, the patient was dysphonic, with associated aspiration. Flexible nasolaryngoscopy demonstrated immobile vocal folds in the paramedian position, suggestive of bilateral RLN paralysis.
Management
A magnetic resonance imaging scan of the neck demonstrated a minor seroma only. Oral steroids and thickened fluids were commenced, and she was discharged 3 days post-operatively. Neurology opinion was of bilateral vocal fold dysfunction secondary to neuropraxis.
Serial out-patient endoscopic evaluation demonstrated gradual recovery of vocal fold movement, slower on the non-operated, right side. By eight weeks, her voice and vocal fold function was normal.
Discussion
Compression of the RLN by the endotracheal tube cuff and stretching of the vagus nerves during neck overextension have both been described in the literature, and a combination may have been responsible in this case. Miss Chevretton raised the point that the endotracheal tube may have been displaced proximally during transfer to the operating table, or have an overinflated cuff, thus jeopardising the RLNs. Miss Pitkin also mentioned that endotracheal RLN monitors make the tubes more bulky and thus increase the risk of neuropraxia.
Conclusion
In all cases of endotracheal intubation, ensuring that the tube is inserted distally enough and avoiding excessive neck extension can reduce the risk of RLN injury.
Introduction
We present a case of severe achalasia with an incidental finding on imaging.
Case report
A 90-year-old female presented with a 6-month history of progressive dysphagia, weight loss and frailty. Past medical history included coronary disease and achalasia. Indirect laryngoscopy revealed marked anterior displacement of the larynx with a large post-cricoid space. Computed tomography was requested to exclude upper oesophageal malignancy and to assess the extent of achalasia.
Radiological findings
Computed tomography (CT) and positron emission tomography-CT imaging showed no post-cricoid lesion. There was gross oesophageal dilatation from C6 to the gastroesophageal junction. There was an incidental finding of a 6.7 × 5.6 cm, metabolically active, left anterior mediastinum mass.
Histological findings
Computed tomography guided biopsy was requested, which the patient did not undergo.
Management
The achalasia was treated with oesophageal dilatation. Management of the mediastinal mass must be considered in the context of an independent, fit 90-year-old woman. Management decisions will be made following a patient-centred discussion exploring the risks versus the benefits of endoscopic intrathoracic removal compared to conservative management.
Discussion and lessons learned
It is unlikely for surgery to be the best treatment option, given the status of this patient. Miss Chevretton made the case that perhaps interval scanning would be better than CT-guided biopsy. This would allow surveillance of the tumour. If fast-growing, biopsy is an option, whilst slower growth would prompt observation.
Conclusion
The difficulty of dual pathology and the importance of a patient-centred approach are highlighted in this case.


