Introduction
Mucous retention cysts are a common incidental finding in the maxillary sinus.Reference Becker, Larson, Duncavage and Becker1 They are products of obstructed submucosal mucinous glands.Reference Becker, Larson, Duncavage and Becker1 Their ovoid and non-gravity-dependent shape is clearly recognisable on computed tomography (CT), especially on coronal imaging.Reference Becker, Larson, Duncavage and Becker1 However, in most cases, the cysts are asymptomatic, except in cases where they impact on sinus drainage patterns.Reference Becker, Larson, Duncavage and Becker1 Therefore, mucous retention cysts of the maxillary sinus are not always an indication for functional endoscopic sinus surgery (FESS).
Mucous retention cyst is the commonly used name for this disease. However, from our experience, the fluid contained in the cyst is not mucous but serous. The cysts include both true cysts lined by epithelium and pseudocysts not lined by epithelium. Hence, the authors use the term ‘retention cyst’ in this study.
Maxillary dental infections can cause sinusitis; this pathophysiological condition is called odontogenic maxillary sinusitis. Dental diseases with endodontic or periodontic lesions of the maxilla accompanied by unilateral opacification of the maxillary sinus are common types of odontogenic maxillary sinusitis.Reference Sato2–Reference Sato, Chitose, Sato, Sato, Ono and Umeno7
Other atypical pathophysiological conditions of odontogenic maxillary sinusitis caused by odontogenic infections precipitated by the maxilla or maxillary sinus lesionsReference Sato8,Reference Sato9 are not well known. There are two types of maxillary sinus lesions: acute maxillary sinusitis and retention cysts. There are also two types of maxilla lesions: post-operative maxillary cysts and odontogenic cysts.Reference Sato8,Reference Sato9
Usually, as retention cysts of the maxillary sinus are asymptomatic and detected incidentally on X-ray examinations, they are not always an indication for FESS. Hence, there is no consensus regarding the management of retention cysts of the maxillary sinus, especially the optimal timing of FESS.
This study aimed to investigate the pathophysiology of odontogenic infections precipitated by retention cysts of the maxillary sinus and consider the optimal timing of FESS.
Materials and methods
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guidelines on human experimentation by the Ethics Committee of Kurume University (permission number: 21189), and with the Helsinki Declaration of 1975, as revised in 2008.
Five adults (three males and two females), ranging in age from 42 to 51 years (mean ± standard deviation, 46 ± 3.4 years), who underwent FESS for odontogenic infections precipitated by retention cysts of the maxillary sinus, were retrospectively examined.
Diagnosis of odontogenic infections precipitated by maxillary sinus retention cysts
Regarding the diagnosis of odontogenic infections precipitated by retention cysts of the maxillary sinus, evaluation of all patients with retention cysts of the maxillary sinus included inspection of the maxillary teeth with a cone-beam CT scan. Furthermore, the relationships between the retention cysts and apex of the teeth were observed using a cone-beam CT scan, to obtain an accurate diagnosis. All retention cysts occurred on a mucosal surface of the maxillary sinus floor (Figure 1). In all patients, the natural ostium of the maxillary sinus was open, and ventilation and drainage of the maxillary sinus seemed to be fine. There was no maxillary sinusitis.
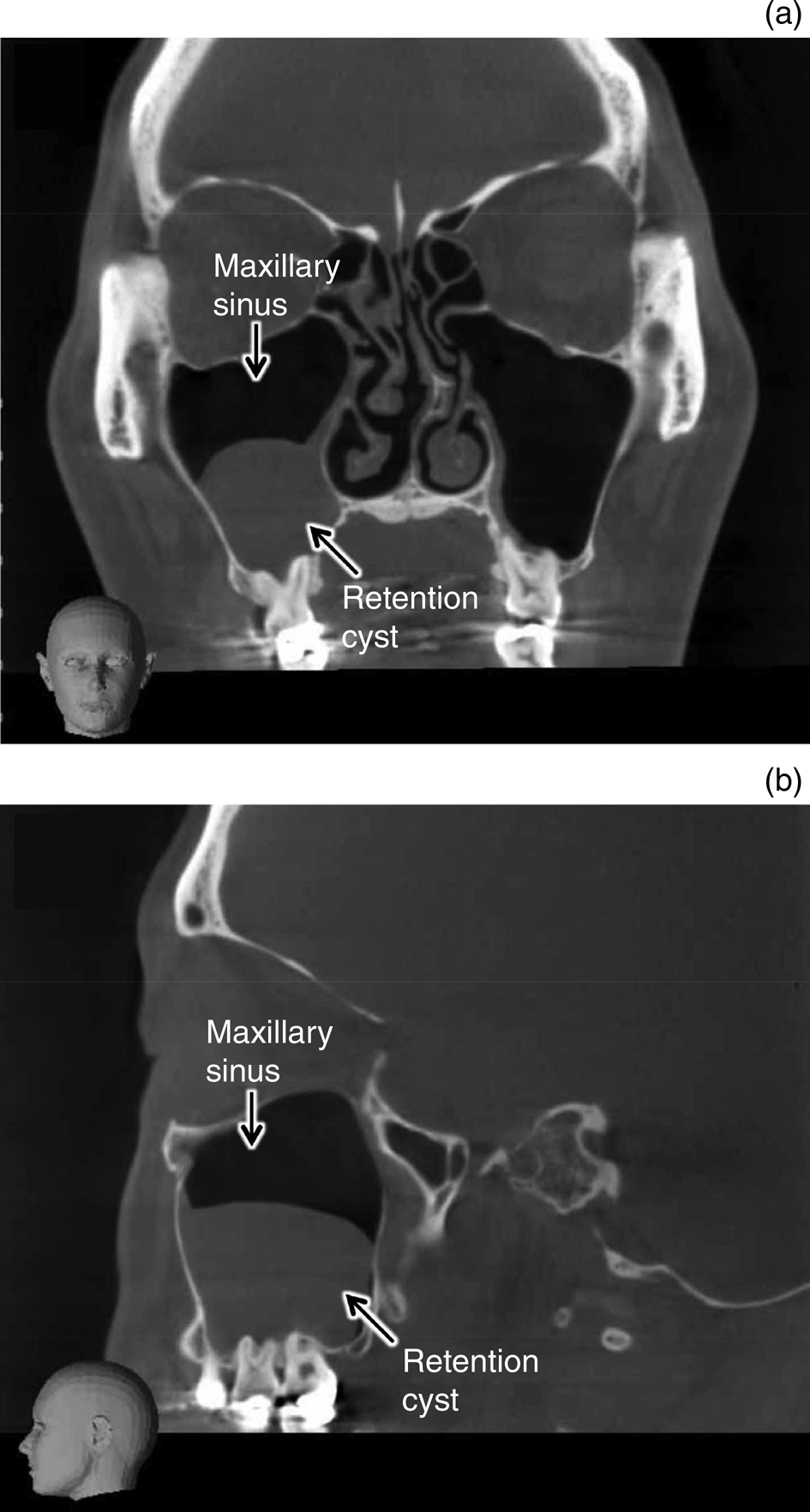
Fig. 1. (a) Coronal and (b) sagittal multiplanar reconstructions of cone-beam computed tomography (CT) scans of a maxillary sinus retention cyst. Ovoid opacification in the right maxillary sinus was clearly recognised on CT. A retention cyst occurred on a mucosal surface of the right maxillary sinus floor. Root apexes of molars protruded into the maxillary sinus. Although dental restoration had been performed, there were no lesions in the tooth crown, tooth root or periodontal tissue.
In all patients, dental symptoms outweighed sinus symptoms, with patients having no sinus complaints. The symptoms of odontogenic infections precipitated by the retention cysts were unilateral, and consistent with facial pressure and cheek pain. In addition, the patients had percussion pain, indicating they had periodontitis and pulpitis around the root apex. The teeth with odontogenic infections were vital teeth. There were no lesions of the tooth crown (except dental restoration), tooth root or periodontal tissue.
Early surgical intervention was performed only when the retention cyst had caused periodontitis and pulpitis of the root apex and it was progressing to ascending pulpitis and pulpal necrosis.
Sinus surgery and post-operative treatment
The FESS was performed as a first-line therapy for these cases. The FESS was used to enlarge the natural ostium and membranous portion of the maxillary sinus, and widely open the ostiomeatal complex (Figure 2a). The upper three-quarters portion of the retention cysts were removed; the lower one-quarter portion of the cyst wall attached to the floor of the maxillary sinus and root apex were left intact under nasal endoscopy, to avoid injury to the apical foramen and dental nerve (Figures 2b and 3). In all patients, the fluid contained in the retention cyst was not mucous but serous.

Fig. 2. Functional endoscopic sinus surgery (FESS) performed for maxillary sinus retention cyst. (a) Endoscopic view of the right maxillary sinus (70-degree rigid endoscopic view) obtained during FESS. A retention cyst was observed on a mucosal surface of the right maxillary sinus floor (arrows). (b) Endoscopic surgical procedure for maxillary sinus retention cyst. The upper three-quarters portion of the retention cyst was removed; however, the cyst wall attached to the maxillary sinus floor and root apex were left intact under nasal endoscopy.
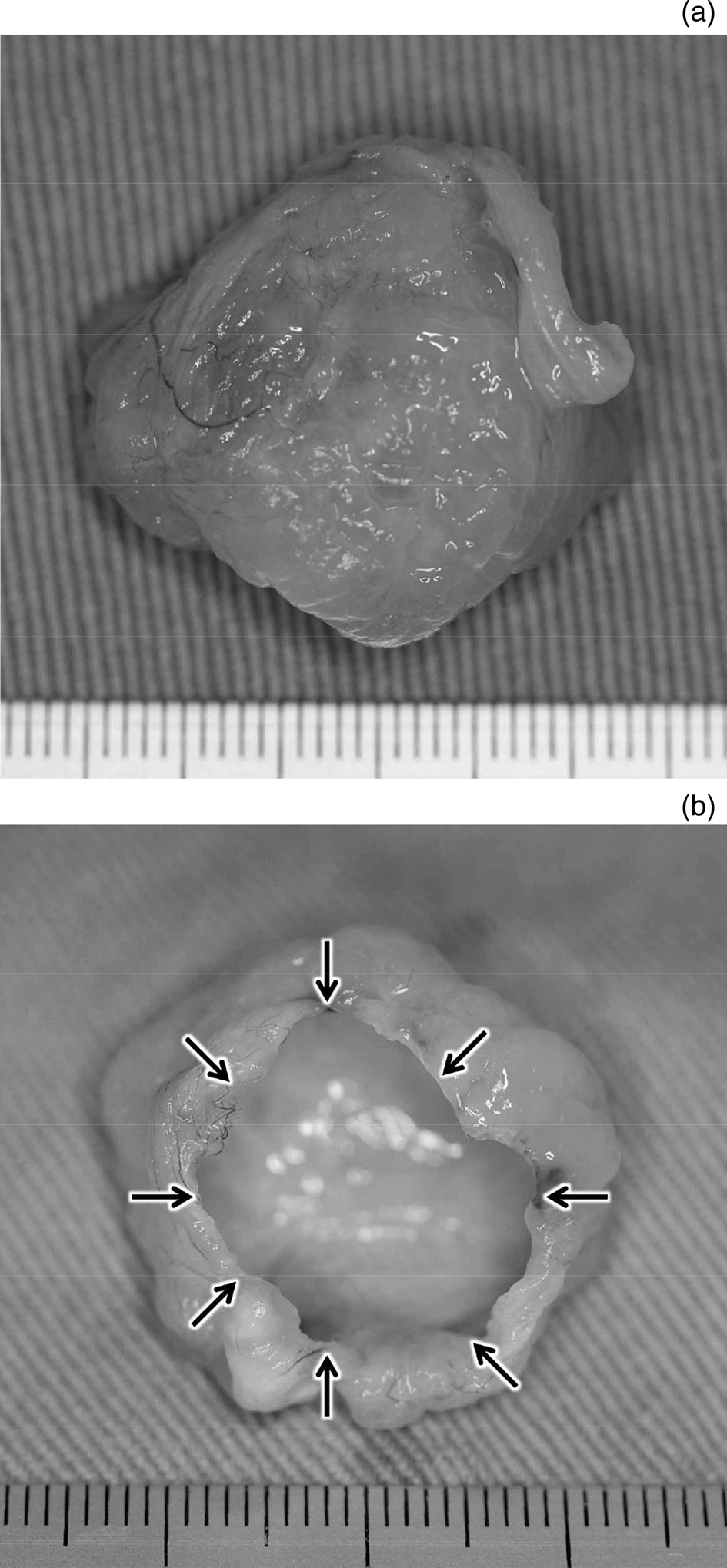
Fig. 3. Views of a removed maxillary sinus retention cyst (fixed in 10 per cent formalin): (a) from above and (b) from below. The lower one-quarter portion of the retention cyst was not removed (arrows). The cyst wall attached to the maxillary sinus floor and root apex were left intact.
After FESS, antibiotic administration without dental treatment was performed for the odontogenic infections precipitated by the retention cysts of the maxillary sinus.
Assessment of sinus surgery outcomes
Surgical outcomes of retention cysts were assessed on nasal endoscopy or by cone-beam CT scans.
Results
Aetiology of odontogenic infections precipitated by maxillary sinus retention cysts
The clinical symptoms of odontogenic infections precipitated by retention cysts of the maxillary sinus were persistent facial pressure and cheek pain, although there were no lesions in the tooth crown (except dental restoration), tooth root or periodontal tissue.
All of the retention cysts occurred on a mucosal surface of the maxillary sinus floor (Figure 1). Root apexes of all teeth that had odontogenic infection protruded into the maxillary sinus (Figure 1).
All teeth with odontogenic infections precipitated by the retention cysts were molars and had percussion pain, indicating they had periodontitis and pulpitis around the root apex. They were vital teeth, indicating they did not have pulp necrosis.
Sinus surgery outcomes
On post-operative nasal endoscopy and cone-beam CT scans, the natural ostiums and the membranous portions of the maxillary sinuses were enlarged, and the ostiomeatal complexes remained widely open. The ventilation and drainage of maxillary sinuses seemed to be successfully restored during the follow-up period (one to two years). The small area of cyst wall attached to the floor of the maxillary sinus and root apex were left intact during FESS; however, no recurrence of the retention cyst was detected on nasal endoscopy or on the cone-beam CT scans.
Outcomes of teeth with odontogenic infections precipitated by maxillary sinus retention cysts
Persistent facial pressure and cheek pain improved in all patients. The teeth that had odontogenic infections precipitated by the retention cysts of the maxillary sinus continued to be vital, with no symptoms. This indicates how important it is to perform FESS before the periodontitis and pulpitis of the root apex caused by the retention cyst progress to ascending pulpitis and pulp necrosis. In other words, FESS should be performed while the affected teeth are still vital.
Discussion
Retention cysts are a common disease in the maxillary sinus and are observed incidentally on X-ray examination. In most cases, they are asymptomatic, except in cases where they impact on sinus drainage patterns.Reference Becker, Larson, Duncavage and Becker1 Therefore, retention cysts of the maxillary sinus are not always an indication for FESS.
Retention cysts causing periodontitis and pulpitis of the root apex, and aggravating ascending pulpitis and pulpal necrosis, are not common in daily practice. The present study revealed that retention cysts of the maxillary sinus are an indication for FESS when they cause odontogenic infection (periodontitis and pulpitis of the root apex).
There is an atypical pathophysiological condition of odontogenic maxillary sinusitis caused by odontogenic infections precipitated by maxilla or maxillary sinus lesions.Reference Sato8,Reference Sato9 Retention cysts of the maxillary sinus are included in this category of maxillary sinus lesions. There is no consensus regarding the management of retention cysts of the maxillary sinus, especially the optimal timing of FESS.
Odontogenic maxillary sinusitis caused by odontogenic infections
Regarding the aetiology of usual odontogenic maxillary sinusitis, because of an increase of personal hygiene awareness in Japan, it has become rare that untreated dental diseases (i.e. dental caries) cause odontogenic maxillary sinusitis.Reference Sato2–Reference Sato, Chitose, Sato, Sato, Ono and Umeno7 Instead, most teeth that cause odontogenic maxillary sinusitis have already received dental treatment, especially root canal treatment, that is, endodontics.Reference Sato2–Reference Sato, Chitose, Sato, Sato, Ono and Umeno7 Consequently, it is important that the teeth always be suspected as the cause of odontogenic maxillary sinusitis, even if a dental procedure has already been performed.Reference Sato2,Reference Sato3
When the root canals of teeth are incompletely filled with a filling material during endodontics, insufficient root canal treatment causes pulpitis and pulp necrosis in the root canal at the root apex.Reference Sato2–Reference Sato4 Pathological studies of the problematic teeth (those causing the odontogenic maxillary sinusitis) show pulp necrosis and apical lesions after root canal treatment.Reference Sato2,Reference Sato3 Pulp inflammation causes apical lesions (apical periodontitis); consequently, odontogenic infection such as alveolar osteitis occurs.Reference Sato2,Reference Sato3 When the odontogenic inflammation is constantly presented at the floor of the maxillary sinus, the maxillary sinus is at risk of becoming inflamed.Reference Sato2,Reference Sato3
Odontogenic maxillary sinusitis precipitated by maxilla or maxillary sinus lesions
As mentioned above, the pathophysiology of the usual odontogenic maxillary sinusitis is well understood. However, atypical odontogenic maxillary sinusitis caused by odontogenic infections precipitated by the maxilla or maxillary sinus lesions is not well known.
Dental caries cause pulpitis in the pulp chamber, and pulpitis and pulp necrosis progress from the root canal to the root apex (Figure 4). However, there is another atypical pathophysiological condition of pulpitis and pulp necrosis. An inflammation around the root apex causes pulpitis in the root apex and root canal via the apical foramen, and pulpitis and pulp necrosis progress from the root apex, root canal and pulp chamber, that is, pulpitis and pulp necrosis are ascending (Figure 4).

Fig. 4. Progress of pulpitis and pulp necrosis caused by ascending pulpitis.
Sato reported an atypical pathophysiology of odontogenic maxillary sinusitis caused by odontogenic infections precipitated by the maxilla or maxillary sinus lesions.Reference Sato8,Reference Sato9 The pathological findings of the odontogenic infections are ascending pulpitis and pulp necrosis precipitated by the maxilla or maxillary sinus lesions, after which, ascending pulpitis and pulp necrosis cause apical lesions and odontogenic maxillary sinusitis.Reference Sato8,Reference Sato9 The maxillary sinus lesions are acute maxillary sinusitis and retention cysts, and maxilla lesions include post-operative maxillary cysts and odontogenic cysts.Reference Sato8,Reference Sato9
Odontogenic maxillary sinusitis precipitated by maxillary sinus retention cysts
Figure 5 shows the pathophysiology of odontogenic maxillary sinusitis caused by odontogenic infections precipitated by retention cysts in the maxillary sinus. When the root apex protrudes into the maxillary sinus and is covered by a retention cyst occupying the floor of the maxillary sinus, compression resorption and periodontitis of the root apex occur. Furthermore, pulpitis progresses from the root apex to the root canal (ascending pulpitis) (Figure 4). Once the ascending pulpitis and pulp necrosis occur, secondary apical lesions also occur. When secondary odontogenic inflammation such as apical periodontitis is constantly present at the floor of the maxillary sinus, the maxillary sinus is exposed to the potential danger of inflammation.Reference Sato2,Reference Sato3 The inflammation and infection from tooth roots can spread through the maxillary alveolar bone and sinus mucosa, thereby causing sinus inflammation and infection (secondary odontogenic maxillary sinusitis) (Figure 5).
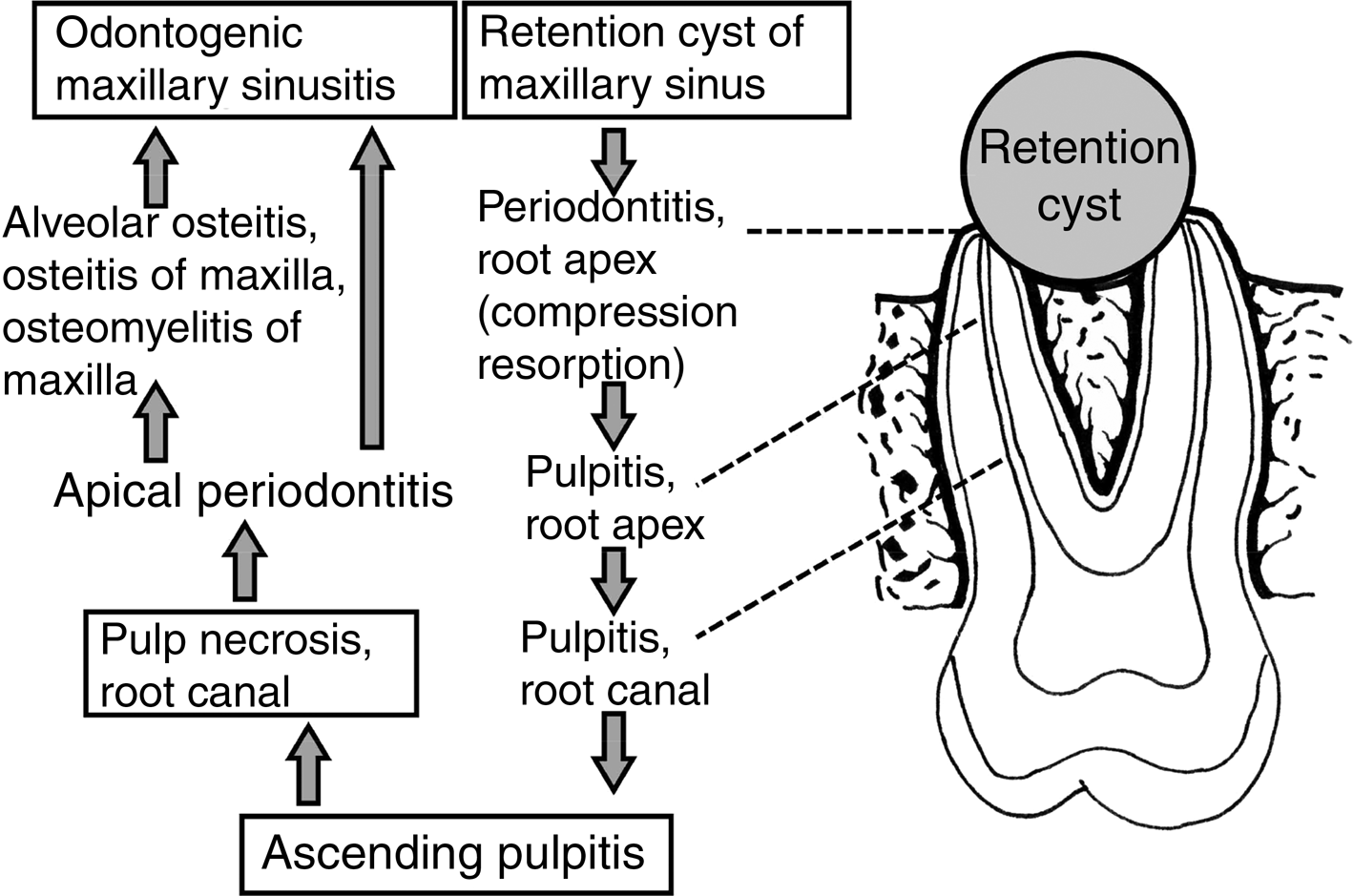
Fig. 5. Pathophysiology of odontogenic maxillary sinusitis caused by odontogenic infections precipitated by the maxilla or maxillary sinus lesions such as retention cysts. The main pathophysiology of odontogenic maxillary sinusitis caused by odontogenic infections precipitated by the maxilla or maxillary sinus lesions is ascending pulpitis and pulp necrosis.
Diagnosis of odontogenic infections caused by maxillary sinus retention cysts
Regarding the clinical symptoms, when persistent facial pressure and cheek pain continues even though there are no lesions in the tooth crown (except dental restoration), tooth root or periodontal tissue, the tooth should be suspected to have periodontitis and pulpitis around the root apex. In addition, when the tooth has percussion pain, the tooth should be suspected to have periodontitis and pulpitis around the root apex.
Cone-beam CT scanning is extremely accurate and useful in the diagnosis of odontogenic maxillary sinusitis.Reference Sato10–Reference Shahbazian, Vandewoude, Wyatt and Jacobs12 This study showed that cone-beam CT scanning is also extremely accurate and useful in the diagnosis of odontogenic infections caused by retention cysts of the maxillary sinus, in addition to physical examination. Furthermore, the relationships between the retention cysts and the apex of the affected teeth can be observed using cone-beam CT scanning. The retention cysts occur on a mucosal surface of the maxillary sinus floor, and they surround the root apex of the teeth protruding into the maxillary sinus.
Dental evaluations by plain dental radiography frequently fail to detect odontogenic infections caused by retention cysts of the maxillary sinus. The relationship between the retention cysts and the apex of teeth can be accurately observed using cone-beam CT scans.
Optimal timing of sinus surgery
As mentioned above, there is an atypical pathophysiology of odontogenic maxillary sinusitis caused by odontogenic infections precipitated by maxillary sinus lesions such as retention cysts. The pathological findings of the odontogenic infections are ascending pulpitis and pulp necrosis precipitated by maxillary sinus lesions.Reference Sato8,Reference Sato9
Functional endoscopic sinus surgery is highly indicated when a maxillary sinus retention cyst causes periodontitis and pulpitis of the root apex. In the present case series, the upper three-quarters portion of retention cysts was removed; however, the lower one-quarter portion of the cyst wall attached to the floor of the maxillary sinus and root apex were left intact under nasal endoscopy, to avoid injuring the apical foramen and dental nerve. The results of the present study showed that the treatment outcome was exceptionally good once the drainage of the retention cysts was successfully restored after surgery.
• The optimal timing of functional endoscopic sinus surgery (FESS) for odontogenic infections precipitated by retention cysts of the maxillary sinus was investigated
• The FESS should be performed before periodontitis and pulpitis of the root apex progress to ascending pulpitis and pulp necrosis
• In other words, FESS should be performed while the affected tooth is still vital
Regarding the optimal timing of FESS, The procedure should be performed before the periodontitis and pulpitis of the root apex progress to ascending pulpitis and pulp necrosis. In other words, FESS should be performed while the affected tooth is still vital. This surgical indication aims to prevent odontogenic maxillary sinusitis caused by odontogenic infections that are precipitated by maxillary sinus lesions such as retention cysts.
Conclusion
There is a pathophysiology of odontogenic infection caused by retention cysts of the maxillary sinus. Functional endoscopic sinus surgery should be performed before the periodontitis and pulpitis of the affected root apex progress to ascending pulpitis and pulp necrosis, and before odontogenic maxillary sinusitis caused by odontogenic infections that are precipitated by a retention cyst occurs. In other words, surgery should be performed while the affected tooth is still vital. Drainage of the retention cysts (leaving the cyst wall attached to the floor of the maxillary sinus and root apex intact) is recommended to avoid injuring the apical foramen and dental nerve.
Competing interests
None declared







