Focal cortical dysplasia (FCD) refers to malformation of cortical development with abnormalities of cortical layering, neuronal differentiation, and maturation.Reference Prayson 1 Focal cortical dysplasia is responsible for most cases of medically refractory epilepsy in the paediatric population, and medically intractable seizures in adults.Reference Palmini 2 The coexistence of FCD and low-grade glial tumours such as ganglioglioma (GG) and dysembryoplastic neuroepithelial tumour (DNT) have been classified by the International League Against Epilepsy (ILAE) as FCD Type IIIb.Reference Blümcke, Thom and Aronica 3 Patients with FCD Type IIIb generally present with increased seizure frequency compared with isolated FCD or brain tumours.Reference Santos, de Oliveira and Machado 4 Herein, we describe the first report of FCD Type IIIb discovered incidentally in a seizure-free patient, which is the fifth reported case associated with oligodendroglioma.Reference Santos, de Oliveira and Machado 4 , Reference Cossu, Fuschillo and Bramerio 5
A 20-year-old male with suspected arteriovenous malformation of the right pinna underwent MRI. None was found; however, the gadolinium-enhanced MRI showed an incidental solitary lesion (32×30×17 mm) in the medial right frontal lobe (Figure 1), involving the parasagittal cortical ribbon and subcortical white matter. The area was hypo-intense on T1-weighted imaging and hyper-intense on T2, with no diffusion abnormality or enhancement. There was no midline shift, hydrocephalus, or abnormal flow void(s). The patient had no neurological or systemic symptoms. Past medical, family, and social history were unremarkable.
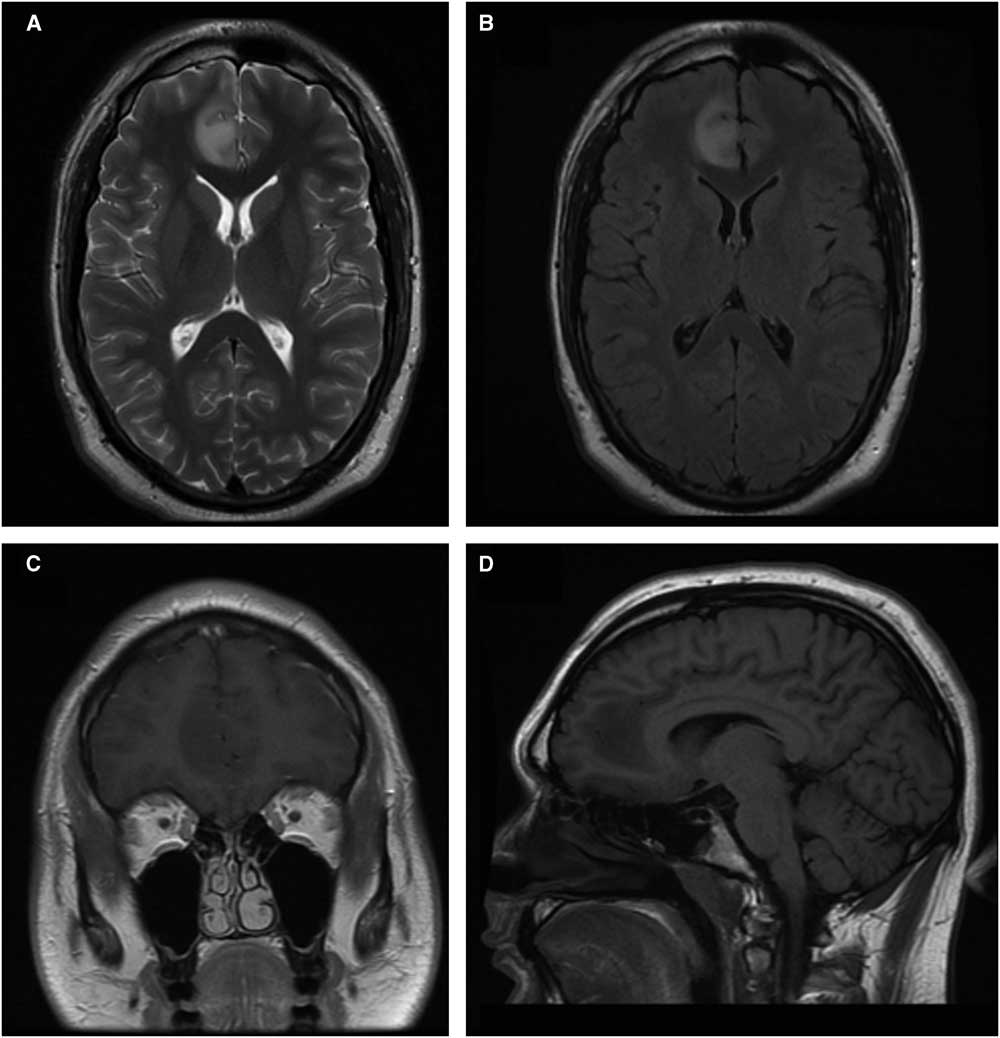
Figure 1 MRI images of focal cortical dysplasia associated with oligodendroglioma. Axial (A) and axial fluid-atenuated-inversion-recovery (B) T2-weighted images. Coronal gadolinium enhanced (C) and sagittal (D) T1-weight imaging.
Bifrontal craniotomy and resection of the tumour was performed without complication.
The right frontal lobe neoplasm consisted of cells with round to oval nuclei with minimal atypia. Many cells displayed perinuclear halos (Figure 2A). Some of these infiltrated the adjacent cortex, forming perineuronal aggregates. One mitosis was noted in the entire specimen. These appearances are those of a low-grade oligodendroglioma. A higher-grade was excluded by the absence of more than a few mitoses, necrosis, and vascular proliferation. Other low-grade gliomas were excluded by the absence of dysplastic ganglion cells or perivascular inflammation, specific glioneuronal elements, lack of Rosenthal fibres and eosinophilic granular bodies. Immunohistochemical staining showed that the neoplastic cells were positive for the R132H mutant form of isocitrate dehydrogenase (IDH)-1. Ki67 (a proliferation marker) stained no more than 5% of the nuclei in the most heavily stained region. Glial fibrillary acidic protein was mostly negative around the cells, with a rare perinuclear rim. Fluorescent in-situ hybridization studies showed co-deletions of chromosomes 1p and 19q, a molecular hallmark of oligodendroglioma. Cells also exhibited retained nuclear staining for Alpha-Thalassemia/Mental Retardation X-linked (ATRX). This confirmed the diagnosis of oligodendroglioma, IDH-mutant and 1p/19q-codeleted (World Health Organization Grade II).Reference Louis, Perry and Reifenberger 6 The adjacent right frontal cortex showed both tangential and radial disorganization of neurons, the defining features of FCD (Figure 2B, C). Histologically, radial microcolumns are defined as eight or more neurons aligned in a vertical direction, where the section is stained with the neuronal marker NeuN (Neuronal Nuclei), oriented perpendicular to the pial surface.Reference Blümcke, Thom and Aronica 3 Aligned neurons present with a small diameter and cell size of <250 μm2. As emphasized by the black lines in Figure 2C, there are at least three cortical microcolumns present, with at least eight neurons in each. The tangential disorganization is based on the presence of large and small neurons in close proximity, clusters of neurons, and neurons orientated in varying directions, instead of the normal orientation of the axon hillock towards the cortical surface (Figure 2B). The neurons were not themselves dysmorphic (with clumped Nissl substance or nuclear abnormalities including binucleate neurons) and balloon cells were not identified. The cortex was adjacent to the neoplasm, and not infiltrated by it, as indicated by negative staining for mutant IDH-1. By current classification, this is defined as FCD Type IIIb.Reference Blümcke, Thom and Aronica 3
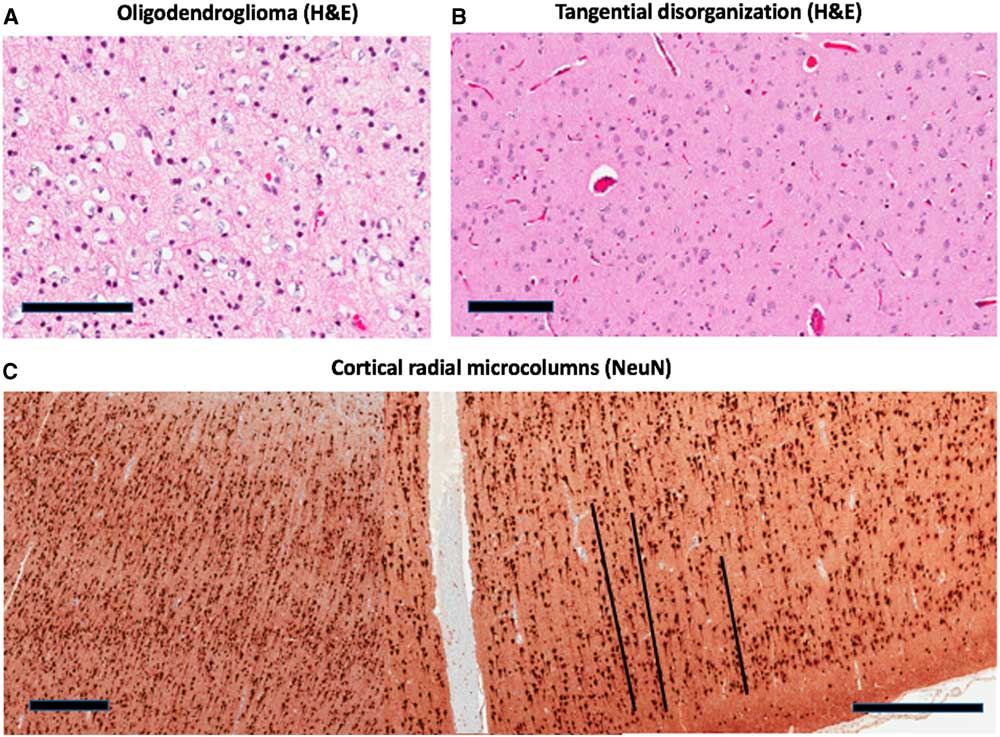
Figure 2 Pathologic features of the case. (A) shows the oligodendroglioma with perinuclear halos (H&E image). (B, H&E; C, NeuN) show focal cortical dysplasia in adjacent right frontal cortex. This consists of tangential (B) and radial (C) disorganization of neurons. Black lines are included in (C) next to each of three microcolumns. Scale bar=100 µm (A,B) or 500 µm (C). H&E=haematoxylin and eosin; NeuN=Neuronal Nuclei.
An ILAE consensus classification system for FCDs was published in 2011,Reference Blümcke, Thom and Aronica 3 revising the widely accepted histopathologic classification scheme published by Palmini et al.Reference Palmini, Najm and Avanzini 7 The latter recognized FCDs to be comprised of intracortical laminar and columnar disorganization (dyslamination) with associated neuronal-glial element variation. This system classified Type I FCD as cortical dyslamination, Type II as concomitant dyslamination and either dysmorphic neurons (IIA) or balloon cells (IIB).Reference Palmini 2 , Reference Palmini, Najm and Avanzini 7 The ILAE classification system features an FCD Type III category, including cases of FCD associated with other epileptogenic lesions: hippocampal sclerosis (Type IIIa), tumours (IIIb), vascular malformations (IIIc), and gliotic scars (IIId). Focal cortical dysplasia Type III cortical lamination abnormalities usually affect the same lobe as the principal lesion and are most common in the frontal and temporal lobes.Reference Blümcke, Thom and Aronica 3 , Reference Santos, de Oliveira and Machado 4
As many as 25% of patients undergoing epilepsy surgery have an underlying epileptogenic neoplastic lesion, whereas ~50% of patients with brain tumours have seizures.Reference Blumcke, Aronica and Urbach 8 Chronic focal epilepsy associated with benign glioneuronal tumours mostly relates to GG and DNT.Reference Blumcke, Aronica and Urbach 8 Only 2.7% of epileptic patients with brain tumours are attributed to oligogendroglioma.Reference Blümcke 9 The primary clinical manifestation of FCD is epilepsy.Reference Blümcke, Thom and Aronica 3 Glioneuronal tumours may be surrounded by cortical disorganization in up to 80% of cases; such coexistence adds to their epileptogenicity, having only been described in the epileptic patient.Reference Cossu, Fuschillo and Bramerio 5 Although FCD is commonly associated with GG and DNT, the coexistence of FCD with oligodendroglioma has been reported in four previous cases.Reference Santos, de Oliveira and Machado 4 , Reference Cossu, Fuschillo and Bramerio 5
The histological characteristics of FCD Type IIIb include cortical dyslamination and hypoplasia without six-layered structure and/or hypertrophic neurons of the neocortex, occurring adjacent to tumours (e.g., GG or DNT).Reference Blümcke, Thom and Aronica 3 The mechanism(s) by which glioneuronal tumours and perilesional cortical tissue develop and contribute to epileptogenicity have not been clearly defined.Reference Blümcke, Thom and Aronica 3 The lack of seizure activity in this case may suggest that FCD is not inevitably associated with epilepsy, or point to a reduced risk of seizures when combined with oligodendroglioma, rather than other tumours, many of which also have neuronal components (e.g., GG and DNT).
In summary, FCD Type IIIb refers to cortical lamination abnormalities adjacent to a glial tumour. The ILAE consensus classification system for FCD is employed when assessing surgical specimens removed to treat epilepsy. There is a known association between FCD and tumours such as GG and DNT. Herein, we present a rare association with oligodendroglioma. This is the first reported case of FCD Type IIIb discovered in a seizure-free patient.
Disclosures
The authors do not have anything to disclose.
Statement of Authorship
GEP performed the surgical resection; histologic analysis was performed by ASE. MAM performed the literature review and was primary author of the manuscript. All authors edited the final manuscript.




