Non-melanoma skin cancer (NMSC) is a common form of skin cancer that occurs either in basal or squamous cells. These cells are located at the epidermal layer of the skin and protect the internal organs and the outer surface of the body. Skin cancer cells vary in their proliferation rate depending upon the type of skin cancer, but rarely spread to the other parts of the body. More than 1 000 000 new cases and less than 1000 deaths from NMSC have been reported in the USA in 2010(1). UVA and UVB (UV radiation) exposure to exposed skin is the leading cause of NMSC(Reference Ramos, Villa and Ruiz2). Outdoor workers, people of fair skin, large number of moles in the body, large dark-coloured birth mark known as congenital melanocytic nevus, pre-cancerous skin lesion such as actinic keratosis, family history of sunburn and skin cancer, and aged people are at a serious risk of developing skin cancer.
Oxidative stress, which is defined as an excess of toxic reactive oxygen species (ROS), and concomitant inadequate expression levels of various ROS detoxification enzymes, such as phase II detoxification and antioxidation enzymes, play a crucial role in developing several cancers including skin carcinogenesis(Reference Acharya, Das and Chandhok3). ROS is produced during distinct intracellular pathways and has been found to be elevated during infection, inflammation, and exposure to environmental carcinogens, radiation and sunlight(Reference Sander, Hamm and Elsner4), which in part might lead to the development of NMSC. Cancer chemoprevention, as first defined by Sporn in 1976(Reference Sporn, Dunlop and Newton5), utilises naturally occurring phytochemicals, biological compounds and/or synthetically synthesised chemical agents to reverse, repress or prevent the development of several cancers including skin cancer. Spices and condiments are naturally occurring dried herbs that are known for their high therapeutic potential. Numerous epidemiological studies have shown that a diet rich in vegetables, fruits, herbs and spices is associated with a reduced risk of most cancers, and thus serve as potent chemopreventive agents(Reference Sporn, Dunlop and Newton5, Reference Tapsell, Hemphill and Cobiac6).
Cardamom is a well-known aromatic spice that is regularly used in Eastern, Arab and Scandinavian cuisines for its aroma. From ancient times, it has also been used as herbal medicine especially for the common cold. Cardamom has also been used for teeth, gum and throat infection, as well as against lung congestion, pulmonary tuberculosis and digestive disorders. Cardamom is one of the common ingredients of Indian Ayurveda and Chinese traditional medicine(7). Cardamom belongs to Elettaria and Amomum genera of the ginger family Zingiberaceae. Both forms have small spindle-like seedpod but Elettaria is smaller and light green in colour, whereas Amomum is big and blackish grey in appearance. T. John Zachariah in his chapter titled ‘Chemistry of cardamom’ from the book Cardamom, The Genus Elettaria(Reference Zachariah, Ravindran and Madhusoodanan8) had compiled different components of cardamom that have been investigated and published earlier. The main chemical ingredients of cardamom is the oil component that is composed of α- and β-pinene, α-phellandrene, sabinene, limonene, myrcene, 1,8-cineole, γ-terpinene, p-cymene, terpinolene, linalool, terpinen-4-oil, α-terpineol, α-terpineol acetate, linalyl acetate, citronellol, geraniol, nerol, methyl eugenol and trans-nerolidol(Reference Zachariah, Ravindran and Madhusoodanan8, Reference Acharya, Das and Singh9). A couple of bioactive compounds of cardamom have been studied for anti-cancer, anti-inflammatory and chemopreventive properties. Monoterpene compounds of cardamom oil were shown to enhance the activity of indomethacin on skin. A lower dose of cardamom suppressed oedema to a lesser extent, whereas a higher dose of cardamom reveals a more potent anti-inflammatory effect on the skin in the presence of indomethacin(Reference Huang, Fang and Hung10). Chemopreventive function of cardamom has also been demonstrated earlier to regulate colorectal cancer(Reference Bhattacharjee, Rana and Sengupta11). The present study was designed to evaluate the chemopreventive efficacy of nutritional cardamom on 7,12-dimethylbenz[a]anthracene (DMBA)-induced skin carcinogenesis in a well-defined mouse model(Reference Das and Saha12) that highly mimics human NMSC.
Experimental methods
Chemicals
DMBA, croton oil, acetone, NADPH (nicotinamide adenine dinucleotide phosphate, reduced form), pyrogallol, thiobarbituric acid, diethylene triamine penta-acetic acid and pyridine were purchased from Sigma Chemicals Company.
Animals used and dose selection for 7,12-dimethylbenz[a]anthracene and cardamom
Female Swiss albino mice aged 5–6 weeks, and weighing 20–22 g were housed in plastic cages with stainless-steel wire lids (four mice per cage). The housing facility was maintained at 30°C temperature under alternating light and dark conditions. Standard food pellets and drinking water were provided ad libitum to all the treated/untreated mice.
7,12-Dimethylbenz[a]anthracene treatment
DMBA was purchased from Sigma Chemicals Company. In the first week, three topical applications of 100 nmol DMBA in 100 μl acetone were applied on the shaved dorsal skin. This was followed by 1 % (w/v) croton oil in acetone at the same site twice per week up to 8 weeks for the initiation and development of skin papillomatogenesis.
Cardamom treatment
Small-pod cardamom was bought from the local market (available to common people) in bulk in anticipation to complete one set of experiments (3 months of supply) so that the batch of cardamom does not differ between feedings to the animals. Just before the oral administration of cardamom to DMBA-treated mice, the required amount of spice was ground in a mixer and an aqueous suspension of cardamom solution was prepared fresh that contained all the oil components of cardamom as emulsion. Initially, a pilot study was carried out using different doses, namely 250, 500, 750 and 1000 mg cardamom/kg body weight per d, in order to standardise the most effective dose against papilloma formation during DMBA-induced skin carcinogenesis. Treatment with 500 mg cardamom/kg body weight per mouse per d was found to be most effective without any toxic manifestation.
Experimental design and treatment groups
The experiments were divided into three sets such that mice can be killed after 2nd, 8th and 12th week of first DMBA application. Each set was again divided into five groups with eight mice in each group. Each set comprised forty mice that were divided into ‘untreated’ (normal control), ‘acetone’ (vehicle control), ‘DMBA’ (carcinogen control), ‘DMBA+CARD’ (DMBA-treated and cardamom-ingested) and ‘CARD’ (cardamom-ingested) groups. The protocol used for DMBA application on the shaved dorsal skin of Swiss albino mice, and oral administration of cardamom to wild-type and DMBA-treated mice are given in Table 1. Acetone treatment was done exactly similar to the DMBA treatment and considered as the vehicle control because DMBA was dissolved in acetone. All animal protocols have been approved by the Institutional Animal Care and Use Committee of the institution. The animals were carefully examined once per week for recording the body weight and papilloma growth.
Table 1 Correlation between the different groups of mice, treatments and body weight
(Mean values and standard deviations)
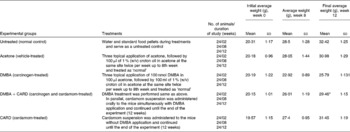
DMBA, 7,12-dimethylbenz[a]anthracene; CARD, cardamom ingested.
* Mean value was significantly different from that of the DMBA group (P < 0·001).
Tissue preparation for histology with haematoxylin and eosin and immunohistochemistry
Collected skin tissues were fixed in 10 % neutral formalin for 24 h and then dehydrated by graded ethyl alcohol, starting from 50 to 95 %. The tissues were then soaked in xylene and paraffin blocks were prepared. Serial microtome sections, in the form of a paraffin ribbon, were made at a thickness of 5 μm. The tissues were soaked in lukewarm water (58°C) for stretching, and the desired portion of the paraffin ribbon was placed on a clear glass slide previously coated with egg albumin and gently stretched using forceps or needles. Any excess water on the slide was drained off, and the slide was placed on a hot plate to allow the paraffin to dry and adhere to the slide.
Haematoxylin and eosin staining was performed with the sectioned tissues. The slides were rehydrated by graded ethyl alcohol series (from 95 to 50 % ethyl alcohol) and were stained with 1 % haematoxylin for 3 min. The slides were washed slowly in running tap water for 8–10 min to develop the colour of haematoxylin that stains DNA-rich nuclei. The stained slides were then dipped in an acid–alcohol solution (1:1 HCl–C2H5OH) to remove extra stain and washed under running water. The haematoxylin-stained slides were again passed through ascending grades of ethyl alcohol. Counterstaining was done with eosin (0·5 g in 100 ml of 95 % absolute alcohol). The slides were then treated with xylene for 15 min each. Mounting was performed with a small amount of DPX mounting solution over a thin 22–50 mm coverslip.
Immunohistochemical staining of mouse skin samples was performed with the following antibodies: nuclear factor erythroid-2-related factor 2 (Nrf2; Santa Cruz SC-722, 1:100); NF-κB (Santa Cruz SC-109, 1:75); IκBα (Santa Cruz SC-371, 1:600); kelch-like ECH-associated protein 1 (Keap1; Sigma AV38981, 1:4000). A 5 μm section from formalin-fixed paraffin-embedded tissues was deparaffinised with xylene and rehydrated through a graded alcohol series (from 95 to 50 % ethyl alcohol). Antigen retrieval was performed by immersing the tissue sections at 98°C for 20 min in 10 mm-citrate buffer (pH 6·0) with 0·05 % Tween. Immunohistochemical staining was performed using the Vectastain Kit (Vector Labs), according to the manufacturer's instructions. Briefly, slides were pretreated with 3 % H2O2, avidin/biotin blocking and 10 % normal goat serum, and then exposed to the stated dilution of primary antibody for 1 h at room temperature. The slides were exposed to appropriate biotin-conjugated secondary antibodies (Vector Labs), Vectastain ABC reagent (Vector Labs) and DAB chromagen (Dako) to detect horseradish peroxidase. The slides were then counterstained with haematoxylin (Fisher, Harris Modified Haematoxylin) at a 1:17 dilution for 2 min at room temperature, blued in 1 % ammonium hydroxide for 1 min at room temperature, dehydrated and mounted with Acrymount. Consecutive sections with the omitted primary antibody were used as negative controls. Images were captured using an Olympus DP70 microscope (Olympus) at 200 × magnification.
Preparation of tissue lysates for immunoblotting
Treated/untreated skin tissues from the dorsal sides were excised from each group of mice for lysate preparation. In the case of the ‘DMBA’ and ‘DMBA+CARD’ groups, skins with three to four papillomas per mice were excised to prepare the tissue lysates. This whole procedure had been repeated three times for reproducibility and statistical significance. Approximately 50 mg of skin tissues from treated and untreated mice were excised from the different groups of mice and subsequently soaked in tissue lysis buffer (Roche Biochemicals) containing protease inhibitor cocktail (Roche Biochemicals) at 4°C. The tissues were then homogenised for 30 s and then centrifuged at 14 000 g for 20 min at 4°C. The supernatants (tissue lysates) were collected into a fresh tube and stored in − 80°C until further use in subsequent Western blotting. Concentrations of the total proteins were measured by the Lowry method using bovine serum albumin as a standard.
Methods for biochemical assays
Skin tissues were sampled for biochemical assays from all groups of mice for the measurement of lipid peroxides (LPO), glutathione-S-transferase (GST), glutathione peroxidase (GPx), catalase (CAT), superoxide dismutase (SOD), glutathione reductase (GR) and reduced glutathione (GSH) as published protocols(Reference Das and Saha12). For the 4-hydroxynonenal (4-HNE) assay, generation of 4-HNE was measured by following the manufacturer's instructions using OxiSelect HNE-His Adduct Elisa Kit from Cell BioLabs.
LPO generation in mice was obtained from 400 mg of the treated/untreated skin tissue lysates by measuring thiobarbituric acid-reactive substance, formed/mg protein using an extinction coefficient of 1·56 × 105 mol/l per cm(Reference Ando, Kon and Aino13). Thiobarbituric acid-reactive substance assay is a tool for the direct measurement of malondialdehyde (MDA) in the treated/untreated skin tissue lysates. In brief, skin tissues were washed in 0·9 % NaCl and homogenised with nine volumes (3·6 ml) of 1·15 % KCl, followed by centrifugation at 12 000 g for 10 min at 4°C. The supernatant was further centrifuged for 10 min at 10 000 g at 4°C. Finally, the supernatant was centrifuged at 25 000 g at 4°C for 1 h and the precipitate was retained. The precipitate was then resuspended in KCl and aliquots were stored for future use. SDS, acetic acid, thiobarbituric acid and water were then added to the selected aliquots and heated at 95°C for 1 h. The butanol–pyridine solution (15:1) was added to the above reaction mixture and the mixture was vortexed vigorously for 2 min followed by centrifugation at 3000 g for 10 min. The upper organic layer was collected, and optical density at 532 nm was measured against the control. Control was prepared in the same way as described above, but water was taken instead of sample lysate.
4-HNE is considered as a marker for oxidative stress and is a well-known naturally occurring toxic by-product of lipid peroxidation. It was measured in a ninety-six-well format where samples (about 10 μg/ml) were allowed to adsorb in the wells for 2 h at 37°C. 4-HNE protein adducts were then incubated with anti-HNE-His antibody, which was further incubated with horseradish peroxidase-conjugated secondary antibody. Initially, a standard curve was prepared with known concentrations of HNE-bovine serum albumin standards. 4-HNE contents in the treated/untreated skin tissues from the different groups of mice were measured as above and quantified using the HNE-bovine serum albumin standard curve.
Activity of GST was measured from 200 mg of the treated/untreated skin tissue lysates by documenting the increase in the absorbance of 1-chloro-2-4-dinitrobenzene (CDNB) as the substrate at 340 nm(Reference Habig, Pabst and Jakoby14). Specific activity of the enzyme is expressed as the formation of CDNB–glutathione (CDNB–GSH) conjugate/min per mg protein. In brief, tissues were homogenised and centrifuged at 35 000 g for 2 h at 4°C. The supernatant was collected and incubated with 100 μl CDNB in distilled water at 30°C for 5 min. Then the reaction was initiated by the addition of 100 μl GSH and optical density was taken at 340 nm. Control was prepared as described above and distilled water was taken instead of tissue homogenate.
Activity of GPx was measured from 100 mg of the treated/untreated skin tissue lysates(Reference Paglia and Valentine15). For the assay, NADPH and GR were mixed with the sample and the decrease in the absorbance of NADPH at 340 nm was immediately measured in the presence of H2O2. GPx activity is expressed as nmol of NADPH utilised/min per mg protein using the molar extinction coefficient of NADPH at 340 nm (6·22/nm per cm).
CAT activity was also measured spectrophotometrically from 100 mg of the skin tissue lysates(Reference Luck16). Tissues were homogenised in phosphate buffer and centrifuged at 2500 g for 10 min. The supernatant was used for the enzyme activity assay in the presence of H2O2 and measured spectrophotometrically at 240 nm. The results are expressed as units/mg protein. The unit is defined as follows: one unit of CAT is the amount of enzyme that liberates half of the peroxide oxygen from H2O2 in 100 s at 25°C.
SOD activity was measured from 200 mg of the skin tissue lysates from the different groups of mice. Extraction and purification of SOD was performed according to the published protocol(Reference Marklund and Marklund17). SOD was quantified as an inhibition of pyrogallol auto-oxidation in Tris–HCl buffer (50 mm, pH 7·5), which was measured spectrophotometrically at 420 nm, and the results are expressed as units/mg protein. The unit is defined as follows: one unit of enzyme activity is expressed as the amount of enzyme necessary for inhibiting the reaction by 50 %.
GSH activity was measured with the cytosolic fraction from 200 mg of skin tissues obtained from the different groups of mice(Reference Sedlak and Lindsay18). The assay was designed to measure a decrease in dithiobis(2-nitro)-benzoic acid reduced by –SH groups and expressed as nmol/mg protein. First, a standard curve was prepared by measuring the absorbance of different known concentrations of GSH. The GSH enzyme activities from the treated/untreated skin samples were determined from the GSH standard curve.
GR is a flavoprotein catalysing the NADPH-dependent reduction of glutathione disulphide to GSH. GR activity was measured from 200 mg of the skin tissue lysates obtained from the different groups of mice(Reference Carberg, Mannervick, Fleisher and Packer19). The oxidation of NADPH was measured spectrophotometrically at 340 nm. Enzyme activity is expressed as nmol NADPH consumed/min per mg protein based on the extinction coefficient of NADPH, which is 6·22/nm per cm.
Statistical analysis
All the experiments were performed at least three times and were analysed and expressed as means and standard deviation. The data obtained from the ‘untreated’, ‘acetone’, ‘DMBA’ and ‘DMBA+CARD’ groups were statistically analysed by one-way ANOVA via Tukey's test, which is a pairwise comparison of the mean responses to the different treatment groups using Sigmastat statistical software (version 3) for Windows; Systat Software Inc.). P < 0·05 was considered significant for all experiments.
Results
Morphological evidences of papillomas following the 7,12-dimethylbenz[a]anthracene and cardamom treatments
Female Swiss albino mice were grouped and treated as described in Table 1. The ‘untreated’, acetone- and ‘DMBA’-treated groups served as the normal control, vehicle control and carcinogen control, respectively. The effect of cardamom was determined in carcinogen-treated and cardamom-ingested mice designated as (DMBA+CARD). At the end of the 12th week, after the first topical DMBA application on mouse skin, the total incidences of papilloma growth were found to be reduced significantly both in number and sizes in the ‘DMBA+CARD’-treated group with respect to the ‘DMBA’ group. No papillomas were observed in the ‘untreated’ and ‘acetone’ groups at any time point. A representative snapshot of mice from each group is shown in Fig. S1 of the supplementary material (available online at http://www.journals.cambridge.org/bjn). Cardamom-treated mouse skin did not show any papilloma growth on the skin at any time point (Fig. 1(b)).

Fig. 1 Effects of topical application of 7,12-dimethylbenz[a]anthracene (DMBA) and ingestion of cardamom on body weight and papilloma growth. Swiss albino mice were grouped and treated as given in Table 1. (a) DMBA-treated mice (DMBA, ![]() ) demonstrated a significantly lower growth rate than that of DMBA-treated and cardamom-ingested mice (DMBA+CARD,
) demonstrated a significantly lower growth rate than that of DMBA-treated and cardamom-ingested mice (DMBA+CARD, ![]() ). The normal control (untreated,
). The normal control (untreated, ![]() ) and acetone control (acetone,
) and acetone control (acetone, ![]() ) groups of mice showed a normal growth pattern. (B) Table describing the total incidences of papilloma growth on the skin in the experimental mice groups. Of the DMBA group, 92 % had papilloma growth on their treated skin but the percentage dropped down to 29 % for the DMBA+CARD group. The untreated, acetone-treated and CARD groups showed no papillomatous growth during the experimental period.
) groups of mice showed a normal growth pattern. (B) Table describing the total incidences of papilloma growth on the skin in the experimental mice groups. Of the DMBA group, 92 % had papilloma growth on their treated skin but the percentage dropped down to 29 % for the DMBA+CARD group. The untreated, acetone-treated and CARD groups showed no papillomatous growth during the experimental period.
Effects of aqueous suspension of cardamom on the body weight and papilloma growth
A normal growth pattern in body weights was observed in the ‘untreated’ and ‘acetone’-treated groups throughout our experimental time points (0–12 weeks). The body weights of the ‘DMBA’ group followed a much lower slope in growth pattern when compared with the other groups of mice (Fig. 1(a)). Growth pattern of the ‘DMBA+CARD’ group falls in between the growth rate of the ‘DMBA’ and ‘acetone’/‘untreated’ groups. Papillomas started to appear on the DMBA-treated skin from the 5th week onwards and continued to grow until the end of the 12th week. Of these mice, 92 % had papilloma growth due to the DMBA treatment on the shaved skin. Of the mice that received the aqueous suspension of cardamom by oral administration after the first DMBA application, 29 % showed papilloma growth from the 7th week instead of the 5th week and showed regression in papilloma growth when compared with the DMBA group (Fig. 1(b)).
Histology of the skin following induction of carcinogenesis and the cardamom treatment
The histology of the skin from the ‘DMBA’ group demonstrated marked differences when compared with the ‘acetone’ group as described previously(Reference Das and Saha12, Reference Das, Das and Saha20). Severe hyperkeratosis and acanthosis were observed in DMBA-treated mouse skin, demonstrating progression towards skin carcinogenesis after 8 and 12 weeks (see Fig. S2(B and E) of the supplementary material, available online at http://www.journals.cambridge.org/bjn). ‘Acetone’-treated mice demonstrated similar histology to that of the untreated mouse skin of the same age as shown previously(Reference Das and Saha12) (see Fig. S2(A and D) of the supplementary material, available online at http://www.journals.cambridge.org/bjn). Histology of the affected skins from the ‘DMBA+CARD’ group demonstrated mild hyperkeratosis and moderate acanthosis of the epidermis, which revealed a near-normal morphology of the skin after 8 and 12 weeks (see Fig. S2(C and F) of the supplementary material, available online at http://www.journals.cambridge.org/bjn).
Effect of the aqueous suspension of cardamom on lipid peroxidation
Lipid peroxidation is the unstable indicator of oxidative stress in cells that decompose to form more complex and reactive compounds such as MDA and 4-HNE. LPO are generated in the aerobic cells due to oxidative stress and the deleterious interaction of ROS with lipid molecules. These free radicals are produced in the body as normal consequences of biochemical processes and increased exposure to xenobiotics. Here we wanted to see whether aqueous suspension of cardamom has any effect on the DMBA-induced generation of LPO in the treated skins from the different groups of mice. We killed the different groups of mice at the end of 2, 8 and 12 weeks from the first dose of DMBA treatment. LPO values obtained from the 2nd and 8th week are given in Table S1 (available online at http://www.journals.cambridge.org/bjn) and the LPO data obtained after 12th week are shown in Fig. 2. The DMBA treatment induced the formation of LPO in the mouse skin, which was significantly higher than that of the ‘untreated’ and ‘acetone’-treated mouse skins. At the end of the 12 weeks, the generation of MDA and the production of 4-HNE were down-regulated to 5·25-fold (P < 0·001; Fig. 2(a)) and 2·75 fold (P < 0·001; Fig. 2(b)), respectively, in the ‘DMBA+CARD’ group when compared with ‘DMBA’-treated mice.

Fig. 2 Effects of ingestion of aqueous cardamom and 7,12-dimethylbenz[a]anthracene (DMBA) treatment on the generation of lipid peroxides (LPO) in treated skin tissue lysates after 12 weeks from first DMBA application. Malondialdehyde (MDA) and 4-hydroxynonenal (4-HNE) are the known toxic by-products of LPO. Swiss albino mice were grouped and treated as given in Table 1. Treated/untreated skin tissue lysates from all the groups of mice were subjected to the (a) MDA assay and (b) 4-HNE assay to determine the levels of LPO among the samples. In both the cases, the DMBA+CARD group showed significantly reduced LPO (* P < 0·001) when compared with DMBA-treated mice only. Values are means, with standard deviations represented by vertical bars. TBARS, thiobarbituric acid-reactive substance. CARD, cardamom ingested.
Effect of the aqueous suspension of cardamom on host cellular defences
Detoxification enzymes and antioxidants are the key players that maintain redox homeostasis of the cells and help in metabolism of the xenobiotics as a part of cellular defence system. Thus, we investigated the effects of cardamom ingestion against the development of skin papillomas initiated by DMBA on the activities of GST, GPx, GSH, GR, SOD and CAT. The treated/untreated skin tissue lysates obtained from the different groups of mice were used for the activity assays. Cardamom ingestion, following the DMBA treatments, elevated the activity levels of GST by 13·1-fold, combined GPx by 8·62-fold, GSH by 8·17-fold, GR by 16·45-fold, combined SOD by 22·13-fold and CAT by 13·14-fold when compared with DMBA-treated mice only. The increase in enzyme activities exceeded the basal levels of activities set by either ‘untreated’ or ‘acetone’-treated mice in each case (Fig. 3).

Fig. 3 Effects of ingestion of aqueous cardamom and 7,12-dimethylbenz[a]anthracene (DMBA) treatment on the activities of the detoxification enzymes in the treated/untreated skin tissue lysates obtained from the different groups of mice (Table 1) after 12 weeks from first DMBA application. The activities of (a) glutathione-S-transferase, (b) glutathione peroxidase, (c) reduced glutathione, (d) glutathione reductase, (e) superoxide dismutase and (f) catalase were significantly increased in the ‘DMBA+CARD’ group compared with the ‘DMBA’ group. The ‘untreated’ and ‘acetone’ groups demonstrate basal enzyme activities in each case. Values are means, with standard deviations represented by vertical bars. Mean value was significantly different from that of the DMBA group: * P < 0·001, ** P < 0·005. CARD, cardamom ingested.
Cardamom rescues 7,12-dimethylbenz[a]anthracene-induced down-regulation of nuclear factor erythroid-2-related factor 2 and kelch-like ECH-associated protein 1 in mouse skin
Nrf2 is a basic region-leucine zipper transcription factor that regulates the induction of phase II detoxification enzymes during stress condition(Reference Cho, Reddy and Debiase21). Keap1 is a cytoplasmic anchor for Nrf2 that tethers Nrf2 in the cytoplasm under basal unstressed conditions. Keap1 prevents Nrf2 from translocating to the nucleus, where it would bind to the antioxidant response element and activate gene transcription(Reference Kensler and Wakabayashi22). It has been reported that Nrf2 is released from Keap1 under oxidative stress, resulting in an enhanced nuclear accumulation and transcriptional induction of target genes (phase II detoxification enzymes) that ensure cell survival(Reference Motohashi and Yamamoto23). Immunohistochemistry (IHC) with Nrf2 and Keap1 on the untreated/treated skins from the different groups of mice is shown in Fig. 4(a–c) (Nrf2) and Fig. 4(d–f) (Keap1) (one representative area from each group is shown). Skin tissue slides were stained with either Nrf2 or Keap1 antibody to evaluate the protein expression; the average expression of Nrf2 and Keap1 from each group of mice was quantified using the IHC pictographs, and analysed through Metamorph imaging software (Molecular Devices). The quantifications of the expressed proteins are represented as bar diagrams in Fig. 4(g) (Nrf2) and Fig. 4(h) (Keap1). It appeared that cardamom ingestion partially rescued the loss of expression of both Nrf2 and Keap1 due to the DMBA treatments.

Fig. 4 Cardamom stimulates the expression of nuclear factor erythroid-2-related factor 2 (Nrf2) and kelch-like ECH-associated protein 1 (Keap1). Skin tissues from the different groups of mice (Table 1) were excised and tissue slides were prepared for immunohistochemistry (IHC). IHC with Nrf2 antibody was performed on the skin tissues obtained from (a) acetone-treated, (b) DMBA-treated and (c) DMBA+CARD-treated mice. Similarly, Keap1 antibody was also used to stain the skin tissues obtained from (d) acetone-treated, (e) DMBA-treated and (f) DMBA+CARD-treated mice. The magnifications of the pictographs are 200 × . Quantification of the expressions of (g) Nrf2 and (h) Keap1 from several mouse skin tissues was evaluated using metamorph imaging software (Molecular Devices). Values are means, with standard deviations represented by vertical bars. * Mean value was significantly different from that of the DMBA group (P < 0·001). The arrowhead indicates loss of the expression; the arrows indicate gain in the expression. CARD, cardamom ingested. (A colour version of this figure can be found online at http://www.journals.cambridge.org/bjn).
Cardamom restores the 7,12-dimethylbenz[a]anthracene-initiated activation of NF-κB
NF-κB is a transcription factor that has a crucial role in cell proliferation, inflammation, immunity and apoptosis(Reference Baud and Karin24). During oxidative stress or UV radiation, activation of NF-κB mainly occurs via IκB kinase-mediated phosphorylation of inhibitory molecules, such as IκBα. Once activated, IκB kinases phosphorylate IκBα on Ser32 and Ser36 that lead towards ubiquitination and degradation of IκBα via the ubiquitin proteasome pathway(Reference Zandi, Rothwarf and Delhase25). During stress conditions, NF-κB transcription factor subunit (p65) translocates into the nucleus, where it binds to several regulatory proteins and regulates gene transcription. So, nuclear import is a key event of NF-κB activation(Reference Sochanowicz, Szumiel and Gradzka26). Thus, deregulation of NF-κB and IκBα phosphorylation is crucial in inflammation and cancer(Reference Acharya, Das and Chandhok3), and it has become a popular target for therapeutic applications. IHC with NF-κB-p65 and IκBα on the treated/untreated skins from the different groups of mice is shown in Fig. 5(a–c) (NF-κB-p65) and Fig. 5(d–f) (IκBα) (one representative area from each group is shown) to understand the impact of cardamom ingestion on the DMBA-treated mice in regulating NF-κB signalling. Several mouse skins from the different groups of mice were stained; the average staining intensities from each group of mice were quantified using IHC and analysed through Metamorph imaging software (Molecular Devices) and are represented as bar diagrams (Fig. 5(g), NF-κB-p65; Fig. 5(h), IκBα).

Fig. 5 Cardamom modulates the NF-κB signalling pathway. Different groups of mice were treated as described in Table 1. Skin tissues were excised and slides were prepared. Immunohistochemistry with NF-κB-p65 antibody was performed on the skin tissues obtained from (a) acetone-treated, (b) DMBA-treated and (c) DMBA+CARD-treated mice. Similarly, IκBα antibody was also used to stain the skin tissues obtained from (d) acetone-treated, (e) DMBA-treated and (f) DMBA+CARD-treated mice. The magnifications of the pictographs are 200 × . Quantification of the expressions of (g) NF-κB-p65 and (h) IκBα on skin tissues from several mice was evaluated using Metamorph Software (Molecular Devices). Values are means, with standard deviations represented by vertical bars. * Mean values were significantly different (P < 0·05). (h) * Mean value was significantly different form that of the DMBA group (P < 0·001). The arrowhead indicates loss of the expression; the arrows indicate gain in the expression. CARD, cardamom ingested. (A colour version of this figure can be found online at http://www.journals.cambridge.org/bjn).
Effect of cardamom on 7,12-dimethylbenz[a]anthracene-induced cyclo-oxygenase-2 expression
Cyclo-oxygenase-2 (COX-2; an isoform of COX), an important inducible protein expressed during several carcinogenesis processes, is associated with PG synthesis, mitogenesis, apoptosis, angiogenesis and metastasis through various biological pathways(Reference Miglietta, Toselli and Ravarino27). COX-2 has been shown to express both in malignant epithelial cells and in neovasculature that continuously feed the tumour cells. Thus, COX-2 is considered as one of the markers of cancer progression and targeted inhibition of COX-2 is a promising approach to prevent skin cancer. Elevated level of COX-2 expression has been observed with NMSC(Reference An, Athar and Tang28). The level of COX-2 expression in skin tissues was increased due to the DMBA treatment when compared with ‘untreated’ and ‘acetone’-treated mice, which corroborates with the lines of evidence that tumour progression is associated with increased COX-2 expression (Fig. 6). COX-2 expression in the skin tissue obtained from the ‘DMBA+CARD’ group was reduced by 37 % when compared with the DMBA-treated mouse skin only, demonstrating inhibition of neoplasia on the mouse skin by the aqueous ingestion of cardamom (Fig. 6).

Fig. 6 Effects of ingestion of aqueous cardamom and 7,12-dimethylbenz[a]anthracene (DMBA) treatment on cyclo-oxygenase-2 (COX-2) expression. Swiss albino mice were grouped and treated as given in Table 1. COX-2 is a marker of carcinogenesis. (a) DMBA+CARD group showed reduced expressions of COX-2 when compared with the DMBA group as determined by Western blot. (b) Densitometry was performed with at least three different immunoblotting experiments. Percentage decrease in expression is indicated by the arrows. Values are means, with standard deviations represented by vertical bars. * Mean value was significantly different from that of the DMBA group (P < 0·01). CARD, cardamom ingested.
Discussion
NMSC is the most frequent skin cancer in the USA with an incredible impact on physical condition and morbidity(1). Although solar radiation is the leading cause of human skin cancer, it is also acknowledged that significant levels of chemical agents present in today's environment also contribute to growing incidences of cutaneous neoplasia in humans. In the area of cancer prevention, the use of natural phytoproducts and their constituents as potential chemopreventive agents remains a hot topic of intense research. In the present study, we have demonstrated the chemopreventive action of cardamom, which is a spice mostly used in Asian and Scandinavian cuisines, on DMBA-induced skin carcinogenesis in female Swiss albino mice. Phytochemicals that can metabolise or inhibit the formation of free radicals in vivo may be considered as potential anti-carcinogenic agents for cancer chemoprevention. In recent years, phytochemicals present in the common human diet have gained considerable attention as photoprotective and chemopreventive agents against skin cancers(Reference Surh29). These phytochemicals belong to numerous classes that include phytoalexins, phenols, polyphenols, anthocyanidins flavonoids, isoflavonoids and carotenoids. The chemopreventive approach appears to have realistic implications in inhibiting skin cancer in individuals because of their ability to modify dietary intake and change in the lifestyle.
There are several dietary phytochemicals that demonstrate an immense effect on chemically induced skin carcinogenesis. Oral administration of epigallocatechin gallate, which is a polyphenol, blocked the growth of UV-induced skin tumours in mice, by decreasing H2O2-induced ROS and reducing inducible NO synthase expression in the UV-irradiated skin(Reference Katiyar and Mukhtar30). Pretreatment with genistein, an isoflavone, to hairless mice before UV exposure considerably blocked the UV-induced H2O2 and MDA formation in the skin, as well as minimised the generation of 8-hydroxy-2'-deoxyguanosine in the epidermis(Reference Wei, Zhang and Wang31). In SENCAR mice, topical application of genistein before UVB radiation reduced c-fos and c-jun expression(Reference Wang, Zhang and Lebwohl32) that are linked with cancer progression. Resveratrol is a polyphenol phytoalexin, and topical application of resveratrol before UVB irradiation to SKH-1 hairless mice resulted in considerable inhibition of UV-induced skin oedema as well as inhibition of the formation of H2O2(Reference Afaq, Adhami and Ahmad33). Resveratrol treatment to mouse skin also significantly inhibited the induction of COX-2 and lipid peroxidation, as well as repressed UVB-mediated activation of the NF-κB pathway(Reference Adhami, Afaq and Ahmad34). Silymarin, which is a polyphenol flavonoid, promotes the reduction of UVA-caused oxidative stress by reducing GSH depletion, blocking ROS and LPO production, as well as deactivating NF-κB activation in irradiated cells. Moreover, topical application of silymarin protects SKH-1 hairless mice against tumour initiation either with UVB or DMBA, stimulates CAT activity and inhibits COX-2 expression(Reference Katiyar, Korman and Mukhtar35). Topical application of another well-known phytochemical, curcumin, also inhibited COX-2 expression by suppressing p38 and c-Jun N-terminal kinase activities in HaCaT cells(Reference Cho, Park and Kweon36). Gingerol, on the other hand, repressed the UVB-induced intracellular ROS levels, inhibited the activation of caspase-3, -8, -9 and TNF receptor superfamily, member 6 (Fas) expression, down-regulated COX-2 expression and NF-κB activation(Reference Kim, Kim and Na37). Moreover, delphinidin, a dietary anthocyanidin, protected cells against UVB-mediated decrease in cell viability, as well as down-regulated the levels of lipid peroxidation and blocked DNA damage. Application of lycopene, which is found in tomatoes, inhibited UVB-induced ornithine decarboxylase and proliferating cell nuclear antigen inhibition, down-regulated myeloperoxidase activities and significantly reduced bifold skin thickness(Reference Fazekas, Gao and Saladi38). Thus, several individual components show excellent promise to protect cells against the propagation of skin carcinogenesis. Researchers are now interested in the combinatorial effects of several phytochemicals against chemically induced skin carcinogenesis. Recently, Kowalczyk et al. (Reference Kowalczyk, Kowalczyk and Tolstykh39) demonstrated the inhibitory effect of combined phytochemicals on DMBA-induced murine skin tumorigenesis and obtained a significantly higher efficacy than individual compounds.
DMBA is a well-known carcinogen and often used with croton oil or 12-O-tetradecanoylphorbol-13-acetate (TPA) to generate experimental papillomas on the skin. TPA and croton oil have been used for ages to initiate the two-stage skin carcinogenesis in mice(Reference Kowalczyk, Kowalczyk and Tolstykh39–Reference Schneider, Bowden and Sutter43). The use of DMBA with TPA or croton oil generates ROS, promotes DNA damage, modulates p53 and COX-2 function, deregulates the cell cycle and also alters apoptosis in the skin(Reference Das and Saha12, Reference Das, Das and Saha20, Reference Bhattacharyya, Paul and Mandal44, Reference Chaudhary, Alam and Siddiqui45). Thus, our system of generating experimental skin papilloma in mice by croton oil and DMBA somewhat mimics NMSC in humans. ROS also induces peroxidation of PUFA and causes lipid peroxidation in the cellular membrane. Increased lipid peroxidation has been found to be triggered due to amplified arachidonic acid metabolism via increased activities of cyclo-oxygenases, such as COX-1 and COX-2, to produce PG(Reference Bartsch and Nair46). MDA and 4HNE, the toxic by-products of lipid peroxidation formed during PG biosynthesis, are mutagenic and genotoxic that can promote cancer growth. Oral administration of aqueous cardamom to DMBA-treated mice showed significantly inhibited lipid peroxidation (Fig. 2), as well as demonstrated a decrease in the expression of COX-2 (Fig. 6), indicating beneficial functions of cardamom.
Cardamom extracts were also tested on the activities of phase II detoxification enzymes and antioxidation enzymes. GST and GPx play a vital role in inducing the detoxification of foreign compounds in the body to non-toxic and easily soluble components that can be easily excreted from the system. On the other hand, GR catalyses the conversion of glutathione disulphide to GSH for a fresh round of detoxification action. The antioxidation enzymes, particularly CAT and SOD, also provide protection to cells against ROS by detoxifying them on the site where they are produced. SOD and CAT are regarded as the first line of antioxidant defence that protect cells against oxidative stress. SOD neutralises the ![]() anion to H2O2 and O2, whereas CAT neutralises H2O2 to O2 and water(Reference Das and Saha12). Hence, the significant enhancement of the level of activities of GST, GPx, GSH, GR, SOD and CAT in the ‘DMBA+CARD’ group (Fig. 3) may be beneficial for inhibiting the incidences of papilloma generation due to DMBA application on mouse skin. Cardamom ingestion by DMBA-treated mice even elevated the levels of the enzyme activities beyond the basal levels of the ‘untreated’ and ‘acetone’-treated groups. Thus, it indicates that intake of whole cardamom every day in the normal diet has an enormous potential to boost the cellular defence system of the body that will be more appropriate to combat different stress conditions.
anion to H2O2 and O2, whereas CAT neutralises H2O2 to O2 and water(Reference Das and Saha12). Hence, the significant enhancement of the level of activities of GST, GPx, GSH, GR, SOD and CAT in the ‘DMBA+CARD’ group (Fig. 3) may be beneficial for inhibiting the incidences of papilloma generation due to DMBA application on mouse skin. Cardamom ingestion by DMBA-treated mice even elevated the levels of the enzyme activities beyond the basal levels of the ‘untreated’ and ‘acetone’-treated groups. Thus, it indicates that intake of whole cardamom every day in the normal diet has an enormous potential to boost the cellular defence system of the body that will be more appropriate to combat different stress conditions.
To understand the mechanism, we have investigated the molecular function of cardamom on Nrf2 and NF-κB transcription factors. The present data indicate that there is a loss of expression of Nrf2 (Fig. 4(b and g)) as well as Keap1 (Fig. 4(e and h)) in the ‘DMBA’-treated skin when compared with the ‘acetone’-treated skins (Fig. 4(a), Nrf2; Fig. 4(d), Keap1). ‘Acetone’-treated mouse skin expresses Nrf2 in the cytoplasmic region, which closely resembles the expression of Nrf2 on the skin of ‘untreated’ mice (compare Fig. 4(a) and Fig. S3(A) of the supplementary material, available online at http://www.journals.cambridge.org/bjn). Interestingly, cardamom ingestion rescues the nuclear expression of Nrf2 in the mouse skin of the ‘DMBA+CARD’ group, which suggests that the cardamom treatment might trigger an activation of Nrf2 despite the deleterious effects of DMBA, to maintain cellular homeostasis during oxidative stress (Fig. 4(c and g)). Nrf2 transcription factor is well known for leading the induction of phase II detoxification enzymes during oxidative stress, and we have already demonstrated an induction of several phase II detoxification enzymes due to the cardamom treatments in ‘DMBA+CARD’ mice (Fig. 3). Moreover, Keap1 is highly expressed in the cytoplasm of the ‘untreated’ and ‘acetone’-treated mouse skin (Fig. 4(d) and Fig. S3(B) of the supplementary material, available online at http://www.journals.cambridge.org/bjn). Loss of Keap1 in the ‘DMBA’-treated skin is restored by cardamom intake, suggesting a reversion of DMBA-associated malfunction in the skin (Fig. 4(f and h)). Although an association between Keap1 and Nrf2 is required by the resting cells, our experimental observations with these two proteins may not be linked to each other in the present scenario. Keap1 has often been found to be expressed in low levels and mutated in patients with cancer(Reference Hayes and McMahon47). Low expression of Keap1 is probably due to the epigenetic silencing via Keap1 promoter methylation(Reference Wang, An and Ji48).
Furthermore, nuclear expression of NF-κB-p65 has been observed in 30–40 % of the epidermal cells in the ‘DMBA’-treated skin (Fig. 5(b and g)) when compared with the ‘untreated’ and ‘acetone’-treated skins (see Fig. S3(C) of the supplementary material, available online at http://www.journals.cambridge.org/bjn and Fig. 5(a and g)). This observation suggests an activation of the NF-κB signalling cascade in carcinogen-treated mice, by facilitating the release of NF-κB-p65 protein from its cytoplasmic inhibitor protein, IκBα. Additionally, IHC with IκBα displayed down-regulation of IκBα expression in the skins of DMBA-treated mice, suggesting that the ability to sequester NF-κB-p65 protein in the cytoplasm was lost (Fig. 5(e and g)). The cardamom treatment restored the expression of NF-κB-p65 protein in the cytoplasm regardless of the deleterious effects of DMBA on the skin (Fig. 5(c and g)). It is possibly due to simultaneous up-regulation of the inhibitory protein IκBα in the cytoplasm (Fig. 5(f and h)) that resembles the resting phase in ‘untreated’ or ‘acetone’-treated mice (see Fig. S3(D) of the supplementary material, available online at http://www.journals.cambridge.org/bjn and Fig. 5(d and h)). We observed subtle differences in the expression levels in NF-κB-p65 or IκBα between the ‘untreated’ and ‘acetone’-treated groups that may be due to the variation in the animal pool. There are multiple lines of evidence supporting the hypothesis that the induction of COX-2 is regulated by NF-κB(Reference Ulivi, Giannoni and Gentili49). Activation of NF-κB occurred due to DMBA application on the mouse skin, and thus there might be an increase in COX-2 expression. Additionally, both SOD and COX-2 expressions are partly regulated by NF-κB. So it is likely that cardamom modulates the NF-κB signalling and induces the expression of SOD to inhibit the translocation of NF-κB-p65 to the nucleus and concurrently block NF-κB activation.
In general, NF-κB activation is often linked with increased survival of the tumour cells and resistance to chemotherapy. Several anti-carcinogenic compounds that could act as potential inhibitors of NF-κB activity are in the process of development for an anticancer therapy(Reference Kim, Hawke and Baldwin50). However, activation of NF-κB can also sensitise cells to apoptosis(Reference Perkins and Gilmore51). For example, a combination of both UV radiation and adriamycin treatment can activate the NF-κB signalling pathway, which in turn inhibits the expression of a couple of anti-apoptotic genes. Induction of anti-apoptotic proteins by activating NF-κB might be one of the many possible ways that is required for the development of skin carcinogenesis(Reference Kobielak and Fuchs52). Activation of NF-κB has been convincingly shown to promote melanoma progression(Reference Huang, DeGuzman and Bucana53, Reference Payne and Cornelius54). Furthermore, in dysplastic nevi and melanoma lesions, NF-κB activity was found to be highly up-regulated when compared with the normal human nevi or melanocytes(Reference Payne and Cornelius54, Reference Richmond55). Thus, expression of any proteins or agent/s that could potentially deactivate NF-κB would be of high interest in the therapy against skin carcinogenesis. For example, in keratinocytes, expression of mutant JUN leads to the down-regulation of NF-κB and that eventually suppresses the tumour phenotype(Reference Li, Rhim and Schlegel56). In contrast, it has also been reported that mice with down-regulated NF-κB function display features of squamous cell carcinoma(Reference Dajee, Lazarov and Zhang57). Similar effects have been shown by using lupeol, an anticarcinogenic compound, on TPA-induced skin papillomatogenesis in CD1 mice. Lupeol treatment helps in the reduction of skin oedema/hyperplasia, and it is associated with the decrease in the expression/activity of COX-2, NO synthase and epidermal ornithine decarboxylase. Additionally, a decrease in the activation of phosphatidylinositol 3-kinase (PI3K) and NF-κB signalling, as well as a decrease in the degradation of IκBα, was observed in lupeol-treated mice(Reference Saleem, Afaq and Adhami58). Another group also showed that skin papillomas generated in DMBA/TPA in LACA mice were associated with increased expression of NF-κB and activator protein 1 (AP1). Inhibition of papillomatosis by Azadirachta indica (a leaf extract) was accompanied by the induction of signal transduces and activator of transcription 1/AP1 and simultaneously knocked down the activity of NF-κB(Reference Arora, Bansal and Koul59).
In the present study, we have also shown the histology of mouse skin obtained from different groups of mice. Histology of the skin from the ‘DMBA+CARD’-treated group showed a near-normal phenotype similar to either the ‘acetone’ or ‘untreated’ group (no squamous cell carcinoma characteristics), which was remarkably different from the ‘DMBA’-treated group (Fig. S2 of the supplementary material, available online at http://www.journals.cambridge.org/bjn). Extrapolating these facts, we can state that cardamom might also have an impact on the function and expression of TNF-α. NF-κB activation also facilitates COX-2 expression. We have showed that cardamom ingestion in DMBA-treated mice shows down-regulation of COX-2, and could potentially also down-regulate NO synthase and epidermal ornithine decarboxylase. Moreover, cardamom might also modulate the PI3K and AP1 signalling pathways to restore the normal cellular homeostasis of the papilloma-bearing cells.
It is well known that squamous cell carcinoma, which are responsible for the majority of NMSC-related deaths, result from the accumulation of genetic alterations. Several molecular events occur in skin epidermal cells following UV exposure such DNA damage, generation of ROS, induction of p53 and p53-regulated proteins, cell-cycle arrest, DNA repair and apoptosis. Natural phytoproducts, such as cardamom, with antitumorigenic properties have an immense potential to maintain cellular homeostasis when continuously taken as dietary supplements. There are several active components of cardamom and not all the components are examined separately. Several reports have demonstrated that most of the components of cardamom act as antioxidants such as limonene, cineole, linalool, pinene and borneol(Reference Acharya, Das and Singh9). Cardamom contains Cu and Mn that are required for the activation of SOD enzyme, which in turn helps in the decrease in the process of lipid peroxidation. So in conclusion, generation of DMBA-induced skin papillomatogenesis most probably mimics UV-induced NMSC in humans, and the present data suggest that whole cardamom as a nutritional diet plays an anti-carcinogenic role in preventing the progression of skin carcinogenesis in mice. Further investigations with individual components are required to establish the chemopreventive role of cardamom against NMSC.
Acknowledgements
I. D. wishes to thank the Director, Jaydeep Biswas, and all the other staff members of the Department of Cancer Chemoprevention, CNCI. T. S. thanks the Lombardi Comprehensive Cancer Center, Histopathology core and acknowledges the support from the pilot grants from the American Cancer Society (IRG no. 97-152-16-2) and the Fisher Center for Familial Cancer Center, Georgetown University (Washington, DC, USA). The authors' contributions are as follows: I. D. designed and performed the experiments (mouse set-up, tissue preparation, biochemical and immunohistochemical assays) as well as assisted in organising the manuscript; A. A. performed the experiments (immunoblotting with the tissue lysates) and reviewed the writing of the manuscript. D. L. B., S. S., E. W. and E. P. were involved in tissue handing, slide preparation, haematoxylin and eosin and IHC staining of the skin slides in the USA. A. S. and S. B. provided space and reagents in India. T. S. supervised the research, designed the experiments, provided the reagents, space and scholarly wrote the manuscript. The authors declare that they have no conflict of interest.









