Pulmonary venous anomalies are classified as anomalous connections, anomalous drainage, or abnormal numbers of pulmonary veins. A single common pulmonary vein belongs in the latter category. Normally, the pulmonary vascular bed drains into the left atrium through four individual pulmonary veins. The most common variation is the presence of a single pulmonary vein on either the right or left side, with a prevalence of about 24% in anatomic studies. Reference Healy1 Rarely, all pulmonary veins enter a single common pulmonary vein that drains into the left atrium. A single common pulmonary vein, usually without stenosis, occurs almost exclusively in cases of visceral heterotaxy with asplenia. Reference Shaddy2
Here, we present a single common pulmonary vein case with polysplenia in detail.
Case
A two-month-old girl was brought to our hospital by ambulance because of slow breathing and bluish colour in the skin noticed by her mother. When the patient came to the emergency room, she had a respiratory arrest, but she responded to pulmonary resuscitation.
We obtained from her medical history that she was born at 38 weeks and weighed 2800 gm as the first child of a 23-year-old mother. She was kept under observation in the regional hospital due to a cleft palate. Additionally, she had been hospitalised twice because of a pulmonary infection. A nasal biopsy had been performed to determine the possibility of ciliary dyskinesia during the second hospitalisation. After a week of home rest, she again experienced respiratory problems and came to our hospital.
In the physical examination, we detected irregular and slow breathing with cyanosis, which responded to nasal oxygenation and aspiration. The first physical examination parameters were as follows: oxygen saturation: 86%, heart rate: 143 beats per minute, respiratory rate: 22 per minute, and body temperature: 37.8 degrees celsius. There was a 2/6-degree heart murmur. In the electrocardiography, we saw sinus rhythm with an incomplete right bundle branch block pattern. A chest radiography showed bilateral pulmonary infiltration. Subsequently, the paediatric cardiologist performed transthoracic echocardiography to understand the cause of the repeating lung infiltration. As the patient had a pulmonary infection, the echocardiography provided suboptimal results. Still, it led to the suspicion that there was a single common pulmonary vein without obstruction at the junction of the left atrium. There was no stenosis or regurgitation of any valve. The presumed pulmonary pressure measured from tricuspid valve with Bernoulli’s equation was 22 mmHg. Also, an enlargement of the right side of the heart and a large atrial septal defect, approximately 10–11 mm in size, were identified (Fig. 1).

Figure 1. (a,b) Modified apical four-chamber images show the pulmonary veins and single common pulmonary vein (c, d) apical four-chamber Doppler images show no obstruction at the junction of the SCPV and left atrium and additional atrial septal defect with left-right shunt. LLPV = left lower pulmonary vein; LUPV = left upper pulmonary vein; RLPV = right lower pulmonary vein; RUPV = right upper pulmonary vein; SCPV = single common pulmonary vein.
To confirm our suspicion and to detect if there is an obstruction in the pulmonary venous tract, a chest CT scan with contrast was performed. It revealed a pulmonary vein abnormality (Figs. 2 and 3). We detected that all four pulmonary veins drained all pulmonary segments and connected to the left atrium through a single common pulmonary vein. In this unusual arrangement, the right upper and lower pulmonary veins joined to form a common right trunk, which traveled posterior to the left atrium and under the left pulmonary artery. Left upper and lower pulmonary veins combined in the anterior of the thoracic aorta. The common right and left trunks then joined to form a single common pulmonary trunk in the anterior of the oesophagus. Ultimately, the right and left pulmonary veins joined the common pulmonary vein and drained the entire pulmonary venous return through a single orifice into the left atrium. There was no evidence of pulmonary venous obstructions along the course of the pulmonary parenchyma and at the junction where the single common pulmonary vein enters the left atrium. Moreover, it was noticed that the right veins were a little dilated. Additionally, hepatic veins entered the right atrium directly, the hepatic segment of the inferior vena cava was absent and both lungs had two lobes indicating left atrial isomerism. Subsequent abdominal ultrasound revealed that the liver was located on the left and extended greatly to the right of the midline; the stomach and spleen were located on the right, and there were multiple spleens.
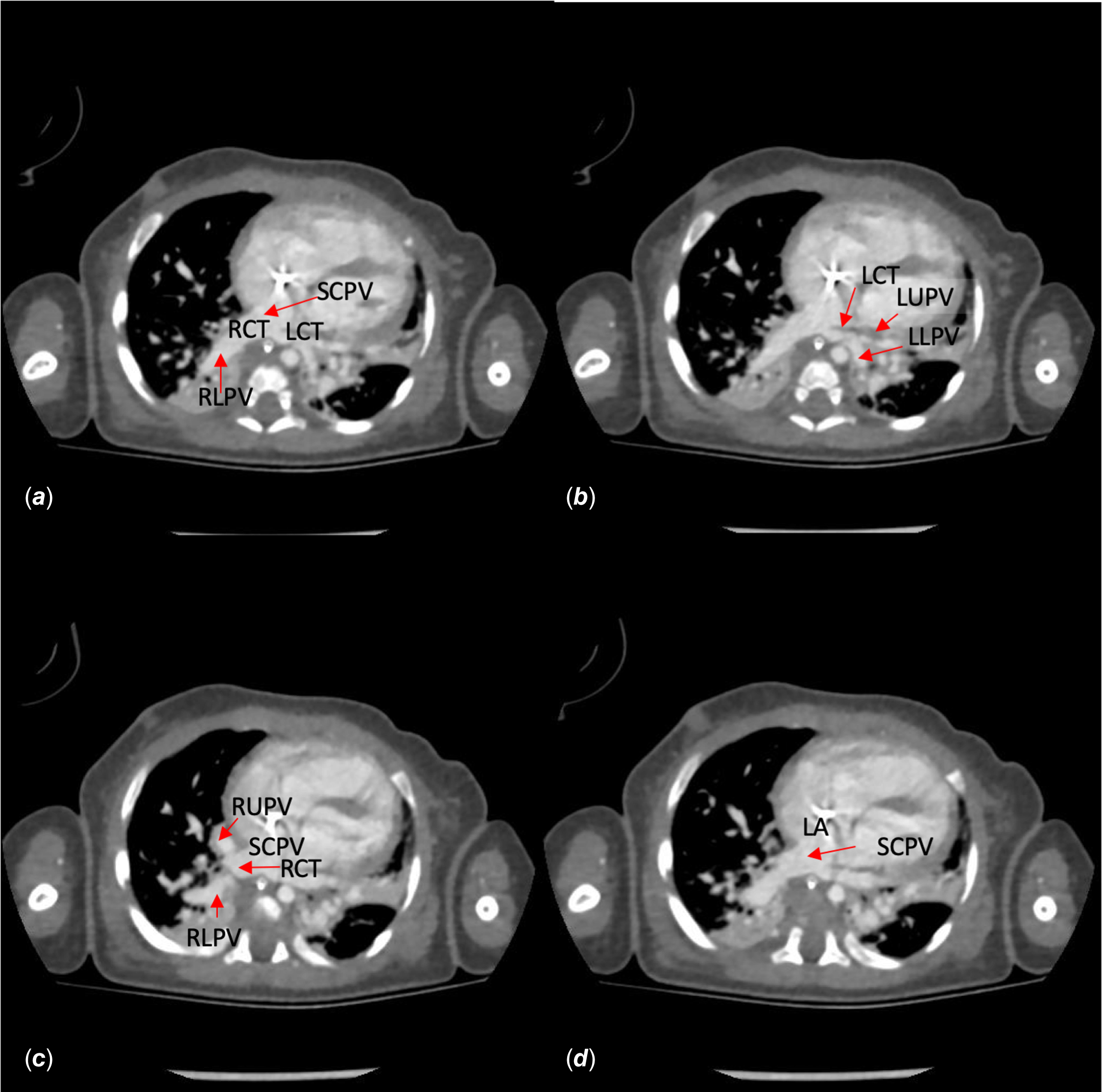
Figure 2. Transvers image. (a) Right and left common trunks combine on the anterior of the oesophagus and join to a single common pulmonary vein ( b) left upper and lower pulmonary veins combine on the anterior of the thoracic aorta. (c) Right upper and lower pulmonary veins combine before joining the single common pulmonary vein. (d) Single common pulmonary vein joining the left atrium. LA = left atrium; LCT = left common trunk; LLPV = left lower pulmonary vein; LUPV = left upper pulmonary vein; RCT = right common trunk; RLPV = right lower pulmonary vein; RUPV = right upper pulmonary vein; SCPV = single common pulmonary vein.

Figure 3. (a,b) Coronal images show the single common pulmonary vein and polysplenia. (c, d) 3D images show the right and left pulmonary arteries SCPV, RUPV, RLPV, RCT, and hepatic veins. Hepatic veins enter the right atrium directly. HVs = hepatic veins; RA = right atrium; RCT = right common trunk; RLPV = right lower pulmonary vein; RUPV = right upper pulmonary vein; SCPV = single common pulmonary vein.
The patient was diagnosed with ciliary dyskinesia according to the nasal biopsy result. After the last pulmonary infection, extubating was not made possible for our patient. We performed a tracheostomy due to prolonged ventilation. Finally, the patient was discharged with a home ventilator.
In the follow-up, the patient underwent atrial septal defect closure surgery at the age of 9 months due to persistent right ventricle dilatation. No early or mid-term complications were observed after the surgical procedure. An echocardiographic examination, 3 months after the operation, showed some decrease in the right ventricular size. The patient is currently under follow-up in our department without any cardiac medicine.
Discussion
Understanding the embryological development of the pulmonary venous system is necessary to figure out pulmonary venous anomalies. The common pulmonary vein develops around the embryonic day 24 at the sinoatrial region to the left of the septum primum. Reference Healy1 There is no connection to the left atrium by embryonic day 32. Then, the pulmonary vascular bed drains via four individual major pulmonary veins into the common pulmonary vein sometime between embryonic days 38 and 40. As the common pulmonary vein is a transient anatomic structure, by a process of differential growth, it results in the ultimate anatomic arrangement. Finally, the four individual pulmonary veins connect separately and directly to the left atrium. Reference Shaddy2
Abnormal development of the common pulmonary vein results in different anomalies. These are classified as follows: (a) Anomalous connection and drainage; total or partial anomalous pulmonary venous return, (b) Stenotic connection; cor triatriatum sinister and stenosis of the individual pulmonary veins, and (c) Abnormal number of the pulmonary veins due to anomalous incorporation of the common pulmonary vein; single left or right pulmonary vein and single common pulmonary vein. Reference Healy1
To our knowledge, a single common pulmonary vein draining into the left atrium is a rare occurrence. Reference Healy1–Reference Fretzayas and Moustaki6 This anomaly may mimic pulmonary arteriovenous malformation on chest radiography. When radiography results are confusing, contrast-enhanced CT or magnetic resonance angiography may be used to differentiate the two clinical entities. Reference Hanson, Wood, Seymour and Petheram4 We just have seen the widespread infiltrates on chest X-ray. Accompanying recurrent pulmonary infection may be what obscured the sign of pulmonary arteriovenous malformation in our case.
The co-existence of a single common pulmonary vein with heterotaxy defects, mostly with asplenia, has been reported previously. Reference Shaddy2 However, our patient had polysplenia syndrome (left atrial isomerism) according to the following criteria; Reference Kaulitz, Ziemer and Hofbeck7 the absence of hepatic segment of the inferior vena cava, lungs with two bilateral lobes, left-positioned liver extending greatly to the right of the midline, right-positioned stomach and spleen and multiple spleens. To our knowledge, this co-existence has not been previously reported.
As we see in our case, heterotaxy defects are also encountered in patients with ciliary dyskinesia. In a study by Fretzayas et al., situs inversus totalis and situs ambiguous were seen with ciliary abnormality in 47.7 and 6.3% of patients, respectively. Reference Fretzayas and Moustaki6 To better define the heterotaxy defects, CT or magnetic resonance angiography may be performed, especially in case of a deficiency of echocardiographic visualisation.
A single common pulmonary vein usually occurs without obstruction. Reference Shaddy2 However, obstruction should be kept in mind in case of recurrent lung infection story. To be sure if there is an obstruction in pulmonary veins, conventional or CT angiography should be performed. In this case, we detected no obstruction in CT angiography and the patient had ciliary dyskinesia explaining the recurrent pulmonary infiltrates. This recurrent pulmonary infection may lead to lung damage over time. Reference Paff, Omran, Nielsen and Haarman8 It explains why we could not extubate the patient. Additionally, we thought that the right heart dilatation occurred at an earlier age in our patient because the flow of a single common pulmonary vein goes directly to the right atrium through the atrial septal defect. Therefore, we decided to perform atrial septal defect closure surgery at the age of 9 months.
Thanks to this patient, we first wanted to remind the medical community about this rare combination. Secondly, we wanted to emphasise that flow pattern differentiation due to the common pulmonary vein may require early surgical treatment.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interests
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Declaration of patient consent
Written informed consent was obtained from the patients’ legal guardians.






