The use of pacemaker implantation for paediatric patients started in the 1960s. Previously, the conventional pacing site was the right ventricular apex. Right ventricular apical pacing alters the sequence of electrical conduction, leading to pacemaker-related cardiac dysfunction (incidence, 5.9%–19.1%). Reference Shalganov, Paprika and Vatasescu1,Reference Balaji and Sreeram2 With recent advancement in technology, His-Purkinje system pacing was proven to be an ideal pacing strategy and closely approximates physiologic status. However, the technology of pacing therapy as well as experience in children is far behind that of adults. Until now, right ventricular septal pacing is considered as the suitable pacing strategy for children according to the recommendation of the 2013 European Heart Rhythm Association/Association for European Paediatric and Congenital Cardiology consensus statement on pharmacological and non-pharmacological therapy for arrhythmias in the paediatric population. Reference Brugada, Blom and Brugada3 Meanwhile, the 2021 PACES expert consensus statement on the indications and management of CIED in paediatric patients did not provide an ideal pacing site for children. Reference Shah, Silka and Avari4 Only a few studies reported on the use of left bundle branch area pacing in children. Reference Chencheng, Dai and Baojing5,Reference Jimenez, Zaban and Sharma6 Therefore, this study aimed to determine the ideal pacing site in children by investigating the difference in postoperative ventricular synchrony in children with left bundle branch area pacing and those with right ventricular septal pacing using two-dimensional speckle tracking echocardiography.
Materials and Methods
Patients
This retrospective observational study enrolled 65 children with bradycardia who were consecutively hospitalised in the First Affiliated Hospital of Tsinghua University from March 2019 to August 2021. All children met the indication of permanent pacemaker implantation Reference Shah, Silka and Avari4 and received pacemaker implantation.
The inclusion criteria were age <18 years, complete atrioventricular block, successful ventricular electrode implantation through transvenous approach, ventricular pacing burden >80%, and duration of follow-up exceeding 6 months postoperatively.
Patients with ventricular pacing burden <80%, those with CHD and underwent surgical correction, and those whose abnormal cardiac structure or with cardiomyopathy, tachyarrhythmia, or other diseases that potentially interfere with the assessment of cardiac function and ventricular synchrony were excluded.
Left bundle branch area pacing was attempted in 19 patients from September 2020 to August 2021. It was successful in 15 patients; the remaining, 4 patients, whose left bundle branch area pacing procedure failed, underwent right ventricular septal pacing. In the remaining 46 patients, right ventricular septal pacing was performed from March 2019 to August 2020. These children were non-randomly divided into two groups according to different ventricular pacing sites: the left bundle branch area pacing group and the right ventricular septal pacing group.
Pacemaker implantation
For the left bundle branch area pacing, a guide wire was inserted (diameter, 0.005 inches) via left axillary approach according to standard procedure. Reference Keping, Xueying and Yan7 Under right anterior oblique 30° fluoroscopy view, a Medtronic C315-S4 delivery sheath (Medtronic, Minneapolis, MN, USA) was inserted, whilst maintaining the tip of the sheath perpendicular to right side of the septum. Subsequently, a Medtronic 3830 electrode was delivered through the sheath. The electrode was screwed clockwise and advanced inside the septum (near the region of the left bundle branch). During this process, peak left ventricular activation time was measured under different voltage outputs (1.0–10.0 V). The morphology of the QRS complex on electrocardiogram was observed. The left bundle branch potential was recorded under under intrinsic rhythm. Under left anterior oblique 40° fluoroscopy view, angiography was performed to evaluate the depth of the electrode inside the septum. After satisfactory pacing parameters were confirmed, the electrode was fixed, and a suitable curvature in the right atrium or inferior caval vein was reserved. Finally, the electrode and pacemaker generator were connected, and pacemaker pocket was closed.
The criteria for successful left bundle branch area pacing Reference Keping, Xueying and Yan7 were the following: the left bundle branch potential was recorded; the electrocardiogram presented a right bundle branch block pattern; the peak left ventricular activation time (which be calculated from stimulus signal to the peak of “R” wave on lead V5 or V6) was shortened abruptly and remained the shortest and constant under different voltage outputs.
The right ventricular septal pacing procedure was basically as same as left bundle branch area pacing procedure except that the electrode was placed at the right-side surface of the septum but was not advanced inside the septum.
For patients who received dual-chamber pacemaker implantation, the atrial electrode was placed in the right atrial appendage.
Electrocardiogram examination
Routine examination of 12-lead electrocardiogram was performed at resting status (paper speed, 25 mm/s; voltage, 10 mm/mV). The broadest QRS complex amongst all leads was defined as paced QRS duration. Electrocardiogram diagnostics were completed by the same physician.
Echocardiography examination
Cardiac function
The left ventricular end-diastolic dimension was measured by two-dimensional echocardiography (GEVivid E9; GE Healthcare, Chicago, IL, USA) and corrected with the patient’s body surface area. The left ventricular ejection fraction was calculated using Simpson’s method. Echocardiographic assessment was completed by the same physician and under blindness condition.
Ventricular synchrony assessment Reference Voigt, Pedrizzetti and Lysyansky8
For the intraventricular synchrony in the left ventricle, Reference Trivedi, Altman, Stanton and Thomas9 speckle tracking echocardiographic images (three consecutive cardiac cycles) were derived from standard left ventricular apical 4-, 3-, and 2-chamber views and from parasternal short axis view. Off-line software (EchoPAC version 7.0; GE Healthcare) was used to analyse ventricular synchrony. The left ventricular global peak longitudinal strain was calculated based on 18 segments that were derived from the three apical views. Peak radial strain and peak circumferential strain were calculated based on the six segments derived from the parasternal short-axis view (papillary muscle level). The standard deviation of the time to peak strain and the maximal difference of time to peak strain (amongst all left ventricular segments) in different types of strain modes (including longitudinal strain, radial strain, and circumferential strain) were calculated. The standard deviation of the time to peak strain ≥ 40 ms or maximal difference of the time to peak strain amongst all segments ≥130 ms was defined as intraventricular dyssynchrony. Reference Klitsie, Roest and Hulst10 Longitudinal Δtime was defined as the delay time of the peak longitudinal strain between the septal and lateral segments (basal level of the left ventricle). Radial Δtime and circumferential Δtime were defined as the delay time of the peak radial strain and peak circumferential strain, respectively, which be calculated from the anterior and posterior segments in the left ventricle. Longitudinal Δtime, radial Δtime, or circumferential Δtime ≥ 130 ms was defined as intraventricular dyssynchrony. Reference Klitsie, Roest and Hulst10 For each segment, the difference between peak strain and the strain value that corresponds to the time when the aortic valve closed was calculated. The strain dyssynchrony index was defined as the average difference amongst all 18 segments. Eventually, the left ventricular longitudinal strain dyssynchrony index, radial strain dyssynchrony index, and circumferential strain dyssynchrony index were calculated.
For the intraventricularI synchrony in the right ventricle, Reference Johnson, Kuyt, Oxborough and Stout11 speckle tracking echocardiographic images were derived from the right ventricular apical four-chamber view. The peak longitudinal strain was calculated from the six segments of the right ventricle. According to the measurement method of the left ventricle, the standard deviation of the time to peak strain and the maximal difference of the time to peak strain in the right ventricle were calculated. Longitudinal Δtime in right ventricle was defined as the delay time of the peak longitudinal strain between the right ventricular septal and lateral segments.
For the interventricular synchrony, interventricularI mechanical delay time was measured by tissue Doppler imaging. An interventricular mechanical delay > 40 ms was defined as interventricular dyssynchrony. Reference Ortega, Morejon and Ricardo12
Pacemaker programming
The pacing mode of dual chamber (DDD) or single chamber (VVIR) was adopted. The pacing frequency was set individually according to patients’ age.
Follow-up
Patients were followed up at 1 week, 3 months, 6 months, 12 months, and once per year postoperatively. Examinations (e.g. echocardiography, electrocardiogram, and chest X-ray) and pacemaker programming were completed at each follow-up. Measurement of capture threshold was performed under the condition of bipolar pacing, with the output width set as 0.4 ms.
Statistical analysis
SPSS version 19.0 (IBM Corp, Armonk, NY, USA) was used for statistical analysis. Continuous variables with normal distribution were expressed as mean ± standard deviation, and Student’s test was used for comparison. Variables with non-normal distribution were expressed as median and interquartile range, and non-parametric test (Mann–Whitney U test) was used for comparison. Categorical data were expressed as number of cases (percentage), and χ2 was used for comparison. Repetitive measurement deviation analysis was used to analyse the trend in echocardiographic parameters over time. Bilateral p values <0.05 were considered statistically significant.
Results
Patient characteristics
Of the 65 patients, 17 were excluded (pacing burden <80%, 4 patients; surgical history of CHD, 7 patients; follow-up duration < 6 months, 6 patients). Finally, 48 patients (male, 28; female, 20) were included in this study. The patients’ age ranged from 0.7 to 14 years, with a median of 2.7 years (interquartile range, 1.7–4.6 years). The median weight was 13.5 kg (interquartile range, 10.3–18.1 kg). All children were diagnosed with complete atrioventricular block. Four children (8.3%) were implanted with a dual-chamber pacemaker, whereas 44 children (91.7%) were implanted with a single-chamber pacemaker. Of the 48 patients, 45 (93.75%) underwent pacemaker implantation for the first time; meanwhile, 3 (6.3%) underwent reoperation because of previous epicardial pacemaker or electrode malfunction malfunction. These three patients received ventricular electrode implantation through the intravenous approach, and the previous epicardial electrode was abandoned. Before pacemaker implantation, Holter examinations showed that the average heart rate was 50 ± 4 beats per minute and that the daily average of total heart rate was 70,000 ± 6000 beats per day. Preoperatively, left ventricular enlargement (left ventricular end-diastolic dimension Z score >2) was observed in 33 patients (68.8%). Normal cardiac function (left ventricular ejection fraction ≥55%) was observed in all patients. The general characteristics of the patients of the left bundle branch area pacing and right ventricular septal pacing groups are presented in Table 1.
Table 1. Comparison of patient characteristics in the LBBaP and RVSP groups

Values are presented as median [interquartile range], n (%), or mean±standard deviation.
LBBaP = left bundle branch area pacing; RVSP = right ventricular septal pacing; PM = pacemaker; LVEDD = left ventricular end-diastolic dimension; LVEF = left ventricular ejection fraction; QRSd = QRS duration on electrocardiogram.
Intraoperative pacing parameters
Intraoperatively, the capture thresholds (ventricular electrode) of the left bundle branch area pacing and right ventricular septal pacing groups were 0.55 ± 0.11 and 0.58 ± 0.10 V, respectively (p = 0.436). The R-wave amplitudes (ventricular electrode) of the patients of the left bundle branch area pacing and right ventricular septal pacing groups were 13.3 ± 4.5 and 14.6 ± 3.7 mV, respectively (p = 0.342). The impedance values (ventricular electrode) of the left bundle branch area pacing and right ventricular septal pacing groups were 710.4 ± 112.7 and 721.0 ± 118.7 Ω, respectively (p = 0.966). The intraoperative pacing parameters did not significantly differ between the two groups.
Under bipolar pacing (voltage output, 3.0 V), the average peak left ventricular activation time of the left bundle branch area pacing group was significantly shorter than that of the right ventricular septal pacing group (51.6 ± 6.6 versus 72.5 ± 15.4 ms, p = 0.000). Additionally, the average paced QRS duration of the left bundle branch area pacing group was significantly narrower than that of the right ventricular septal pacing group (100.2 ± 9.3 versus 115.4 ± 15.1 ms, p = 0.001).
Follow-up
Pacemaker-related complications
The permanent pacemaker implantation was successful in all patients. No electrode-related complications (e.g. electrode dislocation, myocardium perforation, pericardial tamponade, infectious endocarditis, and thromboembolism) were recorded during follow-up.
Pacing parameters
The median follow-up duration for all patients was 1.5 years (interquartile range, 1–2 years). The average ventricular pacing was 96.2 ± 2.0%. The capture threshold (ventricular electrode) of the right ventricular septal pacing group was higher than baseline. The capture threshold the left bundle branch area pacing group was maintained well and stable during follow-up (Fig 1-A). At the last follow-up, the average capture threshold of the left bundle branch area pacing group was lower than that of the right ventricular septal pacing group (0.79 ± 0.18 versus 1.20 ± 0.56 V, p = 0.008). The capture thresholds of the left bundle branch area pacing group were all <1.0 V. On the contrary, a capture threshold >1.0 V was observed in 8 patients (39.4%) in the right ventricular septal pacing group. The average R-wave amplitude (ventricular electrode) of the left bundle branch area pacing group was higher than that of the right ventricular septal pacing group (16.8 ± 5.0 versus 13.6 ± 4.5 mV, p = 0.033). The impedance (ventricular electrode) did not significantly differ between the two groups (538.4 ± 63.5 versus 533.8 ± 100.8 Ω, p = 0.872). The change tendency of the pacing parameters during follow-up is presented in Figure 1.

Figure 1. Change tendency of the pacing parameters of the left bundle branch area pacing (LBBaP) and right ventricular septal pacing (RVSP) groups during follow-up. ( a ) Capture threshold. ( b ) R-wave amplitude. ( c ) Impedance.
Cardiac function
At the last follow-up, the left ventricular end-diastolic dimension Z score and left ventricular ejection fraction of the left bundle branch area pacing and right ventricular septal pacing groups were 0.5 ± 1.0 versus 0.6 ± 1.1 and 67.3 ± 3.8% versus 66.3 ± 4.3%, respectively (all p values >0.05).
Ventricular synchrony (evaluated at last follow-up)
Intraventricular synchrony in the left ventricle
Assessment of the longitudinal strain synchrony showed that the parameters (e.g. standard deviation of the time to peak longitudinal strain, maximal difference of the time to peak longitudinal strain, and longitudinal strain dyssynchrony index) of the left bundle branch area pacing group were significantly shorter than those of the right ventricular septal pacing group (all p values <0.05).
Assessment of the radial strain synchrony showed that the parameters (e.g. radial Δtime and radial strain dyssynchrony index) of the left bundle branch area pacing group were significantly shorter than those of the right ventricular septal pacing group (all p values <0.05).
Assessment of the circumferential strain synchrony showed that the parameters (e.g. standard deviation of the time to peak circumferential strain, circumferential Δtime, maximal difference of the time to peak circumferential strain, and circumferential strain dyssynchrony index) of the left bundle branch area pacing group were significantly shorter than those of the right ventricular septal pacing group (all p values <0.05).
The comparison of intraventricular synchrony (left ventricle) between the two groups is presented in Table 2. The comparisons of the postoperative electrocardiogram, and the synchrony images of a patient with left bundle branch area pacing and another patient with right ventricular septal pacing are presented in Figures 2 and 3, respectively.

Figure 2. Postoperative electrocardiogram (ECG) and echocardiographic image in one patient with left bundle branch area pacing (LBBaP) and in another patient with right ventricular septal pacing (RVSP). A-1: ECG in a patient with LBBaP that presented a right bundle branch block pattern with a QRS duration of 102 ms. A-2: Postoperative echocardiographic image of the patient with LBBaP showing the ventricular electrode placed inside the septum (red arrow). B-1: Postoperative ECG in another patient with RVSP that presented a left bundle branch block pattern with a QRS duration of 116 ms. The QRS duration of this patient was broader than that of the other patient. B-2: Postoperative echocardiographic image of the patient with RVSP showing the ventricular electrode placed at the right-side surface of the septum (not placed inside the septum).

Figure 3. Echocardiographic images of ventricular synchrony in one patient with left bundle branch area pacing (LBBaP) and in another patient with right ventricular septal pacing (RVSP). A-1 to A-3: In the patient with LBBaP, the assessment images of the left ventricular longitudinal synchrony were derived from the left ventricular apical 4- (A-1), 3- (A-2) and two-chamber viewsview (A-3). In this patient, the synchrony of the left ventricular myocardium was maintained well, standard deviation of the time to peak longitudinal strain (longitudinal Ts-SD) was 29.4 ms. B-1 to B-3: In the patient with RVSP, the assessment images revealed that the synchrony of the left ventricular myocardium was not as good as that of the former one (longitudinal Ts-SD = 49 ms).
Table 2. Comparison of intraventricular synchrony (left ventricle) parameters between the LBBaP and RVSP groups
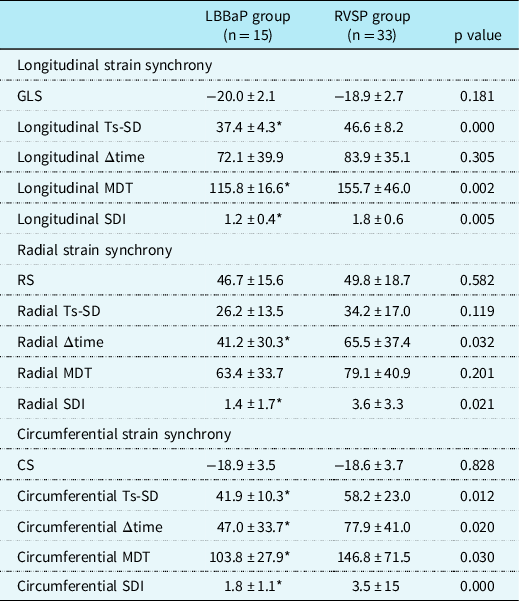
Values are presented as mean ± standard deviation.
* Statistically significant difference (p < 0.05) between the groups.
LBBaP = left bundle branch area pacing; RVSP = right ventricular septal pacing; GLS = left ventricular global peak longitudinal strain; RS = peak radial strain; CS = peak circumferential strain; Ts-SD = standard deviation of the time to peak strain; Δtime = delay time of the peak strain between specific segments; MDT = maximal difference of the time to peak strain amongst all segments; SDI = strain dyssynchrony index.
Intraventricular synchrony in the right ventricle
The absolute value of the peak longitudinal strain (right ventricle) of the left bundle branch area pacing group was greater than that of the right ventricular septal pacing group. The parameters (e.g. standard deviation of the time to peak strain and maximal difference of the time to peak strain) of the left bundle branch area pacing group were significantly shorter than those of the right ventricular septal pacing group (Table 3).
Table 3. Comparison of intraventricular synchrony (right ventricle) parameters between the LBBaP and RVSP groups

Values are presented as mean ± standard deviation.
* Statistically significant difference (p < 0.05) between the groups.
LBBaP = left bundle branch area pacing; RVSP = right ventricular septal pacing; RV = right ventricle; LS = peak longitudinal strain; Ts-SD = standard deviation of the time to peak strain; Δtime = delay time of the peak strain between specific segments; MDT = maximal difference of the time to peak strain amongstamong all segments.
Interventricular synchrony
The average interventricular mechanical delay time of the left bundle branch area pacing group was significantly shorter than that of the right ventricular septal pacing group (36.4 ± 14.2 versus 52.5 ± 22.7 ms, p = 0.016).
Analysis of the trend in ventricular synchrony over time
In 35 patients, the ventricular synchrony parameters evaluated at different time points of follow-up (1 week, 3 months, and 6 months postoperatively) were used to analyse the trend in synchrony parameters over time. The standard deviation of the time to peak longitudinal strain, peak radial strain, and peak circumferential strain did not show statistically significant differences amongst different time points (all p values >0.05) (Fig 4).

Figure 4. Ventricular synchrony parameters evaluated at different time points of follow-up: 0.25 month, 3 months, and 6 months. Analysis of variance was used for the comparison of repetitive measurement. ( a ) The standard deviation of the time to peak longitudinal strain (longitudinal Ts-SD) showed no difference amongst different time points. ( b ) The standard deviation of the time to peak radial strain (radial Ts-SD) showed no difference amongst different time points. ( c ) The standard deviation of the time to peak circumferential strain (circumferential Ts-SD) showed no difference amongst different time points.
Discussion
Right ventricular apical pacing was widely adopted in the past, and many studies had proven the disadvantage of this pacing strategy. Reference Shalganov, Paprika and Vatasescu1,Reference Balaji and Sreeram2 At present, the right ventricular septum, via the transvenous approach, is the major pacing site for children. Reference Brugada, Blom and Brugada3 Although right ventricular septal pacing produces narrow-produce paced QRS duration, it still has shortcoming. During right ventricular septal pacing, the right ventricle is excited earlier than the left ventricle; thus, the motion of the left ventricular free wall is delayed compared with that of the right ventricle (the so-called interventricular dyssynchrony). The effects of right ventricular septal pacing in terms of maintaining ventricular synchrony and cardiac function are still controversial. Reference Mahfouz, Mesbah, Ammar, Khedr and Abdullah13–Reference Mizukami, Matsue and Naruse18
With the rapid development of technology, many studies have confirmed the advantage of left bundle branch area pacing. Studies proved that left bundle branch area pacing produces narrower-paced QRS duration and better echocardiographic cardiac function than does right ventricular septal pacing. Reference Liu, Li, Wang, Zhou and Wu19,Reference Li, Zhang and Qiu20 Meanwhile, a study that reported on the use of left bundle branch area pacing in children. Reference Chencheng, Dai and Baojing5 The results of our study showed that left bundle branch area pacing was safe and effective in children. The paced QRS duration of the left bundle branch area pacing group was significantly narrower than that of the right ventricular septal pacing group (100.2 ± 9.3 versus 115.4 ± 15.1 ms). During follow-up, the capture threshold of the ventricular electrode in the left bundle branch area pacing group was lower than in the right ventricular septal pacing group. Capture thresholds were all <1.0 V in the left bundle branch area pacing group. On the contrary, a capture threshold >1.0 V was observed in 39.4% of the patients in the right ventricular septal pacing group. Some studies also proved that left bundle branch area pacing produces constant electrical parameters. Reference Huang, Su and Wu21,Reference Li, Chen and Dai22 Maintaining good electrical parameters is important for children, especially for those with a high percentage of pacing burden. An increased capture threshold would lead to premature battery depletion and shorten the service life of a pacemaker. Furthermore, the reoperation (pacemaker replacement) would increase the risk of surgical complications and medical expenditure. In terms of the stability of electrical parameters, left bundle branch area pacing hold an advantage over right ventricular septal pacing.
Assessment of ventricular synchrony is essential. Cai et al. Reference Cai, Huang and Li23 and Sun et al. Reference Sun, Di, Gao, Lan and Peng24 used speckle tracking echocardiography method to compare the difference of postoperative ventricular synchrony in patients with left bundle branch pacing and those with right ventricular septal pacing. Results showed that the intraventricular synchrony parameters (e.g. standard deviation of the time to peak strain and strain dyssynchrony index) in the left bundle branch area pacing group were better than those in the right ventricular septal pacing group. Song et al. Reference Song, Kim and Bae25 and Tomaske et al. Reference Tomaske, Breithardt, Balmer and Bauersfeld26 used two-dimensional speckle tracking echocardiography to assess the intraventricular synchrony in children with pacemaker. Reference Song, Kim and Bae25,Reference Tomaske, Breithardt, Balmer and Bauersfeld26 In their studies, intraventricular synchrony parameters such as peak strain, standard deviation of the time to peak strain, and maximal difference of the time to peak strain were adopted. However, no study has assessed the ventricular synchrony in children with left bundle branch area pacing. The assessment methods adopted in the said studies were referenced. According to the guidelines that recommended the practical standard in measuring ventricular synchrony, Reference Voigt, Pedrizzetti and Lysyansky8,Reference Trivedi, Altman, Stanton and Thomas9 different types of intraventricular synchrony parameters (e.g. longitudinal strain, radial strain, and circumferential strain) were measured in this study. Results proved that the parameters such as the standard deviation of the time to peak strain, maximal difference of the time to peak strain, and strain dyssynchrony index in the left bundle branch area pacing group were all better than those in the right ventricular septal pacing group, which implies that, compared with right ventricular septal pacing, left bundle branch area pacing has a better intraventricular synchrony in the left ventricle. In this study, intraventricular synchrony in the right ventricle was assessed according to the guideline published by the European Association of Cardiovascular Imaging and the American Society of Echocardiography in 2018. Reference Badano, Kolias and Muraru27 To date, no other study has reported on right ventricular synchrony in children with pacemaker. Results showed that the patients of the left bundle branch area pacing group maintained a better intraventricular synchrony in the right ventricle than the patients of the right ventricular septal pacing group. Additionally, we used tissue Doppler imaging technology to measure interventricular mechanical delay in order to assess interventricular synchrony. Our results proved that left bundle branch pacing has an advantage in maintaining interventricular synchrony over right ventricular septal pacing. The possible mechanism might be explained as follows: during left bundle branch pacing, the left bundle branch, and regional myocardium are excited simultaneously. Then, electrical activation transmits down and spreads to the bilateral ventricles, and the electrical activation sequence is close to normal physiologic status. On the contrary, the phenomenon of interventricular delay is common observed under right ventricular pacing. Maintaining a good ventricular synchrony contributes in the maintenance of cardiac function during long-term pacing therapy.
This study proved that left bundle branch area pacing is safe and effective for children. Paced QRS duration in patients with left bundle branch area pacing was narrower than that in patients with right ventricular septal pacing. Additionally, left bundle branch area pacing produces acceptable electrical parameters (in comparison with right ventricular septal pacing, which is known to be problematic in this regard). Echocardiographic cardiac function parameters (e.g. left ventricular ejection fraction) did not show significant differences between the two groups. All patients maintained their cardiac function during follow-up. In fact, all patients had normal cardiac function before pacemaker implantation. A study in adult showed that left bundle branch area pacing can reverse cardiac insufficiency, Reference Li, Zhang and Qiu20 the advantage of left bundle branch area pacing is pronounced in patients with cardiac insufficiency. Nevertheless, the duration of follow-up is short in our study. In children, the advantage of left bundle branch area pacing in terms of maintaining cardiac function for long-term should be confirmed by future studies.
Acknowledgements
None.
Financial support
This study was supported by the Dr Wu Shunde Foundation for Research in Medical Science (grant/award number: 20240000811).
Conflict of interest
All authors declare that this study was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical statement
All procedures in this study involving human participants were performed in accordance with the ethical standards of the institutional and the Helsinki Declaration of 1975. This study was approved by the ethics committee of our hospital (ethics document batch number: 202003).










