SARS-CoV-2 infection and long COVID
The COVID-19 pandemic, caused by SARS-CoV-2, has had major consequences for health and well-being globally. The effects of SARS-CoV-2 infection vary widely between individuals, from being asymptomatic to multi-organ failure and death. For many people, symptoms persist far beyond the acute phase of the disease.1–Reference Davis, Assaf, McCorkell, Wei, Low and Re'em3 Various names have been given to this condition, including ongoing symptomatic COVID-19, post-acute COVID-19 syndrome, ‘long-haulers’ and ‘long COVID’.1,4 Here we use the term long COVID, as it has become popular among many people with the condition and is widely used in the medical literature;1 however, we appreciate that discussions continue.1,4,Reference Gorna, MacDermott, Rayner, O'Hara, Evans and Agyen5
Long COVID prevalence estimates are inconsistent because of the rapidly evolving research base, non-standardised diagnostic criteria and different populations studied.Reference Meagher6 Current research suggests that approximately 10% of people in the UK will have ongoing symptoms 12 weeks after initial infection, and substantial numbers have symptoms lasting over 6 months.1,Reference Davis, Assaf, McCorkell, Wei, Low and Re'em3 There is a growing burden of ill health from long COVID in the UK, alongside patient reports that their needs are not currently being met by existing health services.Reference Routen, O'Mahoney, Ayoubkhani, Banerjee, Brightling and Calvert7 Long COVID symptoms can be variable and wide-ranging, relating to multiple organ systems, including respiratory, cardiovascular, neurological, psychological/psychiatric, gastrointestinal, musculoskeletal and dermatological; or they can be general and non-specific.Reference Shah, Hillman, Playford and Hishmeh8 Symptoms are likely to result from multiple potentially overlapping disease mechanisms.1,Reference Nalbandian, Sehgal, Gupta, Madhavan, McGroder and Stevens9 The most commonly reported symptoms include fatigue, breathlessness, cardiovascular abnormalities, decreased cognitive function, difficulties sleeping and abnormalities in taste and smell.Reference Crook, Raza, Nowell, Young and Edison10 Comparisons have been made between long COVID and other conditions, including post-intensive care syndrome, myalgic encephalomyelitis/chronic fatigue syndrome and the sequalae of infection with coronaviruses like SARS and MERS, which can cause protracted multisystem disease.1,Reference Ahmed, Patel, Greenwood, Halpin, Lewthwaite and Salawu11 However, although certain shared features exist, caution should be applied when drawing parallels with symptoms experienced in other conditions, as doing so may detract from appropriate investigation and management.Reference Gorna, MacDermott, Rayner, O'Hara, Evans and Agyen5
An evolving research base has sought to understand the types of services and support available to people experiencing long COVID, whereas UK clinical guidelines recommend supported self-management and a multidisciplinary approach to rehabilitation following investigative tests, as well as active monitoring and follow-up.12 However, reports suggest multiple difficulties accessing appropriate care, including uncertainty about treatment options and a lack of coordinated care.Reference Kingstone, Taylor, O'Donnell, Atherton, Blane and Chew-Graham13,Reference Ladds, Rushforth, Wieringa, Taylor, Rayner and Husain14 These experiences have resulted in patients resorting to self-management of symptoms through trial and error and via information and advice taken from informal peer support networks.Reference Mahase15
Mental health and wellbeing
Well-being can be defined as functioning well at both a personal and social level.Reference Michaelson, Mahony and Jonathan16 The PERMA (Positive emotion, Engagement, Relationships, Meaning and Accomplishment) theory of well-being represents five elements required for individuals to flourish, including positive emotion, engagement in tasks and activities, connections with others, having meaning and purpose, and a sense of achievement.Reference Seligman17 Adapting to living with a chronic illness has the potential to profoundly affect multiple components of well-being as described by the PERMA theory. For example, reduced function can lead to difficulties engaging in daily activities, a reduced sense of purpose and achievement, and increased social isolation, which influences mental health;Reference Hwu18 having a long-term physical health condition is associated with a twofold increased risk of depression or anxiety compared with the general population.Reference Read, Sharpe, Modini and Dear19 Social identity theory also posits that having meaning and purpose in the roles that individuals play within society is crucial for health and well-being, and that any disruption in ability to fulfil these roles, for example as a result of chronic illness, can negatively affect mental health.Reference Jetten, Haslam, Cruwys, Greenaway, Haslam and Steffens20
Effects on mental health and well-being are commonly reported by people with long COVID, in particular features of anxiety, depression and post-traumatic stress disorder,Reference Shah, Hillman, Playford and Hishmeh8,Reference Nalbandian, Sehgal, Gupta, Madhavan, McGroder and Stevens9,Reference Naidu, Shah, Saigal, Smith, Brill and Goldring21,Reference Buttery, Philip, Williams, Fallas, West and Cumella22 with cognitive processing disorders (or ‘brain fog’) also frequently reported.Reference Shah, Hillman, Playford and Hishmeh8,Reference Nalbandian, Sehgal, Gupta, Madhavan, McGroder and Stevens9 Mental health effects are likely multifactorial in origin, including the psychosocial context of the pandemic,Reference Fancourt, Steptoe and Bu23,Reference Troyer, Kohn and Hong24 pre-existing individual susceptibilitiesReference Fancourt, Steptoe and Bu23,Reference Llach and Vieta25 and physical biological processes related to SARS-CoV-2 infection.Reference Troyer, Kohn and Hong24,Reference Llach and Vieta25 Although mental health effects are widely reported, there is limited in-depth research exploring the perspectives of people with long COVID regarding factors shaping their mental health and well-being. Addressing this gap has been identified as a key priority by an international, multi-stakeholder forum,Reference Norton, Olliaro, Sigfrid, Carson, Paparella and Hastie26 to improve understanding, promote empathic healthcare interactions and facilitate development of patient-centred and appropriate healthcare provision for people with long COVID. Therefore, this study aimed to explore the perspectives of people with long COVID with regards to how their mental health and well-being has been affected.
Method
Sample and recruitment
We conducted semi-structured qualitative interviews with people who self-reported long COVID. Participants were recruited via an online long COVID support group, an advertisement in the University College London COVID Social Study27 newsletter and through social media. Seventy-four people responded to the invitation to take part, and from this participant pool, 53 people were purposively sampled to ensure that people of different ages, ethnicity and genders were represented in the study. All 53 potential participants were sent a study information sheet and a screening form to determine eligibility. Twenty-nine screening forms were returned, we received no further response from 23 people and one person declined further participation. Twenty-one people went on take part in the study.
To assess participant eligibility for the study, we used the post-acute COVID-19 criteria proposed by Greenhalgh et al, which was broadly representative of the consensus at the time.Reference Greenhalgh, Knight, A'Court, Buxton and Husain28 Eligibility criteria consisted of a positive swab test/antibody test or one or more commonly reported COVID-19 symptoms at illness onset (persistent cough, loss or change in taste/smell, high temperature); and experiencing one or more broader symptoms ≥3 weeks following the onset of their first symptomsReference Greenhalgh, Knight, A'Court, Buxton and Husain28 (Supplementary Appendix 1 available at https://doi.org/10.1192/bjo.2022.38). Eligible participants were encouraged to ask questions about the study before providing written informed consent to take part and completing a demographics form. All participants gave their written informed consent to participate in the study. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human patients were approved by the University College London Ethics Committee (project identifier 14895/005).
Data collection
All interviews followed a semi-structured topic guide and were audio recorded. Questions explored onset and initial impact of COVID-19 symptoms, ongoing impact and development of longer-term health problems, impact of long COVID on social lives and mental health, and worries about the future. Example topic guide questions are listed in Fig. 1 and the full topic guide is provided in Supplementary Appendix 2. Interviews were conducted by a female postdoctoral applied mental health services researcher (A.B.) via video (14 interviews) or telephone call (seven interviews), depending on participant preference. Interviews lasted on average 67 min (range 41–99 min), and participants received a £10 shopping voucher for their time. Data collection continued until no new concepts related to mental health and well-being were discussed by interviewees.Reference Braun and Clarke29

Fig. 1 Topic guide question examples.
Data analysis
Audio files were transcribed verbatim by an external transcription company. Personal and identifiable data were removed from transcripts to maintain confidentiality. Transcripts were then imported into NVivo 12 software for Windows (QSR International Pty Ltd, Doncaster, Australia; see https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/support-services/nvivo-downloads) and analysed using reflexive thematic analysis.Reference Braun, Clarke and Hayfield30 An initial coding framework was built based on concepts taken from the topic guide. Initial codes were organised and labelled under the following headings: impact of long COVID symptoms on normal life, social activities, health and well-being; ability to access services and support; and activities that protect mental health. Codes were applied to the text with line-by-line coding, and when new concepts were identified within the text, additional codes were added to the framework.. Three transcripts (14%) were independently double-coded by three researchers (A.B., H.A. (a male medical trainee and doctoral student in behavioural science and health) and K.E.J.P. (a male physician and clinical research fellow with training in qualitative research)) who met to discuss emerging codes and themes and generate the coding framework. H.A. then applied the coding framework to all remaining transcripts, adding new codes as transcripts became available and until no new codes were identified. Codes were then arranged into themes pertaining to the research questions. The research team met to finalise themes and approve the final report.
Results
We interviewed 21 participants between November 2020 and September 2021. All but one interview was conducted within a 4-month period (between November 2020 and March 2021). Participants were aged between 26 and 70 years (mean 47 years) and were predominantly female (67%) and White British (67%). All participants reported a case of suspected or confirmed COVID-19 between 28 February 2020 and 11 January 2021, and experienced on average 12 symptoms (range 4–18 symptoms) for 29 weeks (range 8–52 weeks) at the time of interview, with the most common symptoms being fatigue (95%), muscle pain/weakness (86%), shortness of breath (81%), difficulties concentrating (76%) and memory lapses (71%). A total of 52% of participants reported a confirmed positive swab test or had tested positive for antibodies. Four participants were hospitalised during the initial phase of their illness. All participants were still experiencing symptoms at the time of the interview. See Table 1 for participant characteristics and Table 2 for symptoms and self-reported laboratory confirmation of SARS-CoV-2 infection.
Table 1 Participant characteristics

a. Data are self-reported via a demographics form.
b. Hypothyroid, irritable bowel syndrome, arthritis, asthma, type 2 diabetes, heart failure, hypertension, vestibular migraine, gout, prostate problems, radicular pain and bile acid malabsorption.
c. Depression, depression and anxiety.
Table 2 COVID-19 status and symptoms
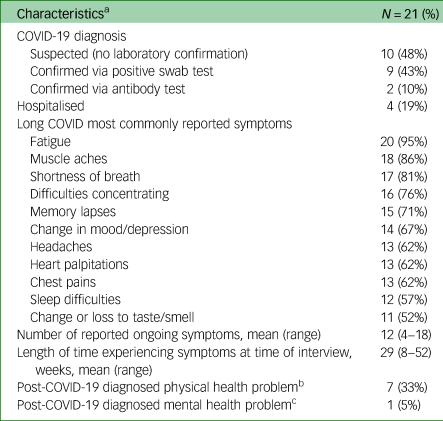
a. Data are self-reported via a demographics form.
b. Myocarditis, tachycardia, irritable bowel syndrome, blood clots, arthritis, dysbiosis, pre-diabetes and neuropathy.
c. Depression.
Themes
We identified five themes regarding factors shaping mental health and well-being for people living with long COVID: symptoms causing severe disruption to daily life, lack of service and treatment options, uncertainty of illness trajectories, care and understanding from others, and changes to identity. Fig. 2 demonstrates the relationships between themes.
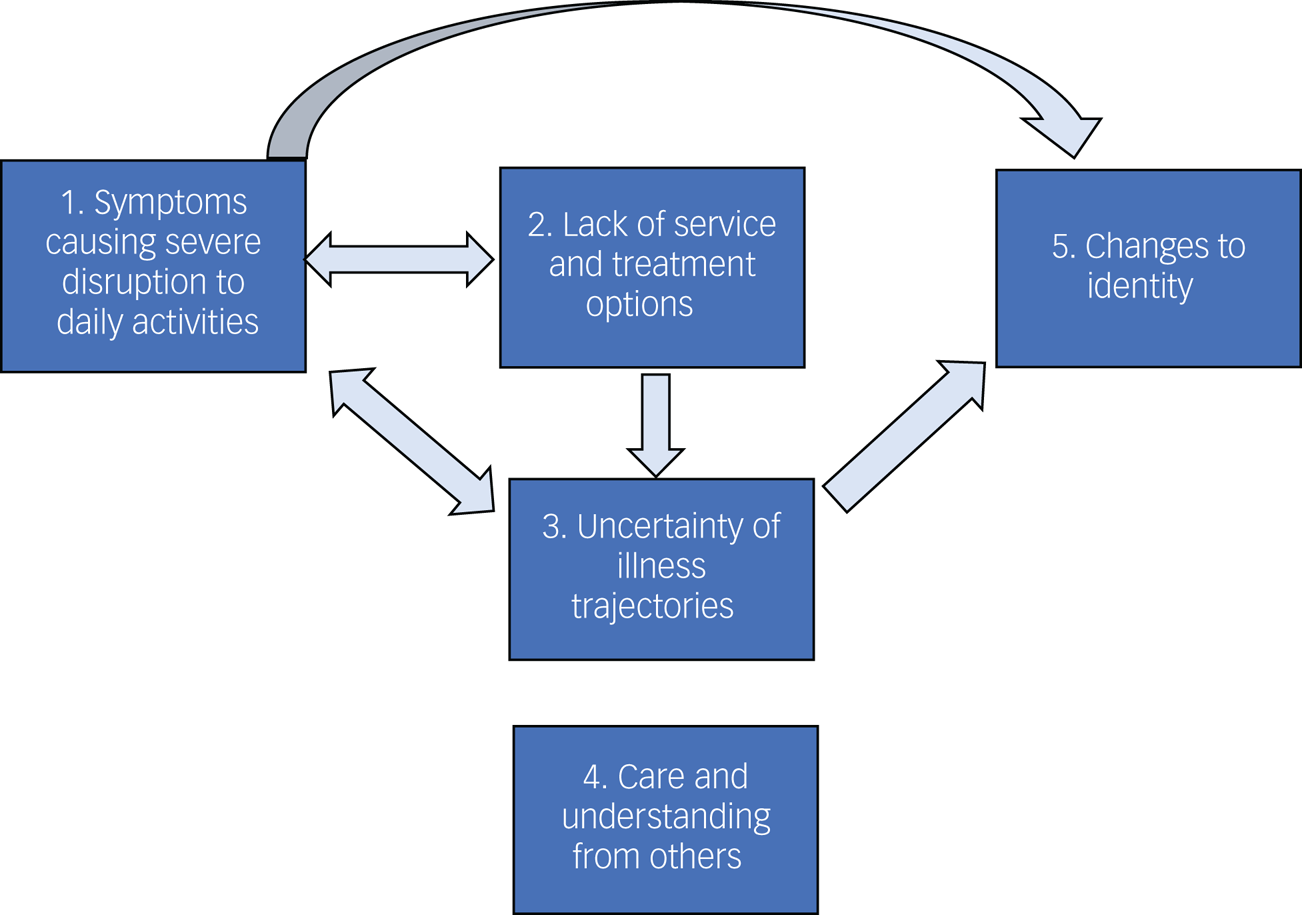
Fig. 2 Themes and interactions between themes regarding factors that affect mental health and well-being in people experiencing long COVID.
Long COVID symptoms led to severe disruption to daily life and activities (theme 1) and prevented participation in enjoyable activities that might normally protect participant well-being. This disruption was exacerbated by a lack of service and treatment options (theme 2) and by uncertainty of illness trajectories (theme 3). This, in turn, made managing uncertainties regarding trajectories, and pushing for service and treatment options even more challenging.
A lack of service and treatment options (theme 2) led to worries of exacerbation of symptoms and continued uncertainty around illness trajectories (theme 3); uncertainty of illness trajectories (theme 3) led to difficulties planning daily activities (theme 1), and subsequently affected ability to engage in enjoyable activities.
Positive experiences of care and understanding from others (theme 4) protected mental health, whereas a lack of care negatively affected well-being.
Ongoing long COVID symptoms that led to severe disruption to daily activities (theme 1) and uncertain illness trajectories (theme 3) led to changes to identity (theme 5), which negatively affected mental health because people were no longer able to fulfil their usual social roles.
Theme 1: symptoms causing severe disruption to daily life
Most participants described leading active lives before COVID-19 infection, working in full-time employment, participating in regular exercise and having busy social lives; however, ongoing symptoms had significantly curtailed activities of daily living.
Daily activities
Ongoing fatigue and ‘brain fog’ were commonly described as having a huge impact on people's working lives, with almost half of the sample not able to fully return to work: ‘I couldn't have even picked the laptop up and opened it, to be honest, you're completely just wiped out’. The impact on daily life for some participants was profound, resulting in difficulties ‘even being able to manage basic household chores’ or struggling to maintain personal care:
‘I haven't showered for 3 days. I have to think about showering, I have to sit down and spend like 2 hours thinking about will I be able to manage showering today? Because even taking a bath makes me tired’ (550_female_aged_25-29).
Some participants described experiencing a prolonged loss or change in taste and smell that resulted in no longer being able to enjoy food. For those who had previously used cooking as way to de-stress, this was experienced as particularly detrimental to well-being:
‘That's kind of disheartening … I could make a really nice meal which before lockdown would've been the kind of thing that I would a) like to do, but also for me personally, I see it as more of if you've had a bad day I'm going to do a nice thing for myself and invest in making a nice dinner for maybe me and someone else’ (565_male_aged_25-29).
Social life
Many participants were no longer able to participate in social activities, which had a profound impact on their mental health and well-being:
‘I want to be able to have laughter, I want to be able to go out and be the life and soul of the party, which I'm just not anymore, so I do grieve’ (557_female_aged_35-39).
For some, the severity of their ongoing symptoms meant they were unable to socialise, mainly because of fatigue and the need to conserve energy by pacing oneself: ‘I haven't got the energy to interact.’ For one participant, socialising became difficult because of breathlessness that made holding a conversation difficult:
‘I couldn't really talk to people … I just limited my [family member] to twice a week calls and I had to have short, 5-minute calls because more than that then I'd have difficulty breathing. So that was a bit frustrating that I couldn't actually talk to people’ (569_male_aged_55-59).
Participants also described withdrawing from their social lives because of ‘not wanting to worry people’ and feelings of ‘guilt because I feel like I'm pouring more pressure on [my family]’ by sharing their experiences with others. Others withdrew because they felt that they had little to contribute to friendships because they were unable to focus on anything other than their health: ‘I was reflecting and thinking maybe I was talking about it all the time’.
‘Well, early days, I'd get emails and stuff and then it's just drifted off. It's my own fault because I could phone up and chat to people, but I just feel it's a bit boring. How are you? You tell them how you are …. How's your heart? You tell them, so, I'd rather not dwell on it. And I've got nothing else to talk to them about now’ (564_female_aged_70-74).
Enjoyable activities
Participants described the importance of engaging in new hobbies and activities or adapting previous activities to give them respite from their health problems, to support their well-being and to create a sense of achievement. Just under half of participants described engaging in low-grade physical activity such as walking: ‘I'm just doing some very gentle, gentle stuff. I'm walking’. Playing or listening to music or podcasts were important for distraction and relaxation:
‘When my relapse started and into 3 weeks of it I think it was when I was in bed most of the time, I had these awful, awful feelings of almost … I felt like crying but I wouldn't, but I'd change my mindset to, oh I'll do something more positive than lying in bed. I had some pastels and I was doing a little bit of drawing, and I'd listen to the radio and put music on and stuff. I'd just alter it just by changing my mind from focusing on, oh I feel ill and will I ever work again, will I ever be able to do anything again, to oh well I'll do this’ (559_female_aged_45-49).
However, for many participants, participating in enjoyable activities that could improve or protect mental health was not possible, such as physical activity: ‘I can't do my exercises, and I can't keep my body fit’, getting out of the house: ‘I've been stuck at home for the whole year’, or engaging in arts and culture:
‘I've been trying to do some interesting things, so I watched a ballet online from the Royal Opera House, I went to a book launch of a book. I thought, I've never done that before, I'll do that online. All sorts of opportunities. But even the things that are joyful and enriching, and would normally be lovely and powerful, if I get really excited about it, it just makes me tired’ (563_female_aged_60-64).
Some participants described replacing their usual physical activities with competitive activities that could be undertaken at home, such as online gaming:
‘That (online game) has been an absolute lifesaver for me because it's kept my brain ticking over a bit, and given me, just a challenge, so I'm very fortunate with that. I'm sure other people have other things, but because I've got, naturally a competitive nature, with my golf, and I used to play tennis’ (564_female_aged_70-74).
Theme 2: access to services and treatments
Although just over half of participants had received investigative tests, many participants described a lack of follow-up: ‘we're now on week 15 and I've still not had any results’ and ongoing stress and worry that the treatments or services they needed to manage their symptoms were unavailable, inaccessible or indeed were available, but not being offered to them:
‘What's bothering me at the moment is I'm not in any plan or regime. So, I'm not on any pharmacological medicine. I'm not on any physical rehabilitation. So, I'm not on any programme. So, I just feel like I'm ambling. I'm just in the ether … A year of my life has gone. I can't carry on’ (553_female_aged_50-54).
Several participants described their frustration at being unable to access treatments or services because diagnostic tests were inconclusive or produced negative results despite ongoing symptoms:
‘I had several chest x-rays, and things, so I was looked after. But there was nothing wrong as far as they could see, but obviously, I was still having symptoms. But I was a bit frustrated. It was several months by then, and I was thinking why has nothing been set up yet for people who are suffering?’ (552_female_aged_50-54).
Although many participants described being aware of long COVID clinics, there was confusion around the referral process: ‘we'd been rejected because they've changed the criteria’, or there was a lack of available services in different areas of the UK:
‘There are no COVID clinics or anything in this area, so no. I have spoken to the doctors quite a lot since I've been ill, and they've been marvellous, but they're still, we don't know, we're still waiting for the clinic to open’ (561_female_aged_50-54).
Just under a third of participants who described being unable to access National Health Service (NHS) care had gone on to access private healthcare, either by paying for care themselves: ‘the only door that is half-open, is if I decide to pay and go privately’, or through insurance provided by their employer:
‘So, without that private healthcare, I don't think I would maybe have got over some of the symptoms that I had because, as I say, the GP [general practitioner] was just obviously it's new for them as well, but they just weren't offering any kind of help at all. And I remember when I went through them and says, well, I can't actually refer you to the specialists with what you're wanting under the NHS’. (564_female_aged_70-74).
Theme 3: uncertainty of illness trajectories
Most participants described feelings of anxiety around the uncertain symptom trajectories they were experiencing, with fluctuating periods of having ‘good days’ of feeling well and even, at times, ‘euphoric’ followed by ‘bad days’, periods of intense exhaustion and being unable to get out of bed. One participant described ‘the ebb and flow of it all’ as the most difficult thing to deal with:
‘There's a lot of relapses involved … which, initially, was very, very demoralising, because you think, or I would think, I've turned a corner, I'm going to get better, and then it would just suddenly get, like take two steps forward and three or four steps back. And that's characterised the entire journey I've had with COVID, up until now really’ (560_female_aged_50-54).
For others, uncertainty about the future and how long their symptoms might continue led to increased anxiety about employment, finances and family life. Participants described feeling less in control of their lives as time went on:
‘I can't live like this, how am I going to go on in the future, am I going to get worse, am I going to get better? Obviously, you think of everything. How are you going to look after your kids, the family, your work situation, how are you going to pay your bills’ (555_male_aged_45-49).
Participants also described having to weigh up the potential consequences of participating in activities that protected their well-being but that ultimately would lead to a relapse, against the immediate short-term benefits to their mental health:
‘I take the opportunities I can. So, a friend's been off work and she messaged me yesterday and said, weather's nice … do you fancy a walk in the park? And I said oh great, yes, lovely, I'm free from here and here. Technically, that was too much in a day, and I knew it was too much and I paid for it later in the evening and this morning, but it was so nice to see her’ (563_female_aged_60-64).
Theme 4: care and understanding from others
Having a supportive and understanding social network, including friends, family and health professionals, was described as important for participant well-being, particularly when faced with fluctuating symptoms and uncertainty (theme 3). When this support was not available, participants described negative effects on their well-being and feelings of anxiety and loneliness.
Health professionals
Participants frequently reported feelings of frustration or anxiety because of a lack of understanding and support from health professionals. Experiences that exacerbated poor mental health included feeling ‘ignored’, ‘abandoned’ or ‘being brushed aside’, feeling that health professionals were unwilling to help or listen, a lack of continuity of care, and instances of diagnostic overshadowing whereby symptoms of long COVID were attributed to the participant's mental health:
‘I have come across a few doctors where I've felt they've made me feel a bit stupid when I'm worrying about certain things … So yes, there's that worrying that people just think you're making it up. I think it's just that anxiety thing, for me that I don't want to be an anxious person. And I think if I sense that I'm talking to a doctor, or sometimes they've said it outright, you're an anxious person, and I think oh great they just think I'm anxious’ (558_female_aged_35-39).
Even when health professionals were unable to offer appropriate medical treatments or answers, it was still important for participants to feel heard and for their stories to be believed and thus validated:
‘In the early days, my GP was fantastic … I sent him a letter to tell him what was going on in my life, all my symptoms and everything. And I said, I am so sorry about harassing you. And he phoned me up, and he said, keep harassing me, he said, if you don't tell me, I don't know’ (564_female_aged_70-74).
Support from family and friends
Participants described the importance of receiving support and empathy from their social networks to protect their well-being during difficult times:
‘I've had a couple of other friends who said, look, don't sit alone at home being miserable. If you need anything, if you just need to talk to someone, just give me a bell, or message me or whatever. So, that's been nice, I think a lot of people didn't realise how ill I was, and I think that when I went back to work, they were quite shocked, and were keen to reach out’ (560_female_aged_50-54).
In the initial stages of illness, participants described receiving emotional and practical support from family and friends: ‘[My sibling] used to do the shopping, and she'd sometimes do the cooking and bring it over’. For some participants, however, as their illness progressed and symptoms remained, emotional support became less available because of a lack of understanding or unwillingness to acknowledge that participants could still be unwell:
‘A lot of people don't understand long COVID, so when you explain to them, I'm still not feeling right 6 months down the line, a lot of people have said, I think you're just worrying too much. That's what I think my parents come back with. They keep saying to me, you worry too much, there's nothing wrong with you’ (555_male_aged_45-49).
Although most participants had not felt stigmatised because of their long COVID, a small number of participants reported experiencing external stigma directed at them from others. This included examples of family members ‘avoiding us like the plague’ for almost a year after initial symptoms or people behaving differently toward participants once they disclosed that they still had not recovered:
I'd walk up to the shops, buy one thing from the chemist or something and walk back. And I'd meet someone I knew, and I'd say, I've had COVID, they would step back, and so I stopped doing it because I realised that for a lot of people, I was still contagious, and I understand that. And I think that's why I isolated, because it was quite difficult being around people that knew, who were not comfortable around me. And that's even after 3 or 4 months afterwards, and even now, if I mention to somebody that I had COVID in March, they step back, and it is quite a difficult thing to deal with’ (564_female_aged_70-74).
For one participant, feelings of stigma arose from the impact of long COVID on mental health and worries that she might be judged by others for not being able to cope:
‘I think the stigma that was I mean around being depressed and having any mental conditions. I think people kind of judging for that. I've seen people do that. Especially in my friends’ circle’ (550_female_aged_25-29).
Peer support
Many participants were members of online long COVID peer support groups and found them empathetic and supportive: ‘I was just feeling really validated that I'm not alone’. These groups also facilitated access to information and resources on management strategies and services:
‘And the best support I got was from all the Facebook groups, believe it or not. That's where I found a lot of information, because everyone else was on a similar timeline to me. So, we were all going through the same symptoms, so I knew I wasn't going crazy’ (552_female_aged_50-54).
Others reported mixed experiences of accessing online peer support groups, with some feeling overwhelmed: ‘I think that can be quite scary when you listen to some of that’, and others acknowledging that some of the information was unhelpful or untrustworthy:
‘I went on Facebook to go on one of those long COVID groups, which I looked at for a couple of days, but to be honest it started doing more harm than good looking at those, especially in the state I was in at the time’ (566_male_aged_40-44).
On balance, however, most participants found the groups helpful and actively filtered out the ‘rubbish’:
‘So, at least I feel like they're trying to do something. There's a lot on there, which is negative. I try not to read that because … But that's like any social media isn't it, you just have to choose’ (553_female_aged_50-54).
Theme 5: changes to identity
Participants described profound changes to their sense of self because of long COVID: ‘I'm a different person now’, and described feeling a loss of certain attributes and self-confidence that had previously defined who they were: ‘I think also it's stripped me of me’. For some, this change manifested itself as a loss of interest in self-care, a decrease in physical fitness: ‘I feel weaker’, and consequently changes to their physical appearance:
‘I don't care anymore that I'm getting a bit soft in my body, that I used to do eight daily exercises and stuff like that. I don't care that I'm looking older … and I suppose in some ways, that bothers me. Every now and then, I just think, this isn't you’ (564_female_aged_70-74).
‘I look like a big six-foot two bloke, but actually have jelly in my arms, just absolutely no energy in there, no physical strength at all. So yes, you feel less confident’ (566_male_aged_40-42).
Others described their identity as diminished because they were no longer able to fulfil their usual caring responsibilities and social roles as professionals, partners, parents and friends, resulting in a sense of loss and feeling ‘like a burden or waste of space’:
‘I do feel a little bit lost because I just don't know. I was a carer and now I'm being cared for. I've had to change, and I've struggled coming to terms with it a little bit’ (561_female_aged_50-54).
‘So yes, there's been a big change of identity. I'm a recovering patient from COVID rather than a meritorious consultant … ’ (568_male_aged_60-64).
Discussion
Our study found that people with long COVID experience unique challenges to their mental health and well-being related to the impact of the symptoms on their lives, as well as interactions with health services, family and friends. Limited care and understanding from others, a lack of service and treatment options, disruptions to daily life and activities brought about by symptoms, the uncertainty of illness trajectories and changes to identity all contributed to a deterioration in mental health. Participants often described barriers to engaging in activities that might protect their mental health; however, being listened to and feeling validated by health professionals, family and friends, accessing peer support and engaging in enjoyable activities within the limitations of their condition, were identified as important for psychological well-being. The relationships between the factors identified in our themes and poorer mental health and well-being are likely to be mutually reinforcing. As people experience worsening mental health and well-being, their ability to search out and fight for the limited services that exist is also likely to decrease. Similarly, the mental health and well-being symptoms experienced may compound other symptoms such as fatigue and breathlessness. As such, the bidirectional relationships between many of the drivers of poorer mental health, and worse mental health itself, have the potential to create detrimental cycles of reinforcement.
Our findings align with, and extend, existing research into experiences of long COVID. They echo work that has previously described symptoms, impact on daily life and interaction with healthcare providers.Reference Ladds, Rushforth, Wieringa, Taylor, Rayner and Husain14,Reference Buttery, Philip, Williams, Fallas, West and Cumella22,Reference Philip, Buttery, Williams, Vijayakumar, Tonkin and Cumella31 However, our work extends previous findings by highlighting which features of long COVID are seen as most significant in shaping mental health and well-being from the perspective of people with lived experience. Our findings also improve understanding of how these features are experienced by people with long COVID, and as such, present potentially useful considerations for healthcare, self-management and wider society.
In keeping with the growing body of research, our participants reported multiple, varied, relapsing-remitting symptoms often severely affecting their ability to engage in daily life, resulting in a reduced sense of achievement, meaning and purpose.Reference Ladds, Rushforth, Wieringa, Taylor, Rayner and Husain14,Reference Buttery, Philip, Williams, Fallas, West and Cumella22,Reference Philip, Buttery, Williams, Vijayakumar, Tonkin and Cumella31 The PERMA theory of well-being posits that engagement in tasks and activities is vital to maintaining positive well-being,Reference Seligman17 therefore these limitations have strong negative effects on mental health through limiting participation in enjoyable and meaningful aspects of life and those that gave individuals their sense of identity, including work, leisure and social activities. Social identity theory suggests that we derive meaning and purpose from the roles we play within communities and groups, and that this positively affects individual health and well-being;Reference Jetten, Haslam, Cruwys, Greenaway, Haslam and Steffens20 when participants in our study were no longer able to connect with their previous positive identities and these were replaced with illness-related identities, this posed a threat to well-being. Experiences of loss and threatened identity were also found in a qualitative study involving 114 people with long COVID,Reference Ladds, Rushforth, Wieringa, Taylor, Rayner and Husain14 and research regarding other chronic diseases such as chronic fatigue syndrome.Reference Asbring32 Relatedly, a small number of participants in our study described a lack of understanding from and feeling stigmatised by others as detrimental to well-being. Previous work on chronic illness has theorised that these experiences of illness related stigma may reduce well-being via a reconstruction of an individual's identity with both illness and stigma incorporated.Reference O'Donnell and Habenicht33
Our findings identified the relevance of relapsing-remitting disease trajectories as important drivers of negative mental states because of related uncertainty about the future, which is well-established as a driver of anxiety and depression for people with various chronic diseases.Reference DeJean, Giacomini, Vanstone and Brundisini34 Other research, particularly from earlier on in the pandemic, also identified various barriers to healthcare,1,Reference Ladds, Rushforth, Wieringa, Taylor, Rayner and Husain14,Reference Buttery, Philip, Williams, Fallas, West and Cumella22,Reference Philip, Buttery, Williams, Vijayakumar, Tonkin and Cumella31 including a lack of specialist service provision and limited understanding of the illness from healthcare professionals. Our study also shows that some people resorted to accessing private healthcare and therefore felt better supported to manage their symptoms. This finding raises concerns around health inequalities for people with long COVID who are unable to afford private healthcare. Potentially, with the creation of specialist long COVID services, increasing research and clinical guidelines, such barriers should become less of an issue over time, although given other competing needs faced by healthcare services, access could remain an issue. Feeling ignored or not believed by healthcare professionals, family members and friends has been commonly reported.1,Reference Ladds, Rushforth, Wieringa, Taylor, Rayner and Husain14,Reference Buttery, Philip, Williams, Fallas, West and Cumella22,Reference Philip, Buttery, Williams, Vijayakumar, Tonkin and Cumella31 These experiences are similar to those described by people with myalgic encephalomyelitis/chronic fatigue syndrome.Reference Asbring and Narvanen35 Our findings suggest such experiences have particularly powerful negative effects on mental health.
Factors positively affecting mental health and well-being were infrequently mentioned. As in previous work, we did find that interactions where people felt listened to and believed were greatly valued, and empathy from health professionals, even when faced with limited treatment and referral options,Reference Kingstone, Taylor, O'Donnell, Atherton, Blane and Chew-Graham13 was important. Additionally, long COVID peer support groups appear valued by some individuals, although the potential for overwhelming and inaccurate information, as reported by participants in our study, is an important consideration.
Strengths and limitations
Certain limitations should be discussed. First, our sample included people who met clinical diagnostic criteria but without laboratory confirmation of COVID-19. This is in keeping with relevant guidance and excluding people without laboratory confirmation would have limited our ability to capture experiences of long COVID symptoms lasting up to 12 months, as testing was limited in the first part of the pandemic. Second, a degree of selection bias may have occurred toward those with mental health and well-being effects, and people may have been more likely to share their experiences if they were experiencing extremely positive or negative effects to their well-being. Third, our sample consisted of 21 people living in the UK, therefore assessing the external validity beyond this context is not possible, but likely to be relevant. Also, we did not collect specific data on where people lived within the UK, and we are therefore unable to comment on any potential regional variations in service provision and support. Most interviews were conducted over a 4-month period between November 2020 and March 2021, which may not have captured significant changes in long COVID healthcare provision and an increase in knowledge and awareness of long COVID over time. Finally, online methods of recruitment and data collection may have excluded some participants without access to the internet from taking part, although this method did enable participants to be interviewed in their own homes across different parts of the UK.
Implications
Our findings emphasise and support the need for accessible, patient-centred, specialist multidisciplinary healthcare provision. From healthcare professionals to family members and friends, ensuring people with long COVID are listened to, and their experiences validated, is vital. Importantly, optimising these experiences now features in learning modules and guidance for general practitioners.Reference Atherton, Briggs and Chew-Graham36 Our findings regarding challenges in communicating long COVID experiences to family and friends suggest that it could be of value to adapt similar education and support materials and guidance for informal support networks. Given participants described specific mental health components of long COVID, these should be acknowledged as part of long COVID treatment pathways, and potential contributory factors identified and addressed where possible. Supporting individuals with long COVID in adapting their work, social and physical activities to meet their health capabilities, and to help individuals maintain or adapt their social roles and identity, could also be valuable as part of tailored occupational health programmes.12 Long COVID guidelines now include the ‘Pace, Plan and Prioritise’ principles around ‘pacing’ physical activity for self-management,37 but whether this strategy improves symptom management remains unclear, and participants in previous research describe receiving conflicting advice.Reference Humphreys, Kilby, Kudiersky and Copeland38 Additionally, effects on social participation suggests that there may be a role for tailored community groups and social prescribing, although this should be accompanied by research and evaluation to assess appropriateness and effectiveness.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2022.38.
Data availability
The data are not publicly available due to their containing information that could compromise the privacy of research participants.
Acknowledgements
The authors would like to thank those people who gave up their time to take part and contribute to the study.
Author contributions
All authors meet the criteria for authorship as recommended by the International Committee of Medical Journal Editors. A.B. and D.F. had the original idea for the study. All authors were involved in designing the study. A.B. provided guidance on qualitative methods, including design and analysis. A.B. conducted the interviews. H.A. led the analysis, with support from A.B. and K.E.J.P. Preliminary findings were discussed with the other authors and refined. The first draft of the manuscript was written by A.B. and K.E.J.P.. All authors read, contributed to and agreed on the final manuscript draft.
Funding
This study was funded by the Nuffield Foundation (grant WEL/FR-000022583), the MARCH Mental Health Network funded by the Cross-Disciplinary Mental Health Network Plus initiative supported by UK Research and Innovation (grant ES/S002588/1), and the Wellcome Trust (grant 221400/Z/20/Z). D.F. was funded by the Wellcome Trust (grant 205407/Z/16/Z). K.E.J.P. was supported by the Imperial College Clinician Investigator Scholarship. The funders had no say in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
Declaration of interest
None.








eLetters
No eLetters have been published for this article.