Introduction
The burden of anxiety and depression had escalated since the onset of the COVID-19 pandemic (Alacevich et al., Reference Alacevich, Thalmann, Nicodemo, de Lusignan and Petrou2023; Coley and Baum, Reference Coley and Baum2022; Deng et al., Reference Deng, Zhou, Hou, Silver, Wong, Chang, Huang and Zuo2021; Nápoles et al., Reference Nápoles, Stewart, Strassle, Alhomsi, Quintero, Ponce, Wilkerson and Bonilla2023; Santomauro et al., Reference Santomauro, Mantilla Herrera, Shadid, Zheng, Ashbaugh, Pigott, Abbafati, Adolph, Amlag, Aravkin, Bang-Jensen, Bertolacci, Bloom, Castellano, Castro, Chakrabarti, Chattopadhyay, Cogen, Collins and Ferrari2021; Vai et al., Reference Vai, Mazza, Delli Colli, Foiselle, Allen, Benedetti, Borsini, Casanova Dias, Tamouza, Leboyer, Benros, Branchi, Fusar-Poli and De Picker2021; Zhou et al., Reference Zhou, Zhang, Wang, Guo, Wang, Chen, Liu, Chen and Chen2020; Zhu et al., Reference Zhu, Zhang, Li, Chen and Wang2023). The national emergency due to the COVID-19 outbreak was declared by the US President on 13 March 2020 (The White House, 2023), which lasted until 11 May 2023 (CDC, 2023a). Various nationwide public health measures were implemented, including lockdowns, isolation after testing positive and social distancing restrictions. Such interventions likely exacerbated material hardships, reduced social support, and disrupted physical activity and mental health service routines. Moreover, the pandemic itself heightened fears and uncertainties regarding virus transmission and the health of loved ones. However, longitudinal data on the persistence of symptoms of anxiety and depression throughout the pandemic are scarce. Understanding the enduring impact of the pandemic on mental health is crucial (Penninx et al., Reference Penninx, Benros, Klein and Vinkers2022).
Individuals with mental health symptoms exhibited higher vaccine hesitancy and lower COVID-19 vaccination uptake compared to the general population during the initial vaccine rollout in the US, mirroring patterns observed with similar vaccines like influenza (Jayakumar et al., Reference Jayakumar, Ilango, Kumar, Alassaf, Aljabr, Paramasivam, Hawsah, M. and Aldawish2022; Lorenz et al., Reference Lorenz, Norris, Norton and Westrick2013; Nguyen et al., Reference Nguyen, Chen, Morris, Chui and Allen2022; Rane et al., Reference Rane, Kochhar, Poehlein, You, Robertson, Zimba, Westmoreland, Romo, Kulkarni, Chang, Berry, Parcesepe, Maroko, Grov and Nash2022; Sekizawa et al., Reference Sekizawa, Hashimoto, Denda, Ochi and So2022). The nationally representative Household Pulse Survey (HPS) of 77,000 adults in March 2021 revealed that only 40% of individuals with anxiety or depression symptoms were vaccinated, contrasting with 53% vaccination uptake among those without such symptoms (Nguyen et al., Reference Nguyen, Chen, Morris, Chui and Allen2022). Additionally, a cross-sectional study of over 14,000 US adults from a healthcare system in March 2021 found that individuals diagnosed with major depressive disorder or generalized anxiety disorder had 1.44 (95% CI: 1.25, 1,66) and 1.45 (95% CI: 1.20, 1.77) times higher odds of COVID-19 vaccine hesitancy compared to those without such disorders, respectively (Eyllon et al., Reference Eyllon, Dang, Barnes, Buresh, Peloquin, Hogan, Shimotsu, Sama and Nordberg2022).
The low uptake of COVID-19 vaccines is a significant public health concern. Only 20.5% of US adults had received the bivalent booster by May 2023, and 20.9% (95% CI: 20.3–21.6%) had received the 2023–2024 monovalent vaccine by 27 January 2024 (CDC, 2020, 2024a, 2024b; USAFacts, 2023a). Understanding the association between mental health symptoms and COVID-19 vaccine uptake for both primary series and subsequent boosters is critical for informing strategies to improve vaccination uptake. In a national prospective cohort, we aimed to (1) characterize the prevalence and persistence of moderate to severe anxiety and depression symptoms from July 2020 to July 2023; (2) explore the association between demographic characteristics and symptom persistence during this period and (3) assess how ongoing moderate to severe anxiety symptoms and depression symptoms impact COVID-19 vaccination between May 2021 and July 2023.
Methods
Data source and analytical population
The Communities, Households, and SARS-CoV-2 Epidemiology (CHASING) COVID Cohort study was a national prospective cohort launched on 28 March 2020. The community-based sample included participants aged ≥18 from diverse backgrounds residing in the US or US territories, recruited through internet-based strategies or referrals between March and June 2020. Study participants were recruited through social media ads (Facebook, Instagram and Scruff), Qualtrics Panel and referrals from personal networks. Ads were in English and Spanish, targeting people in the US and US territories aged 18 and older. We monitored demographics and adjusted strategies to ensure a balanced representation, focusing on older participants if needed.
In this fully online cohort, participants completed follow-up assessments approximately quarterly from July 2020 to December 2023, reporting underlying health conditions, anxiety, depression, employment status and COVID-19 vaccination uptake. Comprehensive details regarding recruitment and follow-up were presented in previous articles (Rane et al., Reference Rane, Kochhar, Poehlein, You, Robertson, Zimba, Westmoreland, Romo, Kulkarni, Chang, Berry, Parcesepe, Maroko, Grov and Nash2022; Robertson et al., Reference Robertson, Kulkarni, Rane, Kochhar, Berry, Chang, Mirzayi, You, Maroko, Zimba, Westmoreland, Grov, Parcesepe, Waldron and Nash2021). For this analysis, we included (1) participants completed baseline assessment; (2) participants with at least one of the three follow-up assessments between July 2023 and December 2023 to confirm their COVID-19 vaccine doses as of July 2023 and (3) participants with at least one of 14 follow-up assessments completed between July 2020 and July 2023, to evaluate anxiety and depression symptoms.
The study protocol was approved by the Institutional Review Board of the City University of New York (CUNY) Graduate School of Public Health and Health Policy (New York, NY, USA). Participant consents were obtained online at baseline and periodically during follow-up assessments.
Outcome: COVID-19 vaccination status and doses
During each of the 13 follow-up assessments between December 2020 and December 2023, participants reported their involvement in COVID-19 vaccine trials, manufacturer of their primary series, and dates and doses received. Those completing a single-dose series (e.g., Janssen) or a two-dose series (e.g., Pfizer and Moderna) were considered to have completed their primary series. Between October 2021 and April 2023, participants completing their primary series were asked about receiving booster doses between follow-up assessments. From April 2023, the Advisory Committee on Immunization Practices recommended a single mRNA dose for unvaccinated individuals aged ≥6 without moderate or severe immunocompromise (Moulia et al., Reference Moulia, Wallace, Roper, Godfrey, Rosenblum, Link-Gelles, Britton, Daley, Meyer, Fleming-Dutra, Oliver and Twentyman2023). Starting July 2023, we collected data on recent vaccines for participants who hadn’t completed the primary series, as well as additional doses received between follow-up assessments for those who had completed the primary series. We defined two outcomes: (1) participants who received any COVID-19 vaccine by each follow-up between May 2021 and July 2023, when vaccines were widely available in the US and (2) total COVID-19 vaccine doses received by participants by July 2023. Since the analysis included individuals who completed at least one of three follow-up assessments between July and December 2023, during which their vaccination status and doses as of July 2023 were confirmed, and because participants were asked to recall vaccinations received since their last completed survey, there was no missing data for vaccination status or dosage.
Exposure: Moderate to severe anxiety and depression symptoms and multiple imputation of missing GAD-7 and PHQ-8
During baseline from March to June 2020 and each of 14 follow-up assessments from July 2020 to July 2023, anxiety symptoms were measured using the 7-item Generalized Anxiety Disorder scale (GAD-7). The GAD-7 assessed anxiety-related symptoms over the past month, with responses including ‘not at all’, ‘several days’, ‘over half the days’ and ‘nearly every day’, scored 0, 1, 2 and 3, respectively (Spitzer et al., Reference Spitzer, Kroenke, Williams and Löwe2006). Scores were summed, ranging from 0 to 21, with scores ≥10 indicating moderate to severe anxiety symptoms (Plummer et al., Reference Plummer, Manea, Trepel and McMillan2016). The GAD-7 had exhibited 89% sensitivity and 82% specificity for detecting generalized anxiety disorders in the general population (Kroenke et al., Reference Kroenke, Spitzer, Williams, Monahan and Löwe2007; Löwe et al., Reference Löwe, Decker, Müller, Brähler, Schellberg, Herzog and Herzberg2008).
Similarly, depression symptoms were evaluated at baseline and throughout 14 follow-ups between July 2020 and July 2023. At baseline, the 2-item Patient Health Questionnaire (PHQ-2) was used (Löwe et al., Reference Löwe, Kroenke and Gräfe2005). Subsequently, the PHQ-8, a validated 8-item questionnaire, was employed (Kroenke et al., Reference Kroenke, Strine, Spitzer, Williams, Berry and Mokdad2009; Lee et al., Reference Lee, Schulberg, Raue and Kroenke2007). Response options of ‘not at all’, ‘several days’, ‘over half the days’ and ‘nearly every day’ were scored from 0 to 3, generating a total score ranging from 0 to 24. Scores ≥10 indicated moderate to severe depression symptoms, exhibiting 88% sensitivity and 88% specificity for detecting generalized depression disorders (Thombs et al., Reference Thombs, Benedetti, Kloda, Levis, Nicolau, Cuijpers, Gilbody, Ioannidis, McMillan, Patten, Shrier, Steele and Ziegelstein2014).
Missing GAD-7 and PHQ-8 at each follow-up was addressed using multiple imputations via the Markov Chain Monte Carlo method. The imputation model incorporated various demographic factors, including age, gender, race/ethnicity, education, income, presence of children <18, healthcare access barriers, comorbidities and the respective baseline GAD-7 and PHQ-2 scores. Additionally, employment category, income loss due to COVID-19, food insecurity and housing instability from the last available follow-up were included. We assessed the missing data mechanism to determine whether the data were missing at random (MAR), where missingness could be predicted by observed variables. Based on previous studies and our cohort’s experience, we believed that demographic factors, financial stressors and baseline anxiety and depression symptoms were sufficient to predict the missingness (Bowen et al., Reference Bowen, Wesley, Cooper, Meier, Kaar and Simon2022; Ettman et al., Reference Ettman, Abdalla, Cohen, Sampson, Vivier and Galea2020; Guan et al., Reference Guan, Guariglia, Moore, Xu and Al-Janabi2022; Schlax et al., Reference Schlax, Jünger, Beutel, Münzel, Pfeiffer, Wild, Blettner, Kerahrodi, Wiltink and Michal2019). Ten imputations were conducted for each missing score, each with a weight of 0.1. The weighted average imputed scores were calculated, providing an unbiased estimator of the missing values (Barnard, Reference Barnard1999; Brand et al., Reference Brand, van Buuren, le Cessie and van den Hout2019; Donders et al., Reference Donders, van der Heijden, Stijnen and Moons2006).
To ensure the robustness of multiple imputation, we carefully selected an imputation model that accurately reflected the structure of the data (e.g., incorporating relevant predictors) and was tailored to the nature of the missing data, which in this case involved zero-inflated continuous data (Sterne et al., Reference Sterne, White, Carlin, Spratt, Royston, Kenward, Wood and Carpenter2009). Since we employed iterative imputation methods, we verified that the models had converged and that the imputations remained stable across iterations. Finally, we performed diagnostic checks, including density plots, to evaluate whether the imputation model produced reasonable estimates compared to observed data, ensuring the imputation process did not introduce bias.
Characterizing anxiety and depression symptoms between July 2020 and July 2023: ever experienced symptoms, persistence of symptoms and latent class growth analysis (LCGA) trajectories
Participants were classified as having ever experienced moderate to severe anxiety and depression symptoms if they scored ≥10 on the GAD-7 and PHQ-8 in at least one of the 14 follow-up assessments from July 2020 to July 2023, respectively. Persistence of these symptoms was defined as scoring ≥10 on the GAD-7 and PHQ-8 for ≥7 out of 14 follow-up assessments between July 2020 and July 2023, respectively. Latent class growth analysis (LCGA) modelling were employed to identify common patterns of GAD-7 and PHQ-8 trajectories across 14 time points from July 2020 to July 2023 (Nagin, Reference Nagin2005, Reference Nagin2014; Nagin and Odgers, Reference Nagin and Odgers2010). We used the change in the Bayesian information criterion (BIC) between models and the posterior probability of group membership to determine the optimal number of trajectories for GAD-7 and PHQ-8 (Jones et al., Reference Jones, Nagin and Roeder2001).
Sociodemographic characteristics: risk factors for persistent symptoms and covariates included in multiple imputation and multivariable regression models
Baseline information including age, gender, race/ethnicity, education, household income, presence of children <18 and number of comorbidities were collected between March and June 2020. As a proxy for difficulty accessing healthcare, we used factors that impact medical care access: lack of a primary care doctor, concerns about healthcare costs, concerns about seeing a doctor due to immigration status and lack of insurance. Participants who responded affirmatively to any of these factors were classified as having more barriers. The questions were from the Behavioral Risk Factor Surveillance System (BRFSS) questionnaires (CDC, 2022), and the scale has been previously used to document healthcare barriers during the 2009–2010 influenza A pandemic (Kumar et al., Reference Kumar, Quinn, Kim, Daniel and Freimuth2012; Quinn et al., Reference Quinn, Kumar, Freimuth, Musa, Casteneda-Angarita and Kidwell2011) and the COVID-19 pandemic (Robertson et al., Reference Robertson, Shamsunder, Brazier, Mantravadi, Zimba, Rane, Westmoreland, Parcesepe, Maroko, Kulkarni, Grov and Nash2022). At each follow-up, we evaluated employment category, income loss due to COVID-19, food insecurity and housing instability. Variable definitions were provided in Appendix 1. Participants who completed the baseline assessment were eligible for inclusion in the analytical cohort; therefore, missing data was not a concern for sociodemographic or healthcare access measurements.
Statistical analysis
We compared the demographic characteristics between participants who ever vs. never experienced symptoms, experienced persistent vs. non-persistent symptoms, and by LCGA trajectories. Statistical comparisons of proportions were performed using chi-squared or Fisher-exact tests. Wilcoxon rank-sum tests were used to compare medians and interquartile ranges (IQRs). Unadjusted risk ratios were estimated using robust Poisson regression models to assess the risk of ever experiencing symptoms, experiencing persistent symptoms and having persistently high trajectories of scores. LCGA modelling utilized cubic trends over time, exploring 2–4 trajectories, and a zero-inflated Poisson model was used considering data distribution and type (Jones et al., Reference Jones, Nagin and Roeder2001). The best-fitting model was selected based on ΔBIC (Jones et al., Reference Jones, Nagin and Roeder2001) and clinical relevance. We characterized ever experiencing symptom, persistence of symptoms, and LCGA trajectories using the weighted average imputed score to address missing GAD-7 and PHQ-8 scores in each follow-up.
We presented the prevalence of moderate to severe anxiety and depression symptoms in the cohort at each follow-up by vaccination status as of each follow-up between May 2021 and July 2023, a period when COVID-19 vaccines were widely available in the US. Furthermore, we examined the longitudinal relationship between symptom status at each follow-up and the number of vaccine doses received up to that point using pooled Poisson generalized estimating equation (GEE) models with an exchangeable within-subject covariance structure. The models were adjusted for age, gender, barriers to healthcare access, number of comorbidities and time elapsed since May 2021 and utilized using 10 copies of imputed data.
We performed the following sensitivity analyses: (1) To ensure that the data were collected from individuals who had been consistently engaged over a significant portion of the study period and to evaluate the robustness of our findings to the imputation procedure, we analyzed data from participants who completed at least one of the three follow-up assessments between July 2023 and December 2023, as well as at least 7 of the 14 follow-up assessments conducted between July 2020 and July 2023 (Appendix Tables S3–5). (2) To provide a more accurate estimate of the variability and ensure that findings were robust and not artefacts of a specific imputation, we utilized 10 imputed datasets to characterize ever experiencing symptoms, persistence of symptoms, and LCGA trajectories (Appendix Tables S6, 7). (3) To examine the co-occurrence of anxiety and depression symptoms, we assessed the overlap between these two conditions and analyzed the sociodemographic factors associated with experiencing (a) either persistent anxiety or persistent depression or (b) both persistent anxiety and persistent depression (Supplementary Appendix Table S9). Additionally, we investigated the associations between the co-occurrence of anxiety and depression and COVID-19 vaccine uptake (Appendix Table S10 and Appendix Figure S1).
Statistical analyses were conducted using SAS 9.4 (Cary, North Carolina, USA) using Traj package and R statistical software (version RStudio 2023.12.1 + 402) using packages gtsummary. In this study, results were considered statistically significant if the 95% confidence interval for the estimated effect did not include the null value (1 for relative measures or 0 for absolute differences).
Results
Characterizing anxiety and depression symptoms between July 2020 and July 2023: ever experienced symptoms, persistence of symptoms and LCGA trajectories
A total of 4,851 participants were eligible for inclusion in the cohort (eFigure S1), with 82.2% completing at least 13 out of 14 follow-up assessments (Appendix Table S11). Among these participants, 2,475 (51.0%, 95% CI: 49.6–52.4%) and 2,543 (52.4%, 95% CI: 51.0–53.8%) experienced moderate to severe anxiety and depression symptoms between July 2020 and July 2023, respectively (Table 1A and B ). During this period, 773 (15.9%, 95% CI: 14.9–17.0%) and 935 (19.3%, 95% CI: 18.2–20.4%) had persistent moderate to severe anxiety and depression symptoms, respectively. Trajectories for GAD-7 scores from July 2020 to July 2023 were determined and categorized as ‘persistently low’, ‘persistently lower and around 10’ and ‘persistently high’ (eFigure S2A), with 1,219 (25.1%, 95% CI: 23.9–26.4%), 2,396 (49.4%, 95% CI: 48.0–50.8%), and 1,236 (25.5%, 95% CI: 24.3–26.7%) participants assigned to each trajectory (eTable S1A). Similar trajectories were observed for PHQ-8 scores (eFigure S2B, eTable S1B).
Table 1. Sociodemographic factors comparing participants who ever vs. never experienced symptom, experiencing persistent vs. non-persistent symptom, and persistent moderate to severe anxiety symptom and depression symptoms between July 2020 and July 2023, the CHASING COVID Cohort (N = 4,851)

Comparisons between methods for characterizing persistent anxiety and depression symptoms were presented in eTable S2. Out of 4,851 participants, an additional 463 (9.5%) and 312 (6.4%) who were not identified as having persistent anxiety and depression symptoms ≥7 out of 14 follow-up assessments between July 2020 and July 2023 were classified as having persistently high GAD-7 and PHQ-8 scores by LCGA models, respectively.
Association between demographic characteristics and anxiety and depression symptoms between July 2020 and July 2023
As shown in Table 1A, participants who were younger, female or non-binary, Hispanic, without a college degree, had children <18 in household, had a household annual income <$100k, had greater barriers to healthcare, and had comorbidities were at a higher risk of experiencing moderate to severe anxiety symptoms. These same participants were also more likely to have persistent anxiety symptoms (Table 1A) and exhibit high GAD-7 trajectories (eTable S1A). Similar factors were associated with ever experiencing moderate to severe depression symptoms (Table 1B), persistent symptoms (Table 1B) and having persistently high PHQ-8 score (eTable S1B).
Association between moderate to severe anxiety and depression symptoms and COVID-19 vaccination
Following the universal availability of the COVID-19 vaccines in May 2021, there was a significantly higher prevalence of moderate to severe anxiety symptoms among unvaccinated individuals compared to individuals who received at least one dose of vaccine at each time point between May 2021 and July 2023 (Fig. 1A, eTable S3). Participants experiencing persistent moderate to severe anxiety symptoms had received a median of three doses of a vaccine (IQR: 2–4) as of July 2023, in contrast to a median of four doses (IQR: 3–4) among those without persistent anxiety symptoms (Table 2). Moreover, during the period from May 2021 to July 2023, individuals who developed moderate to severe anxiety symptoms had a 0.95 (95% CI: 0.94–0.97) times incidence rate of receiving one additional COVID-19 vaccine dose, compared to those without ongoing symptoms (Table 2). Similar findings were observed for the association between moderate to severe depression symptoms and COVID-19 vaccination (Fig. 1B, eTable S3, Table 2).

Figure 1. Cohort prevalence of moderate to severe anxiety symptoms and depression symptoms by COVID-19 vaccination status as of each follow-up, May 2021 to July 2023, the CHASING COVID Cohort (N = 4,851).
Table 2. Unadjusted and adjusted incidence rate ratio (95% CI) of ongoing moderate to severe symptoms of anxiety and depression on additional COVID-19 vaccine dose by polled GEE model, between May 2021 and July 2023, the CHASING COVID Cohort (N = 4,851)
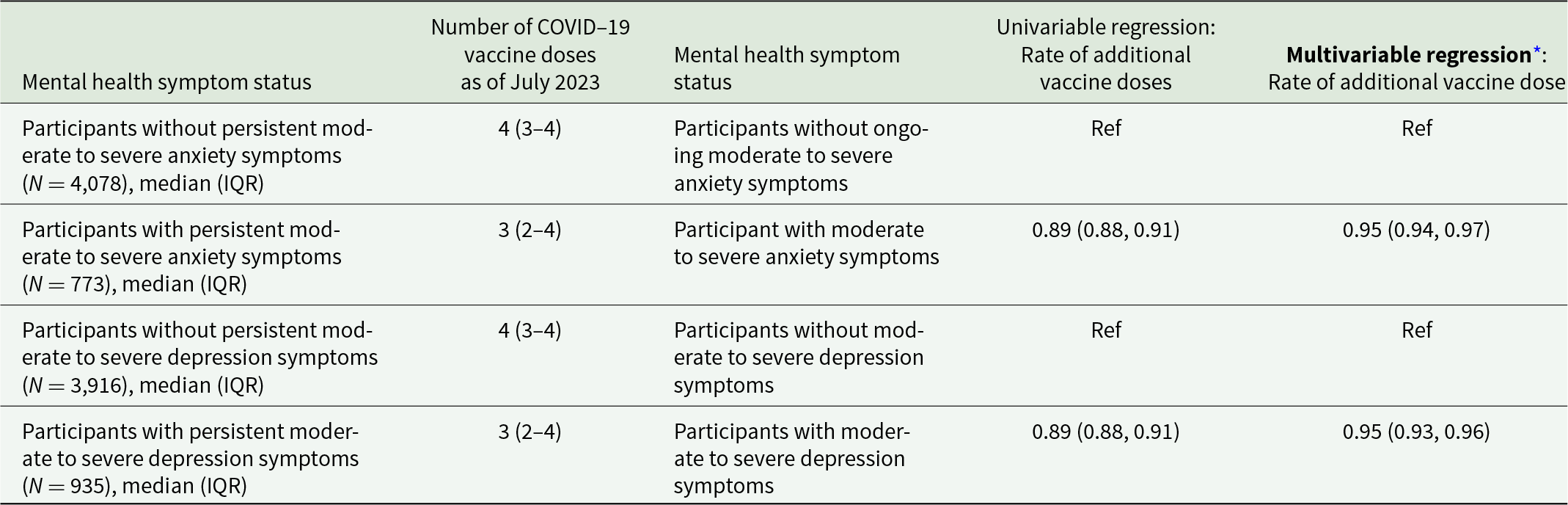
* Adjusted for age, gender, number of comorbidities and access barriers to healthcare.
Discussion
Our study was conducted within a community-based US cohort, which revealed concerning proportions of persistent anxiety and depression symptoms 3 years since the onset of the COVID-19 pandemic. Specifically, 15.9% (95% CI: 14.9–17.0%) and 19.3% (95% CI: 18.2–20.4%) of participants experienced persistent symptoms of anxiety and depression for more than half of follow-up time, respectively. Moreover, more than half of the cohort experienced anxiety and depression symptoms at some point during this period. The HPS, a national routine survey that monitored anxiety and depression symptoms using the GAD-2 and PHQ-2 tools, reported that the proportions of anxiety and depression symptoms among US adults peaked at 37.2% (95% CI: 36.3–38.2%) and 28.6% (95% CI: 27.9–29.3%) in November 2020, gradually declining to approximately 26% and 21% from May 2021 to July 2023, respectively (USAFacts, 2023b). The prevalence of post-pandemic anxiety and depression, as estimated by HPS, has significantly exceeded their pre-pandemic levels. In 2019, HPS reported that 8.1% and 6.5% of adults aged ≥18 exhibited symptoms of anxiety and depression, respectively, as measured by the GAD-2 and PHQ-2 tools (CDC, 2023b). These pre-pandemic figures were consistent with other surveys such as the National Survey on Drug Use and Health (Goodwin et al., Reference Goodwin, Dierker, Wu, Galea, Hoven and Weinberger2022, Reference Goodwin, Weinberger, Kim, Wu and Galea2020). The elevated and persistent prevalence of anxiety and depression symptoms following the onset of the COVID-19 pandemic indicated its profound impacts on mental health, extending beyond periods of isolation practices, lockdowns and social distancing.
We observed a heightened risk of persistent anxiety and depression symptoms from 2020 to 2023 among certain demographic groups. These included individuals who were younger, Hispanic, had lower educational attainment, earned an annual household income below $100k, had children <18 in the household and faced greater healthcare barriers. Additionally, individuals at higher risk of mental disorders also faced greater risk for not staying up-to-date with the COVID-19 vaccine (Saltzman et al., Reference Saltzman, Longo and Hansel2024). In the fall of 2023, it was observed that US adults who are Hispanic, those without health insurance, and individuals with incomes below the poverty line exhibited nearly half the updated vaccine uptake of White adults, a quarter of that uptake for adults with health insurance, and half of that uptake for those with income above poverty line, respectively (CDC, 2024a). In a cohort of adult patients from a large healthcare system, factors associated with not receiving a bivalent booster included younger age, Hispanic and non-Hispanic Black, having ≥1 inpatient or emergency department visits in the prior year, a history of SARS-CoV-2 infection, Medicaid insurance, and residing in neighbourhoods with high deprivation (Bruxvoort et al., Reference Bruxvoort, Sy, Hong, Lewin, Qian, Huang, Holmquist, Han and Xu2023). The co-occurrence of persistent anxiety and depression symptoms with low vaccination uptake among these demographic groups underscored the importance of prioritizing vulnerable populations bearing dual burden of mental distress and increased risk of severe COVID-19 due to low COVID-19 vaccination uptake. Therefore, it’s crucial for public health authorities to collaborate with community-based organizations, healthcare providers, and other trusted messengers to enhance vaccine confidence and expand access to hard-to-reach populations.
A comprehensive examination of the impact of anxiety and depression symptoms on the COVID-19 vaccination uptake is imperative to guide public health interventions aimed at addressing the dual challenge of elevated mental distress and low COVID-19 vaccination uptake. In our current study, participants with ongoing symptoms of anxiety and depression had a lower uptake of receiving an additional vaccine dose compared to those without such symptoms. A meta-analysis of cohort studies corroborated these findings, reported that individuals with mental health conditions tend to have lower COVID-19 vaccine uptake and increased vaccine hesitancy (Jia et al., Reference Jia, Coupland, Vinogradova, Qureshi, Turner and Vedhara2024). Among individuals with mental health conditions (e.g. anxiety and depressive disorder, alcohol and substance abuse), common barriers to vaccination included concerns about vaccine safety, effectiveness and potential side effects (Jia et al., Reference Jia, Coupland, Vinogradova, Qureshi, Turner and Vedhara2024). Using electronic health record data from a cohort of adults in the Northeastern US, it was found that individuals with anxiety disorders had a 1.45 hazard ratio (95% CI: 1.20–1.77) for vaccine hesitancy compared to those without anxiety disorders (Eyllon et al., Reference Eyllon, Dang, Barnes, Buresh, Peloquin, Hogan, Shimotsu, Sama and Nordberg2022). Furthermore, according to the estimates derived from the HPS field in 2021, individuals with symptoms of anxiety or depression were less likely to receive the COVID-19 vaccination (aPR: 0.94 [95% CI: 0.91–0.98]), but more likely to express an intention to get vaccinated (aPR: 1.13 [95% CI: 1.08–1.19]) (Nguyen et al., Reference Nguyen, Chen, Morris, Chui and Allen2022). These findings, in conjunction with our own, underscore the necessity for tailored interventions aimed at addressing anxiety and depression symptoms, while simultaneously tackling barriers to vaccine uptake.
Our study had several limitations that warranted careful considerations. First, the generalizability of our prevalence estimations to the broader US adult population might be restricted, as our cohort was not nationally representative. Compared to the broader US population, the cohort sample included a higher proportion of females compared to males, with an overrepresentation of White non-Hispanic individuals, and an underrepresentation of Black non-Hispanic and Hispanic or Latino individuals (U.S. Census Bureau, 2020). Income levels and education attainment were generally higher, suggesting a more affluent sample with more individuals holding advanced degrees. Given that our cohort tended to overrepresent individuals who were less vulnerable to anxiety and depression symptoms (e.g. non-Hispanic White individuals, those with a college education and higher income earners), there was a likelihood that the prevalence of these conditions were underestimated in our sample relative to the entire US population. Second, since our cohort participants were enrolled from March to June 2020, we lacked pre-pandemic data on anxiety and depression symptoms proportions, preventing a definitive conclusion regarding post-pandemic elevation. Next, the reliance on participants’ self-reported vaccination status could introduce misclassification and reporting bias. However, a separate study reported a 95% concordance between self-reported COVID-19 vaccine status and data obtained from vaccine registries and electronic health records (Stephenson et al., Reference Stephenson, Olson, Self, Ginde, Mohr, Gaglani, Shapiro, Gibbs, Hager, Prekker, Gong, Steingrub, Peltan, Martin, Reddy, Busse, Duggal, Wilson and Qadir2022). Additionally, the exclusion of participants who did not engage in any assessment between July 2023 and December 2023 might introduce selection bias in the estimates of the association between mental health symptoms and vaccination uptake, potentially biasing these estimates towards null. The excluded individuals likely experienced severe symptoms of anxiety and depression, which may had hindered their ability to participate in follow-up assessments. Their lack of active engagement in COVID-19 related surveys might also suggest a lower interest in the pandemic and consequently, they might be less likely to receive COVID-19 vaccines. Similarly, individuals who were opposed to COVID-19 vaccines and mitigation strategies might be underrepresented in our sample due to non-response bias. This non-response could introduce selection bias, potentially affecting the generalizability of our findings. Finally, the exposure and outcome ascertainment windows overlapped for the number of doses and exposure, which limited our ability to establish a clear temporal relationship between persistent anxiety and depression and COVID-19 vaccination. While our results suggested an association, the direction of causality could not be firmly established, and reverse causality remained a possibility.
In conclusion, we found that a significant portion of individuals in the cohort experienced persistent symptoms of anxiety and depression. Young adults, women, and those facing socio-economic difficulties might require access to mental health support. Moderate to severe anxiety and depression symptoms could potentially hinder individuals from obtaining future COVID-19 vaccinations. Further investigation is needed to determine whether providing tailored support to those with anxiety and depression symptoms could effectively remove barriers to COVID-19 vaccine uptake.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796024000763.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request. Access to the data will be provided after review and approval by the institutional review board and in accordance with relevant data privacy regulations.
Acknowledgements
The authors wish to thank the participants of the CHASING COVID Cohort Study. We are grateful to you for your contributions to the advancement of science around the COVID-19 pandemic.
Financial support
Funding for this project is provided by The National Institute of Allergy and Infectious Diseases (NIAID), award number UH3AI133675 (MPIs: D Nash and C Grov), NIMH award RF1MH132360 (MPIs: D Nash and A Parcesepe), National Institute of Child Health and Human Development grant P2C HD050924 (Carolina Population Center), Pfizer Inc., the CUNY Institute for Implementation Science in Population Health (cunyisph.org), and the COVID-19 Grant Program of the CUNY Graduate School of Public Health and Health Policy. The NIH played no role in the production of this manuscript nor necessarily endorses the findings. Pfizer Inc. played no role in the production of this manuscript nor necessarily endorsed the findings.
Competing interests
Author DN receives consulting fees from Gilead Sciences and AbbVie. All other authors have no conflicts of interest, financial or otherwise.
Ethical standards
Informed consent forms were completed in a web browser on participants’ computer or mobile device at baseline, each round of serological testing, and at periodic follow-up assessments. The study was approved by the Institutional Review Boards of the City University of New York (CUNY) Graduate School of Public Health and Health Policy (New York, NY, USA) (protocol 2020-0256).





