Trauma is the leading cause of death for Americans ages 1–44 and is one of the main causes of death among all ages globally. 1 The Stop the Bleed (STB) campaign, a public–private cooperative effort, brings battlefield lessons regarding hemorrhage control to benefit members of the public. Reference Rasmussen, Baer and Goolsby2,3 STB recommends that the public have immediate access to private and public bleeding control kits. 3 Several studies have demonstrated the public’s ability to learn bleeding control techniques and apply tourniquets. Reference Goolsby, Branting and Chen4–Reference Brannen, Howell and Bidigare10 Efforts to apply tourniquets before hospital arrival have saved lives, and there are estimates that rapid response from the public could save even more lives in the future. Reference Scerbo, Holcomb and Taub11–Reference Goolsby, Rojas and Andersen13 The major resuscitative medical training organizations in the United States, the American Red Cross and the American Heart Association, now consider tourniquet application to be the preferred first-line treatment for life-threatening extremity hemorrhage. Reference Pellegrino, Charlton and Carlson14
Despite wide acceptance of tourniquet efficacy and recommendations for the public use of tourniquets, there is no existing evidence to guide the optimal placement of the tourniquets and hemorrhage control supplies in public locations. In 2019, based on an analysis of available literature and data about mass casualty incidents, Goolsby et al. published recommendations to equip public spaces that have more than 50 people present with supplies to treat at least 20 bleeding victims. Reference Goolsby, Strauss-Riggs and Rozenfeld15 The authors concluded, however, that it was not possible to recommend how and where the equipment should be placed in various facilities in that study. Reference Goolsby, Strauss-Riggs and Rozenfeld15
Despite the lack of placement recommendations, bleeding control kits can already be found in many airports, stadiums, schools, and other public spaces. In many cases, they are co-located with automatic external defibrillators (AEDs). However, the nature of a response with hemorrhage control supplies differs from that for cardiac arrest. For one, there may be multiple patients at one time compared to the typically single cardiac arrest patient. Additionally, one recommendation for AED placement is to place them close to exits. Reference Johnson, Cunningham and Zégre-Hemsey16 If bleeding control kits are co-located with AEDs at exits, there may be difficulties in accessing the supplies if people are trying to flee a mass casualty incident through the same exits. Finally, the placement strategy for public access AEDs is typically based on the likelihood of cardiac arrest in densely populated areas, such as train stations and airports. Reference Marijon, Bougouin and Tafflet17–Reference Caffrey, Willoughby and Pepe19 Mathematical models, using discrete event simulations, have been used to optimize AED placement strategies and estimate survival based on certain assumptions about cardiac arrests. Reference Bonnet, Gama Dessavre, Kraus and Ramirez-Marquez20–Reference Sun, Karlsson and Morrison22 Similar models are needed for trauma patients to guide medical major incident preparedness. Reference De Rouck, Debacker and Hubloue23,Reference Debacker, Van Utterbeeck and Ullrich24
The aim of the current study was therefore to create and perform initial tests of a model to evaluate the efficacy of various locations and quantities of hemorrhage control supplies in public spaces. The model simulates a common public space—an enclosed shopping mall—with a bomb blast causing a mass casualty incident. The current study builds on previously reported initial findings based on early development of a simulation model where the simulation outcome indicated a warranted strategy of decentralized and dispersed placement of bleeding control kits, and a need for many tourniquets. Reference Prytz, Grönbäck and Steins25 The model was further developed in the current study to evaluate the optimal placement of bleeding control kits in public venues, such as a shopping mall.
Methods
We used discrete event simulation (DES) to model and simulate several scenarios where an explosion would take place in a public space. The simulation model was implemented in the commercially available simulation software ARENA (Rockwell Automation). Reference Kelton, Sadowski and Swets26 In the model, people are simulated as separate entities with individual characteristics and history. To model the uncertainty and variation in real-world scenarios, random numbers are drawn from several different probability distributions. Each model run (or simulation) will therefore produce a different output, and many runs, called replications, are required to estimate the variation in outcomes of the modeled system. Simulation modeling involves making assumptions and simplifications, as the true nature of the modeled system characteristics is either completely unknown, little studied, or too complex to be captured in its entirety. However, the model allows risk-free, transparent, controlled, and replicable testing of scenarios that would be hard to replicate and repeated in, for example, a field exercise. Reference Robinson27,Reference Banks, Carson and Nelson28
At the start of the simulation, a detonation of an improvised explosive device (IED) takes place at a random location in a simulated shopping mall. The people who are in the proximity of the IED location suffer injuries of varying degrees, proportionate to their proximity to the explosion. Following the explosion, some of the uninjured people will start to help the injured as immediate responders. These can be either trained or untrained. Of the immediate responders, a fraction will try to find the location of the bleeding control kits, retrieve the kits, and bring them to the injured persons. Each kit is modeled to contain bleeding control equipment for a single patient, that is, 1 tourniquet. Other content that would typically be part of such kits is disregarded in the model. The rest of the immediate responders and people trained in first aid will in the meantime move to the injured people directly and try to apply pressure to control the bleeding. After a specified time, emergency medical services (EMS) will start arriving at the scene and try to stabilize and transport injured persons to the hospital. The simulation ends when all injured persons are transported away by EMS.
The key variables of the model are described in Table 1. Assumptions are based on best available evidence generated from an extensive literature review or on subject matter expert opinions. For the main set of experiments, the model was run for 500 replications. The model had 2 main experimental factors—bleeding control kit locations (coordinates) and number of kits at each location. Additional inputs that were changed during sensitivity analyses were whether kits were easy to find, how many times a volunteer would look for a kit before giving up, and the (non-random) location of the explosion.
Table 1. Key variables
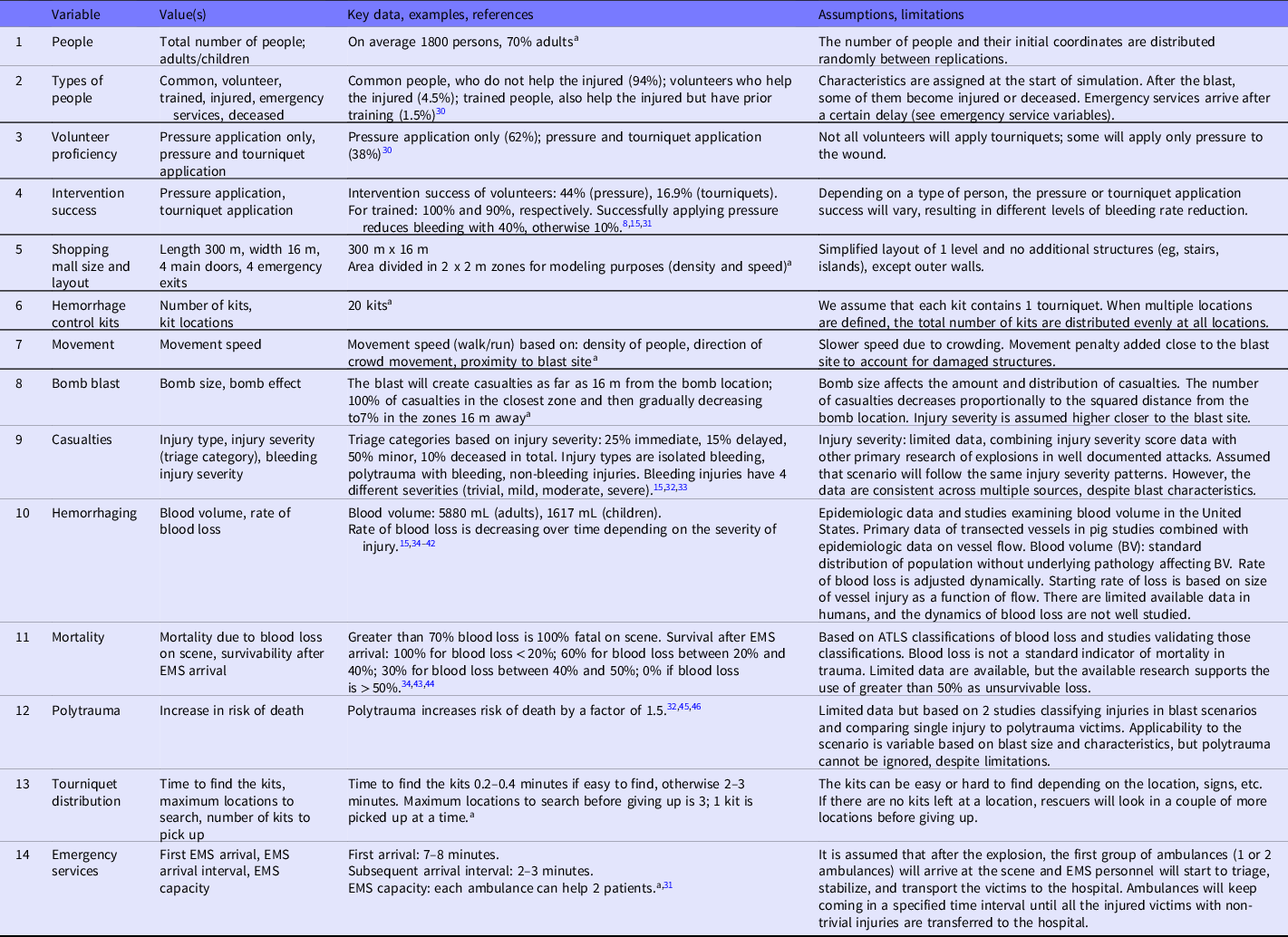
a Values are based on subject matter expert opinions.
The primary outcome in the simulation model was the number of victims who survived with non-trivial bleeding injuries. As secondary outcomes, average blood loss (%), time until tourniquet application and number of tourniquets applied were used.
The following alternative placement strategies were tested in the simulation:
-
Single location at exit. All kits in 1 location, placed near 1 of the main exits.
-
Two locations at exits. Kits equally divided in 2 locations, placed near the 2 main exits.
-
Focused easy reach. Kits equally divided in 2 locations, away from any exits, 100 m apart, co-located with AEDs. This would ensure a 90-second walking distance from any point in the mall, a recommendation typically used for AED placement. Reference Aufderheide, Hazinski and Nichol29
-
Dispersed easy reach. Kits placed in 10 locations equally spread out through the mall, all away from any exits.
For the best strategy, we tested varying the total number of kits (5 to 30 with increments of 5). We compared these results to a case where no kits were available.
Results
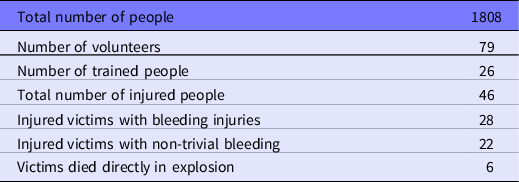
For the main analysis, the simulations resulted in a mass casualty incident with the characteristics summarized in Table 2.
Table 2. Incident characteristics, main analysis, rounded average values from 500 replications
Comparing the alternative placement strategies, using 20 hemorrhage control kits in locations that are clearly marked and easy to find resulted in the outcomes summarized in Table 3.
Table 3. Comparison of four placement strategies, using 20 kits, easy to find locations
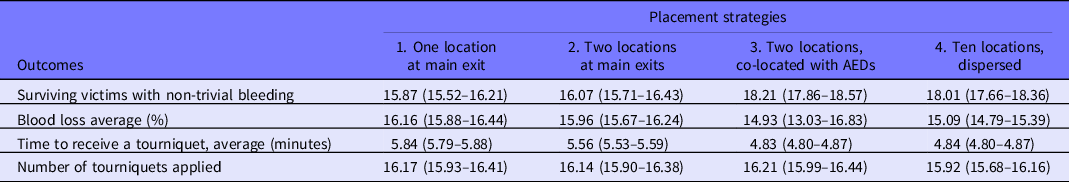
All results are average values and 95% confidence intervals from 500 replications.
Paired t-tests showed that the differences in survivals between strategies are statistically significant (at alpha = 0.05), for example, the difference in survivals between strategies 3 and 4 is 0.202, 95% CI (0.021–0.383).
The change in number of survivals when varying the number of available kits in increments of 5 for the best strategy (3) is illustrated in Figure 1.

Figure 1. Varying number of available hemorrhage control kits for strategy 3.
If the kits are hard to find, which we modeled as increased time for locating them, from 0.3 minutes to 2.5 minutes (on average), the differences between strategies become smaller, for example, strategy 2 results in 15.16 survivals, 95% CI (14.82–15.49), compared to strategy 3 with 15.19 survivals, 95% CI (14.84–15.54).
Discussion
Tourniquets have been shown as either beneficial or likely beneficial in multiple studies of the civilian public and are now widely recommended as first-line treatments for the public by major first aid training organizations. Reference Scerbo, Holcomb and Taub11,Reference Goolsby, Rouse and Rojas12,Reference Pellegrino, Charlton and Carlson14,Reference Inaba, Siboni and Resnick47,Reference Cunningham, Auerbach, Cicero and Jafri48 While a prior study estimated the number of bleeding control kits needed in public venues with at least 50 persons, Reference Goolsby, Strauss-Riggs and Rozenfeld15 our study provides the first evidence of the optimal distribution of these supplies in public spaces.
Our model demonstrates that placing tourniquets at 90-second walk intervals, easy to find locations co-located with AEDs throughout public facilities is the distribution most likely to improve survivability from bleeding injuries during a mass casualty incident. This distribution strategy is statistically better than locating all the tourniquets in a single location, which will increase travel times and decrease the likelihood of rescuers finding equipment. The 90-second walk interval locations away from exits are also better than locating tourniquets at exits, which can cause significant delays in retrieving and returning with equipment as people are trying to flee the location.
There is no significant advantage of locating the tourniquets in more places than where AEDs are placed at 90-second walking intervals, since 10 locations had no advantage over two locations in the model. If a fixed number of kits are spread over many locations, the locations closest to the incident will quickly run out of kits, and people might stop trying to find additional kits. Thus, while we would not recommend locations that have supplies dispersed at more than 90-second walk intervals, we would also not recommend further distributing them. This finding will likely make implementing bleeding control equipment in public spaces more practical.
The results are reassuring for emergency planners and facility managers who have co-located their hemorrhage control supplies with AEDs in public locations, if they are placed away from the exits. If the AEDs are placed at 90-second walking intervals, then the co-located hemorrhage control supplies should be widely accessible to the public and yield results like the model. Furthermore, many AEDs have the advantage of being clearly marked, and this indication of emergency supplies will also likely help the public. Co-locating AEDs and bleeding control equipment together may aid public service campaigns to increase awareness of both rescue items. This is further supported by the effect when a “hard to find” factor was added to the placement strategy that resulted in an erased benefit of the distributed bleeding control kits.
Public locations with hemorrhage control supplies located at exits should consider relocating them. The results indicate a distinct survival advantage for tourniquets that are not clustered at exits. In violent mass casualty incidents like a blast, there will be many people attempting to exit the facility. This will likely make it exceedingly difficult for a would-be rescuer to reach supplies at the exit and return to hemorrhaging victims in a timely fashion. Policymakers should consider including location recommendations for hemorrhage control placement when creating rules that require hemorrhage control supplies in public settings and/or specify the contents of hemorrhage control kits.
This study provides evidence that placing bleeding control kits in multiple locations within 90-second walking intervals provides the optimal outcome of decreasing mortality. Prior work by Goolsby et al. Reference Goolsby, Strauss-Riggs and Rozenfeld15 recommended that public spaces having more than 50 people present be equipped with supplies to treat 20 bleeding victims. Our results indicate a saturation of the benefit of more than 20 tourniquets, which would imply that larger venues could still plan for 20 tourniquets as a base but would need to add a 90-second rule to that, so that each part of the venue should not be more than 90 seconds away from a location of tourniquets. With this work, public health experts can further develop best practices for equipping public spaces to handle mass casualty incidents. Our model can be adapted to simulate other types of mass casualty incidents, the type of which may vary on locality. As mass casualty incidents will continue to occur throughout the world, further modeling studies including validations of the models may be used to guide public health experts in mitigating their particular hazards.
Limitations
As a modeling study, this study heavily relies on the underlying assumptions. All assumptions that were part of the model are consistent in all tested scenarios. The central limitation that this model assumes mortality is a direct correlate to blood loss, as this is the major factor controlled by a tourniquet. However, precise blood loss and rate of loss are not well quantified by most studies of traumatic injury, and instead emphasize other measurable physiologic factors, like vital signs and Glasgow Coma Scale, as indirect indicators of mortality risk. It therefore became necessary to generate a series of calculations and assumptions alongside available data to translate blood loss interventions (tourniquets) to mortality risk. The underlying dependent and independent variables, including bleeding rates, blood volume, injury severity, polytrauma, mortality, and survivability, were developed from the best available data and by consensus from experts in the field. Further, efficacy of bleeding control measures in trained and untrained individuals and ability of rescuers to respond following a mass casualty incident are unknown, both of which are key for time to intervention, and estimates had to be made. While attempts were made to find evidence-based inputs for all assumptions, many have little applicable scientific literature available. As such, assumptions were adjusted to calibrate and validate the model by comparing the simulation results to the expected results by a group of experts. However, even a perfect model may not accurately predict the ways in which real-world events will unfold. While it was assumed for the model that tourniquets were either “easy” or “hard” to find, this study did not explore the specific mechanisms of how to make a bleeding control kit easier to find for a lay rescuer. Further, the scenarios explored by this model were limited to a single blast in a single, long corridor without a follow-on attack. Additional scenarios should be tested with different layouts, including multiple floors, and different injury parameters in terms of the number of injured people and types of injuries.
Conclusions
Co-locating public bleeding control kits with AEDs results in the best casualty outcomes after a computer modeled mass casualty incident in a shopping mall. This study provides the first evidence to support the common practice of co-locating emergency medical response supplies at 90-second walking intervals apart in public locations. Tourniquets can be distributed at shorter walk intervals but should not be located at exits for a large public space.
Acknowledgments
The authors would like to thank Laura Valdez Vidal and Silvia María Cervera López for the development of the early versions of the simulation model.
Author contributions
Krisjanis Steins: Conceptualization, Formal analysis, Investigation, Methodology, Software, Writing – Original draft preparation, Writing – Reviewing and Editing;
Craig Goolsby: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Writing – Original draft preparation, Writing – Reviewing and Editing;
Anna-Maria Grönbäck: Conceptualization, Formal analysis, Investigation, Methodology, Software, Writing – Original draft preparation, Writing – Reviewing and Editing;
Nathan Charlton: Conceptualization, Methodology, Writing – Reviewing and Editing;
Kevin Anderson: Conceptualization, Methodology, Writing – Original draft preparation, Writing – Reviewing and Editing;
Nicole Dacuyan-Faucher: Funding acquisition, Project administration, Writing – Reviewing and Editing;
Erik Prytz: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Writing – Reviewing and Editing;
Tobias Andersson Granberg: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Writing – Reviewing and Editing;
Carl-Oscar Jonson: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Resources, Writing – Original draft preparation, Writing – Reviewing and Editing.
Funding statement
This study was supported by grants from the United States Department of Homeland Security Science & Technology Directorate (DHS-S&T), the Swedish Civil Contingencies Agency and Linköping University institutional funds. The funders had no role in study design; collection, analysis, and interpretation of data; writing the report; and the decision to submit the report for publication.
Competing interests
Craig Goolsby has a patent pending for a layperson tourniquet. Craig Goolsby declares that he has performed paid consulting work for Zoll Medical Corporation (2023–current). Carl-Oscar Jonson and Erik Prytz have a patent for a tourniquet training device. No financial disclosures were reported by other authors of this paper.






