Specialist mental health services should be available to all relevant clients, irrespective of gender, physical capabilities or ethnic background (Department of Health, 2000). All services should strive to achieve equality of access. The existing literature suggests not only that a diagnosis of personality disorder is given less frequently to Black clients than White (Reference Strakowski, Lonczak and SaxStrakowski et al, 1995), but also that Black clients might not have equal access to specialist mental health services (Reference Littlewood and LipsedgeLittlewood & Lipsedge, 1989). Henderson Hospital should receive an ethnic minority referral rate of 14%, based on the geographical area from which the majority of referrals originate (SE England).
The prevalence of personality disorder in the UK is between 4-33% (Reference HobsonHobson, 2000), and increases with the level of health service setting from 13% of general practitioner (GP) clients to 40-50% of in-patient psychiatric patients (Reference Casey and TyrerCasey & Tyrer, 1986, Reference Casey and TyrerCasey, 1988). There are no figures relating to ethnicity (Reference NdegwaNdegwa, 2003). Black clients are less likely than White to be diagnosed with personality disorder, and more likely to be diagnosed with schizophrenia (Reference Strakowski, Lonczak and SaxStrakowski et al, 1995).
Ethnic minorities are over-represented in psychiatric services (Reference LondonLondon, 1986) and especially in compulsory psychiatric care (Reference Ineichen, Harrison and MorganIneichen et al, 1984). This Bristol study found that ethnic minorities accounted for 17% of voluntary and 36% of compulsory psychiatric admissions. Conversely, ethnic minorities are under-represented in specialist psychotherapy services (Reference CamplingCampling, 1989) and are less likely than White clients to be offered counselling (32% v. 75%) (Reference AlexanderAlexander, 1999) or psychological therapy (Reference Commander, Cochrane and SashidharanCommander et al, 1999).
It has been suggested that the therapeutic community, such as that at Henderson Hospital, is a suitable treatment model for ethnic minorities, and that while only 1 in 50 (2%) referrals in 1991 were from ethnic minorities, the appropriateness of the treatment to the client group had not been widely recognised (Reference Dolan, Polley and AllenDolan et al, 1991). The beneficial treatment effect of Henderson Hospital is positively correlated with increasing length of stay (Reference Dolan, Warren and NortonDolan et al, 1997). Therefore, as a general rule, the longer residents can be maintained in treatment, the better. Research on the staff team at Henderson Hospital found that they considered that being in any kind of minority (including ethnicity) is a risk for leaving early (Reference BlountBlount, 2001). Were the therapeutic community less appropriate for people from different cultural groups, it might be expected that those people from different cultural groups would stay less time in treatment than those from the White groups.
Aims
This study intended to identify the proportion of referrals to this specialist service of clients from ethnic groups, to identify whether clients from ethnic minority groups are more likely to leave the referral and treatment process earlier than White clients, and to explore reasons for any differences found.
Method
Henderson Hospital is a residential unit in Surrey offering therapeutic community treatment to adults with severe personality disorders (Reference Warren and DolanWarren & Dolan, 2001). The hospital is centrally funded and is part of a national service for personality disorder, which includes Webb House in Crewe and Main House in South Birmingham. The process of referral to Henderson Hospital begins with a referral letter and standard form submitted by the referring professional. A staff ‘referrals group’ determines one of three possible disposals:
-
1 the referral is rejected
-
2 a referral is made to the outreach service or
-
3 a candidate is invited to attend a selection group.
A client must be selected before they can be admitted to the hospital. The selection group comprises three staff members and nine current residents in the therapeutic community, and decisions to offer admission are made by democratic vote.
Clients can exit the process at three stages (as shown in Figure 1):
-
1 At the time of the initial decision of the referral group
-
2 At the time of the selection group (this might be because the client does not attend the group or the group does not select the client)
-
3 During residential treatment.
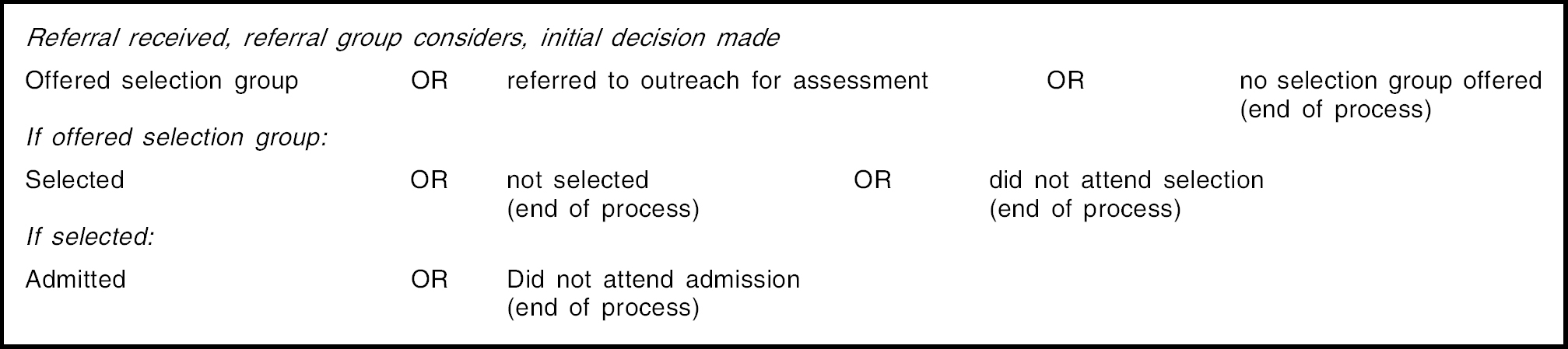
Figure 1: The referral pathway showing points of exit from the process
Sample
Consecutive referrals, selections and admissions between 1 April 1996 and 31 January 2000 (n=792) provided the sample for this study.
Data source
The data derive from the information supplied by the referrer on a standard form, the Referral Information Form, for each client. The form records 32 variables related to social, psychiatric and criminal histories, as well as psychological symptoms of the candidate. These variables are dichotomous and the referrer reports whether the variable is present or absent. The variables were as follows: depression; anxiety; panic; obsessions; deliberate self-harm; phobias; eating disorder; alcohol misuse; drug misuse; gambling; self-mutilation; attempted suicide; overdosing; mania/hypomania; delusions/hallucinations; violence to others; violence to property; firesetting; theft/shoplifting; physical abuse; sex (victim); sex (perpetrator); dissociation; physical illness; registered disabled; any psychiatric treatment; child therapy; ever convicted; on probation now; court case outstanding; taking medication. As can be seen, some of these variables overlap. This is a consequence of old and new forms being logged on the same database. In the cases where the category was no longer used, it was scored as missing.
Ethnicity data
The ethnicity information used in this study came from the Referral Information Form. The ethnicity categories were those routinely used by the hospital and recommended by the Department of Health at the time of the data collection. These were as follows: White, Black African, Black Caribbean, Black Other, Chinese, Asian Other, and Other Ethnic Group. It is to be assumed that those candidates described as ‘other ethnic group’ were not considered by their referrer to be suitably described by the other available categories.
As the form was completed by referrers, this information is their opinion of the client's ethnicity. There is no way to tell whether or not the referrers asked the client about their ethnicity. The ethnicity question was often not completed, and so there was a large amount of missing data (10%). Every effort was made to recover this data. After the search was completed, there remained 79 cases with missing ethnicity information. These cases were not included in the statistical analyses.
Data analysis
Data were analysed using the Statistical Package for the Social Sciences (SPSS) version 10 for Windows (Reference NorušisNorušis, 1988). T-test was used to analyse length of stay. Pearson's χ2 was used to analyse outcome at each stage of the referral process, and the relationship between ethnicity and clinical history. Thirty-two χ2 tests were carried out to see if there was any association between ethnicity and presence or absence of these histories. The Bonferroni correction (corrected critical value of P=0.00156) was used to correct for Type II error.
Results
A total of 792 referrals within the time period had been fully processed by the hospital. The proportion of referrals across ethnic groups is shown in Table 1. In 10% of cases, the referrer has not provided data to the hospital on the ethnicity of the client. Referrals were dichotomised into ‘White’ and ‘ethnic minorities’ because there were insufficient cases in sub-groups of ethnic minorities for statistical analysis. Seventy-four of the referred patients (9.3%) were from ethnic minorities.
Table 1. Ethnicity of referrals between 1 April 1996 and 31 January 2000
| Ethnicity | n | % |
|---|---|---|
| White | 639 | 80.7 |
| Ethnic minorities | 74 | 9.3 |
| Black African | 7 | 0.9 |
| Black Caribbean | 5 | 0.6 |
| Black Other | 2 | 0.3 |
| Chinese | 9 | 1.1 |
| Asian Other | 4 | 0.5 |
| Other Ethnic Group | 47 | 5.9 |
| Total | 713 | |
| Missing ethnicity data | 79 | 10 |
Stage one: the initial decision of the referral group
A selection group was offered to 501 candidates (Table 2). χ2 tests showed that proportionally, fewer of the ethnic minorities (n=44/74; 59.5%) were offered a selection interview than White candidates (n=457/639; 71.5%) by the referral group χ 2=4.389, df=1, P=0.036.
Table 2. The referral process with numbers of candidates by ethnicity at each stage
| The referral process | White | Ethnic minority | Total |
|---|---|---|---|
| Total candidates in time period | 639 | 74 | 713 |
| Stage one: the initial decision of the referrals group (candidates offered a selection group) | 457 | 44 | 501 |
| Stage two: selection groups held | 356 | 39 | 395 |
| Stage three: residential treatment | 211 | 26 | 237 |
Stage two: the selection group
Selection groups were held for 395 candidates. This figure comes from those selection groups that actually took place during the time period under study, rather than those that were offered. There was a non-significant trend for White candidates to be more likely to attend the selection group than ethnic minority candidates (n=356/639; 55.7%, v. n=39/74; 52.7%, χ2= 3.158, df=1, P=0.076, ns).
Stage three: residential treatment
Two hundred and thirty-seven candidates were admitted. Of these, 211 (89%) were White and 26 (10.9%) were from ethnic minority groups, showing that White candidates were in a numerical majority within the resident group. However, the likelihood of being admitted following referral was of a similar level across ethnicities (n=211/639; 33% v. n=26/74; 35%).
Length of stay varied widely for the whole group. For both the White and minority admissions, the shortest length of stay was one day. The longest length of stay for minority residents was 377 days and for White residents 379. No significant difference in length of stay was found between length of stay of White and ethnic minority residents (mean=149, s.d. 139.67 days v. mean=143, s.d. 140.17 days; t(235)=–0.196, P=0.844, ns).
Clinical and demographic factors
These 32 factors were examined to see if there was any association between ethnicity and previous symptomatic, psychiatric and criminal histories, as reported by the referring clinician. A corrected critical value of P=0.00156 was found. Using this value, no significant associations were found. Prior to the Bonferroni correction, three associations were found to be significant at the P=0.05 level. These cannot be viewed as significant as they do not meet the corrected P value, but they are of interest as possible underlying trends. Ethnic minorities were more likely to have had eating disorders (χ2=5.421, df=1, P=0.020, ns), were more likely to have misused drugs (χ2=5.519, df=P=0.019, ns) and were more likely to have had a history of gambling (χ2=7.503, df=1, P=0.006, ns).
Discussion
Although falling short of the ideal 14%, the increase in ethnic minority referrals in the past 10 years from 2-9% indicates a positive trend. Ethnic minority referrals have increased by a factor of 5 (2% to 9.3%), while admissions have increased by a factor of 2 (5% to 11%). A number of interventions have been introduced by the staff team since the 1991 study to try and increase the number of referrals from minority ethnic groups and to raise awareness of issues to do with culture and ethnicity in the therapeutic community. Active measures were taken to recruit more staff from minority ethnic groups, resulting in a more culturally diverse staff group. It is likely that all these factors have had an effect and that Henderson Hospital has been more widely recognised as a suitable treatment for ethnic minority clients.
Being in an ethnic minority was significantly associated with rejection by the referral group, the first stage of the referral process. Two possible explanations for this were that the referral group was rejecting ethnic minority candidates because of their ethnicity, or there were other variables incidentally related to these candidates that led to the rejection, such as more severe clinical presentation. The majority of referrals were excluded automatically according to criteria of suitability, indicating that ethnicity per se was not a factor. However, a possible confounder is that one of Henderson Hospital's exclusion criteria is psychotic illness, which has been established to be diagnosed more frequently in non-white psychiatric patients.
Ethnic minority referrals tended to have more severe clinical factors (eating disorder, gambling, drug misuse). The rejection at stage one could be because ethnic minority referrals are more severely disturbed by the time they get referred for specialist treatment. Given the small sample of ethnic minority referrals, it is not possible to rely on these data, but further exploration of these issues is indicated by the non-significant trends.
An important finding is that the length of stay at Henderson Hospital is unrelated to ethnicity. The Henderson Hospital staff team's perception that being in an ethnic minority would be a risk for early drop out (Reference BlountBlount, 2001) was not borne out by the results. In addition, this would suggest that the treatment is as suitable for those referrals from White and non-White groups.
Limitations
The principal drawbacks of this study were the amount of missing data, the reliance of ethnicity information supplied by the referrer rather than the client and the small sample of non-white referrals. The small sample sizes are inherent in this kind of work, however, given the small number of clients from ethnic minority backgrounds who are referred to tertiary psychotherapy. It is also difficult to assess the importance of any changes over time in referral rates to specialist services without knowledge of changes in the base rates within the population from which referrals come. The methodology, and any future exploration of cultural issues in this context may be improved by the addition of a qualitative approach to assessment of the cultural relevance of this treatment approach, including an exploration of the experiences of this treatment of clients from ethnic minority groups.
Conclusion
Despite the low numbers of ethnic minorities involved, this study suggests that, once offered selection, ethnic minority referrals are no more nor less likely than White referrals to be selected, admitted, or stay longer.
Clinical and research implications
This study suggests that ethnic minority clients may not be referred for specialist treatment until they have more severe difficulties than their White counterparts. Further research with larger sample sizes and including a range of psychotherapy services should be conducted to explore this finding and the reasons for it. The study also suggests that therapeutic community treatment is appropriate for clients from minority backgrounds, and that they are as likely to be admitted and remain in treatment as long as White clients.
Declaration of interest
None.
Acknowledgements
Thanks are due to the Ethnicity Working Group at Henderson Hospital for help and advice, and especially to Kirstin Hubert and Sajdah Zaman. We would also like to thank the Personality Disorder Theme research group at St George's Hospital Medical School for comments and suggestions during the data analysis stage, and Diana Menzies for comments on the final drafts.






eLetters
No eLetters have been published for this article.