A newborn (gestational age 37 + 5 days, birth weight 2676 g) was found to have cyanosis (pulse oximetry 75%) upon birth. Echocardiography resulted in diagnoses of pulmonary atresia with intact ventricular septum, right ventricle hypoplasia, and patent ductus arteriosus. Continuous prostaglandin E1 was administered immediately. CT angiography confirmed the diagnosis. Transcatheter valvotomy with sequential balloon valvuloplasty was performed at 7 days old. Through the femoral vein approach, a 0.014-inch wire (percutaneous transluminal coronary angioplasty guide wire, Sion) was advanced through the Judkins right guiding catheter to the right ventricle outflow tract, and then a microcatheter (Excelsior) was introduced to the right ventricle outflow tract as a supporting system. Pulmonary valvotomy was performed using coronary guidewire (Conquest Pro 8-20 wire) penetration, and then sequential balloon valvuloplasty was conducted. Saturation was improved to pulse oxymetry 90% by the procedure. Nevertheless, desaturation occurred when prostaglandin E1 administration was tapered. Recatheterization for patent ductus arteriosus stenting was performed at 20 days old. Prostaglandin E1 was discontinued before the procedure. Through the femoral artery approach, the 0.014-inch floppy run-through wire with Judkins right catheter guiding was advanced from the descending aorta side of the patent ductus arteriosus (Fig 1a). The wire could not smoothly pass the patent ductus arteriosus to the pulmonary artery side, with mild distortion occurring at the tip of the wire upon fluoroscopy (Fig 1b, Video 1). Contrast extravasation was found (Fig 1c, Video 2). As ductal dissection was diagnosed, the wire was withdrawn. Desaturation was noted (pulse oximetry reduced to 60%). Repeat angiography showed severe ductal spasm. Readministration of PGE1 (20 ng/kg/minute) was performed. The haemodynamics were stable, and the saturation returned to 85% after 20 min of prostaglandin E1 infusion. Finally, a patent ductus arteriosus stent (Energy 5 mm × 18 mm) was implanted (Fig 1d, Video 3). After oversized patent ductus arteriosus stenting, the patient had tachypnea and pulmonary congestion on chest radiography was noted. Diuretics was used (Furosemide 2 mg/kg/day), and the symptom improved after medication and gradually resolved. No further cyanosis episodes occurred, and the patient was soon discharged. The diuretics was then tapered and discontinued 2 months after procedure.
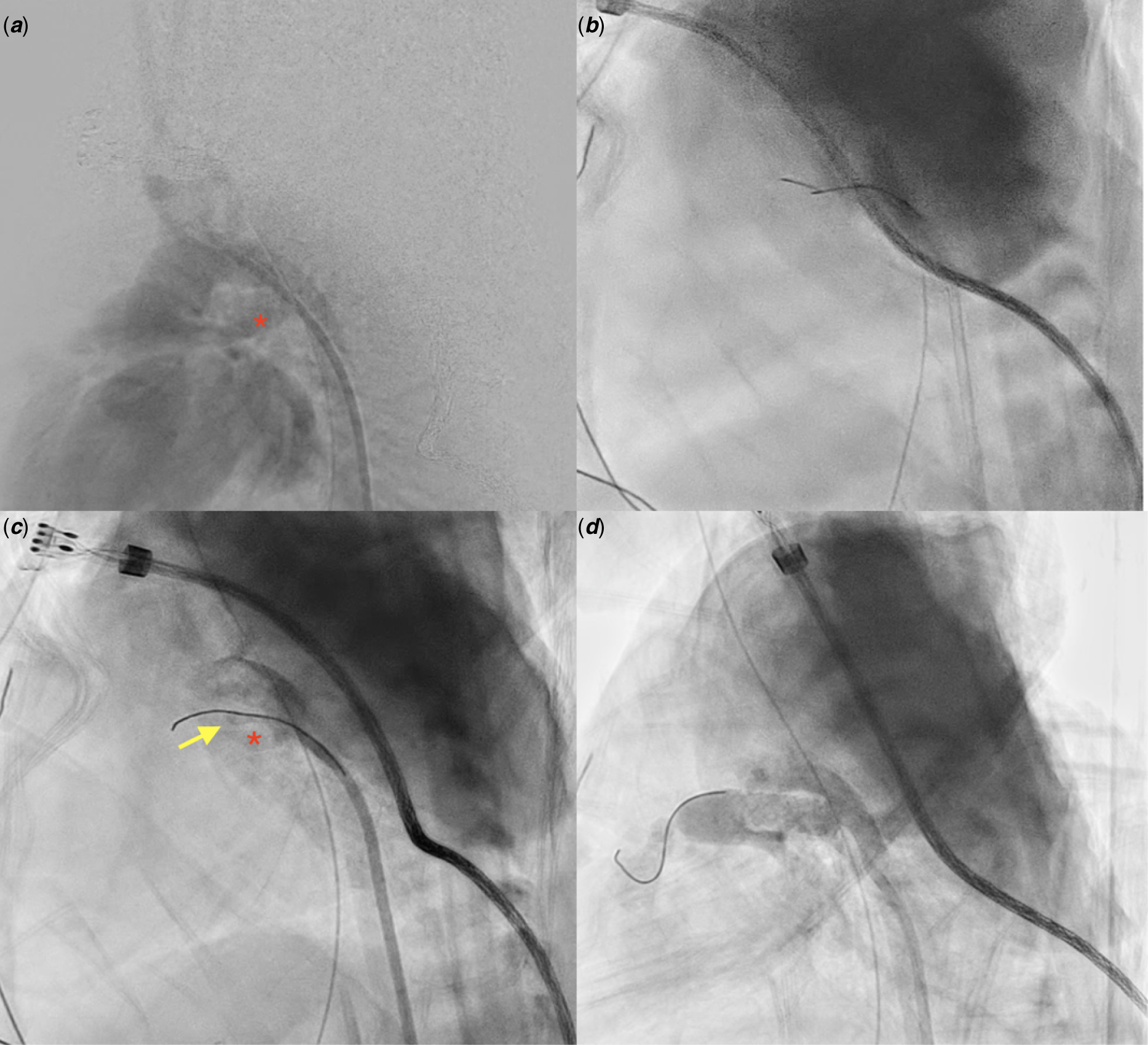
Figure 1. (a) Angiography showed non-tortuous PDA with segmental narrowing on the PA side. Red asterisk: PDA. (b) PTCA-Sion wire was shown by fluoroscopy to be slightly distorted when passed through the PDA. (c) Angiography showed that the Sion wire was dropped in a false lumen, and contrast extravasation and ductal spasm were both found upon angiography. Red asterisk: PDA. Yellow arrow: false lumen. (d) Successful ductal stenting using a coronary stent (5 mm × 18 mm).
Conclusion
Compared with ductal spasm, ductal dissection is rarely mentioned in the literature. Ductal dissection mostly occurs when ducts are crossed by a stiff guidewire. Reference Alwi and Mood1,Reference Aggarwal, Petit, Glatz, Goldstein and Qureshi2 However, even a soft wire may cause the complication. Use of a relatively large stent is an applicable treatment of such cases.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951121003711
Acknowledgements
The authors would like to thank Dr. Jing-Ming Wu for technical suggestions and Dr. Yu-Jen Wei for post-procedure care.
Conflicts of interest
None.




