Introduction
Benign paroxysmal positional vertigo (BPPV) is the most common inner-ear pathology and type of vertigo seen in emergency departments, out-patient neurology and otolaryngology clinics today.Reference von Brevern, Radtke, Lezius, Feldmann, Ziese and Lempert1,Reference Balatsouras, Ganelis, Aspris, Economou, Moukos and Koukoutsis2 It is characterised by brief sensations of dizziness and nystagmus induced by changes in head position with respect to gravity, with associated nausea and vomiting. Patients with BPPV are at an increased risk of depression, anxiety, falls and significant impairment of daily activities, with some studies suggesting an increased risk of osteoporosis.Reference Yu, Liu, Cheng and Wang3–Reference Zhu, Li, Ju and Zhao8 This disease most often occurs in middle-aged patients, with a peak onset between 50 and 60 years of age and an increased incidence among women.Reference Baloh, Honrubia and Jacobson9 For older adult patients aged over 60 years, BPPV has been shown to increase the risk of neurodegenerative dementia.Reference Kim, Yoo, Min and Choi10 The seriousness of the long-term implications of BPPV for quality of life and associated health conditions highlights the need for efficient diagnosis and management.
The basic pathophysiology of BPPV is well elucidated in the literature. Calcium carbonate particles in the utricular otolith membrane of the elliptical capsule are dislodged and enter the semicircular canals.Reference Yetiser11 When there is a change in position with respect to gravity, these particles are moved to different positions in the semicircular canals, leading to the sensation of motion and dizziness. Management for BPPV can vary depending on the suspected location of origin. The posterior semicircular canal is the most common origin site of BPPV (60–90 per cent of cases), as it is the most gravity-dependent canal.Reference Furman and Cass12 The horizontal semicircular canal can also be involved, but this site is more likely to resolve spontaneously. Rarely, particles can gather in the anterior semicircular canal, the most anatomically superior site.
Although BPPV is a common disease with a good prognosis, evidence-based diagnosis and treatment are essential to effectively manage this condition. Studies show that the cost to ultimately diagnose BPPV is on average greater than $2000 per patient, with a majority of patients receiving unnecessary diagnostic testing, including imaging such as magnetic resonance imaging and echocardiography, inappropriate medications, physical therapy and numerous office visits.Reference Grill, Strupp, Müller and Jahn13,Reference Wang, Yu, Song, Su and Yin14 The burden of vertigo has been shown to greatly affect the working population, with 63.3 per cent of afflicted patients losing workdays, 4.6 per cent changing their jobs and 5.7 per cent giving up their employment because of daily symptoms of dizziness.Reference Benecke, Agus, Kuessner, Goodall and Strupp15 Delays in therapeutic intervention of BPPV can greatly impair quality of life and increase healthcare costs for patients.
Clinical practice guidelines are valuable tools used to assist healthcare practitioners to guide clinical decisions and improve patient outcomes. There are multiple guidelines currently available in the international literature, with varying recommendations for BPPV.
The Appraisal of Guidelines for Research and Evaluation II instrument is a validated set of tools used to measure the rigour and quality of clinical practice guidelines.Reference Brouwers, Kho, Browman, Burgers, Cluzeau and Feder16 The Appraisal of Guidelines for Research and Evaluation II tool is used to assess six domains: ‘scope and purpose’, ‘stakeholder involvement’, ‘rigor of development’, ‘clarity of presentation’, ‘applicability’ and ‘editorial independence’. The instrument has been widely used in scientific literature to analyse clinical practice guidelines and has been shown to be a valid measurement tool.Reference Chorath, Garza, Tarriela, Luu, Rajasekaran and Moreira17–Reference Brouwers, Kho, Browman, Burgers, Cluzeau and Feder20
This study aimed to systematically assess the quality of all clinical practice guidelines describing the diagnosis and management of BPPV using the Appraisal of Guidelines for Research and Evaluation II tool.
Materials and methods
Search strategy
This study follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. We conducted a comprehensive search of clinical practice guidelines up to 30 October 2021 using PubMed, Scopus and Embase electronic databases, to identify diagnostic and treatment guidelines, recommendations, and consensus statements for BPPV. The references of relevant clinical practice guidelines were scanned for additional clinical practice guidelines. The database search query was: ((‘benign paroxysmal positional vertigo’ or ‘BPPV’) and (‘guideline’ or ‘recommendation’ or ‘consensus’)). For clinical practice guidelines published in languages other than English, we searched for translated versions of the guidelines and all supplemental materials.
Study selection
All records were exported to Excel and duplicates were removed. We screened all titles for relevant articles and retrieved the full text of relevant clinical practice guidelines for further analysis. Each guideline had to meet the following inclusion criteria: (1) clinical practice guidelines had to be developed by experts, and include recommendations or guidelines to improve patient care; (2) clinical practice guidelines must be available in English language; and (3) clinical practice guidelines must be evidence-based with a set of references. We excluded all clinical practice guidelines for: (1) other causes of dizziness; (2) no specific recommendations or guidelines outlined; and (3) older versions of guidelines. One author (SP) performed the data collection, which was reviewed for consistency by a different author (NVS). The complete clinical practice guideline document, with references, appendices and supplementary material, was collected for analysis.
Quality appraisal
Quality appraisal of the clinical practice guidelines was performed via the Appraisal of Guidelines for Research and Evaluation II instrument. This is a 23-item tool organised into 6 domains. Each item is rated on a seven-point scale. A score of 7 on an item indicates that the quality of the guideline meets all criteria outlined via the Appraisal of Guidelines for Research and Evaluation II tool. Each domain score was calculated as (obtained score − minimum possible score) / (maximal possible score − minimum possible score). Domain scores under 60 per cent were considered to indicate lower quality. Each appraiser completed all necessary online training tools available on the Appraisal of Guidelines for Research and Evaluation II website (www.agreetrust.org) prior to analysing the included guidelines. Four academic appraisers (SP, VS, DR and ED) performed the methodological quality appraisals independently according to the Appraisal of Guidelines for Research and Evaluation II instrument.
Statistical analysis
Intraclass correlation co-efficients were calculated for each Appraisal of Guidelines for Research and Evaluation II domain using Python 3.8.2 and the ‘pingouin’ application programming interface. A random sample of k judges rate each target. The measure is one of absolute agreement in the ratings. Intraclass correlation co-efficient 2 is sensitive to differences in means between raters and is a measure of absolute agreement. The level of agreement was classified according to the following cut-offs: poor (less than 0.40), fair (0.40–0.59), good (0.60–0.74) or excellent (0.75–1.00).
Results
Literature search
The steps of the literature search performed are displayed in Figure 1. The initial literature search yielded 798 articles, of which 519 documents remained after duplicates were removed. These were screened by title, and 56 were selected for further review. These were then assessed for eligibility, and five met the inclusion criteria described earlier. Any discrepancies were addressed in verbal discussion between the authors (SP, NVS and KR).
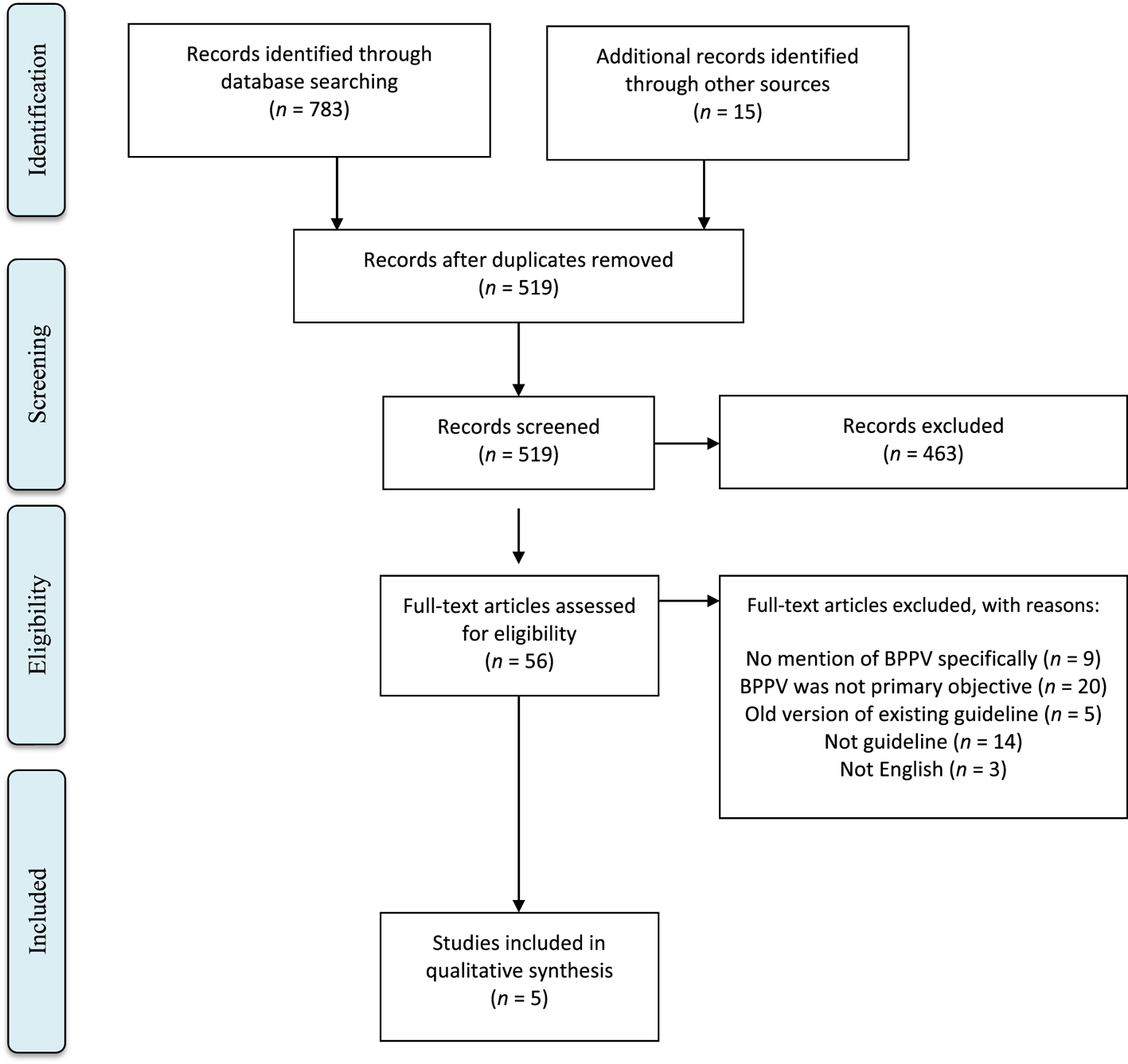
Fig. 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (‘PRISMA’) flowchart of systematic search strategy. BPPV = benign paroxysmal positional vertigo
Guideline characteristics
The general characteristics of the five included clinical practice guidelines are displayed in Table 1. One clinical practice guideline was written by the American Academy of Otolaryngology – Head and Neck Surgery (AAO-HNS),Reference Bhattacharyya, Gubbels, Schwartz, Edlow, El-Kashlan and Fife21 one by the Bárány Society,Reference von Brevern, Bertholon, Brandt, Fife, Imai and Nuti22 which is an international interdisciplinary society of neurotology, one by a group of experts from China,Reference Wang, Chan and Liu23 and the other two by European nations: one from SpainReference Pérez-Vázquez, Franco-Gutiérrez, Soto-Varela, Amor-Dorado, Martín-Sanz and Oliva-Domínguez24 and one from Italy.Reference Gnerre, Casati, Frualdo, Cavalleri and Guizzetti25 All the clinical practice guidelines were published between 2015 and 2019. One was developed using expert consensus via the Delphi study method, two by expert consensus, and the remaining two using both expert consensus and literature review. The developers were diverse, including general otolaryngologists, otologists, general practitioners, nurses, physical therapists, emergency medicine doctors, radiologists and audiologists. The target users in all cases were healthcare providers, with most guidelines specifying particular fields. Funding sources were reported in two of the clinical practice guidelines.
Table 1. General characteristics of included clinical practice guidelines

AAO-HNS = American Academy of Otolaryngology – Head and Neck Surgery
Guideline appraisal
The mean Appraisal of Guidelines for Research and Evaluation II domain scores are displayed in Table 2. The highest average scores were in domain 1 and domain 4, ‘scope and purpose’ and ‘clarity and presentation’, with scores of 51.11 and 58.33, respectively. The lowest scores were in domain 2, domain 3 and domain 5, ‘stakeholder involvement’, ‘rigor of development’ and ‘applicability’, at 35.28, 37.08 and 13.96, respectively, with only the AAO-HNS 2017 guideline clearing the 60-point threshold required for these guidelines to be considered ‘high quality’.Reference Bhattacharyya, Gubbels, Schwartz, Edlow, El-Kashlan and Fife21 The greatest variance between clinical practice guidelines was in ‘stakeholder involvement’, with a standard deviation of 34.2, and the lowest variance was in ‘clarity and presentation’, with a standard deviation of 22.7. Overall, four clinical practice guidelines were found to be ‘low quality’, and one, the AAO-HNS 2017 guideline, was found to be ‘high quality’.Reference Yetiser11
Table 2. Quality appraisal of included clinical practice guidelines using scaled domain scores

AAO-HNS = American Academy of Otolaryngology – Head and Neck Surgery; SD = standard deviation
Intraclass reliability
The intraclass correlation co-efficients for the six domains are presented in Table 3. These values reflect the degree of consistency between the four reviewers (SP, VS, ED and DR). All six domains achieved the maximum ‘very good’ intraclass reliability.
Table 3. Intraclass correlation co-efficients for AGREE II domains

AGREE II = Appraisal of Guidelines for Research and Evaluation instrument; ICC = intraclass correlation co-efficient; CI = confidence interval
Discussion
Because of the wide differential diagnosis for patients presenting with symptoms of dizziness and vertigo, BPPV is often underdiagnosed and misdiagnosed on initial presentation. Appropriate investigation to elucidate the cause of vertigo can be guided by clinical practice guidelines, which serve as valuable tools for clinicians when making healthcare decisions. High-quality clinical practice guidelines can decrease adverse patient outcomes, and they give a clear, standardised approach to managing disease while reducing variations in practice.Reference Brignardello-Petersen, Carrasco-Labra and Guyatt26–Reference Chakraborty, Brijnath, Dermentzis and Mazza28 International collaboration in the provision of evidence-based recommendations for BPPV is crucial to reduce treatment delays and improve quality of life for all patients worldwide. This study analysed five clinical practice guidelines on the diagnosis and management of BPPV, and found multiple domains that can be standardised to improve clarity and guidance for clinical decision making.
The two highest-scoring domains in our analysis were ‘scope and purpose’ and ‘clarity and presentation’, demonstrating the well-defined objectives of each guideline, the intended audience and the easily identifiable recommendations. Multiple guidelines (Italy, 2015;Reference Gnerre, Casati, Frualdo, Cavalleri and Guizzetti25 China, 2019;Reference Wang, Chan and Liu23 and AAO-HNS, 2017Reference Bhattacharyya, Gubbels, Schwartz, Edlow, El-Kashlan and Fife21) presented flow diagrams to assist in directing next steps for varying clinical presentations, with well-defined timelines, diagnosis options and treatment plans. Additionally, the picture diagram representations of the performance of specific manoeuvres necessary for the diagnosis and management of BPPV, such as the Dix–Hallpike manoeuvre, supine roll test, Epley manoeuvre, Semont (‘liberatory’) manoeuvre, Lempert 360-degree roll manoeuvre and Gufoni manoeuvre, were clearly delineated in a series of steps in multiple guidelines, allowing a better understanding of how to properly execute these manoeuvres.
‘Applicability’ received the lowest average score out of all the domains, with only the AAO-HNS 2017 guidelineReference Bhattacharyya, Gubbels, Schwartz, Edlow, El-Kashlan and Fife21 achieving the ‘high quality’ threshold. This domain consists of presenting the facilitators, barriers, resource implications and monitoring criteria for guideline implementation. Our study consisted of international guidelines, with collaboration from physicians from over seven different countries. While the majority of diagnostic and management approaches for BPPV are relatively low cost, differences in international access to resources such as customised vestibular rehabilitation sessions for refractory BPPV cases can lead to an increase in healthcare costs and emergency department visits.Reference Nada, Ibraheem and Hassaan29 Moreover, BPPV has been shown to recur after treatment, with a recurrence rate of 37 per cent at 60 months.Reference Sakaida, Takeuchi, Ishinaga, Adachi and Majima30 The AAO-HNS 2017 guidelineReference Bhattacharyya, Gubbels, Schwartz, Edlow, El-Kashlan and Fife21 provided clear evidence, alternatives, risks, costs, exceptions and differences in opinions for each action statement presented, allowing healthcare professionals to understand the full scope of each recommendation. In future updates to international guidelines, barriers to management should be recognised and alternative approaches must be appreciated.
‘Stakeholder involvement’ and ‘rigor of development’ also received low average domain scores. ‘Stakeholder involvement’ identifies the individuals responsible for creating the final recommendations, and determining patient views and target users for the guidelines. The initial BPPV presentation can be at a variety of healthcare settings, including the emergency room, primary care clinics, or neurology or otolaryngology clinics.Reference Pal'chun, Kryukov, Guseva and Makarov31 One study found that the average time from first referral to BPPV diagnosis was 93 weeks, emphasising the need for oto-neurological skills in primary care settings to allow timely and cost-effective help for patients in need.Reference Fife and FitzGerald32 The role and opinion of healthcare workers in multiple different specialties must be considered when designing guidelines, to ensure expert consensus for clinical diagnosis and management. Of note, the developers for all guidelines were diverse, including general otolaryngologists, otologists, general practitioners, nurses, physical therapists, emergency medicine doctors, radiologists and audiologists, appropriately representing professionals involved in the care of BPPV. Guidelines can be improved to optimise completeness and involve all stakeholders by including patient views and incorporating patient satisfaction from the recommendations presented.
The ‘rigor of development’ domain has been reported to have the greatest weight in determining the overall quality of clinical practice guidelines by some authors.Reference Hoffmann-Eßer, Siering, Neugebauer, Brockhaus, McGauran and Eikermann33 It consists of analysing the comprehensiveness and systematic methods used to search and include evidence for each guideline and provide an explicit methodology for updating procedures. One guideline (Bárány, 2015Reference von Brevern, Bertholon, Brandt, Fife, Imai and Nuti22) was developed using expert consensus via the Delphi study method, which has been widely used in the literature to develop healthcare quality indicators.Reference Boulkedid, Abdoul, Loustau, Sibony and Alberti34 It consists of using a series of questionnaires sent to experts to ultimately create a systematic set of consensus statements. However, a well-known methodological issue with the Delphi method is the lack of concrete definition for ‘consensus’ amongst experts for group agreement. This drawback can also be seen with two more guidelines (China, 2019;Reference Wang, Chan and Liu23 and Italy, 2015Reference Gnerre, Casati, Frualdo, Cavalleri and Guizzetti25), which used expert consensus without a well-defined method for consensus. The remaining two guidelines (AAO-HNS, 2017;Reference Bhattacharyya, Gubbels, Schwartz, Edlow, El-Kashlan and Fife21 and Spain, 2017Reference Pérez-Vázquez, Franco-Gutiérrez, Soto-Varela, Amor-Dorado, Martín-Sanz and Oliva-Domínguez24) used both expert consensus and a literature review, with transparent procedures for including and excluding evidence. Each guideline had a robust set of references to support its recommendations.
Finally, the ‘Editorial Independence’ domain consists of explicitly declaring any conflicts of interests from group members and reporting any influence from funding bodies in the creation of the guidelines. Three guidelines reported no details of funding or conflicts of interests, which raises concern for possible bias (China, 2019;Reference Wang, Chan and Liu23 Italy, 2015;Reference Gnerre, Casati, Frualdo, Cavalleri and Guizzetti25 and Spain, 2017Reference Pérez-Vázquez, Franco-Gutiérrez, Soto-Varela, Amor-Dorado, Martín-Sanz and Oliva-Domínguez24). The remaining two guidelines offered appropriate and transparent mention of any conflicts of interest and funding (AAO-HNS, 2017;Reference Bhattacharyya, Gubbels, Schwartz, Edlow, El-Kashlan and Fife21 and Bárány, 2015Reference von Brevern, Bertholon, Brandt, Fife, Imai and Nuti22). This is essential for ensuring that evidence-based recommendations have no sources of bias.
Limitations
Our study has several limitations. First, while our search strategy was methodological and thorough, it is possible that some recommendations and guidelines were not included in this study. Our analysis included the PubMed, Scopus and Embase databases, but there may be relevant literature that exists outside these resources. Furthermore, there were multiple guidelines with recommendations to diagnose and treat vertigo that may have included a diagnosis of BPPV but were ultimately not included, as these recommendations were not specific to BPPV.
In addition, although the Appraisal of Guidelines for Research and Evaluation II instrument is an evidence-based tool for assessing the rigour and quality of guidelines, the rating assigns equal weight to all domains, despite variations in importance. The tool can only be used to appraise the methodological rigour of included guidelines, but cannot assess the scientific accuracy of the subject matter. Moreover, the tool is based upon subjective interpretation by each reviewer, which is susceptible to individual biases. Although intraclass correlation co-efficient scores were consistent amongst appraisers, the subjective nature of assessing each domain must be considered. Clinical practitioners should use their own judgement and acknowledgement of available resources for each patient when identifying key recommendations from clinical practice guidelines to use in their everyday practice.
Recommendations
Based on the guidelines reviewed, there were certain key recommendations that were common across all clinical practice guidelines. These recommendations are summarised as follows.
Diagnosis of BPPV begins with a focused history and physical examination. The history should focus on defining characteristics, including whether the dizziness occurs with respect to gravity, duration and accompanying symptoms. For the physical examination, the ‘gold standard’ for diagnosis is the Dix–Hallpike manoeuvre. It is important to note the direction of nystagmus and the side with worse symptoms when performing the manoeuvre. A positive Dix–Hallpike manoeuvre is when there is a period of latency of 1–2 seconds, followed by up-beating, torsional nystagmus, lasting less than 1 minute. A positive test confirms the diagnosis of posterior semicircular canal BPPV. If the Dix–Hallpike manoeuvre provides horizontal or no nystagmus, clinicians can proceed to perform the supine roll test. A positive supine roll test, demonstrated by horizontal nystagmus, confirms the diagnosis of horizontal semicircular canal BPPV. After diagnosis, treatment with particle repositioning manoeuvres such as the Semont or Epley manoeuvre can be performed. Patients should be closely followed and may need vestibular rehabilitation for persistent symptoms. Radiographic imaging is not routinely indicated for patients who meet diagnostic criteria for BPPV. Patients should not be prescribed vestibular suppressant medications, as there is no literature supporting their use in managing BPPV.
Conclusion
High-quality clinical practice guidelines and recommendations based on multidisciplinary and rigorous unbiased methodological development can create pathways for providers to optimise outcomes for patients. A variety of guidelines have been developed for the diagnosis and management of BPPV. Of the five guidelines assessed, only the AAO-HNS clinical practice guideline was rated as high quality. Our analysis shows that the ‘applicability’ domain has the greatest potential for improvement, emphasising the need for recommendations to include barriers to management and alternative approaches. In the future, international collaboration amongst multidisciplinary stakeholders should be promoted in order to standardise BPPV clinical practice guidelines, for better healthcare practice and patient care.
Competing interests
None declared






