Urinalysis and urine cultures are routinely overused and misinterpreted in a variety of clinical settings. Reference Advani, Gao and Datta1 Inappropriate urine testing is a major driver of unnecessary antibiotic use, increased healthcare utilization, associated adverse events, and unnecessary costs. Reference Petty, Vaughn and Flanders2
Urinalysis parameters are often used by clinicians and laboratories to determine whether urine cultures should be performed or whether treatment is indicated in cases of suspected urinary tract infection (UTI). Reference Fakih, Advani and Vaughn3 On recent surveys of academic and community hospitals, almost 50% of hospitals and laboratories used reflex urine culture approaches (also referred to as urinalysis with reflex to culture). Reference Sullivan, Morgan and Leekha4,Reference Ling, Seidelman and Dodds-Ashley5 In this approach, when a urinalysis is ordered, the urine specimen is automatically processed for culture if specific urinalysis parameters (eg, leukocyte esterase, white blood cells (WBC), or bacteria) are positive. Reference Humphries and Dien Bard6 Some hospitals used a combination of several different urinalysis criteria for reflexing, while others used a single criterion. Reference Sullivan, Morgan and Leekha4,Reference Ling, Seidelman and Dodds-Ashley5 There is no consensus on which urinalysis parameters should be used for reflexing or which populations are suited for this test. Reference Ling, Seidelman and Dodds-Ashley5 Most laboratories accept all urine specimens (eg, catheterized specimens) for reflexing, which may be an inappropriate practice. Reference Sullivan, Morgan and Leekha4–Reference Humphries and Dien Bard6 Therefore, efforts are needed to identify and validate urinalysis criteria for use in reflex urine cultures and to identify populations best suited for reflex urine cultures. Reference Fakih, Advani and Vaughn3
Our objectives were (1) to compare the performance of different urinalysis parameters in predicting significant bacteriuria irrespective of symptoms and (2) to assess the negative predictive value (NPV) of pyuria based on age, sex, setting, and presence of indwelling catheter. More importantly, our overall goal is to provide guidance to existing laboratories that perform reflex urine cultures related to urinalysis parameters and populations that are best suited for reflexing.
Methods
Design
This retrospective cohort study included all patient encounters (inpatient and outpatient) with paired urinalysis and urine cultures (urinalysis ordered ≤24 hours prior to urine culture) between January 1, 2015, and December 31, 2020. The laboratory did not employ a reflex urine culture approach during the study. This study was considered exempt by Duke University Institutional Review Board (protocol no. 00107418).
Setting
This study was conducted in North Carolina at 3 hospitals and >150 outpatient clinic sites. The hospitals included one academic medical center with 1,048 beds, and 2 community hospitals with 186 beds and 369 beds, respectively.
Outcomes and definitions
Our outcome of interest was “significant bacteriuria,” defined as a urine culture with ≥1 uropathogen growing at ≥100,000 colony-forming units (CFU)/mL. Negative cultures were defined as urine cultures with no bacterial growth. Mixed urine cultures were defined by Duke University Microbiology Laboratory as the presence of 2 or more organisms when all organisms were nonsignificant (not a known uropathogen) or when one of the organisms was considered a significant uropathogen but was in lesser quantity (∼10-fold fewer) than the concentration of the nonsignificant organisms (eg, 1,000 CFU/mL significant organisms compared with 10,000 CFU/mL of nonsignificant organisms). Reference Whelan, Nelson and Kim7 Low-level pyuria on urinalysis (predictor variable of interest) was defined as WBC ≥ 5 per high-powered field (hpf). Low-level bacteriuria on urinalysis was defined as 5–50 bacteria per hpf.
Analysis
We evaluated the performance characteristics [ie, sensitivity, specificity, NPV and positive predictive value (PPV)] of relevant urinalysis parameters (pyuria, leukocyte esterase, nitrite, and bacteria) for predicting significant bacteriuria based on prior evidence. Reference Sullivan, Morgan and Leekha4,Reference Ling, Seidelman and Dodds-Ashley5 We further assessed the NPV of pyuria across different groups: catheterized versus noncatheterized patients, male versus female, and age <65 or ≥65 years. We also combined 18 different urinalysis criteria and used receiver operating characteristic (ROC) curves to identify the top five performing models for predicting significant bacteriuria (based on sensitivity and specificity) (Fig. 1).

Fig. 1. Different combinations of Urinalysis parameters in predicting significant bacteriuria.
Results
In total, 221,933 encounters met inclusion criteria in the study period. During these encounters, 84,334 (38%) specimens were obtained from outpatient clinics and 22,584 (10.2%) specimens were obtained from catheterized patients. Twenty-nine percent of urine cultures were positive, 30.7% were negative, and 46.9% grew mixed flora.
No single urinalysis parameter had both high sensitivity and high specificity. Trace leukocyte esterase and low-level pyuria (WBC ≥ 5) had low specificity (55%) but high sensitivity (87% and 78%, respectively). However, sensitivity decreased with increasing degree of pyuria and leukocyte esterase. Similarly, bacteria on urinalysis had low specificity (37%) and high sensitivity (93%), but sensitivity decreased with increasing degree of bacteriuria (77%). Nitrite had low sensitivity (41%) but high specificity (95%, Table 1). When examining UA parameters for their NPV, trace leukocyte esterase, low-level pyuria and low-level bacteriuria had a high NPV (≥90%, Table 1).
Table 1. Performance of Individual Urinalysis Parameters for Predicting Significant Bacteriuria
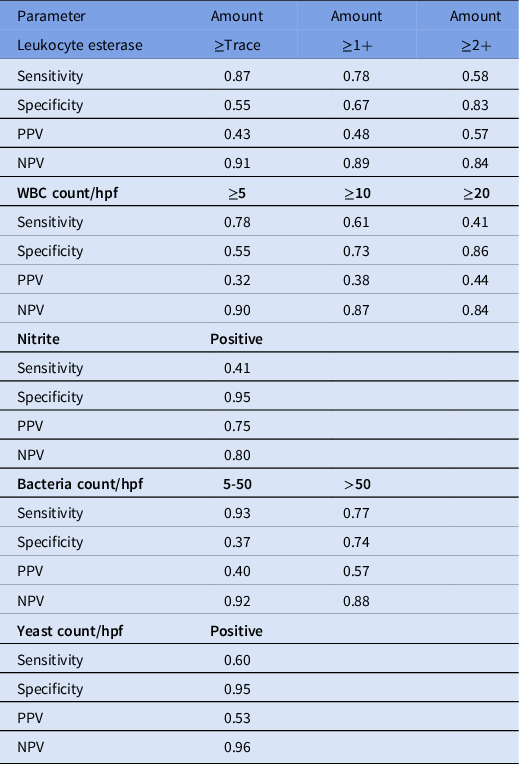
Note. WBC, white blood cell; hpf, high-powered field; PPV, positive predictive value; NPV, negative predictive value.
Combined urinalysis parameters did not perform much better than leukocyte esterase or pyuria in terms of NPV (Table 2). However, NPV of pyuria differed significantly between age and sex groups, with best performance in males <65 and worst performance in females ≥65 (Table 3). Additionally, NPV of pyuria (WBC ≥ 5) was lower in catheterized versus noncatheterized samples (0.87 vs 0.91) but was ≥90 in both inpatient and outpatient settings (Table 3 and Supplementary Tables 1 and 2 online).
Table 2. Complete Parameter Estimates for the 5 Models with the Best Area Under the Receiver Operating Characteristic Curve (AUROC) Performance

Note. WBC, white blood cell; hpf, high-powered field; PPV, positive predictive value; NPV, negative predictive value.
Table 3. Comparing Negative Predictive Value of Pyuria Based on Age, Sex, Location, and Source of Collection

Note. Hpf, high-powered field, WBC- White blood cells
Discussion
Our findings show that absence of leukocyte esterase and pyuria had a high NPV for significant bacteriuria, and combination urinalysis parameters did not perform better than pyuria or leukocyte esterase alone in terms of NPV. Additionally, this is the first study to highlight that performance of pyuria as a clinically relevant predictor differs by age and sex. Specifically, we show that the high NPV of pyuria was maintained in males and in noncatheterized specimens. These findings also suggest that reflex urine culture strategies may not be best suited for use in older females and persons with indwelling catheters.
Low-level bacteriuria on urinalysis also had a high NPV; however, the presence of bacteria on urinalysis cannot discriminate between viable or nonviable organisms and pathogenic or nonpathogenic organisms. Reference Advani, Polage and Fakih8 Hence, presence of bacteria on urinalysis, despite its high NPV, should not be used as a single inclusion or exclusion criteria in reflex urine cultures. Additionally, as combination urinalysis parameters did not perform better than pyuria alone, it is unclear what utility, if any, bacteria on urinalysis will serve in the future.
Based on these findings, how can reflex urine culture practices be optimized in hospitals and laboratories? First, our prior work has shown that reflex urine cultures should not be used to diagnose UTIs but rather to reduce laboratory burden. Reference Fakih, Advani and Vaughn3,Reference Ling, Seidelman and Dodds-Ashley5,Reference Advani and Vaughn9 Discrete orderable tests for urinalysis, reflex urine cultures, and direct urine cultures should be created in the electronic medical record, and appropriate patient selection should be done in the ordering or preanalytic phase. Reflex urine cultures should be directed toward symptomatic patients, either through clinical decision support or by educating ordering clinicians. Reference Advani and Vaughn9 To this effect, urinalysis parameters in a reflex urine culture should be based on their NPV. Reference Ling, Seidelman and Dodds-Ashley5 Secondly, our data suggest that low-level pyuria (WBC ≥ 5) or trace leukocyte esterase may be adequate as single criterion in reflex urine culture algorithms if leveraged for its NPV to avoid unnecessary urine cultures. Deciding between pyuria and leukocyte esterase will depend on types of urinalysis tests available (ie, microscopic vs dipstick). Third, laboratories should avoid the use of reflex urine culture strategies in specific patient populations, such as older women and catheterized patients, due to poor NPV of pyuria. Neonates or patients who are neutropenic, pregnant, or undergoing urologic procedures should be excluded from reflex testing protocols as these populations may either need treatment for asymptomatic bacteriuria (ASB) or may not display pyuria on urinalysis. Reference Ling, Seidelman and Dodds-Ashley5,Reference Advani and Vaughn9 Last, laboratories should validate these findings on their own data to better optimize the local performance of reflex urine cultures. We recommend that institutions at least use include pyuria or leukocyte esterase (depending on availability of microscopic vs dipstick urinalysis) and nitrite when assessing the local performance of reflex urine cultures within their populations.
Our study had several limitations. Our study hospitals and clinics are based in North Carolina, and our findings may have limited generalizability. Overall, >40% of our samples grew mixed urine cultures, but this finding is consistent with rates of mixed urine cultures reported by other large academic medical centers and outpatient clinics. Reference Whelan, Nelson and Kim7 Our data on risk factors for mixed urine cultures have been previously described, but these studies did not include data on delays in collection or transport across the health system. Reference Whelan, Nelson and Kim7 We could not include all urinalysis orders in our analyses; instead we paired urinalysis with urine cultures ordered within a 24-hour period to replicate how clinicians and laboratories would use reflex urine cultures in real life. Lastly, we were not able to assess for ASB versus UTI, and instead used significant bacteriuria as our outcome for 2 reasons. There is no consistent definition for clinical UTI across national infectious disease and urologic societies, and the definition of clinical UTI has been evolving over the past decade. Reference Fakih, Advani and Vaughn3,Reference Advani, Lee, Schmitz and Camins10–12
In conclusion, future reflex urine culture workflows and diagnostic stewardship algorithms should focus on populations in which the absence of pyuria has a high NPV. Our next steps will include incorporating population specific criteria into reflex urine-culture algorithms and examining the impact on urine cultures and antibiotic use. More data are needed to better understand how to incorporate specific WBC thresholds into reflex workflows for populations, specimen types (catheterized vs noncatheterized), and test type (microscopic vs dipstick). As we move away from a one-size-fits-all model for interpretation of urinalysis criteria, our findings will help optimize reflex urine cultures by using a population specific approach to diagnostic stewardship.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/ice.2022.315
Acknowledgments
Financial support
This research was funded by the SHEA Research Scholar Award awarded to S.D.A. Part of S.D.A.’s time is also funded by National Institutes of Health (grant no. NIDDK K12DK100024).
Conflicts of interest
S.D.A. reports grants from the Centers for Disease Control and Prevention (Prevention Epicenters Program 5U54CK000616-02; SHEPheRD 75D30121D12733-D5-E003) and Duke Claude D. Pepper Older Americans Independence Center (grant no. NIA P30AG028716), consulting fees from Locus Biosciences, Sysmex America, GSK, IDSA, bioMérieux, and is a co-owner of IPEC Experts, LLC (unrelated to this grant). All other authors report no conflicts of interest relevant to this article.







