The pandemic caused by the novel coronavirus disease 2019 (COVID-19) has transformed healthcare significantly. COVID-19 is highly contagious and physical distancing is recommended to prevent disease transmission.Reference Chu, Akl, Duda, Solo, Yaacoub and Schünemann1. Telemedicine is a viable option to reduce COVID-19 infection among both healthcare providers and patients while allowing access to medical care.Reference Hollander and Carr2,Reference Wosik, Fudim, Cameron, Gellad, Cho and Phinney3 Although the COVID-19 pandemic posed unprecedented challenges to healthcare delivery systems, it also prompted the rapid adoption of telemedicine, which has revolutionised healthcare delivery. Health systems implementing telemedicine were able to maintain continuity of care for out-patients during the pandemic amid ‘stay at home’ orders and measures requiring physical distancing, reducing the spread of the disease to the community and hospitals.Reference Wosik, Fudim, Cameron, Gellad, Cho and Phinney3 Telemedicine was also effective in in-patient care, particularly in balancing the supply of clinical services with surges in demand across physical or geographical boundaries, saving personal protective equipment and providing isolated patients with connections to family and friends.Reference Hollander and Carr2,Reference Keesara, Jonas and Schulman4 This growing recognition that telemedicine programmes can overcome physical barriers and provide convenient access to care for patients and caregivers has led several countries, including Australia, Brazil, the UK and USA, to relax regulations that had previously limited the spread of telemedicine.Reference Wosik, Fudim, Cameron, Gellad, Cho and Phinney3,Reference Fisk and Livingstone5–Reference Teles, Sacchetta and Matsumoto7 As a result, the use of telemedicine has been expanding worldwide.Reference Fisk and Livingstone5,Reference Teles, Sacchetta and Matsumoto7–Reference Yellowlees, Nakagawa, Pakyurek, Hanson, Elder and Kales9
Telepsychiatry
Psychiatry is probably the most suitable field of medicine for the use of videoconferencing, as diagnoses and symptom assessments are completed by conversing with patients and the use of laboratory tests is limited. Psychiatric consultation and counselling using remote videoconferencing, or telepsychiatry, has been discussed for more than 50 years,Reference Wittson and Benschoter10 and interest in telepsychiatry had been increasing in recent years, even prior to the COVID-19 pandemic. This is due to the development of communication technologies that enable videoconferencing to be performed easily, with high resolution and at low cost. Between 2010 and 2017, the use of telepsychiatry by US state institutions increased from 15.2% to 29.2%.Reference Spivak, Spivak, Cullen, Meuchel, Johnston and Chernow11 According to the REACH Health survey targeting US healthcare providers, the percentage of facilities actively using psychiatric telemedicine grew from 49% to 59% between 2015 and 2018.12 In addition, compared with other medical specialties, telemedicine is most frequently used in psychiatry. According to the above-mentioned survey, psychiatry had the highest utilisation rate among all medical specialties in 2018. Within Canada's Ontario Telemedicine Network, over half of the 204 058 telemedicine consults in 2011–2012 were reported to have been conducted using telepsychiatry.Reference Brown13 In response to this situation, the American Psychiatric Association officially convened a committee on telepsychiatry in 2015.
The advantages of psychiatric telemedicine are manifold. Telepsychiatry increases access to psychiatric care. It can be a necessity for patients living in underserved areas and those for whom visiting hospitals/clinics is difficult because of physical difficulties and/or psychiatric symptoms. Telepsychiatry can also lead to early intervention and can simplify the coordination of treatment involving multiple healthcare providers.Reference Baer, Elford and Cukor14–Reference Chakrabarti19 On the other hand, the potential disadvantages of telepsychiatry include a negative impact on doctor–patient rapport, drop out from long-term treatment, the cost of infrastructure, the possibility of misdiagnosis/maltreatment, essential proficiency in operating web conferencing systems, and limited availability owing to financial and IT skills/ability issues. Moreover, telepsychiatry might be well suited for some psychiatric disorders but not others, depending on the specific disease characteristics.
Study hypothesis and aims
A comprehensive review and meta-analysis comparing telepsychiatry and face-to-face treatment has not yet been conducted for all psychiatric diseases, and the various outcomes have not been examined in a detailed manner. We hypothesised that telepsychiatry is not inferior to face-to-face treatment in terms of therapeutic efficacy, but that some differences in treatment efficacy may exist across psychiatric diseases. We aimed to obtain such information through a review and meta-analysis, as such knowledge will be important for delivering psychiatric care as well as policy-making in the post-pandemic era.Reference Hyler and Gangure20–Reference Davies, Morriss and Glazebrook24
Method
Search strategy and selection criteria
The meta-analysis followed PRISMA guidelines for reporting systematic reviews and meta-analyses of studies. This study protocol was registered with PROSPERO (CRD42021254501).
We conducted a literature search without language restrictions using MEDLINE, PubMed, the Cochrane Library, Scopus, Embase, CINAHL and PsycInfo from database inception.
The following keywords were used to identify articles suitable for inclusion in the analysis: (telemedicine [MeSH Terms] OR telemedicine* [All Fields] OR ‘tele medicine*' [All Fields] OR ‘tele-medicine*' [All Fields] OR videoconferencing [All Fields] OR telepsychiatry [All Fields] OR telehealth [All Fields]) AND (‘mental disorder*' [All Fields] OR mental disorders [MeSH Terms] OR Psychiatry [MeSH Terms] OR Psychiatr* [All Fields]).
Manual searches of the reference lists of relevant publications were also conducted.
At least two investigators (among T.K., K.H., S. Kurokawa, S.F., Y.E., M.F., A.T. and S. Kinoshita) independently conducted the literature search for each database.
We performed the literature search for both RCTs comparing the efficacy of telepsychiatry with face-to-face treatment and trials assessing diagnostic concordance between telepsychiatry and face-to-face treatment. In this article, we report the results of a meta-analysis of RCTs comparing the efficacy of telepsychiatry with face-to-face treatment. Criteria for inclusion in this meta-analysis were:
(a) RCTs comparing telepsychiatry with face-to-face for treatment efficacy
(b) 20 or more patients in the study
(c) including any psychiatric disorders listed in DSM-5 except conditions that are ‘attributable to another medical condition’
(d) the study did not focus only on health economics and outcomes research (HEOR).
Data extraction, primary and secondary outcomes
Data were extracted independently by at least two reviewers (among K.H., S. Kurokawa, S.F., Y.E., M.F., A.T. and S. Kinoshita) experienced in conducting literature searches and data extraction. Disagreements were resolved by a consensus meeting that included a third person (T.K.). The first data extraction was performed on 5 May 2022.
For studies that compared the efficacy of telepsychiatry treatment and face-to-face treatment, the primary outcome was set as the mean change, from baseline to end-point, in the standard symptom scale scores (if an end-point score was not reported) used for each disease.
Secondary outcomes included all-cause treatment discontinuation, discontinuation because of an adverse event, discontinuation because of inefficacy, treatment response, remission, patient satisfaction/acceptability, psychiatrist satisfaction, symptom severity scale score other than the primary outcome, quality of life and functional improvement.
Data synthesis, analysis, and quality assessment
For the primary outcome, the effect size of the symptom scale score was analysed for each disease; finally, the combined effect size for the overall disease was analysed.
In addition, the following secondary outcomes were analysed in an integrated manner, as they evaluated similar symptoms: Clinical Global Impression – Severity (CGI-S) and Global Severity Index; Sheehan Disability Scale and World Health Organization Disability Assessment Schedule (WHODAS); Clinician-Administered Post-Traumatic Stress Disorder (PTSD) Scale (CPAS) and PTSD Checklist; and Quality of Well-Being scale, Quality of Life Enjoyment and Satisfaction Scale (QLES) and Quality of Life Scale (QOLS).
Continuous outcomes were expressed as the standardised mean difference (s.m.d.) and dichotomous outcomes were expressed as the pooled relative risk (RR) using the inverse variance method. The s.m.d. and RR values were reported with their 95% confidence intervals (CIs).
We explored study heterogeneity using the χ2-test of homogeneity and I2 statistics, with P < 0.05 and I2 > 50% respectively indicating significant heterogeneity. All analyses were two-tailed with an α of 0.05. No adjustments were made to the P-values for the multiple comparisons.
All data were double-entered into and meta-analysed using Comprehensive Meta-Analysis Version 3 for Windows (BioStat; Englewood, New Jersey) by applying a random-effects model, as heterogeneity was expected among the studies.
All eligible studies were assessed for methodological quality using the Cochrane Collaboration's tool for assessing risk of bias. We extracted data on study design, patient illness characteristics, age, gender, marital status, educational level, family income, residential area (urban/rural), computer ownership/internet subscription, location of participants and quality of internet connection used for telepsychiatry.
We conducted subgroup/meta-regression analyses to identify potential methodological biases or subpopulations in which the primary outcome differed, as follows: (i) publication year, (ii) mean age, (iii) gender, (iv) sample size, (iv) trial duration, (v) country, (vi) study sponsorship and (vii) disease group.
Publication bias was assessed by visually inspecting funnel plots. In addition, we applied the Egger's regression test to the primary outcome whenever ≥3 studies were analysed. Then, to account for publication bias, we used the trim-and-fill method. Finally, the fail-safe number of negative studies that would be required to nullify a statistically significant effect size (i.e. to make P > 0.05) was calculated.
Results
The initial search produced 6875 records; 6665 records were excluded because they were clearly irrelevant or duplicates. Of the remaining 210 records, 175 were excluded after a full-text review, yielding 35 records, including 32 RCTs, comparing efficacy (Fig. 1).
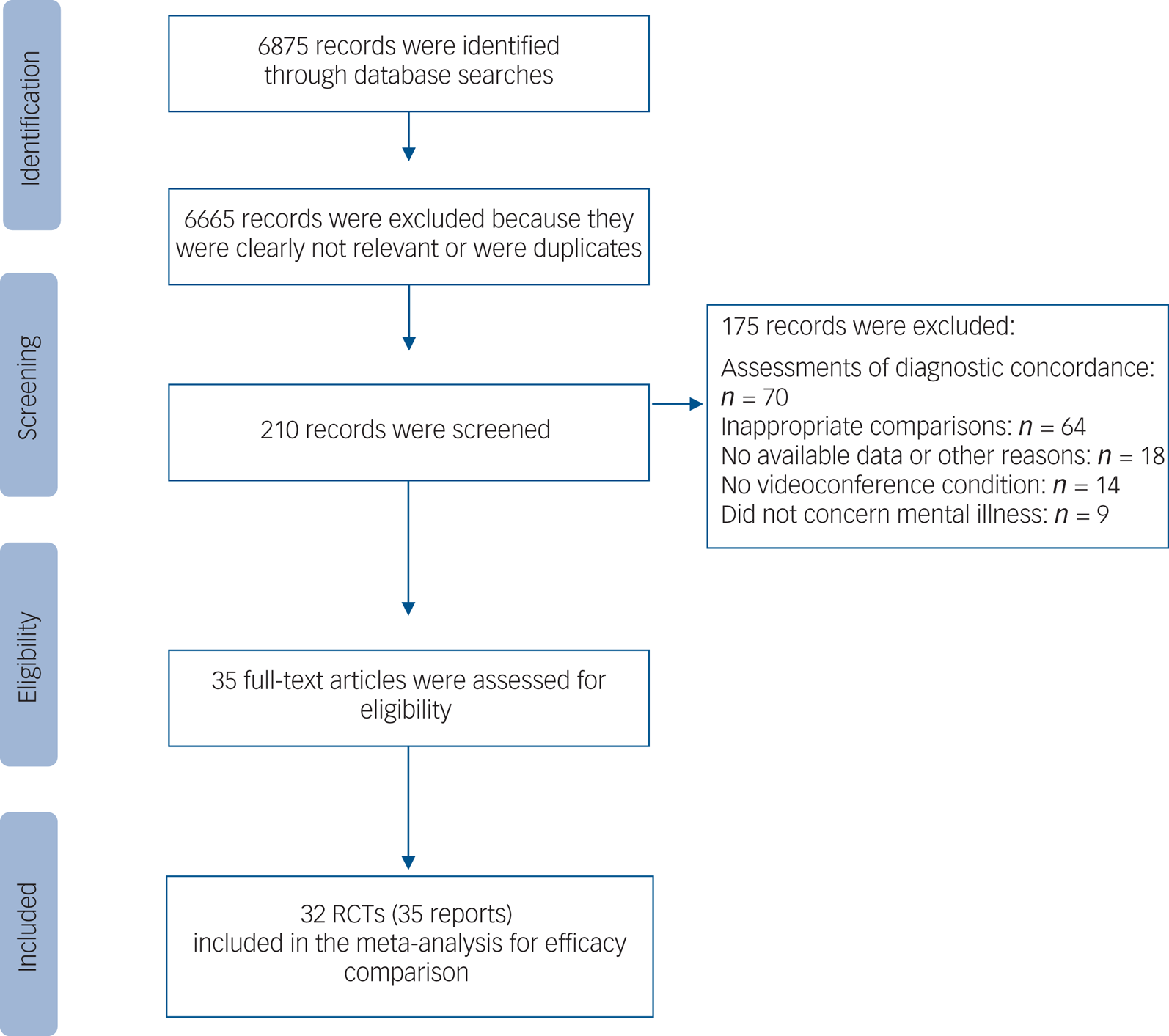
Fig. 1 Flow diagram describing the search process.
The studies, patients, illnesses and treatment characteristics are summarised in Supplementary Table S1, available at https://dx.doi.org/10.1192/bjp.2023.86). A list of the studies is given in the Supplementary References.
Studies, patients and treatment characteristics
All included studies were published or conducted between 2003 and 2021. None of the studies were sponsored by private companies, such as pharmaceutical or medical device manufacturers. The total number of participants was 3592 and the median number of participants per study was 111 (range: 20–495). The mean age of the participants was 41.3 years (s.d. = 17.8) and 58.2% were male (Supplementary Table S1). The numbers of studies and participants according to mental illness diagnosis are shown in Supplementary Table S1. There were many studies for depression (k = 8) and post-traumatic stress disorder (PTSD) (k = 11), but many other diseases had only 1 study each.
Primary outcome
Of the 10 psychiatric disorders analysed, no significant difference in symptom score improvement was found between telepsychiatry and face-to-face treatment for 8 disorders (chronic tic disorders, obsessive–compulsive disorder (OCD), PTSD, insomnia, disruptive behaviour disorder (DBD), substance misuse, mild cognitive impairment (MCI) or mild dementia, and multiple disorders).
For participants with depressive disorders, however, telepsychiatry was significantly more effective than face-to-face treatment for improving depressive symptoms (k = 6, n = 561; s.m.d. = −0.325, 95% CI −0.640 to −0.011, P = 0.043). On the other hand, for eating disorder, face-to-face treatment was significantly more effective than telepsychiatry for improving symptoms, based on one study (n = 128; s.m.d. = 0.368, 95% CI 0.018–0.717, P = 0.039) (Fig. 2).
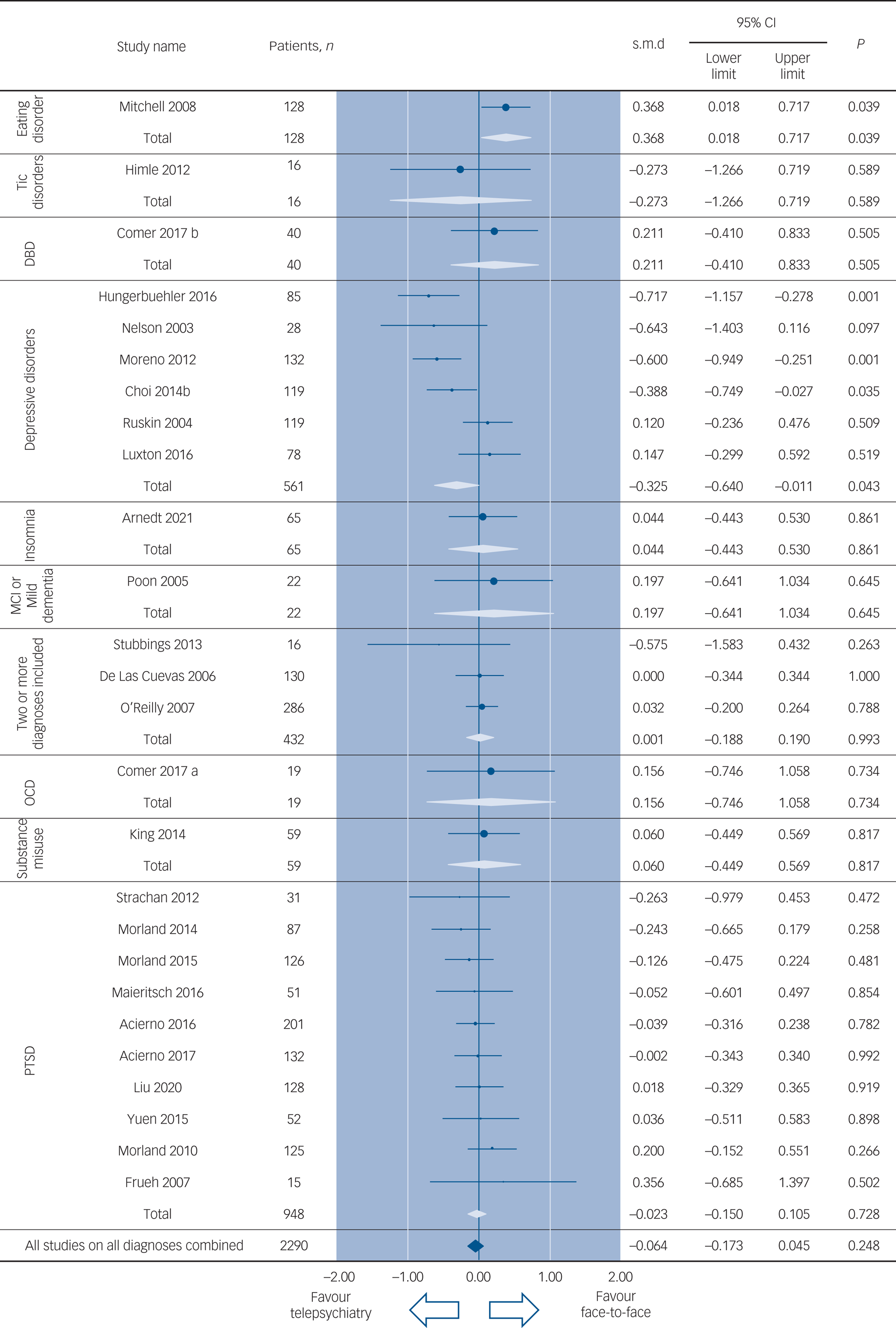
Fig. 2 Primary outcome measure (change in the standard symptom scale scores used for each disease, all diagnoses combined). DBD, disruptive behaviour disorders; MCI, mild cognitive impairment; OCD, obsessive–compulsive disorder; PTSD, post-traumatic stress disorder; s.m.d., standardised mean difference.
When all the studies examining all the diagnoses were combined, the mean change from baseline to end-point in the standard symptom scale scores was not significantly different between telepsychiatry and face-to-face treatment (k = 26, n = 2290; s.m.d. = −0.064, 95% CI −0.173 to 0.045, P = 0.248) (Fig. 2).
Secondary outcomes
All-cause treatment discontinuation
Figure 3 provides the detailed results of comparisons for all-cause treatment discontinuation.
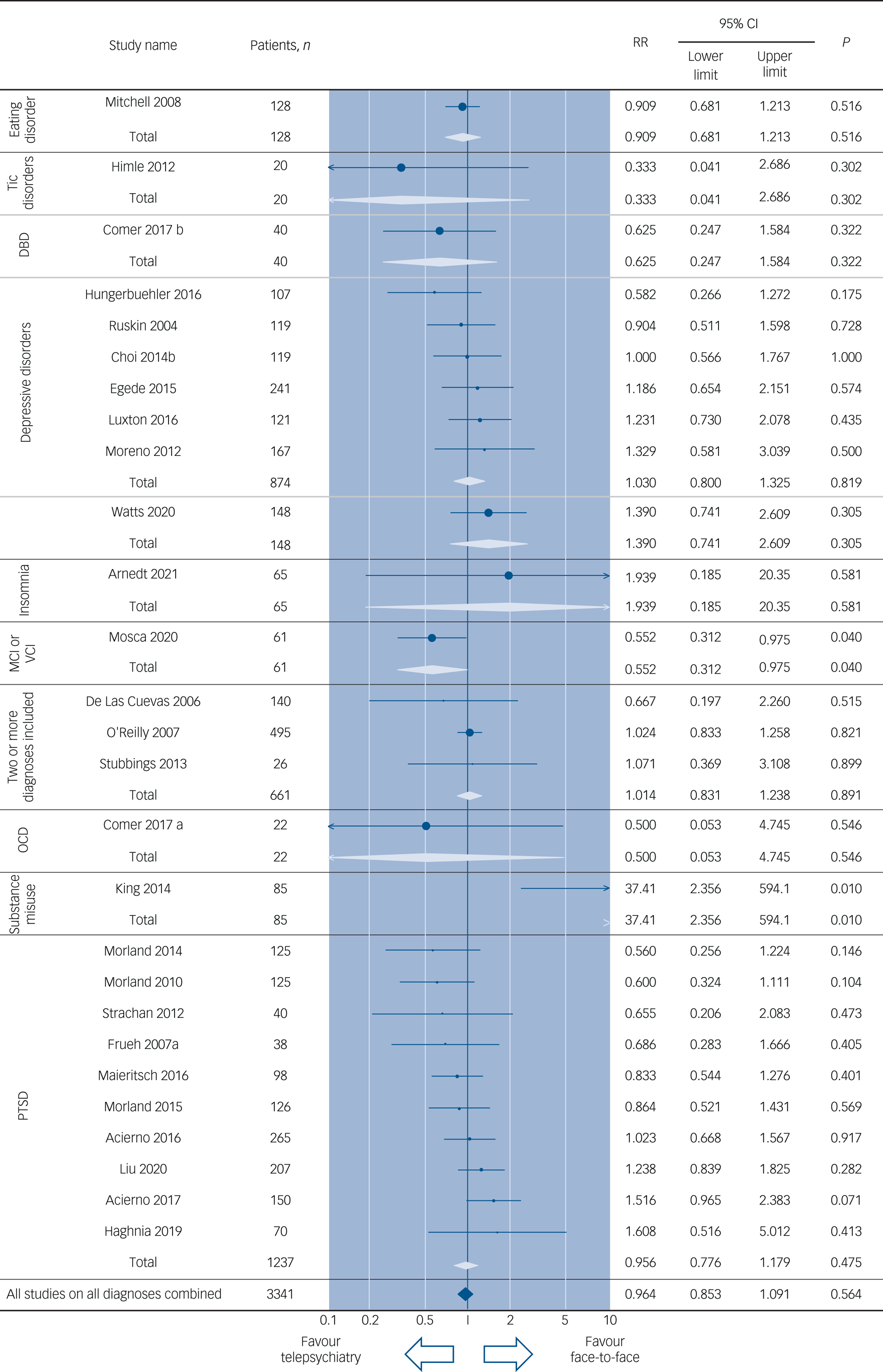
Fig. 3 All-cause discontinuation (all diagnoses combined). DBD, disruptive behaviour disorders; GAD, generalised anxiety disorder; MCI, mild cognitive impairment; OCD, obsessive–compulsive disorder; PTSD, post-traumatic stress disorder; RR, risk ratio; VCI, vascular cognitive impairment.
When the participants were compared according to diagnosis, telepsychiatry was associated with a significantly lower risk of study discontinuation than face-to-face treatment among patients with MCI or vascular cognitive impairment (VCI) (k = 1, n = 61; RR = 0.552, 95% CI 0.312–0.975, P = 0.040, number needed to treat for an additional beneficial outcome for telepsychiatry NNTB = 4). Face-to-face treatment was associated with a significantly lower risk of study discontinuation than telepsychiatry among patients with substance misuse (k = 1, n = 85, RR = 37.41; 95% CI 2.356–594.1, P = 0.010, number needed to treat for an additional harmful outcome for telepsychiatry NNTH = 2). Telepsychiatry was similar to face-to-face treatment in terms of study discontinuation when all the diagnoses were combined (k = 27, n = 3341; P = 0.564).
Other secondary outcomes
In most comparisons, including those for efficacy, adherence and satisfaction, no significant differences were seen between telepsychiatry and face-to-face treatment, with some exceptions (Supplementary Table S2).
Sensitivity analyses and meta-regression analyses
Supplementary Tables S3 and S4 show the results of predefined sensitivity analyses and meta-regression analyses for the primary outcome.
When all the studies on all the diagnoses were combined, the effect sizes for telepsychiatry compared with face-to-face treatment in each subgroup according to publication year were not significant; however, the effect size differed between subgroups (s.m.d. = 0.087 for RCTs published between 2000 and 2009, s.m.d. = −0.122 for RCTs published in 2010 or later; between-group P = 0.048).
For depressive disorders, no significant differences between telepsychiatry and face-to-face treatment were seen when the study period was 26 weeks or shorter. Telepsychiatry, however, was associated with a significantly greater improvement over face-to-face treatment when the study durations were 36 and 52 weeks (k = 1, n = 119, s.m.d. = −0.388, 95% CI −0.749 to −0.027, P = 0.035, and k = 1, n = 85, s.m.d. = −0.717, 95% CI −1.157 to −0.278, P = 0.001 respectively; between-group P = 0.039). We performed an exploratory subgroup analysis by baseline severity of depressive symptoms (Supplementary Table S5). The results showed no significant difference between subgroups.
Publication bias
The publication bias for the primary outcome was assessed using funnel plots, fail-safe estimates and Egger's tests (Supplementary Fig. 1).
The funnel plot was asymmetrical when all the diagnoses were combined. Subsequently, we used the trim-and-fill method to adjust for potential publication biases and found that the effect sizes were similar after adjustment and that the significance of the s.m.d. did not change (Supplementary Fig. S1A).
Discussion
Telepsychiatry has been an important treatment option for patients in underserved areas, for those who do not have access to a nearby specialist or for those who have difficulty leaving their houses because of physical or psychiatric symptoms. As a result of the COVID-19 pandemic, however, telepsychiatry has attracted more attention than ever before because of the need to maintain social distance, and it has become a major mode of delivering psychiatric care in many countries. Although attention to and the importance of telepsychiatry are growing, evidence regarding whether telepsychiatry is as effective as face-to-face treatment and the psychiatric disorders for which telepsychiatry is particularly beneficial or unsuitable remains insufficient. Therefore, we conducted a systematic review and meta-analysis of RCTs comparing the efficacy of telepsychiatry with face-to-face treatment for various psychiatric disorders. To the best of our knowledge, this is the largest meta-analysis on telepsychiatry to include multiple psychiatric disorders, enabling a comparison of the efficacy of treatment methods among disease types for the first time.
Efficacy and treatment discontinuation: all studies combined and depression alone
The results of our meta-analysis suggest that telepsychiatry is mostly equivalent to face-to-face treatment in terms of both efficacy and study completion rate when a wide range of common psychiatric disorders, including depressive disorders, PTSD, insomnia and eating disorders, are considered collectively. When all studies examining all diagnoses were combined, no significant differences in 27 of the 29 outcomes, including the primary outcome, were found between telepsychiatry and face-to-face treatment. For the remaining two outcomes (service delivery perception (SDP) likelihood of referring a friend and SDP overall satisfaction), telepsychiatry was superior to face-to-face treatment .
On the other hand, telepsychiatry and face-to-face treatment were not necessarily equivalent when these two services were evaluated according to disease type. Regarding treatment efficacy, telepsychiatry was significantly more advantageous, compared with face-to-face treatment, for the treatment of depressive disorders. In addition, a sensitivity analysis showed that the longer the duration of the study for depressive disorders, the greater the effect size of telepsychiatry. We do not know the exact reason why longer treatment duration is more effective in depression; we did not find a relative increase in all-cause discontinuation compared with face-to-face treatment, but it is possible that the quality of treatment may have been enhanced by the fact that it was conducted in the patient's home and that more information about their home life was available over the long treatment period. It would be useful for future studies to examine in more detail other factors that might influence treatment efficacy.
Risk of bias
There may be a patient selection bias of ‘patients with mild disorder’ when it comes to being able to participate in telepsychiatry. Therefore we conducted a subgroup analysis based on severity of depressive symptoms. This identified no statistically significant differences between the subgroups, suggesting that greater severity of depressive symptoms would not necessarily preclude the implementation of telepsychiatry, but may result in smaller differences in efficacy when compared with face-to-face treatment.
Furthermore, telepsychiatry was significantly superior to face-to-face treatment in terms of all-cause treatment discontinuation in a study examining participants with MCI or VCI. This result is of particular interest because it suggests that a lack of direct contact with a physician is not necessarily an obstacle affecting the continuation of treatment in people with MCI. Although it is impossible to mask either healthcare providers or patients in a study such as this one, which compares different modes of care, such an unmasked study environment may have worked to the advantage of telepsychiatry proponents. By having raters for the studies masked on allocated arms such bias could be avoided, but we did not find a single study that applied such a design (Supplementary Table S6).
Efficacy and treatment discontinuation: eating disorders, substance misuse
Telepsychiatry was significantly inferior, compared with face-to-face treatment, for improving symptom scale scores among participants with eating disorders. In addition, telepsychiatry had a significantly higher discontinuation rate, compared with face-to-face treatment, for people with substance misuse. The reason for the inferiority of telepsychiatry in the treatment of these disorders is unknown. However, telepsychiatry might be unsuitable for the treatment of diseases that are likely to have higher rates of discontinuation and lower levels of motivation to receive treatment. In fact, the numbers who dropped out in studies examining these diseases were higher than in studies examining other diseases included in the current analysis. However, with the exception of depressive disorders and PTSD, the numbers of studies analysing other diseases were relatively small or were limited to only one study, and the possibility that this relationship was an incidental finding cannot be ruled out. Nevertheless, these results suggest that there are some disorders for which telepsychiatry is more beneficial and others for which it is not necessarily beneficial, suggesting that telepsychiatry protocols should be tailored to specific disease groups.
Duration of treatment, treatment augmentation and challenges of telepsychiatry
Given that psychiatric disorders typically have a chronic course and require long-term treatment, the efficacy of long-term telepsychiatry treatment is an interesting and important question. However, we cannot discuss the risk–benefit trade-off for the long-term use of telepsychiatry accurately, since all the RCTs included in this analysis had relatively short durations (mean 23.7 weeks) and all were shorter than 1 year. For example, questions have been raised regarding the effects on therapeutic relationships over the long term.Reference Grady, Myers, Nelson, Belz, Bennett and Carnahan15 Telepsychiatry may take a longer time to establish a good rapport between patient and physician and may lessen the quality of the rapport that is established, compared with in-person care.Reference Kinoshita and Kishimoto25
Since the number of patients receiving long-term telepsychiatry is expected to increase as a result of the COVID-19 pandemic, it may be useful to examine the results of long-term, real-world clinical practice pragmatically for a variety of psychiatric disorders and patient subgroups within each disorder category.
Combining telepsychiatry with other eHealth tools, such as self-monitoring tools and/or treatment apps, could potentially improve treatment efficacy. On the other hand, the implementation of telepsychiatry poses challenges in terms of technical, legal, social and ethical aspects. In particular, the digital inclusion of users (both access to tools and appropriate connectivity, as well as the ability to use them) seems to be a decisive factor in the success of telepsychiatry practices.
Limitations
The results of the present analysis should be interpreted with consideration of the following limitations. First, the number of studies and the sample size per study were mostly small: except for PTSD and depressive disorders, most of the diseases had only one RCT. Therefore, the results of the present study should be treated with caution with regard to the superiority of telepsychiatry over face-to-face treatment for individual diseases with a small number of studies.
Second, none of the studies were conducted for longer than 1 year. Thus, the present results do not provide insight into whether telepsychiatry can be as effective as face-to-face treatment when performed over the long term.
Third, there was insufficient consideration of the impact of the quality of communication. A system with professional specifications and no communication delays would naturally provide the same therapeutic effect as a face-to-face treatment (although there would be some disadvantages such as not being able to see the whole body and not being able to smell it), but on a small screen, where the communication tends to be choppy, the therapeutic effect may be less good. On the other hand, recent smartphones may be able to achieve clear and low-latency communication even with small screens. We thought of verifying this in our subgroup analysis. However, we were unable to do so as some of the studies did not provide details of the equipment used. In future, it may be necessary to examine screen size, sound quality, communication delay, etc. in a single study and to establish criteria such that if a certain level of quality is not met, telepsychiatry will not be acceptable.
Fourth, data on many relevant clinical variables, such as adherence to medication therapy, quality of rapport (therapeutic alliance) and presence of comorbidities, were not available, and these variables should be considered in future analyses.
In addition, it should be noted that prior to the COVID-19 pandemic, telemedicine, including telepsychiatry, had many restrictions related to the prescription of drugs; these restrictions may have limited the feasibility of conducting research and of using telemedicine as a treatment option, compared with face-to-face treatment.Reference Kinoshita, Cortright, Crawford, Mizuno, Yoshida and Hilty26 As deregulation progresses and conditions related to telemedicine implementation improve, it is expected that high-quality comparative studies will be conducted with more consistent conditions for both telemedicine and face-to-face treatment.
Implications
Technological innovations have enabled early disease detection and treatment optimisation in psychiatry. With the combination of such innovations, telepsychiatry is expected to improve as a means of providing medical care to people with psychiatric disorders and of supporting their caregivers in the COVID-19/post-COVID-19 era.
Supplementary material
Supplementary material is available at https://doi.org/10.1192/bjp.2023.86.
Data availability
As a meta-analysis, this study used data already reported in primary literature. Derived data used to calculate meta-estimates are available on request from the corresponding author.
Author contributions
T.K. and K.H. designed the study. T.K., K.H., S.Kurokawa, S.F., Y.E., M.F., A.T. and S.Kinoshita performed the literature search and extracted data. All authors had access to all the data. K.H. and T.K. analysed data and verified them. T.K. and K.H. drafted the paper and all authors critically reviewed the manuscript.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
K.H. is an employee of Sumitomo Pharma. S. Kurokawa reports personal fees from Sumitomo Pharma, outside the submitted work. A.T. has received grants from Keio University Medical Science Fund and Kanae Foundation for the Promotion of Medical Science. M.F. reports personal fees from Daiichi Sankyo and Towa pharmaceutical, outside the submitted work. S.F. reports personal fees from Sumitomo Pharma, outside the submitted work. Y.E. is an employee of Benesse Style Care Co. and reports personal fees from Eisai and Otsuka Pharmaceutical. T.K. reports personal fees from Banyu, Eli Lilly, Janssen, Kyowa Pharmaceutical Industry, Lundbeck, Novartis, Otsuka, Sumitomo Dainippon, Takeda, grants from Sumitomo Dainippon, Otsuka, i2medical, eMind, I'mbesideyou, outside the submitted work. He also reports research funds from MICIN outside the submitted work.







eLetters
No eLetters have been published for this article.