Disasters (man-made, natural disasters, and climate change) are unpredictable situations, that lead to damage, destruction of local capacities, and great human suffering. It affects local capacities and creates the need to use foreign aid at the national or international level. Reference Azizpour, Mehri and Soola1,Reference Babaie, Barati and Azizi2 According to the Center for Research on the Epidemiology of Natural Disasters in 2019, there were 396 natural disasters with 11,755 victims and 130 billion dollars in financial losses. 3 Iran is 1 of the world’s 10 most vulnerable countries; almost 90% of its population is exposed to natural disasters. 3 During the past 100 y, Iran has spent approximately 29 billion dollars on disasters. Reference Seddighi and Seddighi4
Disasters leave various destructive damage on the health of survivors. In the first 24 h after a disaster, 85 to 95% of survivors need the most care. Reference Bazyar, Pourvakhshoori and Safarpour5 In addition to physical injuries, victims suffer from psychological injuries with a high prevalence. Reference Makwana6 Feelings of insecurity, death of loved ones, socio-economic loss, environmental destruction, mental unpreparedness for disasters, lack of social support, and negative coping skills make disaster victims psychologically vulnerable. Reference Makwana6,Reference Alizadeh, Khankeh and Barati7 However, psychological injuries are often neglected and receive limited attention in disaster management plans. Reference Sheek-Hussein, Abu-Zidan and Stip8,Reference Azizi, Ebadi and Ostadtaghizadeh9 Paying attention to psychological effects should be considered in all aspects of disaster management, including preparedness, mitigation, response, and recovery. Reference Sheek-Hussein, Abu-Zidan and Stip8,Reference Delshad, Stueck and Ebadi10
In this regard, nurses, as the largest group of health-care providers, are among the first responders in disasters. Reference Littleton-Kearney and Slepski11 Meanwhile, nurses play a privileged and unique role in providing humanitarian aid. Reference Menegat and Witt12 Establishing effective and empathetic communication is one of the important factors in improving the mental condition of the victims. Reference Nam and Park13 Empathy means a person’s ability to understand and experience the private world of another person as if that other person’s world were their own. Reference Van Dijke, van Nistelrooij and Bos14 This concept has 2 cognitive and emotional dimensions. Cognitive empathy means understanding the feelings of others, and emotional empathy means communicating emotionally with others and sharing in their emotional states. Reference Kheradmand, Jalal and Shamsesfandabad15 Empathy is a factor in improving the quality of nursing care. Reference Mottaghi, Poursheikhali and L.16 Especially in connection with mental patients, it leads to the creation of an effective therapeutic atmosphere, Reference Yu and Kirk17 promoting a sense of value in patients, Reference Moreno-Poyato and Rodríguez-Nogueira18 and increasing trust and cooperation in patients and the quality of the information provided by them. Lack of empathy leads to fear and helplessness of the patients. Reference Minas, Zamzam and Midin19
Although empathy is one of the important implementations of providing psychological care to people in crisis, this issue is sometimes forgotten. A large number of clients, lack of time, focus on treatment, academic medical culture, and insufficient training in empathy can be the causes of this neglect. Reference Hojat, Louis and Maio20 Also, too much empathy has negative effects on the caregiver, such as anxiety, depression, and compassion fatigue. Therefore, training caregivers in providing controlled empathic care appears essential. In this regard, the standard and universal protocol of psychological first-aid (PFA) in crisis is a guide developed by the World Health Organization, 21 and allows caregivers to establish a controlled empathic relationship with victims and leads to their recovery from the psychological distress of disasters. Reference Zafar, Naeem and Zehra22 During this relationship, victims are helped in a nonaggressive manner, leading to a sense of security and peace, Reference Azzollini, Depaula and Cosentino23 positive adaptation, and resilience. Reference Ramirez, Harland and Frederick24,Reference Khankeh, Alizadeh and Nouri25
Therefore, it is very important to increase the competence of nurses in providing PFA during a disaster. Reference Azizi, Bidaki and Ebadi26 Competence consists of the dimensions of knowledge, skill, attitude, mission commitment, leadership, management ability self-identity of dual roles (such as obedience, empathy, etc), Reference Ma, Lin and Zhang27,Reference Farsi and Rajai28 critical thinking, innovation, and personality traits appropriate to the work field. Reference Chen, Zhang and Li29 No study was found that investigated the level of competence of nurses in providing PFA. But some studies show unfavorable levels of general competence of nurses in the crisis. Reference Latif, Abbasi and Momenian30,Reference Achora and Kamanyire31
Also, in the care management of victims in disasters, physical support is given priority, and often psychological support is neglected or limited, and nonspecialized support is provided. Reference Ingram, Tinago and Cai32
Disasters like the coronavirus disease 2019 (COVID-19) pandemic have created rapid and dramatic changes in all aspects of people’s lives worldwide. Reference Schoultz, McGrogan and Beattie33 Education has also been affected by these pandemic conditions. Nowadays, evidence showed that distance learning such as E-learning (Web-based technologies) and mobile-based education with features such as increasing the quality of learning, ease of access to a large volume of information, and reduction of educational costs are being replaced by traditional teaching methods. Reference Pour, Aliyari and Farsi34
So, this study aimed to investigate the effectiveness of PFA E-learning on the competence and empathy of nurses in disasters. Based on the out search, we did not find any study with this characteristic. In this study, the question will be answered can the E-learning of PFA lead to increasing the competence and empathy of nurses?
Methods
Study Design and Setting
This randomized controlled trial study with pre- and-post-intervention design was conducted on nurses working in 2 hospitals in Isfahan and Tehran, Iran, in December to November 2022. It has been approved by the Iranian Registry of Clinical Trials on 2023-01-31 (ID: IRCT20220923056023N1).
Sample Size and Sampling
The sample size was estimated based on finding the study of Laktarash et al. Reference Laktarash, Kalroozi and Pishgooie35 and the formula suggested for comparing 2 means, an optimal sample size of 23 patients per group was estimated, considering type I error of 5% (α = 0.95) and the power of the test equivalent to 80% (β = 0.2). However, considering the 10% sample attrition, 26 nurses were recruited in each group (Figure 1).
 $$\begin{gathered}n = \frac{{{{\left( {{{\text{Z}}_{1 - \frac{\alpha }{2}}} + {{\text{Z}}_{1 - \beta }}} \right)}^2}\left( {\delta {1^2} + \delta {2^2}} \right)}}{{{{\left( {{\mu _1} - {\mu _2}} \right)}^2}}} \\ \,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\, = \frac{{{{\left( {1.96 + 0.84} \right)}^2}\left( {{{\left( {7.06} \right)}^2} + {{\left( {8.97} \right)}^2}} \right)}}{{{{\left( {66.13 - 59.5} \right)}^2}}} = 23.24 = 23 \\ \end{gathered}$$
$$\begin{gathered}n = \frac{{{{\left( {{{\text{Z}}_{1 - \frac{\alpha }{2}}} + {{\text{Z}}_{1 - \beta }}} \right)}^2}\left( {\delta {1^2} + \delta {2^2}} \right)}}{{{{\left( {{\mu _1} - {\mu _2}} \right)}^2}}} \\ \,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\,\, = \frac{{{{\left( {1.96 + 0.84} \right)}^2}\left( {{{\left( {7.06} \right)}^2} + {{\left( {8.97} \right)}^2}} \right)}}{{{{\left( {66.13 - 59.5} \right)}^2}}} = 23.24 = 23 \\ \end{gathered}$$
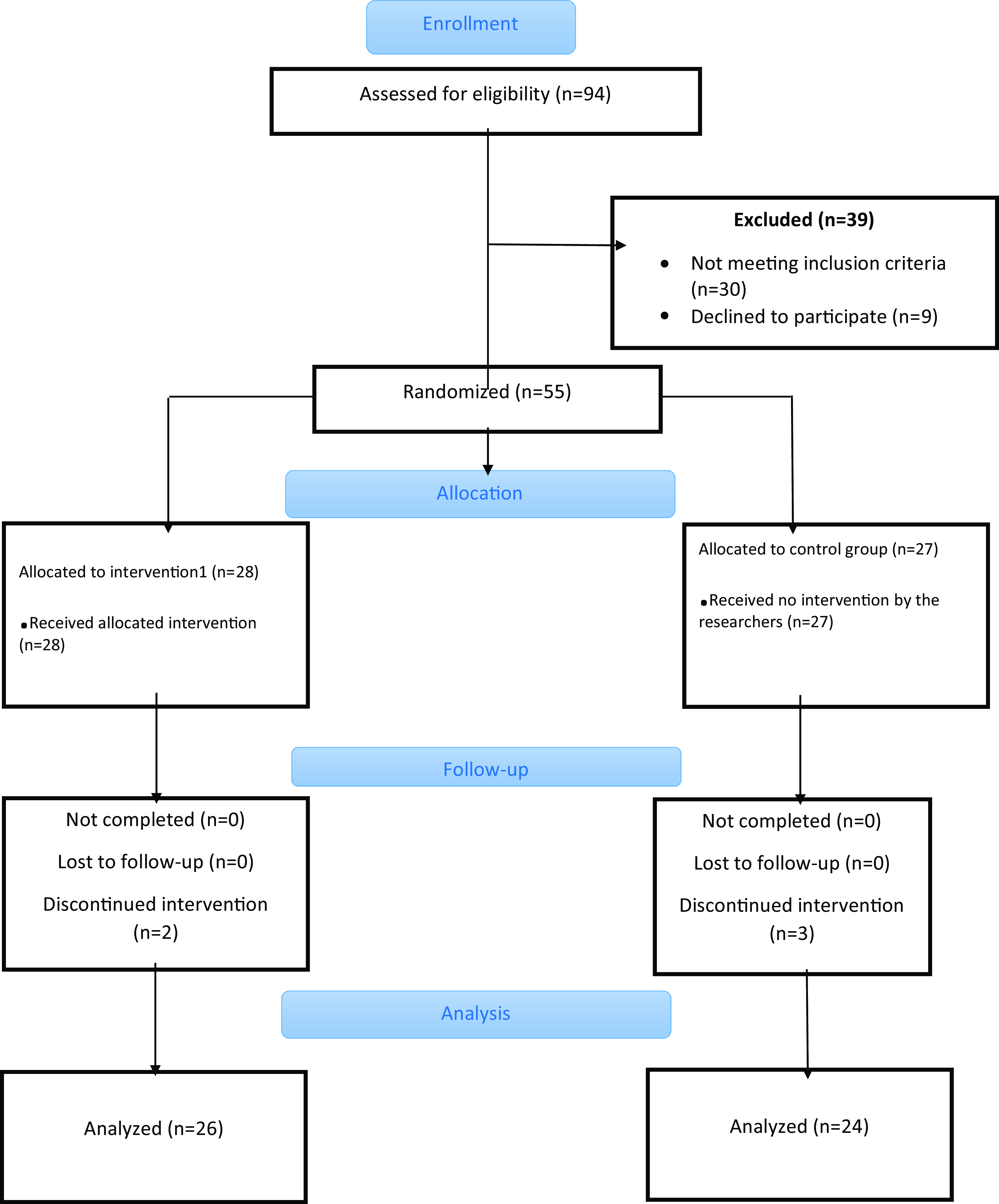
Figure 1. The study process.
The inclusion criteria included: having a bachelor’s degree in nursing or higher, working in one of the departments of hospitals, not participating in preparation courses to deal with crises, and having E-learning devices (such as smartphones, tablets, laptops, etc.) to participate in the E-learning course. The exclusion criteria included: failure to participate in more than 1 session of the E-learning course (4 E-sessions), unwillingness to continue cooperation, and incomplete completion of questionnaires.
First, 94 nurses were recruited by the convenience sampling method. Then, 39 were excluded from the study because they did not meet the inclusion criteria (n = 30) and declined to participate (n = 9). Fifty-five of them were randomly divided into the intervention group (n = 28) and the control group (n = 27) by coin toss. Finally, 26 nurses participated in the intervention group and 24 nurses participated in the control group. There was approximately 9% attrition in the study.
Measurement
Three tools were used in this study:
1. The individual characteristics questionnaire consisted of the following variables: age, sex, place of work, and history of exposure to disasters.
2. To investigate the competence of nurses in providing PFA in disasters, a questionnaire was designed and psychometrically evaluated by the researchers. In the beginning, 37 items were extracted based on different articles and texts and the experiences of a supervisor of study with a specialization in psychiatric nursing, and a PhD in health in disaster and emergency. The content of the questionnaire items consisted of self-care, critical thinking, communication skills, knowledge, attitude, and performance regarding PFA in disasters. To check the face validity, the questionnaire was given to 3 nurses to check the writing points, difficulty, appropriateness, and ambiguity of the items. To check the quantitative face validity, the Item Impact Score was checked. Thus, the questionnaire was given to 13 expert psychologists to determine the suitability of the items. The formula (Item Impact Score = Frequency (%) × Suitable) was used, and a score above 1.5 was considered to retain the items. Reference Keysers, Schärli and Scales36 All the items of this questionnaire were kept according to the formula.
3. Interpersonal Reactivity Index (Davis 1983); This questionnaire consists of 3 dimensions, including empathic concern, perspective-taking, and empathic distress. The perspective-taking measures the reported tendency to spontaneously adopt the psychological point of view of others in everyday life (“I sometimes try to understand my friends better by imagining how things look from their perspective”). The empathic concern assesses the tendency to experience feelings of sympathy and compassion for unfortunate others (“I often have tender, concerned feelings for people less fortunate than me”). Personal distress taps the tendency to experience distress and discomfort in response to extreme distress in others (“When I see someone who badly needs help in an emergency, I go to pieces.”). The items of each dimension are an empathic concern (items of 1, 4, 7, 10, 14, 17, 18), perspective-taking (items of 2, 5, 9, 12, 16, 19, 21), and personal distress (items of 3, 6, 8, 11, 13, 15, 20). The scoring is based on a 5-point Likert scale and is graded from completely agree (5) to completely disagree (1). Items 2, 4, 10, 11, 12, 14, and 15 are scored in reverse. The minimum possible score will be 12 and the maximum score will be 60. Davis calculated the reliability coefficient by the test-retest method and reported between 0.62 and 0.80. Cronbach’s alpha coefficient was also reported between 0.71 and 0.77 for each dimension of questionnaire, Reference Davis37 Also, the total reliability of the Empathy scale was estimated in Iran (0.75). Reference Baghbanpour Azari and Hosseini Nasab38
To check the content validity of the questionnaire, 13 experts were asked to answer each of the items to find out: necessary, useful but not necessary, and not necessary. The formula of Content Validity Ratio (CVR) was used.
In this formula, nE is the number of experts who considered the item necessary and N is the total number of experts who checked an item. Then, the value obtained in this formula is compared with the values of CVR in Lavshe’s table. If this value were greater than the number in the Lavshe table, the item was kept. To determine the content validity index (CVI), the experts will be asked to check the items according to the Likert scale (not related, somewhat related, related, and completely related) and then calculated using the formula (The number of experts who gave a higher score to the item (3 and 4)/the total number of experts). In case of getting a score above 0.8, the item was kept at. Reference Ebadi, Zarshenas and Rakhshan39
Finally, 24 items were retained. To check the reliability, a questionnaire was given to 30 nurses. Cronbach’s alpha coefficient was calculated to check the internal consistency of the scale at 0.789. Also, the internal correlation of the questionnaire was checked with the method of split-half (odd and even items) and the value was 0.813.
Intervention and Data Collection
The educational content was used for training based on the principles of PFA and the instructions issued by the Ministry of Health and Medical Education of Iran and with the approval of the professors of the Department of Psychiatry and Psychology (Table 1). First, a face-to-face training session was held to introduce the research and its objectives for the nurses of both intervention and control groups. In this meeting, the desired questionnaire was given to 2 groups to fill out. Then, for the intervention group, four 1-h E-learning sessions were held on the sky room platform for a period of 4 wk (1 training session per wk). Reference Fox, Burkle and Bass40
Table 1. Training sessions for the intervention group
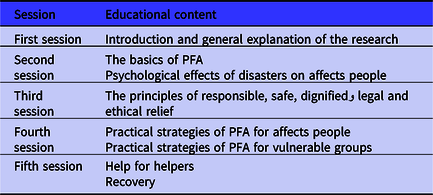
Abbreviation: PFA, Psychological psychological first first-aid.
Also, a group was formed in a virtual network (WhatsAp,p which was practical and popular in Iran), and the nurses of the intervention group became members of this group. In this group, the exchange of information. Recorded training session videos with PowerPoints were put in the WhatsApp group. Also, the possibility of asking questions about ambiguities was provided. To encourage nurses to participate in this study, the Internet fee was considered for them to participate in E-learning sessions (according to their mobile number). After the training sessions, the questionnaires were sent electronically to the nurses of the intervention group to fill out. In the control group, no training took place. The interval between preintervention and the postintervention control group was 4 wk.
Statistical Analyses
SPSS version 16 software was used for data analysis. Kolmogorov-Smirnov Test was used to check the normality of the data in each group. Fisher’s exact test, chi-squared, and independent t-test were used to check the homogeneity of the 2 groups in terms of individual characteristics. Paired t-tests were used to compare the mean score of nurses’ competence and empathy before and after the intervention in each group. Also, a dependent t-test was used to compare the mean score of nurses’ empathy and competence in both groups. P < 0.05 was considered a significant level. The statistical analyst was blinded to the allocation of nurses to 2 groups.
Ethical Considerations
The Ethics Committee of Aja University of Medical Sciences, Tehran, Iran (No.IR.AJAUMS.REC.1401.092) approved this study. Written informed consent was obtained from all nurses. Participation in the study was completely optional for nurses and they could withdraw from the study whenever they wanted. After completing the study, the E-learning content was also given to the control group. All the principles of the Declaration of Helsinki were observed.
Results
Two groups were homogenous in terms of age, sex, place of work, and history of exposure to disasters (P > 0.05) (Table 2). Two groups were homogeneous regarding the competency of nurses in PFA before the intervention (P > 0.05). The paired t-test showed that the intervention group had more competence in the post intervention rather than before the intervention (P < 0.0001). On the other hand, in the control group, the competence of nurses in the post-intervention phase was reduced compared with before the intervention (P = 0.02). Also, in the postintervention phase, the intevention group had more competence compared with the control group (P < 0.0001) (Table 3). Based on Cohen’s method, the overall effect size of PFA E-learning training on the nurses’ competency was 1.9.
Table 2. Comparison of individual characteristics of nurses in the intervention and control groups
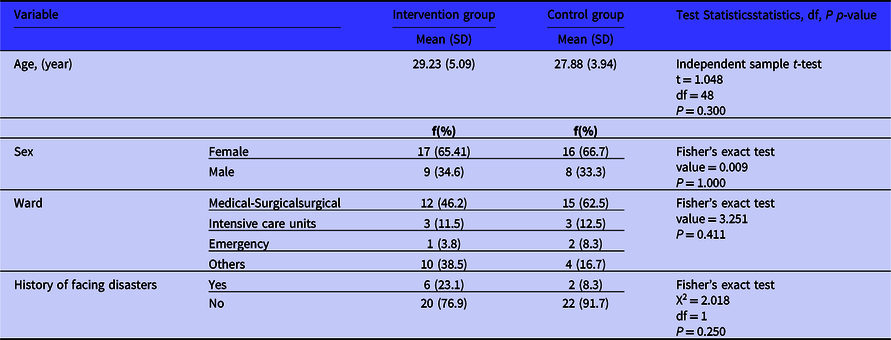
Abbreviations: df, degrees of freedom; f, frequency; SD, standard deviation.
Table 3. Comparison of the mean score of psychological first aid competency in the nurses in the intervention and control groups
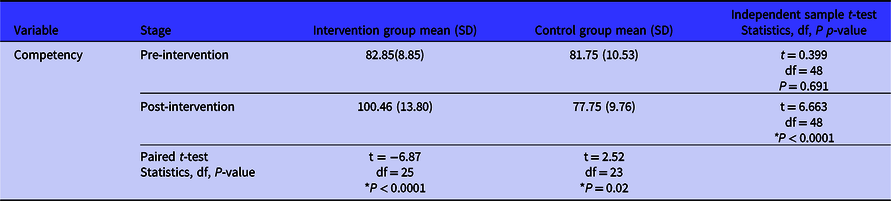
Abbreviations: df, degrees of freedom; SD, standard deviation.
*P < 0.05
Regarding the variable of empathy in PFA, in the pre-intervention phase, the studied groups were homogeneous (P > 0.05). The results of the paired t-test showed that the intervention group did not have more empathy in the later stage than before the intervention (P = 0.727). On the other hand, in the control group, there was no significant difference in nurses’ empathy in the postintervention phase compared with the preintervention phase (P = 0.367). In the postintervention phase, the intervention group did not have more empathy than the control group, which was not statistically significant (P=0.132) (Table 4). Based on Cohen’s method, the overall effect size of PFA E-learning training on the nurses’ empathy was 0.44.
Table 4. Comparison of the mean scores of empathy dimensions of nurses in the intervention and control groups

Abbreviations: df, degrees of freedom; SD, standard deviation.
* P < 0.05.
Discussion
In this study, the effect of E-learning on the competence and empathy of nurses in providing PFA in disasters was investigated. The 2 intervention and control groups were homogeneous in terms of individual characteristics, competency, and empathy before the intervention.
The results showed that E-learning significantly increases the competence of nurses in providing PFA. In this regard, a recent systematic review and meta-analysis study showed that the competency-based educational model increased the competence of new nurses in China. In this model, the dimensions of competence were critical thinking, innovation, interpersonal communication, professional construction and development, comprehensive knowledge, and good personal traits. Reference Chen, Zhang and Li29 Traditional training of nursing students often focuses on increasing knowledge and skills. Reference Jahanpeyma, Sajadi and Rajai41 This is why failure to pay attention to improving the dimensions of competence in the profession leads to emotional damage to the individual and a decrease in the quality of care. Reference Essenmacher, Baird and Houfek42
In past studies, the effect of training on the competence of nurses in providing PFA in disaster has not been investigated. However, supportive studies were found regarding the effect of PFA training on different dimensions of learning. For example, in the study of Sijbrandij et al., 1-day face-to-face PFA training on 202 health-care workers in post-Ebola Sierra Leone promoted knowledge and understanding of responses and appropriate psychosocial skills in providing psychological support to people exposed to acute adversity. Reference Sijbrandij, Horn and Esliker43 Also, in the study of Said et al., PFA training improved nurses’ preparedness (knowledge, skills, optimism, self-esteem, and self-efficacy) during and after emergencies and disasters. Reference Said, Molassiotis and Chiang44
In this study, PFA training had an effect on 2 dimensions of empathy (reduction of personal distress and increase of perspective-taking). Perspective-taking is a kind of cognitive empathy and measures a person’s efforts to see things from their point of view. Personal distress is a type of emotional empathy that shows the feeling of anxiety and discomfort caused by observing the negative experience of others. Reference Rohani and Mohtashami45 In support of the findings of this study, previous studies investigated the impact of educational interventions on empathy in medical and nursing students and showed the positive effects of education on this concept. Reference Tafazoli, Ezzati and Mazloom46–Reference Ferri, Rovesti and Padula48
The findings showed that training did not affect the total score of empathy and the dimension of empathic concern. In this study, the empathy score was checked immediately after the completion of the training sessions. Maybe if an opportunity were given to practice and the empathy score was checked again after some time, some effects would have been shown. Another point, in this case, is that perhaps it would have been better to measure nurses’ empathetic behaviors in a real disaster situation or in a simulated situation. In this regard, Tafazoli et al. investigated the effect of training on the empathy of midwifery students in dealing with pregnant women. To check the effect of the training, the time of the postintervention was considered 1 wk after the intervention, and the tests were done in a real situation (pregnant women referring to the midwifery clinic), and positive results were also reported. Reference Tafazoli, Ezzati and Mazloom46
In general, E-learning was effective on nurses’ competence and empathy in this study, which was very large for the competence component and small for the empathy component. Recently, the desire to use E-learning, especially in continuing nursing education program, has increased. Reference Lawn, Zhi and Morello49 The effectiveness of this learning method is equal or greater in most cases compared with the traditional method. For example, in a study of 93 Japanese nurses, there was no significant difference between traditional and E-learning. Reference Horiuchi, Yaju and Koyo50 Another study found encouraging student performance and employee perceptions of demonstrably improved technical skills. These findings further support changes in future implementations of online medical courses. Reference Elzainy, El Sadik and Al Abdulmonem51 The reason for the effectiveness of this training method can be the elimination of the location dimension, flexibility in training time, cost-effectiveness, less absence in meetings, self-management training in independent people, increasing self-confidence in people due to anonymity, and more participation in discussions. Reference Glogowska, Young and Lockyer52
Limitations
This study had some limitations. Due to the low speed of the Internet, participants were facing problems accessing the educational files, which of course was solved by the efforts of the researcher. Also, due to the limited access to nurses and their very busy schedules, the duration of the intervention and follow-up of the effects of PFA training was considered short. The small sample size was another limitation of the study due to the COVID-19 pandemic, so a study with a larger sample size is suggested.
Conclusions
The results of this study showed the significant effect of PFA E-learning on competence and its limited effect on empathy and its components. It is recommended that future studies investigate the effects of PFA on psychosocial outcomes for disaster-affected people. Considering the importance of psychosocial support in disaster survivors and the effectiveness of this educational intervention, it is suggested that the policymakers include PFA training in the curriculum of rescuers and nursing students, especially the students studying in the specialized field of disasters.
Acknowledgments
We thank all the nurses who participated in this study.
Author contributions
M.A., S.M.S.M., Z.F., A.A., and A.B. designed the study. M.A., A.B., and S.M.S.M. conducted the training sessions. Z.F. and A.A. performed the data analysis and interpreted the data. M.A. and N.R. drafted the manuscript. All authors read and approved the final manuscript before submission.
Funding
Aja University of Medical Sciences, Tehran, Iran on the date (2022.03.14), under project code (97002082).
Competing interests
The authors declare that they have no conflict of interest.
Ethical standards
This study was approved by the Institutional Review Board and Ethics Committee of Aja University of Medical Sciences, Tehran, Iran (No.IR.AJAUMS.REC.1401.092).







