Introduction
In mass casualty incidents (MCI), the immediate needs of the affected community usually exceed the available resources. It is essential to allocate the available resources in a way to ‘treat first what kills first’ and ‘do the most, for the most.’ Reference Nakao, Ukai and Kotani1-6 Categorizing casualties by priority of medical needs until transport and evacuation are available, is called triage. The idea behind triage is to use the available resources and treatments as efficient as possible and save the highest possible number of victims. To facilitate this process, ‘triage systems’ are developed. Reference Nakao, Ukai and Kotani1-6 The first records regarding medical triage can be found from the military surgeons, DJ Larry (1766-1842) and PF Percy (1754-1825), of Napoleon Bonaparte’s army. Larry developed a triage system for wounded soldiers and Percy developed an ambulance system to transport them. Reference Nakao, Ukai and Kotani1,Reference Kennedy, Aghababian, Gans and Lewis4,Reference Jenkins, McCarthy and Sauer5,Reference Burris, Welling and Rich7 These concepts of primary triage were used by Napoleon in a military perspective to give priority to wounded or sick soldiers who were able to fight again on the battlefield. Reference Nakao, Ukai and Kotani1 In modern medicine, the aim is to treat casualties to save as many lives as possible. Triage is an ongoing and repetitive process at various stages to detect possible deterioration. Nowadays, triage is also used in many hospitals in the context of disaster training and preparedness. Reference Nakao, Ukai and Kotani1-6,8 Under-triage and over-triage may occur, regardless of the triage tool used. Under-triage tests the sensitivity of identifying critically ill patients. However, it is dangerous because it means that critical injuries might not be recognized and can thus affect mortality. Reference Frykberg2,Reference Kennedy, Aghababian, Gans and Lewis4,6 Over-triage occurs when slightly injured patients are incorrectly identified as critical ill and receive a higher level of healthcare than actually needed. Over-triage is dangerous too as it diverts assessment and treatment from other patients who need it more. Reference Frykberg2,Reference Kennedy, Aghababian, Gans and Lewis4,6 In general, a certain rate of over-triage is accepted to avoid under-triage. Reference Frykberg2,Reference Kennedy, Aghababian, Gans and Lewis4,6
After a disaster occurs, emergency services need time to arrive at the incident scene and the initial amount of medical help available will probably be less than the demand for medical help by large numbers of patients or multiple critically injured patients. Therefore, the affected community needs to be prepared to manage the incident during the early stages. Reference Waeckerle3 Ideally, medical personnel with experience with trauma patients and MCI should be at the scene immediately after a disaster, but usually only people without medical experience will be on site. In general, these lay person first responders (LPFRs) will, without guidance, not be able to give targeted medical assistance. This concerns people who do not have a professional medical role in a MCI, and, who have completed at most, basic first aid training. However, in some conditions it is important to perform life-saving actions as quickly as possible. 6,8 It would be desirable for LPFRs to be able to perform some important life-saving actions and be able to identify casualties who are in urgent need of help. Early actions of LPFRs could positively contribute to health benefits for casualties. In this context, even the slightly injured patients could help the severely injured casualties as usually, only 10-25% of all casualties in moderate size disasters of 100-200 casualties are seriously injured. Reference Frykberg2,Reference Waeckerle3,6 In major earthquakes, only a small amount of victims are rescued by international professional rescue teams. Most victims will be rescued by family members, neighbors and other local citizens. Reference Peleg9,Reference Uscher-Pines, Chandra, Acosta and Kellermann10 Several studies have determined that these local citizens account for 50% to 95% of survivors following major earthquakes. Reference Peleg, Reuveni and Stein11
Little is known about the capabilities of lay people to perform the earlier mentioned actions. It is known, that official ‘first responders’ without certified medical experience in the field like police officers and firefighters, show a significantly improved triage accuracy after providing them appropriate triage decision-support materials. Reference Kilner and Hall12-Reference Wolf, Bigalke, Graf, Birkholz and Dittmar16
This article intends to clarify this lack of knowledge with respect to lay people without official functions as a ‘first provider.’ The primary aim of this study is to identify whether there are prehospital triage tools for lay people published and if not, to develop a prehospital triage tool to make it possible for LPFRs to perform triage and start basic life support in MCIs. This could potentially lead to more prepared citizens and contributes to a resilient community. Reference Plough, Fielding and Chandra17,Reference Patel, Rogers, Amlôt and Rubin18
Methods
Study Design
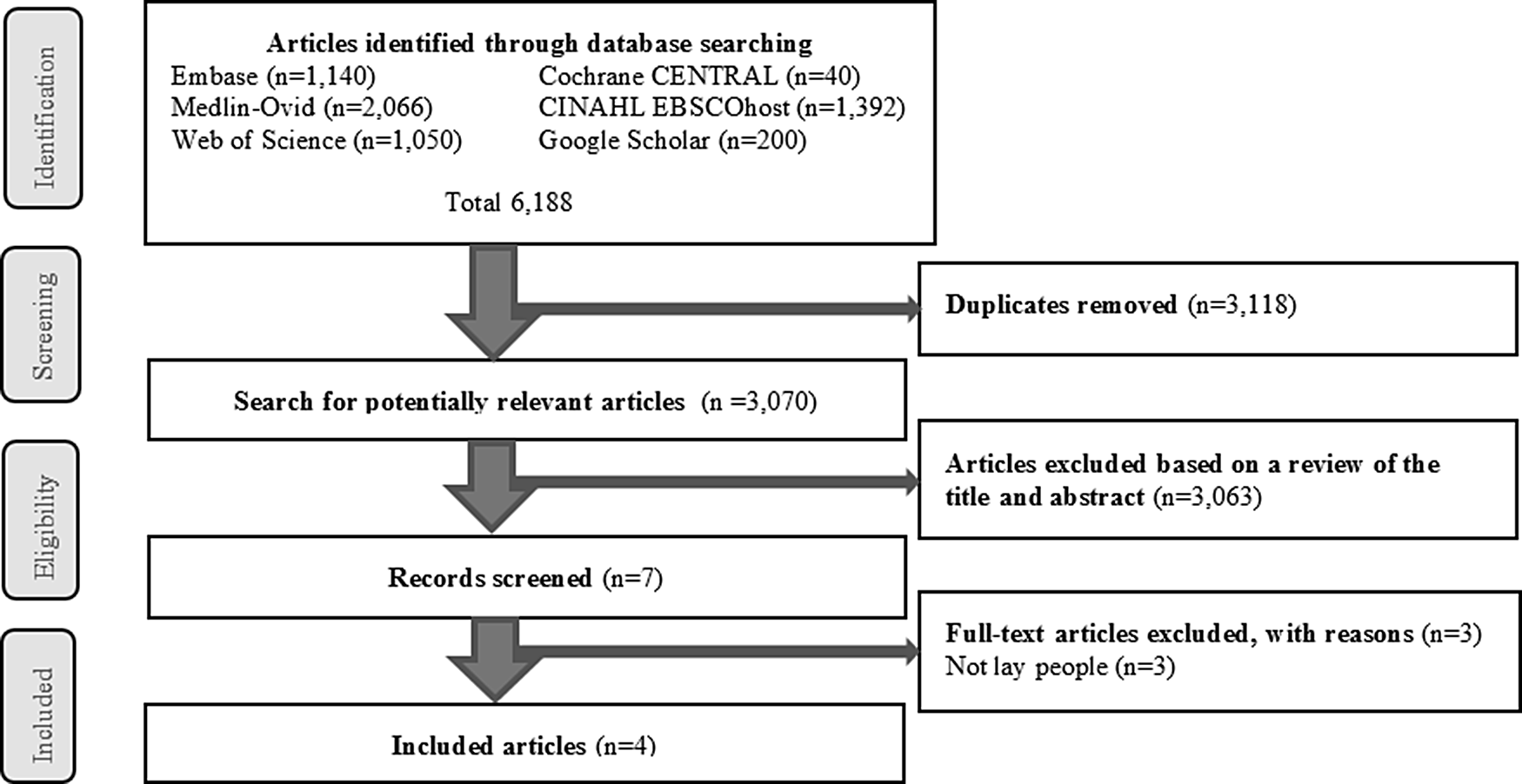
This study set out to be a scoping review of the available, published prehospital triage tools for lay people. To identify those triage tools, a literature search was conducted to identify what is already known about the application of prehospital triage tools by lay people. Although this study is a scoping review, we followed the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) protocol. Reference Moher, Shamseer and Clarke19 The PRISMA 2009 checklist is submitted as Appendix 1.
Search Methods and Inclusion Criteria
In July 2019, Embase (Elsevier, Amsterdam, Netherlands), Web of Science (Thomson Reuters, New York, NY), Cochrane (The Cochrane Collaboration, London, United Kingdom), CINAHL EBSCOhost (EBSCO, Ipswich, MA), Google Scholar (Google Inc, Mountain View, CA), and Medline (PubMed, National Library of Medicine, Bethesda, MD) databases were consulted for data extraction for our primary outcome. Published full-text English language articles were searched by connecting MeSH major topic terms of “prehospital” OR “mass disaster” OR “natural disaster” OR “mass casualty incident” OR “triage” OR “disaster planning” OR “attack” OR “terrorism.” The search strategies were developed in collaboration with an information specialist. The inclusion of subject headings were as appropriate for each database and relevant free-text terms. The search results were limited to humans and no language limits were applied. Reference lists of included studies were hand searched for additional materials. For the full literary search strategy, see Appendix 2. Only studies addressing prehospital triage methods for lay people were included in our analysis. All in-hospital triage tools and articles concerning medical personnel were excluded from this search. To collect prehospital triage models for the second step of this review, all available prehospital triage models as published in relevant recently published reviews were collected.
Data Collection
WJ and JS, were 2 authors who independently reviewed the yielded studies in EndNote X9© (Clarivate Analytics, Boston, MA, USA) where clearly ineligible titles and abstracts were excluded at this stage to determine the inclusion or exclusion of studies for full-text review. Consensus was reached by matching the inclusion criteria and keywords. Disagreements were discussed until a consensus was reached and concerns were resolved. In addition, a third researcher (MK) was involved when necessary. Controversies and disparities during the study selection were resolved by general consensus among the researchers. An identical process was used to determine the final inclusion of full-text articles, listed in Table 1.
Table 1. Overview of reviewed articles
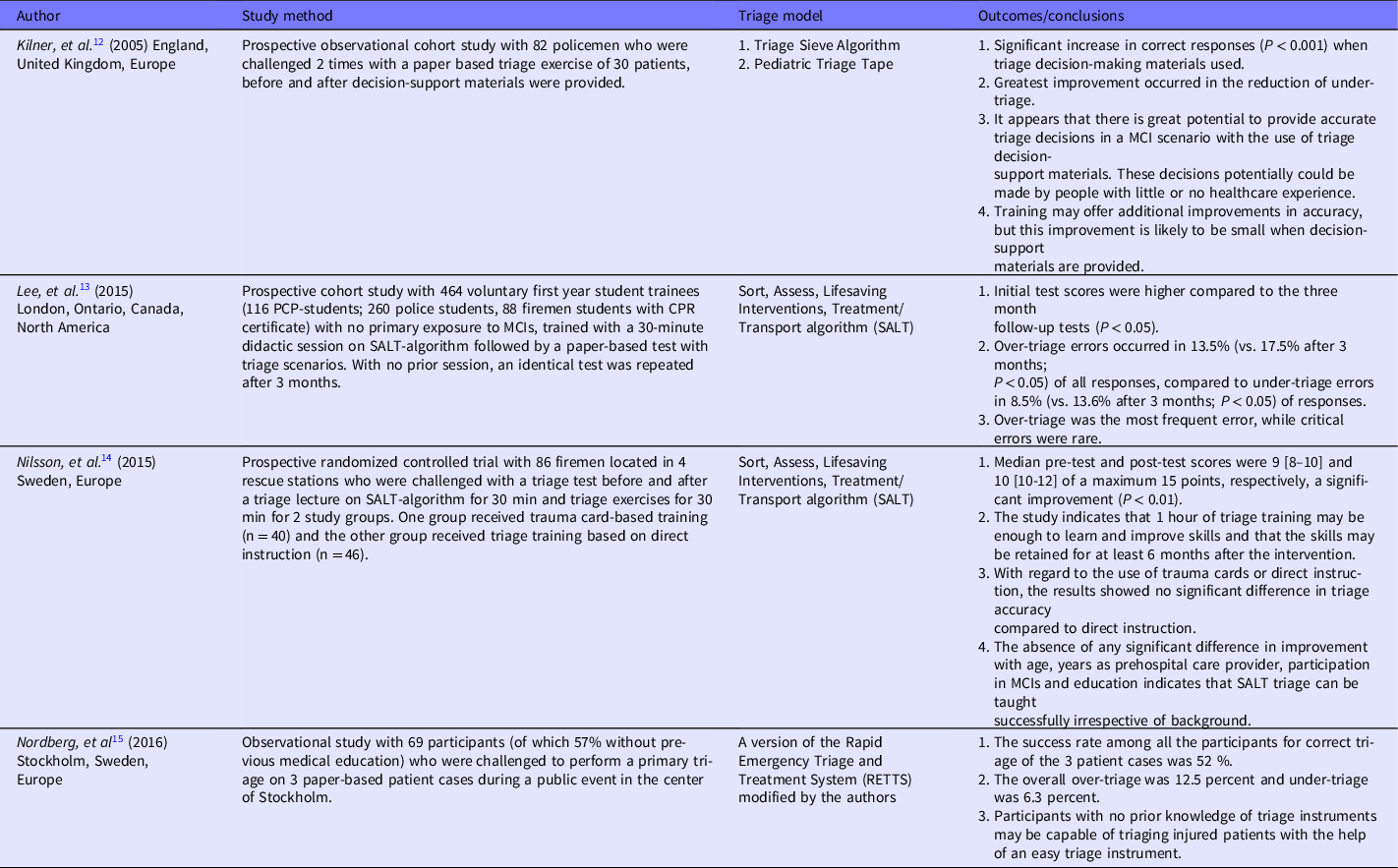
Abbreviations: PCP, Primary Care Provider; MCI, Mass Casualty Incident; EMS, Emergency Medical Services.
Development of a Prehospital Triage Tool for Lay People
The second step in this study was the development of a prehospital triage tool for lay people in a MCI, based on the most well-known prehospital triage tools. Based on the opinion of the authors, and their experience in the field of life support, the goal was to develop a new triage model with actions which are most suitable for LPFRs. Per triage-step, there is an easy-to-follow route with basic life support actions that are considered to be executable by lay people. To develop such a tool, a search for prehospital triage models available in literature was conducted in our database and triage actions were extracted. All relevant triage tools available in recent literature, as listed in Table 2, were valued. The triage tools were analyzed, evaluated and sorted per triage action. These actions were divided into lifesaving actions in the triage categories “mobility,” “airway/breathing,” “circulation,” “disability,” and “other actions.” All categories were ranked according to the order in which they were displayed per individual triage tool. So for example, if a triage tool has ‘mobility’ as the first step in the triage, then it was scored a ‘1,’ if ‘circulation’ was the second step, it was scored a ‘2.’ The average ranking order per different triage tool is showed in Table 3. These outcomes determined the order of steps in prehospital triage. In Table 4 (Appendix 3), all individual triage actions per category are shown. For each action, the following points were described:
-
1) Whether the action is applicable for LPFRs;
-
2) How LPFRs can determine the individual action;
-
3) How, if possible, the action could be modified to make it applicable for LPFRs;
-
4) Which actions in basic life support could be provided in the specific triage category.
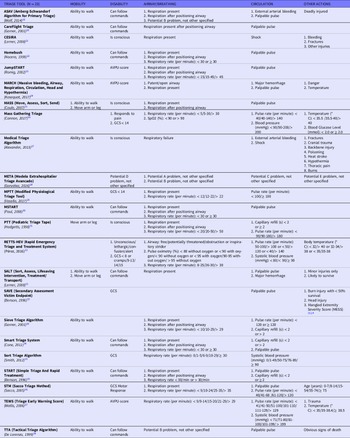
Table 2. Overview of prehospital triage tools, divided per category and actions

Abbreviations: AVPU, alert, verbal, pain, unresponsive; GCS, Glasgow coma score; SpO2, saturation of peripheral oxygen.
Table 3. Overview of prehospital triage tools with order ranking per category of actions

If there were disagreements between the authors (WJ, JS) then a third author (MK) was involved into the discussion. Based on all results in the second step, a prehospital triage tool for LPFRs was developed by selecting to reviewers’ best knowledge, the most suitable set of actions in all different triage steps.
Patient and Public Involvement
Neither patients nor the public were involved in the design, conduct, or reporting of this review at this time.
Results
Initial Search Results
Our initial search resulted in 6188 articles, and after removing all duplicates, into 3070 articles (Figure 1). After screening, there were 2411 articles excluded because of the title and 652 articles excluded because of the abstract which did not match with our primary subject. A total of 7 full text articles were screened and 3 were excluded because the content of the article was not about prehospital triage by lay people. Eventually, 4 articles were included in the scoping review. Reference Kilner and Hall12-Reference Nordberg, Castrén and Lindström15

Figure 1. Flow diagram of the article selection procedure based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline.
Table 1 shows the 4 reviewed articles. Kilner et al, Reference Kilner and Hall12 conducted a prospective observational cohort study with 82 police officers to determine if a paper-based triage test showed better results with triage decision-support materials (Triage Sieve Algorithm and Pediatric Triage Tape) compared to not having these materials. They found a significant increase in correct responses (P < 0.001) when triage decision-making materials were used and stated that there is a great potential to provide accurate triage decisions in a MCI scenario with the use of triage decision-support materials. These decisions potentially could be made by people with little or no healthcare experience. Reference Kilner and Hall12
A prospective cohort study with 464 first year trainees, consisting of firefighters, police officers, and primary care students, was conducted by Lee, et al. Reference Lee, McLeod and Peddle13 The study population was trained in a 30-minute didactic session on SALT-algorithm followed by a paper-based test with triage scenarios. With no prior session, an identical test was repeated after 3 months. The study showed that over-triage and under-triage errors occurred in 13.5% (vs. 17.5% after 3 months; P < 0.05) and 8.5% (vs. 13.6% after 3 months; P < 0.05) of responses, respectively, while critical errors were rare. The researchers concluded that 3 months after the initial training period, all first responder groups showed a decline in triage accuracy. Reference Lee, McLeod and Peddle13
Nilsson, et al. Reference Nilsson, Åslund, Lampi, Nilsson and Jonson14 conducted a prospective randomized controlled trial with 86 firefighters, divided into 2 groups, who were challenged with a triage test before and after a joint 30-minute lecture on SALT-algorithm followed by a trauma card-based training (n = 40) or a direct instruction training (n = 46). The study showed a significant improvement in triage accuracy test scores after training and indicates that an hour of triage training may be enough to learn and improve skills. There was no difference in scores found between the 2 training methods. They further found the absence of any significant difference in improvement with age, years as prehospital care provider, participation in MCIs and education and stated that SALT-triage can be taught successfully irrespective of background. Reference Nilsson, Åslund, Lampi, Nilsson and Jonson14
Finally, Nordberg, et al. Reference Nordberg, Castrén and Lindström15 conducted an observational study with 69 participants (of which 57% were without previous medical education) who were challenged to perform a primary triage on 3 paper-based patient cases during a public event in the center of Stockholm, Sweden. The aim of this study was to evaluate whether bystanders with no training in triage, also known as lay people, can correctly prioritize 3 injured patients by using a triage tool. The authors modified an existing hospital triage tool, the Rapid Emergency Triage and Treatment System (RETTS), and supplied this to the study participants to perform triage correctly. The results showed that the success rate among all the participants for correct triage of the 3 patient cases was 52% with an overall over-triage of 12.5% and an under-triage of 6.3%. The researchers concluded that participants with no prior knowledge of triage instruments may be capable of triaging injured patients with the help of an easy triage instrument, but future research is needed to further evaluate triage by non-medical bystanders. The researchers proposed that by using a Smartphone application, it may be possible for a bystander to use the triage instrument. The emergency medical dispatcher (EMD) could send the application to the caller when the EMD needs support with the prioritization of available resources. Reference Nordberg, Castrén and Lindström15
Prehospital Triage Tools
For the second step of this review we extracted the review of Bazyar, et al. Reference Bazyar, Farrokhi and Khankeh39 from our initial literature search. This recent review describes an overview of the most well-known prehospital triage tools available in literature. Based on this review we found all original articles for available prehospital triage tools, extracted them, and added extra triage tools when found unmentioned in Bazyar, et al. Reference Bazyar, Farrokhi and Khankeh39 Our search yielded a total of 23 prehospital triage tools. Table 2 shows an overview of all the prehospital triage tools, as described in the methodology (Development of a Prehospital Triage Tool for Lay People).
From each triage tool, all actions are described per category to create an overview of any similarities between the different tools. When triage actions do not match one of the 4 main categories “mobility,” “disability,” “airway/breathing,” or “circulation,” they are assigned to “other actions.”
All individual categories are ranked based on their average order of action in the different triage tools as showed in Table 3. The field is blank if a triage tool did not use a certain category. Overall, it shows that assessing “mobility” (mean 1.2; n = 17) is the first category that will be scored in prehospital triage, but not every triage tool uses this category. Respectively, “respiratory,” “circulatory,” and “mental status,” were the second (mean 2.2; n = 22), third (mean 2.9; n = 22) and fourth (mean 3.3; n = 21) in order of triage actions during prehospital triage.
Keep it Safe and Simple (KISS) Triage Tool
The results of the development process of the tool are shown in Table 4 (Appendix 3). Simple basic life support proceedings were added if they seemed suitable for LPFRs. Examples of these were, ‘placing people in a comfortable position,’ ‘opening of the airway,’ ‘put pressure on wounds,’ ‘bring casualties in the recovery position,’ and ‘check breathing,’ Based on Tables 2, 3, and 4, we developed the ‘Keep it Safe and Simple’ (KISS) prehospital triage tool for LPFRs (Figure 2).
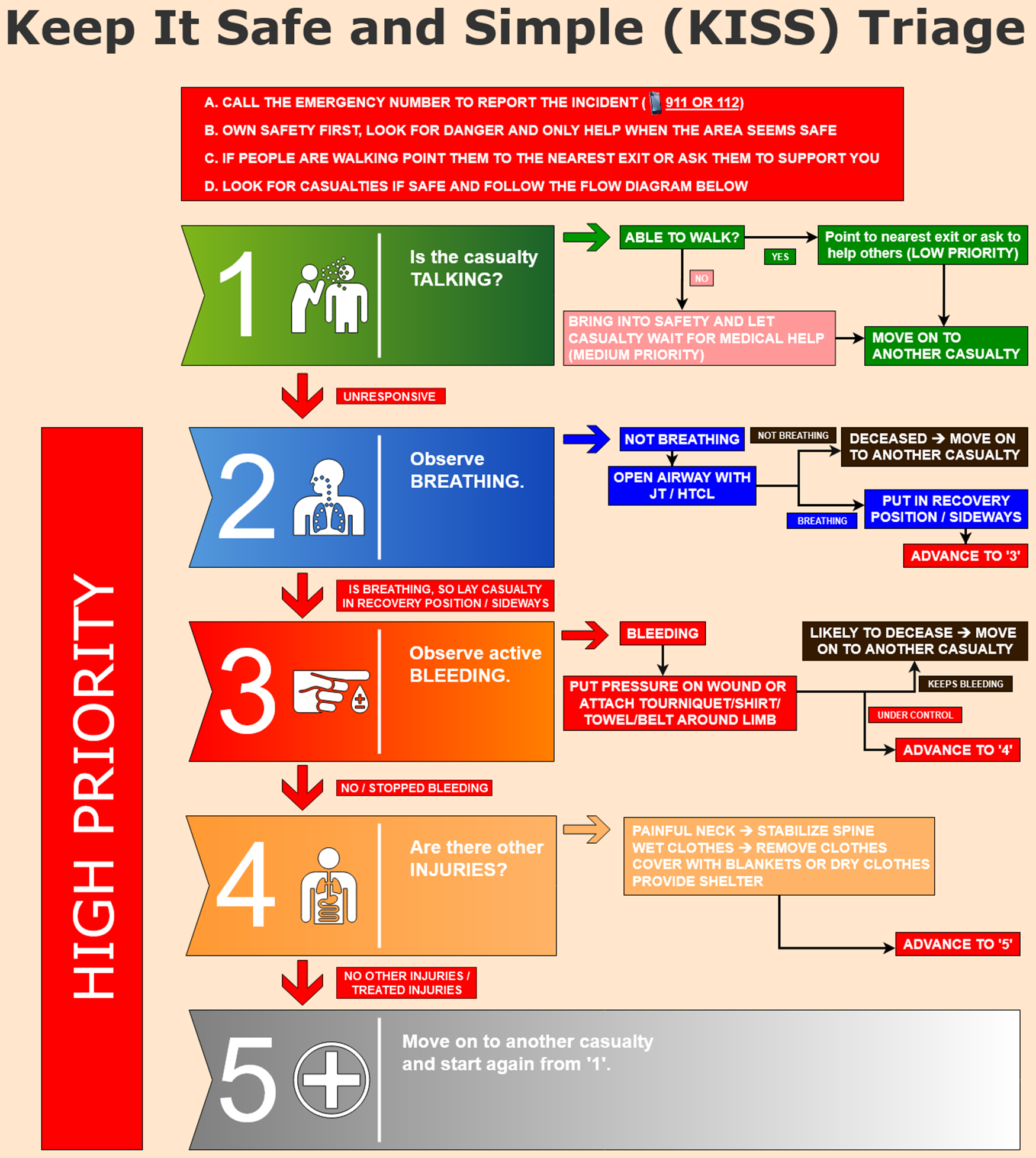
Figure 2. Keep It Safe and Simple Triage tool for lay person first responders.
First Response
The first priority of an unharmed or minor injured LPFR in a MCI is to report the incident to the emergency dispatch center and ensure his/her own safety. Nobody should be obliged to offer help in an unsafe situation. When the scene is relatively safe, the second priority should be starting Basic Life Support for those casualties who are in the most urgent need for help and “do the most, for the most.” The KISS triage tool can be used to triage multiple casualties in a structured way, with scene safety taken into account (Figure 2, step 1). We divided the priority scale into low, medium and high priority medical attention. The tool is developed as a flow diagram to follow 5 steps in which the LPFR can assess the priority fitting the casualty’s situation. If a casualty is talking and able to walk, it indicates that, for now, this is a low priority casualty and attention can be directed at the patient not able to move. The low priority casualties are supposed to be able to gather at a tactical location or could possibly even help with the first treatment of more injured casualties, at least until emergency medical services arrive at the scene. If the casualty is responsive but not able to walk it is scored as a “medium priority” casualty. It is important to safely stabilize the casualty if possible and let them wait for medical help. Having done so, the LPFR will move on to another casualty to perform triage and provide basic life support (BLS). If the casualty is not responding, this indicates a “high priority” casualty in need of urgent medical care, so the LPFR should immediately advance to step 2.
Breathing
At step 2, the LPFR should check if the casualty is breathing. When breathing, the casualty should be placed in the recovery position and advance to step 3. In the case of a non-breathing casualty, the LPFR should open the airway, with a head-tilt chin lift or jaw thrust, body fluids (blood, vomit) in the oral cavity should be removed, and then check if the casualty is breathing. If the casualty is still not breathing, it is likely that there was also a cardiac arrest and that the casualty is deceased. In a MCI there is no capacity for cardiopulmonary resuscitation (CPR). The LPFR should move on to another casualty to help. If the casualty is breathing after the previous mentioned maneuvers, the casualty should be put in the recovery position and the LPFR should advance to step 3.
Bleeding
In step 3, the LPFR should observe for active bleedings on the body of the casualty. If the casualty is losing much blood from an extremity, a tourniquet should be placed proximal to the bleeding site to stop the bleeding. If this is not available, a belt, towel, rope, etcetera, could be placed proximal to the wound to cut off the blood supply due to pressure. In the event of a non-extremity bleeding (e.g., abdomen or thoracic) it is necessary to put pressure on the wound. If above mentioned interventions do not stop the bleeding, the casualty is likely to decease and the LPFR should move on to help another casualty. If the bleeding stops, the LPFR should advance to step 4.
Other Injuries and Transportation
At last, the LPFR should check for other injuries and, if necessary, treat those injuries. In case of a painful neck, the spine should be stabilized, so the casualty cannot accidentally worse an occult spine injury. Wet clothes should be removed and exchanged for dry clothes or blankets to prevent hypothermia. The LPFR should try to perform triage for as many casualties as possible, so if he or she advances to step 5, they should move on to another casualty. The LPFR should draw attention from the first responding medical personnel to direct professional medical help to all “high priority” casualties as soon as possible. After this, the LPFR can follow orders from the responding medical personnel.
Discussion
A scoping review was conducted of studies which examined the use of prehospital triage tools in non-healthcare workers. According to the results (Table 1) we conclude that there is little, but consistent research published on this subject. Of all 632 studies about prehospital triage, four of them were about lay people, but they overall stated that there is great potential to provide accurate prehospital triage by people with little or no healthcare experience and that these LPFRs may be able to assist with MCI field triage. Reference Kilner and Hall12-Reference Nordberg, Castrén and Lindström15 Furthermore, Lee et al. concluded that critical errors were rare, over-triage was most common and that the accuracy can be improved with decision-support materials. Reference Lee, McLeod and Peddle13 These results may implicate that a prehospital triage tool for lay people, who are in fact the “real” first responders in a MCI, will be useful and contributing to help professional medical first responders to determine faster who most urgently needs help in a MCI and possibly provide lifesaving actions as well.
The tool is developed for LPFRs who are present at the disaster scene immediately after occurrence, but who are not severely injured. In Figure 2 the tool is displayed as a flow diagram in which simple steps can be followed to perform the triage and basic life support actions. Based on the reviewed literature, the order of talking, breathing, bleeding and other injuries was consciously chosen for the triage tool. This literary study showed that, on average, the most commonly used triage models adhere to this order (Table 3). Therefore, the KISS-triage tool does not fully follow the order according to the universal ABCDE-principles in trauma used at emergency departments.
This triage tool differs from existing published literature in the way that it is a new developed prehospital triage tool based on the most well-known existing tools for medical personnel. The most basic steps are presented in an easy-to-follow flow diagram (Figure 2) where LPFRs can do the most for the most and buy time for medical first responders who are on their way to the scene. The concept is that medical responders will approach seriously injured casualties who have a chance of surviving after primary lay people triage. Ideally, due to the possible fact that LPFRs “filtered” non-survivors out of the many casualties at the scene or started treating casualties (e.g., recovery position, stop bleedings, and so on).
The future goal for the KISS-triage tool is attempting to improve disaster preparedness and create more awareness of giving first aid among citizens. Ideally, it will show that performing triage and providing help does not have to be difficult and may be beneficial for casualty outcomes. This may contribute to a more resilient community. Reference Plough, Fielding and Chandra17,Reference Patel, Rogers, Amlôt and Rubin18 An effect of the KISS-triage tool might be that LPFRs may also feel empowered and prepared to help, even though they have limited resources to make a difference. However, this tool is not validated and used in practice yet, so therefore predictions of potential beneficial outcomes are unreliable and have to be drawn with caution. Possible ways to validate the tool are with Emergo Train System©, computer simulation, scenario training or blended exercise. After a successful validation study, possible ways to implicate the tool for use within the community should be explored. To create more awareness among citizens, the KISS-triage tool should be easily available for everyone. Today, almost everyone has a smartphone, so configuring the KISS-triage tool into a simple and easy-to-follow mobile application (app), might be a helpful method. Mobile phone developers could install this app as default on their phones to be activated immediately in the event of a MCI. For example, in the Netherlands there is a governmental alert service, called NL-ALERT. 40 It automatically alarms people who are near a disaster scene to create awareness and give advice of what to do in this particular situation. Such a message might directly activate the KISS-triage tool app after which people nearby the MCI can follow the triage flow diagram. As a future addition to the KISS-triage tool, an addendum to use in different types of MCI could be developed. For example, shooting, chemical, nuclear or natural disasters. This addenda should than be available in emergency dispatch centers, so whenever a LPFR calls the emergency number, they get direct instructions through the phone on how to approach the situation. The tool could, for example, be implemented in elementary school or during first aid lessons to get people familiar with the tool starting from young age. Police officers and firefighters could have scenario training and follow the KISS-triage tool to get used to the tool. The smooth spread of automatic external defibrillators in the public space has shown, that people can adopt to modern tools when they understand the advantage of the tool. Reference Mao and Ong41 Because of the un-validated state of our triage tool, hard and definitive conclusions cannot be made at this point, therefore validation of this triage tool is important in future steps.
Local citizens have a critical role within response structure for large disasters as they are on site immediately after occurrence. Therefore individual citizens have a responsibility to take appropriate steps to protect themselves, their families and their community members. Reference Peleg9-Reference Peleg, Reuveni and Stein11 Prepared citizens in a resilient community may be helpful in the triage in the event of a MCI. Reference Patel, Rogers, Amlôt and Rubin18 Many people have, for example, a first aid kit in their car and in some countries, civilians take mandatory first aid courses, so the life support basics are known to many people. Implementation of basic life support training in elementary/high school or in-company and mobile application tutorials might further enhance this ability for lifesaving actions. LPFRs who are at the scene at the time of the incident might have much information about the trauma mechanism to share with the medical first responders. This may contribute to analyzing the situation faster by the medical responders.
When a triage tool for lay people will be implemented in a community, the process should be monitored closely in order to ascertain and avoid possible risks and legal aspects that may occur. When first responders without medical training provide first aid, they could possibly save lives, but it is also possible that they unintentionally do more harm to a patient. Another issue is what will happen if a LPFR received the KISS-triage tool, but skips an important step or does not follow the instructions. As long as such a triage tool is not required by the government, individual willingness to use such a tool is required and the care provider in question remains responsible for doing so. Law and regulations will differ in different countries. In most countries, citizens have a responsibility to help at the level they are capable of and it is an offense not to help someone in distress. An example of this is found in the Netherlands. 42 Ideally, such a tool should be implemented by the government to shield citizens from legal law. If a triage tool for lay people will not implemented by the government, local laws and regulations must be checked in future steps to prevent citizens from being confronted with undesirable surprises if they tried to help in good conscience, but their help resulted in adverse consequences.
At last, our scoping review showed that the most frequent error that was made by lay people is over-triage. This may cause delay for the casualties who need most urgent help, but then again, if the medical first responders have to triage all casualties, it will also delay the time to help. In contrast, Kim, et al. Reference Kim and Lee43 studied a group of 34 graduating nursing students who were, after a 70-min lecture about the START algorithm and MCI care, Reference Benson, Koenig and Schultz33 challenged with performing triage on casualties of a MCI simulation scenario. They found that of all incorrect answers, 73% were related to under-triage and attributed this to the lack of clinical experience of the graduating nursing students. Under-triage may also be a frequent error found in lay people, so a validation study for the KISS-triage tool and further research in prehospital triage by lay people is necessary.
Limitations
Like every other study, our study has limitations. First, our scoping review yielded 4 articles (n = 701 lay people), which indicates that there is little evidence regarding prehospital triage by lay people, and that conclusions from this analysis should be drawn with caution.
Second, this is a relatively new concept of triage and not yet a validated prehospital triage tool. The studies mentioned in this scoping review are mostly based on police officers, firefighters and students, and not on the common citizen, which makes the external validity, for using these tools by the common citizen, doubtful.
Third, the question is whether lay people can perform simple actions (such as a jaw thrust or head tilt chin lift) without training. The most suitable actions to be able to perform by LPFRs following the KISS-triage tool were based on the expert opinions of three researchers with experience in the field of triage and trauma medicine. The use of a Delphi method would be a better choice to evaluate these most suitable actions and could be a great added value for a follow up article. Another limitation is that using and obeying the guidelines of the KISS-triage tool is voluntary. If a LPFR ‘freezes’ or does not wish to use the tool, there will be no benefits of the tool. At last, this prehospital triage tool for LPFRs is not yet validated. All conclusions and potential benefits should therefore be drawn with caution. We share this non-validated version of the tool and look for partners to cooperate with us in the validation process.
Conclusion
In conclusion, this scoping review on prehospital triage by lay people in a mass casualty incident showed that there is little research published on this subject yet. On the other side, there is a great potential to provide accurate prehospital triage even by people with little or no healthcare experience. Lay people may be able to assist with mass casualty incident field triage and their triage accuracy can be improved with decision-support materials. These results implicate that the prehospital triage tool for lay people first responders (Figure 2) could be useful and contributing to help medical first responders to determine faster who most urgently needs help in a MCI. Future research, implementation methods, validation and training has to show whether this prehospital triage tool for lay people first responders is suitable to use in mass casualty incidents.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/dmp.2021.19
Acknowledgements
The authors would like to thank Wichor M Bramer, PhD as biomedical information specialist from the Erasmus Medical Center medical library for the collaboration in developing the literary search strategy.
Authors’ Contributions
WJ, JS, and MK analyzed and interpreted all data. WJ and JS developed all tables and figures. WJ, JS, and MK were all major contributors in writing the manuscript. All authors read and approved the final manuscript. WJ and JS contributed equally to this work.
Availability of Data and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare that they have no competing interests.
Funding
The authors did not receive any form of funding or financial support.