Introduction
Globally, healthcare workers are at the centre of the fight against the COVID-19 pandemic. In the initial phase of the pandemic, healthcare professionals received a lot of media attention and praise from the general public for their heroic work [Reference Cox1]. While many employees started working from home or were even barred from attending their workplace, employees in the healthcare sector were affected in a dual sense: not only were they required to continue working, they were also exposed to increased risks due to the nature of their jobs. This twofold burden has had a global economic and medical impact, while also increasing psychological strain on the affected workers [Reference Zacher and Rudolph2].
As the pandemic spread from country to country, studies investigated the well-being of healthcare professionals in many places, including China, Singapore, Japan, Italy, Saudi Arabia and Switzerland [Reference Krammer3]. The well-being of this target group is of high concern, as health systems depend on their workforces and a collapse would have severe consequences for the general public.
In this study, we set out to investigate whether healthcare professionals in Germany have been affected psychologically by the COVID-19 pandemic and, if so, what kind of work-related stress they have been facing in this new situation.
Evidence from other countries
As China was the first country to face high infection rates of COVID-19, the first studies exploring the well-being of healthcare staff were run in Wuhan and other regions of China from January 2020 onwards [Reference Du4–Reference Kang7]. A systematic review of 14 studies on the impact on healthcare workers in different regions of China and in Singapore demonstrated an extensive rise in experienced stress as well as depression and anxiety symptoms. Across all studies, between 2.2% and 14.5% of respondents exhibited severe anxiety and depression symptoms. Influencing factors included age, gender, occupation, specialisation, type of activities performed and proximity to COVID-19 patients [Reference Bohlken8]. Some of these findings are based on large samples. For instance, Lai et al. [Reference Lai9] assessed N = 1257 healthcare workers in several regions of China and found high levels of depression (50.4%), anxiety (44.6%), insomnia (34.0%) and distress (71.5%).
Increased mental health risks were also observed in Japan [Reference Makino10] and later on in Switzerland [Reference Krammer3]. Italian healthcare professionals showed symptoms of burnout 5 weeks after the local onset of the pandemic [Reference Barello, Palamenghi and Graffigna11]. In Saudi Arabia, healthcare professionals displayed a higher level of anxiety and worry compared to previous outbreaks of MERS-CoV in the country, despite the fact that no cases of COVID-19 had been registered at the time [Reference Temsah12]. Using structural equation modelling on a variety of data sources, Miller [Reference Miller13] demonstrated that frontline staff, who come into contact with either possible or confirmed cases of COVID-19, are exposed to even higher mental and emotional risks than other healthcare workers.
While the COVID-19 pandemic is unprecedented with regard to its prevalence, its rapid spread [Reference El-Hage14] and the type of protective measures applied at large scale, similar effects on healthcare staff have been observed in previous outbreaks of other infectious diseases. A systematic review of 44 studies on former epidemics and pandemics showed that symptoms of mental disorders were common in healthcare workers both during and after the outbreaks [Reference Preti15]. Symptoms of depression were reported by 27.5–50.7%, symptoms of insomnia by 34–36.1% and symptoms of severe anxiety by 45% of participants. Also, between 11% and 73.4% of participants reported post-traumatic stress symptoms. After 1–3 years, the level was still at 10–40%.
Stress factors
Which individual and work-related factors are believed to increase or decrease the risk of developing clinical symptoms? Many healthcare professionals worry about infecting family members, experience fears and uncertainty concerning the mortality and morbidity of the disease, and some must face the death of colleagues [Reference El-Hage14, Reference Hall16, Reference Shanafelt, Ripp and Trockel17]. Surprisingly, the fear of becoming infected oneself seems to be less prominent than the fear of infecting one's family [Reference Chen18]. Intolerance of uncertainty has a strong impact on mental well-being in a pandemic setting. This is significantly mediated by rumination and fear [Reference Satici19].
Key individual protective factors include social support and self-efficacy. Social support increases self-efficacy and sleep quality, which in turn reduces anxiety and stress [Reference Xiao20]. It has been widely demonstrated that self-efficacy beliefs are an important moderator of the impact of work-related stressors [e.g. Reference Jex and Bliese21]. Self-efficacy is also one of the key concepts of the Health Belief Model [Reference Champion, Skinner, Glanz, Rimer and Viswanath22] and a good predictor of health behaviour. Self-efficacy can reduce infection-related worries [Reference Ho23] and insomnia [Reference Xiao20]. However, pandemic conditions are characterised by high levels of uncertainty and rapid changes in both work practices and social life. A general climate of wariness and uncertainty has been observed, as the emergence of mutations sporadically sets back knowledge gained about the disease and vaccination progress is slow. The treatment healthcare professionals can actually provide is still limited, as specific medications are not available yet. Healthcare workers have also raised concerns about not being able to provide competent care [Reference El-Hage14, Reference Kang7, Reference Shanafelt, Ripp and Trockel17]. This kind of situation is detrimental to self-efficacy.
Work-related organisational factors that increase the risk of developing clinical symptoms among healthcare professionals include depletion of personal protective equipment [Reference Hall16], lack of other medical resources such as specific drugs, ventilators and intensive care unit beds, as well as communication issues resulting from rapidly changing information or a lack of up-to-date information [Reference El-Hage14]. Changes in work practices such as having to adjust to wearing personal protective equipment and redeployment are also key concerns [Reference Miotto24]. Frontline staff working with (possibly) infected patients have been shown to be more affected by changes in work practices and stress than healthcare professionals who work with non-COVID-19 patients [Reference Preti15, Reference Miller13]. For detailed information on protective factors for healthcare professionals during epidemics and pandemics, see Preti et al. [Reference Preti15].
Mental health support for healthcare professionals
Various intervention strategies to improve the mental health of healthcare professionals during the COVID-19 pandemic have been proposed. For instance, healthcare providers may establish an emotional support plan, including strategies for information and screening, providing emotional support and building support networks [Reference Miotto24]. Regular interaction among teams can help workers discuss critical situations and check in on each other's well-being [Reference Greenberg25]. Healthcare workers and their team leaders can also learn to apply and support self-care strategies through e-learning programmes [Reference Blake26]. Several countries have established telephone hotlines to provide immediate crisis support [Reference Feinstein27–Reference Reiter and Duden29].
However, despite the severe impact of the pandemic on healthcare professionals, some staff members have proven reluctant to accept mental health support. According to Chen et al. [Reference Chen18], professionals tend to claim that they do not have any problems and just need some uninterrupted rest.
Evidence from the German health sector
In Germany, the pandemic took a somewhat different course than in many other countries. A strategy of early and extensive testing [Reference Cohen and Kupferschmidt30] resulted in less drastic lockdown measures than in other European countries [Reference Torri31] and avoided an overload of the health system.
Nevertheless, research shows that the pandemic and the lockdown measures affected the mental health of the German population as well. For instance, Bäuerle et al. [Reference Bäuerle32] found a significant increase in distress, anxiety and depression symptoms and a decrease in health status since the onset of the COVID-19 outbreak in a cross-sectional study with more than 15,000 participants. These mental health effects were predicted by pandemic-related fear, while trust in the government's actions and subjective level of information predicted a weaker increase in mental strain. Higher levels of psychosocial distress, depressive symptoms and anxiety were also found in a large cross-sectional survey (N = 3545) focusing on the lockdown in Germany between 1 and 15 April [Reference Jung, Kneer and Krüger33]. Furthermore, the survey revealed higher levels of irritability and a decrease in sense of coherence, sexual contentment, overall well-being and sleep quality.
In a longitudinal study with four time points and 979 participants, Zacher and Rudolph [Reference Zacher and Rudolph2] showed that while there were no significant changes in positive and negative affect and life satisfaction between December 2019 and March 2020, there was a significant decrease in these constructs between March and May 2020. In this latter timespan, individual differences in life satisfaction were positively correlated with positive reframing, active coping and controllability appraisals and negatively correlated with centrality appraisals, planning and threat. Negative affect was positively related to denial, substance use, centrality appraisals, threat and self-blame, and negatively related to emotional support and controllability appraisals.
In contrast to most previous studies in Germany, our study aimed to focus on healthcare professionals and the impacts of the COVID-19 pandemic on their mental health. To our knowledge, only two studies so far have looked at the mental health of healthcare professionals in Germany during the pandemic: Zerbini et al. [Reference Zerbini34] investigated the psychosocial burden of healthcare professionals in a hospital in Augsburg during the COVID-19 pandemic. In this study, nurses in COVID-19 hospital units reported more stress, depressive mood and exhaustion and less work-related fulfilment than nurses in regular units. Scores for physicians, on the other hand, were similar across the different units. Uncertainty about the future and job strain were reported as the most common reasons for psychosocial burden. Resources for coping that were mentioned were psychosocial support, leisure time as well as improved structural adjustments to the pandemic in the hospital such as keeping work schedules stable.
Surprisingly, Skoda et al. [Reference Skoda35] found in a cross-sectional study conducted in March 2020 at the beginning of the lockdown period in Germany that N = 2224 healthcare professionals, including physicians, nursing staff and paramedics, showed significantly lower levels of depression, COVID-19-related fears, generalised anxiety and higher health status than their sample of non-healthcare professionals. Similarly to Zerbini et al. [Reference Zerbini34], they found that nurses were the most psychologically strained among the healthcare professionals. An explanation for the lower levels of generalised anxiety in healthcare professionals more generally could relate to the fact that subjective level of information correlated negatively with generalised anxiety levels and was higher among healthcare professionals than non-healthcare professionals.
Similarly to these two studies, our study aimed to determine the mental health effects of the COVID-19 pandemic on healthcare professionals. In contrast to Zerbini et al. [Reference Zerbini34], who focused on a single hospital, we aimed to investigate the mental health of healthcare professionals across professions and German states. We also extended the findings of the two prior studies by investigating the underlying reasons for healthcare professionals' psychological distress and the factors that shaped their help-seeking behaviour.
Method
We created a cross-sectional online survey to assess healthcare professionals' mental well-being and the perceived stress factors they are experiencing.
Instrument
The first section of the survey explored participants' demographics such as age, gender and occupation.
For the second section, a list of potential stress factors was compiled based on literature as well as informal discussions with nurses and healthcare administrative staff. Participants were asked how strongly they were affected by each stress factor on a five-point Likert scale from not at all to extremely. Participants could also indicate if the factor does not apply to their situation.
Psychological well-being was measured with the self-report questionnaire ICD-10 Symptom Rating (ISR) [Reference Tritt36]. The ISR was originally developed based on the well-known ICD-10 [37] to assess the symptoms of psychological disorders in German-speaking countries, and includes subscales for depression, anxiety, eating disorders, obsessive-compulsive disorder and somatoform disorder symptoms as well as an extra-subscale with various additional symptoms. It comprises a total of 29 items, which are rated on a five-point Likert scale from 0 (does not apply) to 4 (extremely). Item ratings are averaged to compute subscale scores (three to four items for each disorder and 12 items for the extra subscale) as well as a total score. ISR total scores have been shown to have very good internal consistency (Cronbach's α = .92). The internal consistency of the subscales is also good (Cronbach's α = .78–.86) [Reference Fischer38]. High retest reliability for the individual scales ranging from .70 to .94 has been reported in different clinical and non-clinical samples [Reference Fischer39]. The scale exhibits a good ability to differentiate clinical groups (N = 12 265, M = 1.22, s.d. = 0.65) from non-clinical control groups (N = 2512, M = 0.40, s.d. = 0.45), with 84–88% sensitivity and 71–75% specificity [Reference Tritt40]. It also highly correlates with similar but longer instruments such as the symptom checklist SCL-90-R [Reference Schmitz41].
We chose the ISR because large clinical (C+) and non-clinical (C−) norm samples are available for Germany. These were assessed before the pandemic (P−) [Reference Tritt36, Reference Tritt42] and are referred to as reference groups RC +P− and RC−P− in our study. We also included a large sample of the general public (C−) assessed at the peak of the first wave of the pandemic (P+) in Germany [Reference Schelhorn43]Footnote 1 which we will refer to as reference group RC−P + (see Table 1).
Table 1. IDs and sample sizes of ISR reference groups context

In the third and final section of the survey, we explored whether participants would consider using different types of mental support and which barriers to seeking help for psychological strain they had experienced.
Sample
Participants were recruited through healthcare providers, a press release and personal contacts between 22 May and 22 July 2020Footnote 2. At that time, the most severe lockdown measures to date had been lifted again across Germany, i.e. shops and restaurants were allowed to resume operation and schools were slowly re-opening, but social distancing and other restrictions were still in place. No incentives were given for participation and no personally identifiable information was collected. Neither IP addresses nor GPS data were stored. All participants gave their informed consent for participation and for their responses to be stored electronically. We obtained institutional review board (IRB) approval from the PFH Private University of Applied Sciences Göttingen for this procedure.
A total of 300 participants completed the survey. One case was removed previously as it was identified as a test answer. No outliers were detected. The majority of participants were female (81%). Participants' age ranged between 17 and 65 years old (M = 40.65, s.d. = 12.9). The majority lived in Lower Saxony (59%), North Rhine-Westphalia (9%) and Hesse (9%). Most participants worked in inpatient nursing care (35.7%). Table 2 provides an overview of the distribution of occupations among participants.
Table 2. Distribution of participants' professions by gender

f, female; m, male; N, total; rel, relative percentage.
N = 4 participants did not indicate their gender.
Using the statistics software R (Version 4.0.2) [44] in RStudio [45] and numerous helper packages, we computed basic descriptive statistics, followed by t-tests and χ 2-tests where group comparisons were warranted. The importance of stress factors was estimated via (multiple) linear regressions after checking for the test prerequisites. Odds ratios for help-seeking were estimated using binary logistic regression. Our anonymised dataset and codebook are available for download via the Open Science Framework (OSF) website at: https://doi.org/10.17605/OSF.IO/EHM67 [Reference Weibelzahl, Duden and Reiter46]
Results
Stress factors
Participants reported that they were most affected by protective measures to avoid spreading the virus, as these impede both patient contact and work processes in general. The pandemic also led to various changes in work procedures. Table 3 provides an overview of the stress factors mentioned.
Table 3. How strongly are you affected by the following aspect during the COVID-19 pandemic at your workplace? (0 = not at all; 4 = extremely)

N, total; M, mean; s.d., std. deviation.
a This item was presented conditional on the response to a previous question about having children; number of children not assessed.
Mental health
When analysing the ISR scores, we first checked their internal consistency. The results were almost identical to previous findings, with Cronbach's α ranging between α = .78 and α = .9 for the subscales and α = .94 for the total scale.
The observed severity of clinical symptoms was high on all five scales (see Table 4 and Fig. 1). In particular, the frequency of depression and anxiety symptoms was unexpectedly high, with 9% reporting severe depression symptoms and another 65% light to medium symptoms. A total of 41% reported at least light symptoms of anxiety, while in reference group RC−P−, assessed before the pandemic, only 21% displayed these levels of symptoms. We split the sample by gender (see Table 5) and by age group (see Table 6), but did not find any systematic differences between the subgroups for any of the scales (gender by severity: χ 2(4, N = 296) ≤ 6.89, p > .05; age by severity: χ 2(12, N = 300) ≤ 19, p > .05).
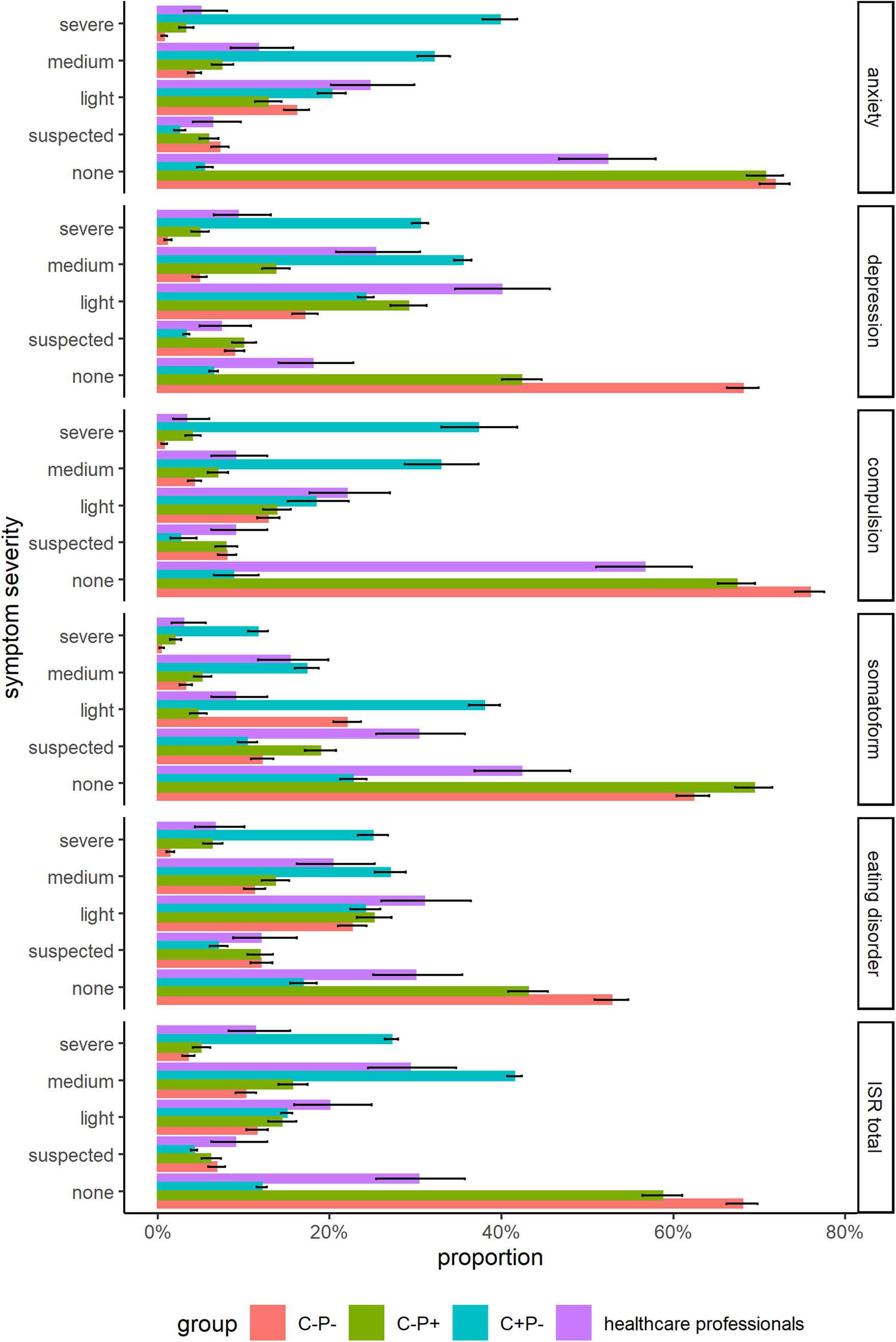
Fig. 1. Comparison of the relative frequency of severity levels for the ISR scales. Error bars indicate 95% confidence interval of the respective proportion.
Table 4. Severity of symptoms in ISR compared to the three reference groups
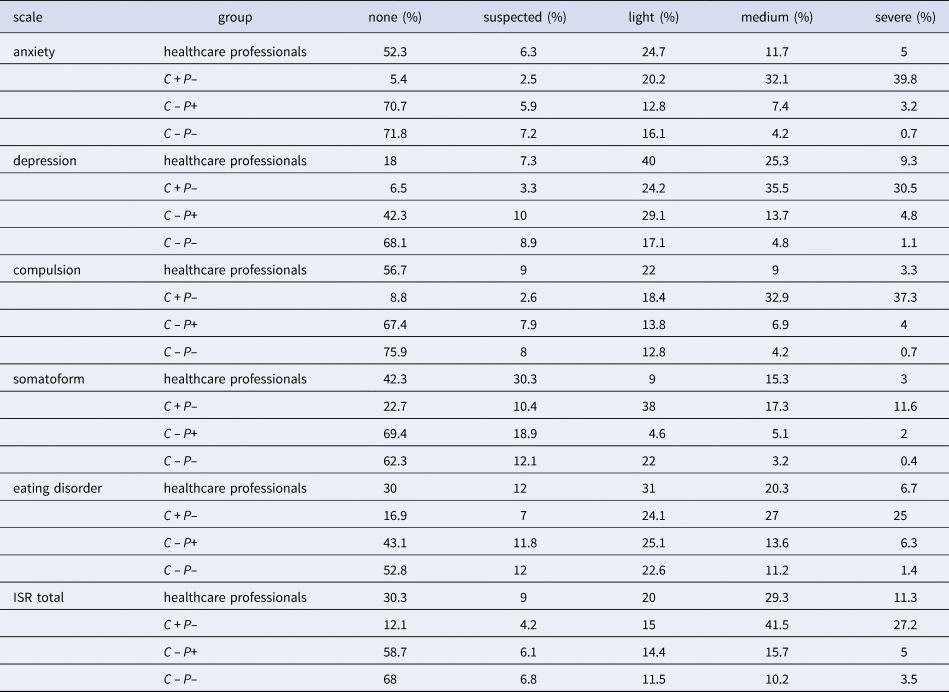
Table 5. Severity of symptoms in ISR split by gender (4 participants did not indicate their gender)

Table 6. Severity of symptoms in ISR split by age

For all symptom scales, healthcare professionals scored significantly higher than the reference group RC−P− before the pandemic (df ≥ 331.53, t ≥ 5.36, p < .001), but lower than the clinical group RC +P− (df ≥ 314.92, t ≤ −9.08, p < .001). However, the increase cannot be explained by the lockdown measures alone. Healthcare professionals also showed significantly more symptoms than the general population reference group during the pandemic (RC−P +) on both the depression scale (ΔM = 0.5, 95% CI [0.39, 0.61], t(2072) = 8.88, p < .001) and the anxiety scale (ΔM = 0.35, 95% CI [0.23, 0.47], t(383) = 5.83, p < .001). Most notably, the rate of severe symptoms was significantly higher on both the depression scale (χ 2(1, N = 1960) = 1022.99, p < .001) and the anxiety scale (χ 2(1, N = 2002) = 1024.29, p < .001).
Which stress factors contributed to anxiety and depression? A multiple regression of ISR depression scores on the eight stress factors (R 2 = 0.211, F(8, 284) = 9.47, p < .001) revealed that job insecurity was the single most important predictor of depression symptoms (see Table 7). While on average, participants felt that job insecurity hardly affected them (M = 1.15, s.d. = 1.24 on a scale from 0 to 4), high levels of job insecurity were strongly associated with psychological symptoms. Anxiety about infection of family members and protective measures that hinder work processes were also good predictors of the level of depression symptoms. A second regression for ISR anxiety scores (R 2 = 0.16, F(8, 284) = 6.75, p < .001) revealed a similar picture. Again, job insecurity and infection of family members were associated with anxiety symptoms. An increasing number of serious illnesses and deaths also contributed to anxiety (see Table 8).
Table 7. Multiple regression of ISR depression scores on stress factors

Note. b, unstandardised regression coefficient; CI, confidence interval; ∗p < .05, ∗∗p < .01, ∗∗∗p < .001, R 2 = 0.211, adjusted R 2 = 0.188, F(8, 284) = 9.47, p < .001.
Table 8. Multiple regression of ISR anxiety scores on stress factors

Note. b, unstandardised regression coefficient; CI, confidence interval; ∗p < .05, ∗∗p < .01, ∗∗∗p < .001, R 2 = 0.16, adjusted R 2 = 0.136, F(8, 284) = 6.75, p < .001.
Professionals with direct patient contact (M = 0.86) did not report more severe symptoms than those in administration (categorised based on profession, M = 1.03, t(50.1) = 1.36, p = .91, 1 − β(d = 0.5) = .91). However, as people with pre-existing medical conditions are at higher risk during the pandemic, those with a pre-existing condition were significantly more worried (M yes = 1.13, M no = 0.75, t(253.5) = 3.36, p < .001) and reported more severe symptoms overall (M yes = 1.04, M no = 0.76, t(260.2) = 3.88, p < .001).
Help-seeking
Overall, the majority of participants described themselves as experiencing symptoms of depression and anxiety. However, when asked whether they would like to receive psychological support to deal with the crisis, most participants declined (see Table 9). Out of the 300 participants, 209 (70%) scored 0.5 or higher on the ISR total scale which is considered a suspected clinical diagnosis or more. However, only 84 (40%) of these participants said that they would consider seeking psychological support. A binary logistic regression revealed that participants with higher ISR scores were more likely to seek help (b = 1.61, OR = 5.01, z = 6.54, p < .001).
Table 9. Frequency of responses to ‘Would you like to receive psychological support to deal with the crisis?’ categorised by supposed need for support based on ISR scale

‘not in need’ means ISR < 0.5; ‘in need’ means ISR ≥ 0.5
Why are healthcare professionals who supposedly need help not seeking help? One hundred (48%) of the 209 participants who were supposedly in need claimed that others needed the support more urgently. Seventy (33%) were not aware of suitable support services or offerings. Sixty-six (32%) felt that they were not distressed enough to require support. Fifty-two (25%) claimed that they did not have time to seek help. The majority–82% of all participants and 79% of those who supposedly needed help–indicated that they had sufficient social support outside the workplace.
Discussion
Consistent with reports from other countries and with our expectations, healthcare professionals in Germany reported high levels of depression and anxiety during the pandemic. Severe levels of depression symptoms were reported by 9.3% and severe symptoms of anxiety by 5% of participants. These values were similar to those reported in another German sample [Reference Zerbini34] assessed 2 months earlier under more severe lockdown conditions. Moreover, comparisons show that mental stress levels of healthcare staff were consistently above those reported by a general population sample during the pandemic and below a clinical sample prior to the pandemic; nevertheless, reported help-seeking intentions were low.
Naturally, these findings are subject to certain limitations. First, our data are cross-sectional, which limits the extent to which causal claims are possible. While it is possible for us to report to what extent participants themselves think pandemic-related work-specific stressors caused deteriorations in their mental health, a true test of causality over time, both for work-related stressors and help-seeking behaviour, would require longitudinal data. Second, our data may be biased by self-selection. While the online survey was widely accessible and the survey was fairly short, thus lowering the cognitive load required to complete it, it is conceivable that the healthcare workers suffering the most did not participate because they could not muster the time or mental energy. This would imply an underestimation of actual psychological strain among healthcare staff. Finally, our findings are limited by the timing of the survey. The questionnaire was circulated after the first wave of the pandemic and after the end of the first lockdown measures, during early summer. At this point in time, a second wave was expected, but still in the distant future, and the first wave had largely died down. This, too, may bias the data towards under-representing the true strain healthcare staff were exposed to at the peak of the crisis. In countries that are currently experiencing a second wave, it has consistently hit harder than the first wave, with more hospitalisations and higher death counts. Therefore, current data should continue to be collected to examine the mental burden among healthcare professionals today and how the ongoing strain is affecting them.
The reported severity of symptoms is in line with previous studies on the mental health effects of the COVID-19 pandemic on healthcare staff from other countries [e.g. Reference Kang7, Reference Liu6], which, according to a review, place the prevalence of severe symptoms between 2.2% and 14.5% [Reference Bohlken8]. German healthcare workers' level of strain is even more elevated than that of the general population during the pandemic assessed a few weeks before our sample. This is particularly concerning. As the pandemic reached its first peak across the globe, even countries that had been under-funding and neglecting their healthcare systems were made aware of the crucial importance of healthcare workers.
Politicians and members of the general public expressed their appreciation for absolutely essential workers–with frontline medical staff representing a key group. In light of this, it seems crucial to take measures to reduce psychological strain among these workers–particularly because both the pandemic and the consequences of the psychological distress caused by it are expected to persist for the foreseeable future. To demonstrate the consequences by example: depression and fatigue are correlated with major medical errors. In a study with doctors in training, the odds ratio associated with a positive depression screening was OR = 2.22, i.e., those screened positively were twice as likely to report a major medical error [Reference West47].
However, in spite of the severity of reported psychological strain, reported help-seeking behaviour and help-seeking intentions were consistently low. Many healthcare professionals are not seeking help, citing either concerns about the distribution of resources (i.e. based on the assumption that a limited amount of psychological support is available, they stated that others needed it more than they did, they themselves were not distressed enough to require support, and/or they already had a sufficient support network) or accessibility issues (not having the time to seek help, not being aware of a service that meets their needs).
This points to two underlying issues: First, while numerous employers, public agencies and non-profit organisations hurried to create mental health services to support healthcare staff during the pandemic, e.g. telephone hotlines like Talk2Us [Reference Reiter and Duden29] and free-of-charge psychotherapy provided to nursing staff by the German professional association for nursing staff [48], it seems that these were not accessible enough overall or did not meet healthcare staff's perceived needs. One issue was most likely awareness; since most of these support services were set up at the beginning of the pandemic and had thus only been active for a few months at the time we conducted our survey, they were not yet well-known and established among healthcare workers. This would explain why about one-third of our sample claimed to not be aware of a suitable service. Just over a quarter of participants stated they did not have time to seek help, which might indicate that current support offerings do not fit with demand. Future research should investigate how support services need to be designed to meet healthcare staff's needs, e.g. by being flexible to suit staff's schedules, being less time-consuming than current services are perceived to be, and being more easily accessible.
Second, the large portions of our sample claiming that they were not in need of support despite severely elevated levels of mental strain, that they already had sufficient support and that others needed it more urgently seem to be indicative of a climate that discourages help-seeking behaviour and speaking out about mental health issues in the healthcare community. A work culture pervaded by a general expectation to prioritise patient care before personal well-being and to refrain from acts that could be interpreted as displaying weakness, such as admitting to being overwhelmed or seeking professional help [Reference Galbraith, Brown and Clifton49], could be a crucial factor inhibiting help-seeking behaviour.
It is crucial that future research also investigates the work climate and culture in the healthcare sector and the norms they set around mental health; exploratory qualitative studies seem warranted. While social norms of this kind are complex and slow to change, it is crucial they be identified and addressed, because if help-seeking behaviour truly is widely stigmatised in the healthcare community, improving the accessibility of support services alone is bound to have very limited effects on the rates of healthcare workers seeking help. What our data, alongside various other studies, have done is establish that there is a need to provide mental health support to the healthcare community; the question that research must target next is why and when this need does and does not translate into uptake of support.
Data availability statement
Our anonymised dataset and codebook are available for download via the Open Science Framework (OSF) website at: https://doi.org/10.17605/OSF.IO/EHM67












