In a world increasingly beset by natural disasters, pandemics, and complex humanitarian emergencies, the imperative to incorporate disaster medicine into medical education has never been more urgent. With climate change leading to more frequent and severe natural disasters, and global connectivity heightening the spread of infectious diseases, medical professionals are increasingly likely to encounter disaster scenarios in their careers. Moreover, the coronavirus disease 2019 (COVID-19) pandemic has underscored the importance of preparing health-care providers for large-scale medical crises. Reference Marcassoli, Leonardi and Passavanti1
Yet, traditional medical education often falls short in preparing students for these exigencies. This gap can be addressed through innovative teaching methods, notably simulation-based training. Simulation in medical education provides a safe, controlled environment where students can learn and practice disaster response skills without real-world consequences. Reference Shrestha, Kanchan and Krishan2 It offers hands-on experience in managing mass casualty incidents, triaging patients, and making critical decisions under pressure—skills that are difficult to acquire through lectures or textbook learning alone. Additionally, the ethical aspects of disaster medicine, such as resource allocation and prioritizing care under duress, can potentially also be taught through these simulation exercises, providing a more comprehensive and realistic learning experience.
In accordance with this, International Federation of Medical Students’ Association’s (IFMSA’s) initiatives offer more insight into incorporating disaster medicine by means of short courses/trainings using different pedagogical exercises. The methodology used in these trainings includes lectures, workshops, role-plays, simulations, and presentations by external speakers, such as representatives from the International Committee of the Red Cross (ICRC). Reference Ragazzoni, Linty and Della Corte3 The objectives of the IFMSA training workshops align with broader efforts to incorporate disaster medicine into medical curricula. These workshops aim to provide basic knowledge of disaster medicine, foster a platform for discussion among students from diverse backgrounds, and create momentum for advocating better disaster preparedness within health systems. Importantly, these trainings also address hospital safety and health professional endangerment in frontline disaster response, a concern that has gained prominence considering recent events in conflict zones like Afghanistan.
Similarly, the Disaster Medicine Interest Group (DMIG) at the University of California, Riverside School of Medicine exemplifies the practical integration of disaster medicine into medical education. Established by medical students, the group focuses on equipping their peers with the necessary skills to deliver high-quality emergency care in a range of challenging conditions. Using the university’s advanced Center for Simulated Patient Care, DMIG provides immersive, realistic training experiences. This includes hands-on practice in managing emergencies in various settings, from wilderness scenarios to active shooter situations. 4 Concurrently, incorporating disaster electives has been received well from participating students and portrays higher student proficiency. Reference Kaji, Coates and Fung5
Therefore, DMIG’s simulation-based approach and IFMSA’s global training initiatives exemplify effective strategies for integrating disaster response into medical curricula. To support these efforts, a comprehensive schematic has been developed, serving as a practical guide for medical schools (Figure 1). This resource outlines critical training components, ensuring that medical students are not only theoretically proficient but also practically prepared for disaster scenarios. However, it is important to note that integrating disaster medicine into the curriculum comes with a unique set of challenges. Medical programs are densely packed, and incorporating disaster medicine requires a careful balance to avoid overwhelming students or diminishing other vital subjects. Alongside this, resource allocation needed for simulation-based training poses its own set of difficulties. These simulations, crucial for hands-on experience, demand not just advanced equipment but also skilled personnel to facilitate the sessions and ample time for students to engage in these learning activities. Moreover, ensuring consistency and standardization across various educational institutions adds another layer of complexity. It is vital to establish a core set of competencies and learning objectives that are applicable across institutions, ensuring that all medical students, irrespective of their place of training, receive uniform instruction.
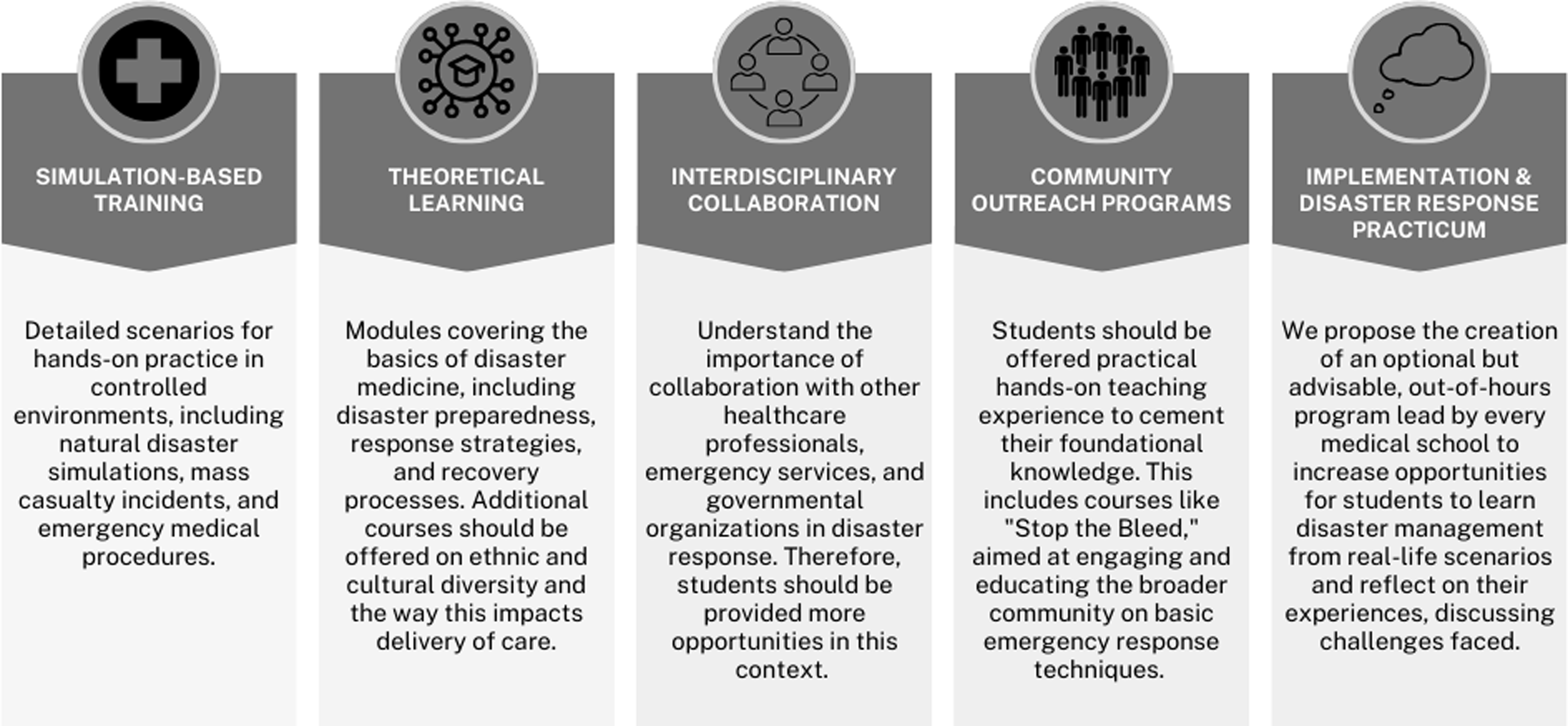
Figure 1. Comprehensive framework for disaster medicine integration in medical education.
All in all, by integrating real-life scenario-based learning into the medical curriculum through an extracurricular framework, we are not only enhancing the practical skills and preparedness of future medical professionals but also ensuring their education remains responsive to the challenges of modern health-care landscapes. It is a step forward in aligning medical education with the dynamic demands of health care in disaster and crisis situations.
Author contributions
Both M.H.S. and S.R. carried out the concept and design of the research question. S.R., M.H.S., and E.F. drafted the manuscript and edited and revised the manuscript, offered administrative, technical, or material support and approved the final version.
Competing interests
None.



