Introduction
Social disinhibition is becoming increasingly recognised in the neuropsychological literature as a complex and debilitating sequalae associated with acquired frontal lobe damage (Croker & McDonald, Reference Croker and McDonald2005; Green et al., Reference Green, Turner and Thompson2004). Although there is no consensual definition of social disinhibition, it can be broadly understood as the inability to supress socially inappropriate verbal, physical, or sexual acts in order to conform with social or cultural behavioural norms (Kocka & Gagnon, Reference Kocka and Gagnon2014). The impact of social disinhibition on both the individual and those around them, such as carers, partners, or family members, can be profound. For the person with the acquired damage, the difficulties may result in reduced quality of life, poorer rehabilitation outcomes, increased psychopathology, and difficulties establishing and maintaining relationships (Gould et al., Reference Gould, Ponsford, Johnston and Schonberger2011; Hoofien et al., Reference Hoofien, Gilboa, Vakil and Donovick2001; Honan et al., Reference Honan, Allen, Fisher, Osborne-Crowley and McDonald2016; Winkler et al., Reference Winkler, Unsworth and Sloan2006). Family, caregivers, and partners can also experience reduced quality of life, increased carer burden, increased psychopathology, and long-term distress (Gould et al., Reference Gould, Hick, Hopwood, Kenardy, Krivonos, Warren and Ponsford2019; Livingston et al., Reference Livingston, Brooks and Bond1985; Marsh et al., Reference Marsh, Kersel, Havill and Sleigh2002; Qadeer et al., Reference Qadeer, Choudry, Amin, Murtaza, Khaliq and Shoaib2017). Although outcomes associated with social disinhibition difficulties are becoming well-documented, opinions regarding the identification and assessment of these difficulties remain divided. This is likely, in part, due to the way in which social disinhibition has been conceptualised, described and examined in both clinical and research contexts.
Several different terms have been used to describe behaviours consistent with the concept of social disinhibition, including impulsivity and behavioural dysregulation. Whilst these terms are often used interchangeably, they are also used by others to describe separate behavioural constructs. For example, some authors will refer to impulsivity when describing socially disinhibited behaviours whereas others will describe impulsivity and social disinhibition as being two separate constructs. This lack of standard and consistent use of the term ‘social disinhibition’ is a potential source of confusion for those researching and working with individuals who exhibit these behaviours, the implications of which may include broad and inaccurate estimates of incidence and prevalence, non-targeted (and potentially inappropriate) rehabilitation programmes, and a general lack of understanding of this pervasive and disabling difficulty. Clarification of the concept of social disinhibition has the potential to refine knowledge of its constituent behaviours and to progress further research and treatment practices in the area. The purpose of this paper is to explore and examine the concept of social disinhibition in the context of brain injury and other organic neurological conditions. Whilst the terms that are frequently used interchangeably with social disinhibition will not be specifically examined as part of this analysis, a definition of each of these terms and how they fit within the context of social disinhibition will be provided to aid clarity. The methods described by Walker & Avant (Reference Walker and Avant2019) will be employed to undertake this analysis.
Concept analysis
Concept analysis refers to a process by which a vague, ambiguous, or underdeveloped concept is explored with the objective of improving clarity (Hughes & Duffy, Reference Hughes and Duffy2018). According to Walker & Avant (Reference Walker and Avant1994, pg. 38), concept analysis is “a process of determining the likeness and unlikeness between concepts” and its “basic purpose is to distinguish between the defining attributes of a concept and its irrelevant attributes”. Whilst concept analysis originated in the field of mathematics, it is now a widely used method within the health and medical fields (Hughes & Duffy, Reference Hughes and Duffy2018). Thus, our objective was to gain a greater understanding of how ‘social disinhibition’ as a term has been defined within the literature (relating to brain injury and other neurological conditions) through the process of concept analysis. We also aimed to develop a clearer definition of the concept of social disinhibition within the context of acquired brain injury and other neurological conditions.
Method
Walker & Avant’s (Reference Walker and Avant2019) concept analysis framework has been selected for this analysis due to its successful use in analysing concepts within the healthcare literature (e.g., Meeberg, Reference Meeberg1993; Ridner, Reference Ridner2004). The framework comprises eight steps: select a concept; determine the purpose of the analysis; identify all uses of the concept; determine the defining attributes; construct a model case; construct borderline and related cases; identify antecedents and consequences; and define empirical referents.
Two separate systematic searches for articles published in the English language from journal inception to June 2021 were conducted using MEDLINE, PsycINFO, Embase (via OVID) CINAHL (via EBSCOhost) and Web of Science databases. The purpose of the first search was to extract publications relating to social disinhibition among individuals with an organic neurological condition (e.g., Williams syndrome, frontotemporal dementia). The purpose of the second search was to extract publications relating to social disinhibition among individuals with an acquired brain injury. This approach was taken to provide insight into differences and/or similarities in conceptualisation and use of the concept across different neurological populations for which there may be damage or significant organic alterations to regions of the brain that are thought to underlie socially disinhibited behaviours.
Medical Subject Headings (MeSH) were used and combined with relevant search terms (e.g., ‘social disinhibition’, ‘brain injury’, ‘acquired brain injury’, and ‘head injury’). Database specific Boolean operators and truncations were used to capture all appropriate use across the literature (for the full search strategy, see supplementary material). The reference list of all articles were also reviewed to identify any additional relevant citations. While terms such as ‘disinhibition’ and ‘behavioural dysregulation’ may be used in the context of social behaviours (e.g., Hanna-Pladdy, Reference Hanna-Pladdy2007), ‘social disinhibition’ was the only term (relating to disinhibited behaviours in a social context) used as part of the search strategy. This enabled us to identify how social disinhibition as a term and behaviour (our construct of interest in this paper) has specifically been defined and used in the current literature. The inclusion of broader terms returned items that were not describing social behaviours (e.g., neural response inhibition) or were reflective of neural processing more generally (e.g., inhibition of neuronal responses), and thus was not conducive to our focused search. Including ‘social’ as a conditioner to ‘disinhibition’ permitted us to screen out irrelevant content. Extending on this focused systematic search, we did find some evidence in the literature of terms, such as behavioural dysregulation and impulsivity, that have been used to describe behaviours consistent with social disinhibition (e.g., Hanna-Pladdy, Reference Hanna-Pladdy2007). While a systematic examination of these items could not be conducted (i.e., due to the lack of specific use of terminology), they were identified as part of broader reading and discussed in the context of our findings related to our focused search on ‘social disinhibition’. Given the focused search and desire to explore how this concept is used in brain injury and neurological populations, publications relating to personality types and/or personality disorders, as well as those relating to psychological disorders, such as schizophrenia and bipolar disorder, were not included.
All publications were imported into Covidence and duplicates were automatically removed. Two of the authors (SS and CP) independently screened the title and abstract of each publication (and when necessary, full-text) for inclusion or exclusion. Where there were disagreements regarding the inclusion of a publication, SS and CP were able to reach a consensus.
Data analysis and screening
A summary of the process by which publications were included in this concept analysis is shown in Fig. 1. A total of 284 publications were retrieved from the initial electronic database search. Following the removal of duplicates, a total of 153 publications were screened by reviewing the title and abstract. Of these, 44 were selected for full-text review, one of which was found as part of an updated search to ensure currency immediately prior to publication. Six additional publications were identified through manual searching of reference lists and included in the analysis.

Figure 1. Process of inclusion of literature in the concept analysis.
The first author read all included publications (N = 22) in full, paying particular attention to the conceptualisations, defining attributes, antecedents, and consequences. The following inclusion criteria were used when determining whether to include an article in the analysis: (1) the article was published in a peer-reviewed journal, (2) contained the results of human studies, (3) the participants in the study were adults, (4) the article was published in English, (5) the research mentioned social disinhibition by name at some point throughout the manuscript (i.e., title, abstract, keywords, or in the body of the paper), (6) the study sample were brain injured individuals and/or other neurological groups (e.g., William’s syndrome, fronto-temporal dementia), and (7) the research was published from journal inception to June 2021.
Analytic questioning (Ikuenobe, Reference Ikuenobe2013) was employed when examining the data (information about the concept provided by the authors) to gain greater insight into how the concept of social disinhibition had been interpreted in the relevant brain injury/neurological literature. Questions included: “How was social disinhibition defined by the author?”; “Were there degrees of social disinhibition?”; “Are there different types of social disinhibition?”; and “How was social disinhibition measured?”.
Definitions and uses of the term “social disinhibition”
While it was frequently asserted that social disinhibition is a common and disabling outcome associated with frontal lobe impairment (Osborne-Crowley & McDonald, Reference Osborne-Crowley and McDonald2018), there was no clear universal definition referred to across the 22 included papers in this review. Table 1 contains a summary of definitions provided in each included article. We argue that given a taxonomy of socially disinhibited behaviours does not currently exist, the identification of an appropriate universal definition is difficult. However, based on the papers included in this analysis, a taxonomy of behaviours as they occur within the brain injury and neurological populations has been proposed (see Fig. 2). It is hoped that this taxonomy, along with the definition later provided, will provide a stronger understanding of what social disinhibition is and how it may present.
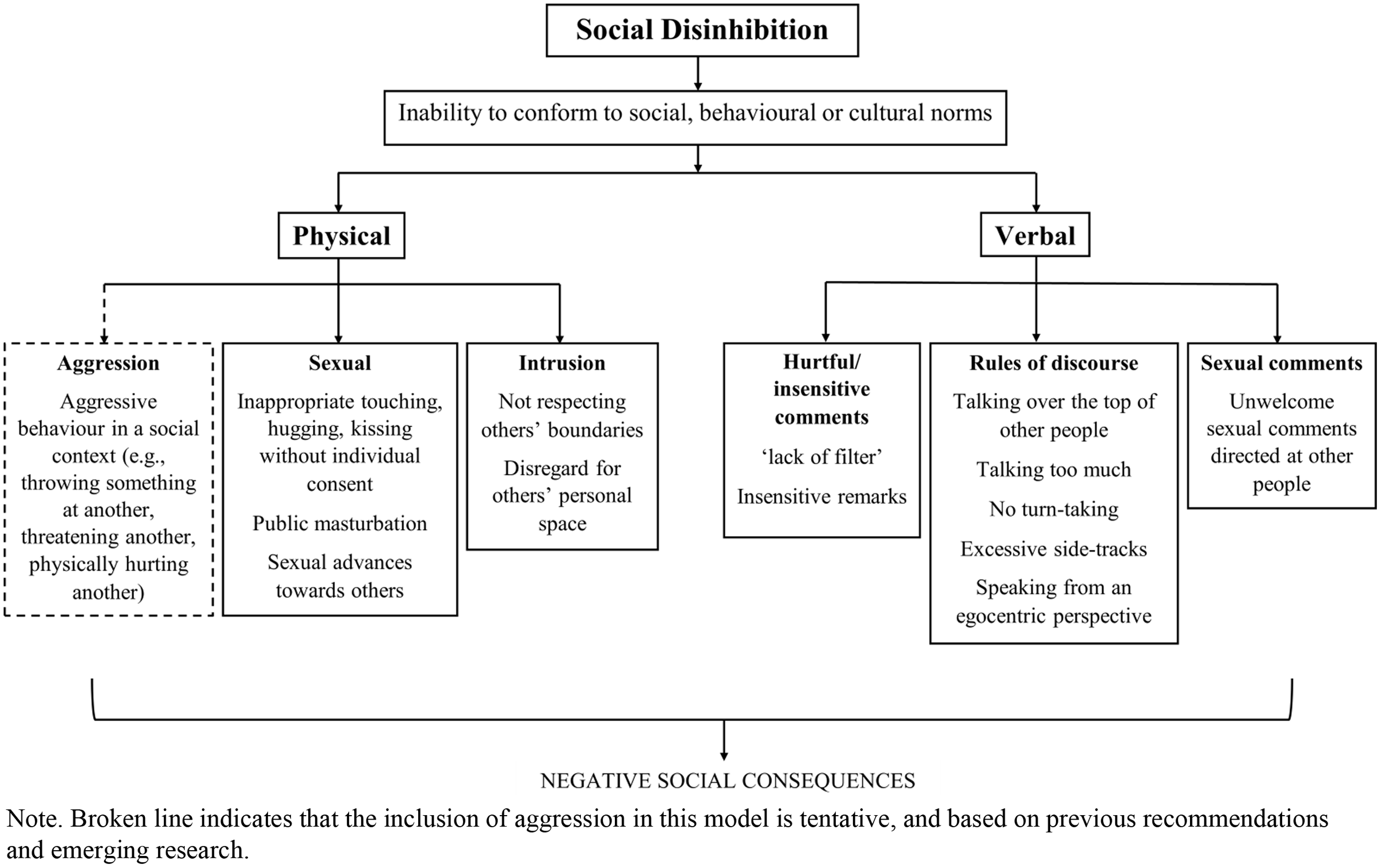
Figure 2. Proposed taxonomy of socially disinhibited behaviours.
Table 1. Summary of all included articles

Note. Behaviours consistent with social disinhibition refer to those behaviours that are reflective of social disinhibitory behaviour but that are not specifically noted by the authors as such.
Among many neurological groups with compromised cognitive functioning (e.g., brain injury, frontotemporal dementia, William’s syndrome), social disinhibition has been described as encompassing inappropriate physical behaviours such as hugging, kissing or touching of others (particularly strangers) without their consent, hurtful or socially inappropriate comments (often described as a ‘lack of filter’), lack of manners, unacceptable sexual acts (e.g., public masturbation or sexual advances), immaturity, a lack of respect for others’ boundaries, insensitivity towards others, and a lack of understanding around rules of discourse (e.g., talking over the top of other people, talking too much, no turn-taking) (Honan et al., Reference Honan, Allen, Fisher, Osborne-Crowley and McDonald2016; Kelly & McDonald, Reference Kelly and McDonald2020; Osborne-Crowley, McDonald, & Francis, Reference Osborne-Crowley, McDonald and Francis2016; Osborne-Crowley & McDonald, Reference Osborne-Crowley and McDonald2018; Osborne-Crowley et al., Reference Osborne-Crowley, McDonald and Rushby2016; Porter et al., Reference Porter, Coltheart and Langdon2007; Saxon et al., Reference Saxon, Thompson, Jones, Harris, Richardson, Langheinrich, Neary, Mann and Snowden2017).
In other clinical populations, specifically Tourette’s syndrome, social disinhibition is regarded quite differently. Here, individuals endorsing behaviours such as coprolalia (repetitive use of obscene language), copropraxia (inappropriate touching), echolalia (repetition of vocalisations made by other people), animal noises, bending and gyrating (e.g., bending over, rotating or spinning on one foot) are referred to (Hirschtritt et al., Reference Hirschtritt, Darrow, Illmann, Osiecki, Grados and Sandor2016). What does appear to be consistent across much of the literature, however, is that social disinhibition reflects an inability to conform to social and/or cultural behavioural norms (Arciniegas & Wortzel, Reference Arciniegas and Wortzel2014).
Interestingly, a number of authors mention the presence of social disinhibition but fail to provide a definition and/or behavioural examples (Benhamou et al., Reference Benhamou, Marshall, Russell, Hardy, Bond, Sivasathiaseelan, Greaves, Friston, Rohrer and Warren2020; Chan et al., Reference Chan, Anderson, Pijnenburg, Whitwell, Barnes and Scahill2009; Frigerio et al., Reference Frigerio, Burt, Gagliardi, Cioffi, Martelli, Perrett and Borgatti2006; Järvinen-Pasley et al., Reference Järvinen-Pasley, Bellugi, Reilly, Mills, Galaburda, Reiss and Korenberg2008; Klein-Tasman et al., Reference Klein-Tasman, Li-Barber and Magargee2011; Laws & Bishop, Reference Laws and Bishop2004; Morris, Reference Morris2010; Rankin et al., Reference Rankin, Mayo, Seeley, Lee, Rabinovici and Gorno-Tempini2011; Shoumitro et al., Reference Shoumitro, Lyons and Koutzoukis1999; Skwerer et al., Reference Skwerer, Borum, Verbalis, Schofield, Crawford, Ciciolla and Tager-Flusberg2009). Similarly, others describe behaviours consistent with social disinhibition, however fail to recognise them as such (Davies et al., Reference Davies, Howlin and Udwin1998). It is reasonable to assume that the lack of consistent definition (both within disciplines and across brain injury/neurology groups) and confusion surrounding what behaviours constitute social disinhibition, has resulted in some authors and researchers avoiding the use of the term altogether.
It is important to note that aggression has also been proposed as being reflective of social disinhibition, although there is currently a lack of empirical support in the literature for this claim (Osborne-Crowley & McDonald, Reference Osborne-Crowley and McDonald2018). Two types of aggression are commonly reported in the TBI literature; namely, impulsive aggression and episodic aggression (Wood & Thomas, Reference Wood and Thomas2013). Episodic aggression is typically characterised by an ‘explosive rage’ and is often not precipitated by any kind of stimulus. Individuals with episodic aggression reportedly express remorse for their behaviour and return to ‘normal’ social functioning in between episodes. Alternatively, impulsive aggression is characterised by verbal or physical behaviours that typically stem from feelings of irritability, agitation and emotional fragility. Whereas episodic aggression is thought to typically occur as a result of neuronal dysfunction in the temporal lobe, impulsive aggression has been attributed to deficits in inhibitory control resulting from impaired modulatory mechanisms in the prefrontal cortex (Wood & Thomas, Reference Wood and Thomas2013). These modulatory mechanisms seen in impulsive aggression are also implicated in social disinhibition (Douglas, Reference Douglas2010), suggesting that there may be overlap between the two constructs. We propose that impulsive aggression, when it occurs in a social context, may constitute social disinhibition. This tentative claim is denoted by a dotted line in Fig. 2. Given the current lack of direct empirical support, future studies are needed to delineate the likely overlap between aggression and social disinhibition.
Interchangeable use between constructs
Further complicating the issue of a consistent definition is the use of interchangeable terms. Prior to conducting the search strategy, a broad scan of the literature revealed several terms that are frequently used synonymously with social disinhibition. These include impulsivity and behavioural dysregulation, with impulsivity and social disinhibition being most frequently interchanged. For example, in a study examining conversational abilities among individuals with a traumatic brain injury (TBI), disinhibition and impulsivity represented a single factor (saying rude or embarrassing things) (Struchen et al., Reference Struchen, Pappadis, Mazzei, Clark, Davis and Sander2008). Further, when readers are searching for ‘disinhibition’ in the book Neuropsychological Assessment they are also encouraged to refer to ‘impulsivity’ (Lezak et al., Reference Lezak, Howieson, Bigler and Tranel2012). A study conducted by Saxon et al., (2017) also referred to impulsivity as being reflective of social disinhibition. This interchangeable use of terms makes distinguishing between them difficult. Further, while there does appear to be a general consensus that impulsivity is a multidimensional construct, these dimensions seem to differ among authors (Kocka & Gagnon, Reference Kocka and Gagnon2014). For some, impulsivity is comprised of motor impulsivity (acting without thinking), cognitive impulsivity (making spontaneous decisions without thorough thought) and non-planning impulsivity (no forethought for future consequences) (Barratt, Reference Barratt1959; Patton et al., Reference Patton, Stanford and Barratt1995), whereas for others impulsivity is regarded as being a spontaneous behaviour that is either motoric (e.g., engaging in a behaviour or action without forethought for possible undesirable outcomes) or verbal (e.g., making spontaneous statements that have the potential for negative outcomes) (Votruba et al., Reference Votruba, Rapport, Vangel, Hanks, Lequerica, Whitman and Langenecker2008). Aeschleman & Imes, Reference Aeschleman and Imes1999) took a similar stance, suggesting that impulsivity can be reflected either verbally, gesturally or physically.
A completely different definition of impulsivity, however, is provided by Rochat et al. (Reference Rochat, Beni, Billieux, Azouvi, Annoni and van der Linden2010) who suggest four dimensions of impulsivity. These include urgency (the tendency to act on strong impulses), premeditation (engaging in an action or behaviour before considering the consequences), perseverance (inability to remain focused on a task that may be regarded as boring or difficult) and sensation seeking. In summary, it appears that there are many different conceptualisations of impulsivity, and consequently many different ways that the construct of impulsivity can be assessed. Given the overlap in behaviours (e.g., saying rude or embarrassing things, inappropriate tone of voice, getting “side-tracked” by irrelevant parts of a conversation) (Struchen et al., Reference Struchen, Pappadis, Mazzei, Clark, Davis and Sander2008), it is not at all surprising that we see impulsivity and social disinhibition being used interchangeably within the literature.
Behavioural dysregulation is another term often used to describe behaviours consistent with social disinhibition. Hanna-Pladdy (Reference Hanna-Pladdy2007) for example, argues that self-regulatory dysfunction can manifest in a number of ways, including behavioural disinhibition, difficulties understanding the emotional consequences of behaviour, impaired ability to recognise another individual’s perspective, and the inability to use appropriate judgements in social behaviour. Another study employed the Head Injury Behaviour Scale to compare patient and caregiver assessments of the frequency of behavioural problems following TBI (Marsh & Kersel, Reference Marsh and Kersel2006). Comprising two subscales, the Emotional Regulation subscale contains items relating to impatience, irritability, aggression, and being overly sensitive, and the Behavioural Regulation subscale contains items relating to impulsivity, apathy, poor decision making, and poor control over social behaviours. Given the direct relationship between behavioural dysregulation and social disinhibition (that is, social disinhibition occurring as a result of behavioural dysregulation), it is clear why some researchers may continue to use these two terms interchangeably rather than recognising them as two separate constructs.
Construct distinguishability
There are various sources of evidence to suggest that the above terms, and the constructs that they are intended to represent, are distinguishable. First, the theoretical origins from which these concepts are derived differ (Kocka & Gagnon, Reference Kocka and Gagnon2014). Whereas impulsivity is derived from literature relating to personality and likely reflects a particular disposition of being, (social) disinhibition is derived from the neuropsychology literature and is reflective of a loss of function following brain injury and/or neurological disease (Kocka & Gagnon, Reference Kocka and Gagnon2014). Secondly, the consequences associated with the two terms or concepts differ. Impulsivity can result in both positive and negative consequences, whereas social disinhibition typically leads to negative consequences (Kocka & Gagnon, Reference Kocka and Gagnon2014). For example, someone who is impulsive may make spontaneous financial decisions that result in immediate gratification (e.g., purchase of a luxury item), but that also may result in negative consequences (e.g., lack of finances to pay everyday bills). This is not typically true for social disinhibition with inappropriate social behaviours resulting in fractured relationships, distrust and occupational difficulties, to name a few. Finally, social disinhibition occurs within a social context and typically involves a transaction between two or more people (e.g., saying something inappropriate to another person, touching a stranger non-consensually), whereas impulsivity can occur outside of a social context and in solitude (e.g., impulsive spending as might be seen in someone experiencing a manic episode).
Behavioural and emotional dysregulation can also be distinguished from social disinhibition. First, behavioural dysregulation is often used to describe the executive cognitive processes required to inhibit or redirect behaviours rather than the actual expression of behaviours per se. Specifically, planning, flexibility, initiation and goal setting, response inhibition and inhibitory control, are thought to be the primary cognitive processes required for efficient behavioural regulation (Kocka & Gagnon, Reference Kocka and Gagnon2014). Behavioural regulation may also be dependent on successful emotional regulation. Emotion regulation concerns the ability to successfully monitor, evaluate and modify emotional reactions according to one’s environment (Selby et al., Reference Selby, Anestis and Joiner2008). Like behavioural dysregulation, emotional dysregulation reflects a series of complex cognitive processes and is typically thought to reflect poor top-down control of internal emotions (e.g., difficulty applying an appropriate strategy to prevent an outburst due to being frustrated) (Fitzgerald et al., Reference Fitzgerald, DiGangi and Phan2018; Mennin et al., Reference Mennin, Heimberg, Turk and Fresco2002). Importantly, an inability to successfully control emotions and regulate behaviour may occur in the social setting and be a response to environmental social cues. It is here in this unique social environment where we might expect to see socially disinhibited behaviours. Despite social disinhibition seemingly being a unique case of behavioural and/or emotional dysregulation that is dependent on unique social parameters, researchers continue to use these terms synonymously.
While social inhibition may in some cases be underpinned by the cognitive processes of inhibition and inhibitory control that are involved in both emotion and behaviour regulation, there is also clear involvement of social-cognitive processes, such as ToM and self-awareness (McDonald, Reference McDonald2013). A theoretical model proposed by McDonald (Reference McDonald2013) suggested that social cognition is comprised of three elements: perception/representation (e.g., perception of speech and face, representation of socially relevant movements), evaluation/interpretation (e.g., emotion recognition, emotional empathy, ToM), and regulation (e.g., emotional regulation, self-awareness, monitoring, cognitive control). The social disinhibition seen in those with a brain injury or other neurological condition is likely driven by a complex relationship between these social-cognitive processes (see Fig. 3). Understanding the relationship between these different facets of social-cognitive processes and how they relate to social disinhibition, may be the focus of future research.
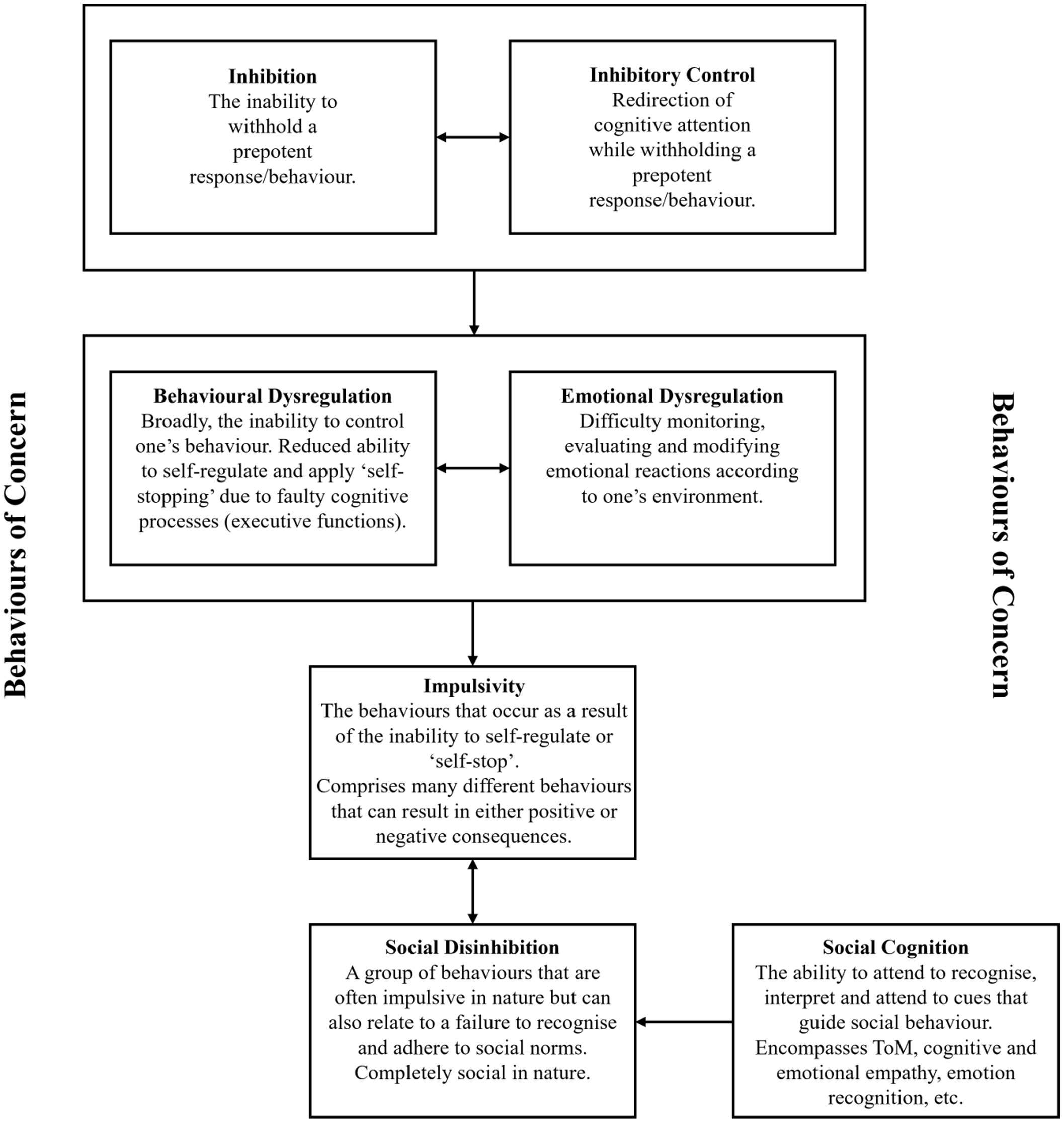
Figure 3. Proposed model of social disinhibition and related constructs.
It is evident that there are several different terms that are closely related to, and often used interchangeably with, social disinhibition. Distinguishing between these different terms or concepts is challenging because a consensual definition does not exist for any of them. Based on the findings of our systematic search of the use of the term ‘social disinhibition’ and broader reading, we propose a model that delineates these differing concepts and their underlying cognitive processes (see Fig. 3).
At the peak of the model is inhibition and inhibitory control. Whereas inhibition refers to the ability to inhibit a prepotent response, inhibitory control refers to the ability to redirect attention, behaviour, thoughts and/or emotions and instead respond in a more appropriate, goal-directed way (Diamond, Reference Diamond2013). Deficits in either one of these core executive functions can result in either behavioural or emotional dysregulation. Behavioural dysregulation represents the inability to self-regulate or ‘self-stop’ and emotional dysregulation represents difficulties monitoring, evaluating and modifying emotional reactions according to one’s environment. This dysregulation then results in impulsivity, behavioural responses that do not necessarily occur in a social context and that can result in either positive or negative consequences. At the base of the model is social disinhibition, a group of behaviours that can either be impulsive in nature (e.g., feeling and acting on an impulse to make a rude comment to another person despite understanding that it is not socially appropriate) or simply due to an inability to recognise and adhere to social norms (e.g., being emotionally reactive or making a rude comment to another person purely due to the inability to recognise that it is socially inappropriate). Social disinhibition occurs solely in a social environment and typically leads to negative social consequences. It is important to note that not everyone who experiences impulsivity will experience social disinhibition and social disinhibition does not always need to be driven by an impulse (e.g., making a hurtful comment about someone without the intention of doing so; a ‘lack of filter’). Finally, social disinhibition is largely mediated by social cognitive abilities such as emotion recognition, emotional empathy, and ToM.
Defining attributes
According to Walker & Avant (Reference Walker and Avant2019), defining attributes refer to characteristics that are most frequently associated with the concept and that allow the analyst the greatest insight into the concept. Defining attributes allow for differentiation between the concept and other related or similar concepts. Our review indicates that socially disinhibited behaviours reported within the brain injury/neurology literature are diverse and varied. Although a taxonomy of socially disinhibited behaviours has been proposed in this paper, future research should continue to focus on what other behaviours constitute social disinhibition and what behaviours are reflective of separate behavioural profiles. It is important to note that the defining attributes discussed in this paper are provisional and may change as understanding of the concept develops. In the brain injury and other neurological condition literature, the following defining attributes of social disinhibition were noted: the inability to regulate behaviour to meet social goals (Kelly & McDonald, Reference Kelly and McDonald2020), not respecting others’ boundaries and/or personal space (Porter et al., Reference Porter, Coltheart and Langdon2007), insensitivity towards other people (e.g., making inappropriate comments, sexual acts) (Arciniegas & Wortzel, Reference Arciniegas and Wortzel2014; Osborne-Crowley & McDonald, Reference Osborne-Crowley and McDonald2018), inability to conform to behavioural and cultural norms (Arciniegas & Wortzel, Reference Arciniegas and Wortzel2014), inability to respond according to social environmental contingencies (Hanna-Pladdy, Reference Hanna-Pladdy2007; Rieger & Gauggel, Reference Rieger and Gauggel2002), and a lack of understanding of ‘rules’ governing social behaviours (Osborne-Crowley & McDonald, Reference Osborne-Crowley and McDonald2018). It is important to note that minimal detail was provided in the included articles about these defining attributes. As such, expanding on each of the abovementioned points was not achieved in this present paper.
Antecedents and consequences
Antecedents refer to events or incidents that precede the occurrence of the concept (Walker & Avant, Reference Walker and Avant2019). The primary antecedent associated with social disinhibition in the context of those with a brain injury or other neurological condition is compromised activity in the orbitofrontal and lateral prefrontal cortex, and the insular and temporal regions of the brain. The acquired brain injury or neurological condition may either directly or indirectly affect these regions of the brain (Hooker & Knight, Reference Hooker, Knight, Zald and Rauch2006; Knutson et al., Reference Knutson, Dal Monte, Schintu, Wassermann, Raymont, Grafman and Krueger2015; Løvstad et al., Reference Løvstad, Funderud, Endestad, Due-Tønnessen, Meling, Lindgren and Solbakk2012).
The ability to inhibit a prepotent behavioural response (a response whereby positive or negative reinforcement is immediately available) and provide a more socially appropriate and controlled response, is a core function of the frontal sub-cortical executive system (the frontal sub-cortical executive system is comprised of the frontal lobe, striatum, globus pallidus, substantia nigra, and thalamus) (Dimoska-Di Marco et al., Reference Dimoska-Di Marco, McDonald, Kelly, Tate and Johnstone2011; Mega & Cummings, Reference Mega and Cummings1994). It is therefore unsurprising that inappropriate social behaviours are displayed among individuals with either focal or indirect damage to these abovementioned regions. These same brain regions are known to be implicated in several higher order social cognitive functions, including emotion perception and theory of mind (ToM). Because of this, it has been suggested that dysfunction in these areas may in fact contribute to the socially disinhibited behaviours seen among those with a brain injury and other organic neurological conditions (Muller et al., Reference Muller, Simion, Reviriego, Galera, Mazaux, Barat and Joseph2010; Osborne-Crowley & McDonald, Reference Osborne-Crowley and McDonald2018; Torralva et al., Reference Torralva, Gleichgerrcht, Ardila, Roca and Manes2015). It has also been proposed that among individuals with Williams Syndrome, autonomic nervous system (ANS) dysfunction, as well as reduced amygdala reactivity for negative social information (e.g., for faces or vocalisations), may result in the absence of the fight or flight response, therefore resulting in social disinhibitory behaviours (Meyer-Lindenberg et al., Reference Meyer-Lindenberg, Hariri, Munoz, Mervis, Mattay, Morris and Berman2005; Ng et al., Reference Ng, Bellugi and Järvinen2016). Although the mechanisms underlying this set of complex social behaviours remain largely unknown, the regions of the brain involved have been consistently reported.
It is important to note that while compromised brain function may be viewed as an antecedent of socially disinhibited behaviours, the presentation of these behaviours are also likely to be contextually dependent. For example, in high stake social environments, such as a job interview, it may be that these behaviours are less likely to occur than if the person is in a low stake social environment, such as the home (Hooker & Knight, Reference Hooker, Knight, Zald and Rauch2006). While research examining how the social environment might govern socially disinhibited behaviours is limited, a prior study by Honan et al. (Reference Honan, Allen, Fisher, Osborne-Crowley and McDonald2016) found that when provided with explicit guidance, individuals with a TBI are able to successfully inhibit automatic negative and socially inappropriate responses. Thus, successful inhibition may be more likely to occur with the presence of salient environmental cues that prompt an individual to alter their behaviour. Successful social inhibition may also be dependent on the detection and understanding of social cues such as facial expressions or language pragmatics (Lin et al., Reference Lin, Zhang, Liu, Zhao, Zhang, Wang and Yi2021; Watts & Douglas, Reference Watts and Douglas2006). Difficulties with perceiving emotions and language pragmatics are a common outcome of brain injury and other neurological illnesses and thus are of relevance to the occurrence of socially disinhibited behaviours. For example, a reduced ability to detect anger may mean that an individual is perceived as being less threatening, resulting in an increased likelihood of a disinhibited response.
Although not discussed in the literature included in this analysis, it is possible that internal factors may also act as antecedents for socially disinhibited behaviours. For example, if an individual is highly frustrated, upset or angry they may be more inclined to behave in a socially inappropriate manner. It may also be that external triggers (e.g., someone making an unkind comment) can increase an individual’s propensity to behave in a socially disinhibited manner. Future research examining the role of internal factors such as feelings of frustration and anger may increase our understanding of other possible antecedents associated with socially disinhibited behaviours.
Conversely, consequences refer to those events or incidents that follow the occurrence of the concept (Walker & Avant, Reference Walker and Avant2019). Several consequences of social disinhibition were identified within the literature, highlighting the profound impact this can have on multiple aspects of an individual’s life, as well as the lives of those around them (Osborne-Crowley & McDonald, Reference Osborne-Crowley and McDonald2018). One of the most prominent consequences of social disinhibition is the reduced capacity to establish and maintain social relationships, resulting in social isolation, reduced life satisfaction, psychiatric illness (particularly depression and anxiety) and increased suicidal endorsement, as well as difficulties in gaining and maintaining employment (Gosch & Pankau, Reference Gosch and Pankau1997; Gould et al., Reference Gould, Ponsford, Johnston and Schonberger2011; Hoofien et al., Reference Hoofien, Gilboa, Vakil and Donovick2001; Juengst et al., Reference Juengst, Kumar, Arenth and Wagner2014; Koskinen, Reference Koskinen1998; Osborne-Crowley et al., Osborne-Crowley et al., Reference Osborne-Crowley, McDonald and Rushby2016). According to Thomsen (Reference Thomsen1984), lack of social connectedness is reported as one of the most disabling consequences of brain injury. Another common outcome associated with disinhibited behaviours is exploitation and abuse. Many individuals displaying disinhibited behaviours are often victims of sexual assault and domestic abuse (Davies et al., Reference Davies, Howlin and Udwin1998; Manning et al., Reference Manning, Smith and Mazerolle2013). An individual’s disinhibited behaviours (particularly inappropriate touching, sexual comments and displays of affection) may also be experienced by others as sexual abuse or harassment. Whilst it is not necessarily the intention of the individual to touch someone sexually or make inappropriate sexual comments, it can certainly result in a negative experience for the person affected (Davies et al., Reference Davies, Howlin and Udwin1998). Unfortunately, sexually aberrant behaviours can also lead to legal problems for many individuals (Simpson et al., Reference Simpson, Blaszczynski and Hodgkinson1999).
The negative consequences associated with social disinhibitory behaviours can be divided into three separate domains, namely, psychological, behavioural, and negative personal experiences. A diagrammatic representation of these consequences can be seen in Fig. 4.
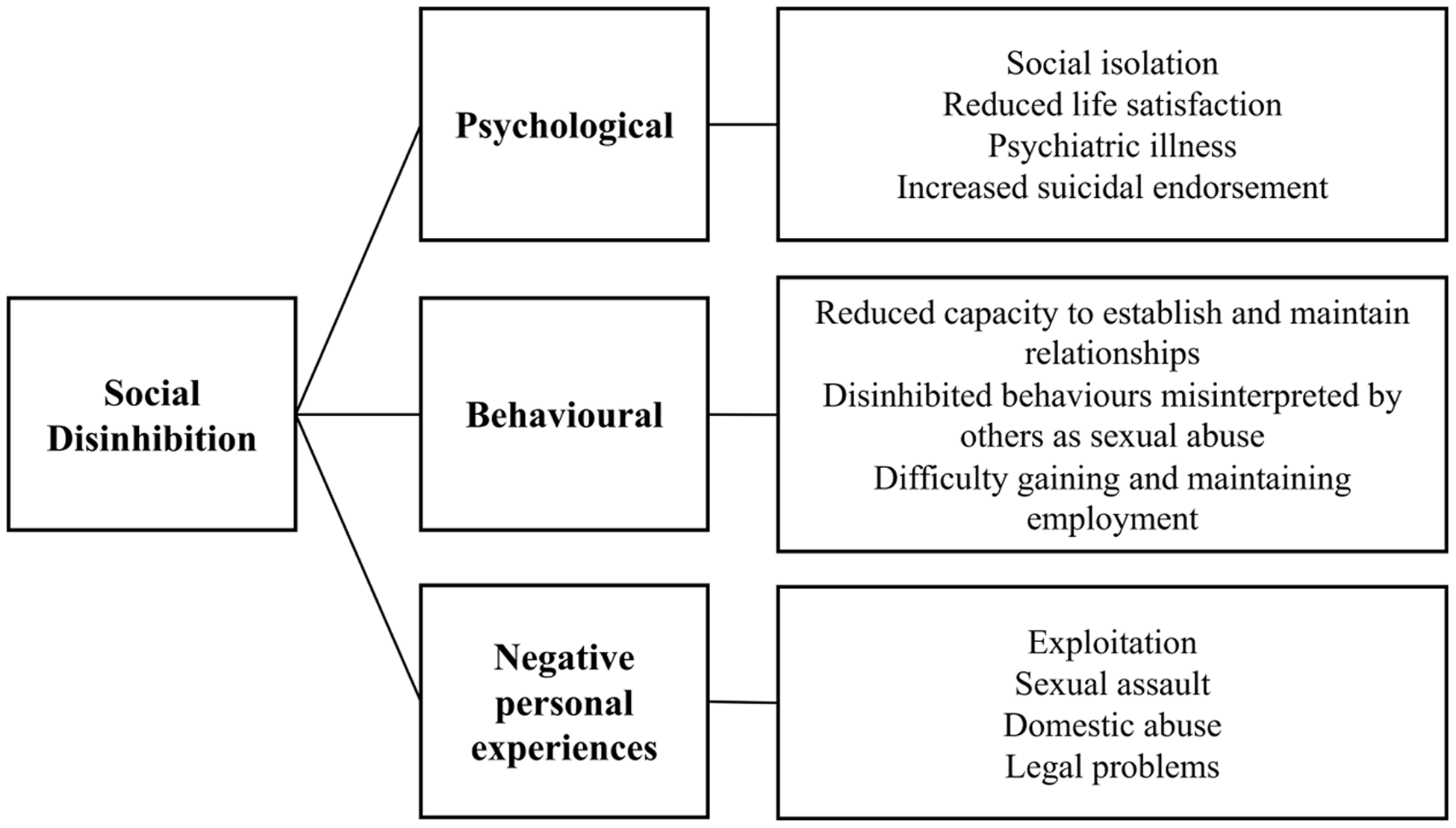
Figure 4. Negative consequences associated with social disinhibition for the individual with a brain injury or neurological condition.
The impact of disinhibited behaviour extends well beyond the individual with the brain injury or neurological condition. Primary caregivers in particular are often affected. One study found that mothers of individuals with a TBI reported significantly higher levels of emotional distress than mothers of healthy individuals without a TBI (Kinsella et al., Reference Kinsella, Packer and Olver1991). In this study, of all of the difficulties reported by these mothers, it was the behavioural difficulties (e.g., disinhibition, impulsivity, frequent mood changes and irritability) that caused greater burden than any cognitive or physical difficulties. Similar concerns have also been reported in other studies, with behavioural difficulties and lack of temper control causing greatest concern among caregivers of individuals with head injuries (McKinlay et al., Reference McKinlay, Brooks, Bond, Martinage and Marshall1981; Oddy et al., Reference Oddy, Humphrey and Uttley1978). The increased carer burden will inevitably strain relationships and increase the propensity for poor outcomes (e.g., reduced support and social isolation). For this reason it is one of the most impactful outcomes associated with brain injury and neurological conditions.
Constructed cases
Model cases are used to reflect all of the defining attributes of the concept (Walker & Avant, Reference Walker and Avant2019). They are a pure representation of the concept and they enable the reader to be absolutely certain about the instance of a concept. A borderline case is a case that contains most, but not all, of the defining attributes and they allow the reader to see how the concept differs from other related concepts. Related cases are instances of concepts that are related to the concept and, finally, contrary cases are those cases that are definitely not the concept.
The following hypothetical cases have been devised to illustrate what is and what is not the concept.
Model case
Mary is a 55-year-old woman who sustained a severe TBI six years ago. Mary’s husband reports considerable changes in her behaviour, noting that she often touches strangers when out in public, has a ‘lack of filter’ in that she often tells people exactly what she is thinking about them, is unable to recognise when it is appropriate to take her turn when speaking during a conversation (and consequently will speak over the top of people), and often makes inappropriate sexual comments about almost everyone she sees. He mentioned that Mary’s behaviour has resulted in her losing many friends and her family no longer visiting her.
Borderline case
Geoff is a 72-year-old man who was recently suspected by his neurologist as having an emerging frontotemporal dementia. Geoff is known to enjoy spending time in his garden. His daughter has recently observed that he has started to occasionally become frustrated when gardening and swears and mutters inappropriate comments, particularly about others, as a result. However, this has only occurred when Geoff is by himself, and despite his daughter believing he is on the verge of displaying inappropriate behaviour around the company of others (e.g., by looking agitated and talking out of turn), he has not behaved in a way that offends others or appears overly inappropriate.
Related case
Sally is a young 23-year-old nurse who recently sustained a moderate-to-severe TBI. Her family have noticed her making thoughtless financial decisions. Although Sally’s excessive spending makes her feel good, she has been unable to pay her bills as a result and is falling into considerable financial debt. Sally’s financial decisions have not impacted anyone else.
Contrary case
Peter is a 54-year-old man who has recently been experiencing difficulties with his memory. His wife reports that he has also been having trouble following conversations. Despite these challenges however, Peter has never said anything or behaved in a way that may be construed as being socially inappropriate by others.
Implications and future directions
Understanding social disinhibition and how it presents has important implications for both research and clinical practice, including the development of targeted assessment tools, the delivery of client-centred interventions, and how patient care is managed. Based on this concept analysis and our increased understanding of the elements that underlying social disinhibition, we propose the following tentative working definition of social disinhibition. It is anticipated that this definition, along with the proposed taxonomy previously mentioned, will provide researchers with a clearer understanding of what social disinhibition entails and how it might be distinguished from other related terms (e.g., impulsivity, behavioural dysregulation).
“Social disinhibition occurs within a social context and typically involves a transaction between two or more individuals. Social disinhibition is a spontaneous social behaviour that may be verbally (e.g., making inappropriate sexual comments, interrupting conversations, talking over the top of others) or physically (e.g., impinging on personal space, inappropriate touching, hugging or kissing) exhibited. The behaviour is such that it often results in negative social consequences such as distrust, fractured relationships and loss of employment.”
Concept clarification is also a fundamental step in developing appropriate assessment tools for use in both research and clinical environments. To date, much of the research examining social disinhibition has relied on standardised self- or informant-report questionnaires (e.g., Frontal Systems Behaviour Scale; FrSBe, Behaviour Rating Inventory of Executive Function; BRIEF), self- or informant-report interviews, or laboratory assessment tools designed to examine inhibitory control (e.g., Go/NoGo tasks, Sustained Attention to Response Test, and the Stop-Signal task) (Cicerone, Reference Cicerone1997; Dimoska-Di Marco et al., Reference Dimoska-Di Marco, McDonald, Kelly, Tate and Johnstone2011; Osborne-Crowley & McDonald, Reference Osborne-Crowley and McDonald2018; Tinius, Reference Tinius2003). Whilst the use of these instruments enable some insight into the possible extent of social disinhibition that may be present in an individual, none of them have been designed specifically to assess social disinhibition difficulties. Other tasks, such as the Social Disinhibition Task (Honan et al., Reference Honan, Allen, Fisher, Osborne-Crowley and McDonald2016) and an adaptation of the Self-Disclosure Task (Osborne-Crowley, McDonald, & Francis, Reference Osborne-Crowley, McDonald and Francis2016) (whereby participants are asked a series of questions and told that it is their choice how much information they choose to disclose) have been devised to specifically examine social disinhibition difficulties among clinical groups. Whilst these tasks are more ecologically valid, they also have their limitations (e.g., they are devoid of important social information, such as dynamic social context). This concept analysis provides a strong basis from which additional targeted assessment tools may be developed.
Limitations
It is important to note the limitations of this analysis. First, our search strategy was limited to articles published in English, therefore limiting our understanding of social disinhibition within other cultures. Grey literature was also not examined, meaning some relevant literature may have been missed. Secondly, there is a substantive quantity of literature describing behaviours that may be reflective of social disinhibition, however the authors do not refer to them as such. Because these articles did not use the term ‘social disinhibition’, they were not identified as part of the search, and consequently, were not included in this analysis. Similarly, social disinhibition was the only term (relating to disinhibited behaviours) included in the search strategy, therefore, articles using different terms to describe behaviours that may be consistent with social disinhibition were not included in the analysis. This decision was made to allow a focused examination of how researchers and clinicians were using the term ‘social disinhibition’ specifically. Thirdly, literature relating to social disinhibition in psychological and psychiatric conditions (e.g., schizophrenia, personality disorders) was excluded. Future research examining social disinhibition in these populations may lead to further insights about these behaviours and how they present. Finally, minimal information was provided throughout the included articles about the defining attributes of social disinhibition given the lack of coverage of this in the articles themselves. Future research may focus on further understanding these attributes associated with social disinhibition and how these may differ to similar or related concepts.
Conclusion
Social disinhibition is a common and challenging outcome following brain injury or other neurological condition. A lack of consensus regarding both the definition and assessment of this construct has continued to thwart research efforts. By systematically examining the concept of social disinhibition, a greater understanding of its structure and function and uses within the brain injury and other neurological condition literature, as well as how it is similar and/or different to other related concepts, has been reached. Increasing our understanding of social disinhibition and how it presents within different clinical populations has important implications in both research and clinical practice, including more accurate estimates of prevalence, development and implementation of targeted rehabilitation programmes, and increased empathy for those experiencing it. It is hoped that, in future, researchers and clinicians have a better understanding of the full extent of social disinhibition, how it presents, and it’s associated consequences.
Supplementary materials
For supplementary material for this article, please visit https://doi.org/10.1017/BrImp.2022.23
Financial support
Miss Skromanis is supported by an Australian Government Research Training Scholarship awarded by the College of Health and Medicine, University of Tasmania. Miss Skromanis is also supported by the Dianne Eerden Elite Research Scholarship.
Conflicts of interest
None.







