Introduction
Depressive disorders are of global public health concern and one of the leading causes of disability (World Health Organization, 2017). Worldwide, the overall pooled prevalence of these mental disorders has been estimated at 4.4%, with Latin America among the most affected regions (World Health Organization, 2017). Depressive disorders substantially contribute to the burden of suicide and self-harm worldwide and are significantly associated with excess mortality (Vigo et al., Reference Vigo, Thornicroft and Atun2016; Walker et al., Reference Walker, McGee and Druss2015). The recurrent and heterogeneous nature of depressive disorders and their common medical and psychiatric comorbidities define a challenging global public health concern (Cuijpers et al., Reference Cuijpers, Stringaris and Wolpert2020; Deschênes et al., Reference Deschênes, Burns and Schmitz2015; Hardeveld et al., Reference Hardeveld, Spijker, De Graaf, Nolen and Beekman2010; Hasin et al., Reference Hasin, Sarvet, Meyers, Saha, Ruan, Stohl and Grant2018; Jansen et al., Reference Jansen, van Schijndel, van Waarde and van Busschbach2018; Newton-Howes et al., Reference Newton-Howes, Tyrer and Johnson2006). Notably a high proportion of depressive disorders have been attributed to early adverse stress (Li et al., Reference Li, D’Arcy and Meng2016), a link that might have devastating clinical consequences in adulthood (Lippard & Nemeroff, Reference Lippard and Nemeroff2020).
Early adverse stress refers to a group of experiences during childhood and adolescence that leave a permanent and negative imprint on a substantial part of the exposed individuals (such as abuse, neglect, and household dysfunction). Early adverse stress is one of the most critical contributors to health-harming behaviors and many of the leading causes of diseases in adulthood (Afifi et al., Reference Afifi, Enns, Cox, Asmundson, Stein and Sareen2008; Bellis et al., Reference Bellis, Hughes, Ford, Ramos Rodriguez, Sethi and Passmore2019; Felitti et al., Reference Felitti, Anda, Nordenberg, Williamson, Spitz, Edwards, Koss and Marks1998; Merrick, Reference Merrick2019; Waehrer et al., Reference Waehrer, Miller, Marques, Oh and Harris2020), including mental disorders. The association between early adverse stress and adult depression has been comprehensively studied. A robust body of literature has found that exposure to childhood trauma confers an additional layer of complexity to depressive episodes (Dagnino et al., Reference Dagnino, Ugarte, Morales, González, Saralegui and Ehrenthal2020; Dube et al., Reference Dube, Anda, Felitti, Chapman, Williamson and Giles2001; Gaudiano & Zimmerman, Reference Gaudiano and Zimmerman2010; Gloger, Vöhringer, et al., Reference Gloger, Vöhringer, Martínez, Chacón, Cáceres, Diez de Medina, Cottin and Behn2021; Lippard & Nemeroff, Reference Lippard and Nemeroff2020; Nanni et al., Reference Nanni, Uher and Danese2012; Nelson et al., Reference Nelson, Klumparendt, Doebler and Ehring2017; Withers et al., Reference Withers, Tarasoff and Stewart2013): earlier onset of disease, chronic and recurrent course of illness, higher severity of symptoms, poor response to standard interventions, atypical features, increased risk of suicidal ideations and comorbidities.
Recent systematic reviews and meta-analyses have identified promising psychological interventions to attenuate the negative consequences of early adverse stress in adult life (Martínez, Gloger, Diez de Medina, González, Carrasco, Schilling, et al., Reference Martínez, Gloger, Diez de Medina, González, Carrasco, Schilling and Vöhringer2021; Martínez, Gloger, Diez de Medina, González, Carrasco, & Vöhringer, Reference Martínez, Gloger, Diez de Medina, González, Carrasco and Vöhringer2021). These interventions generally recognize the impact of childhood trauma on interpersonal conflicts and coping strategies in adulthood (Martínez, Gloger, Diez de Medina, González, Carrasco, Schilling, et al., Reference Martínez, Gloger, Diez de Medina, González, Carrasco, Schilling and Vöhringer2021; Martínez, Gloger, Diez de Medina, González, Carrasco, & Vöhringer, Reference Martínez, Gloger, Diez de Medina, González, Carrasco and Vöhringer2021). However, more research on the psychological mechanisms through which these traumatic experiences are associated with depression severity is needed, as they might greatly inform psychological interventions that have shown potential. For instance, Riggs (Reference Riggs2010), relying on a varied body of knowledge, hypothesizes a model in which infant and adult attachment insecurity, emotional dysregulation, negative internal working models, maladaptive coping strategies, and poor social functioning, might be affected by early adverse stress, leading to the development of psychopathology. Herein, we draw our attention to three psychological mechanisms affected by early adverse stress that, according to the literature, might have a pivotal role in depression severity: the attachment system, personality styles, and emotion regulation strategies.
The attachment system
Since Bowlby’s seminal work, it has been emphasized that early attachment relationships provide children with relatively stable representations of the self, intimate relationships, and the world (Bowlby, Reference Bowlby1980; Sroufe, Reference Sroufe1979). These representational schemas influence intimate relationships in adult life as they contribute to understanding loving and caring relationships (Riggs, Reference Riggs2010). Evidence consistently shows early adverse stress contributes to insecure attachment (Cicchetti & Toth, Reference Cicchetti and Toth2005). Developmentally, insecure attachment in childhood can disrupt peer relationships and lead to insecure attachment in adulthood (Riggs, Reference Riggs2010). Riggs (Reference Riggs2010), in an extensive theoretical and empirical review of the subject, defines three types of insecure romantic attachment: avoidant, anxious, and fearful. The avoidant style is characterized by distrust, disengagement, compulsive self-reliance, and instrumental care-seeking. In contrast, the anxious style exhibits exaggerated emotions and dependency, feelings of unworthiness, and excessive care-seeking (Riggs, Reference Riggs2010). The fearful style is a mixture of high anxiety and avoidance (Riggs, Reference Riggs2010). Studies have found mixed results regarding the role of adult attachment styles in the association between early adverse stress and adult depression. A cohort study of individuals with or without recorded childhood maltreatment and another study in low-income mothers revealed a significant role for anxious attachment style following childhood neglect (Widom et al., Reference Widom, Czaja, Kozakowski and Chauhan2018), physical abuse (Widom et al., Reference Widom, Czaja, Kozakowski and Chauhan2018), and emotional abuse (Caldwell et al., Reference Caldwell, Shaver, Li and Minzenberg2011). However, a study in acute or recovered depressed individuals reported that avoidance in close relationships jointly with emotion dysregulation and depressive attributional style, partially mediated the association between higher levels of childhood trauma and depression severity (Schierholz et al., Reference Schierholz, Krüger, Barenbrügge and Ehring2016).
Personality styles
Blatt described the dependent and the self-critical styles that would define different experiences of depression (Blatt, Reference Blatt1974, Reference Blatt2004, Reference Blatt2008). These personality styles result from a pathological fixation on a continuum of two developmental dimensions: interpersonal relationships and self-definition. Dependent individuals overemphasize feelings of loneliness and abandonment, while self-critical individuals exaggerate feelings of failure and worthlessness (Blatt, Reference Blatt1974, Reference Blatt2004, Reference Blatt2008). Interestingly, Riggs’s early mentioned theoretical and empirical synthesis of child maltreatment and the attachment system across the life cycle converges with Blatt’s framework on the etiology of dependent and self-critical depression (Blatt & Homann, Reference Blatt and Homann1992; Riggs, Reference Riggs2010). Distortions in early attachment representations can engender relatively stable negative internal working models (Blatt & Homann, Reference Blatt and Homann1992; Riggs, Reference Riggs2010), resulting in pathological personality styles. Ambivalence in early caregiving relationships may lead to overemphasis on feelings of dependency. In contrast, avoidance in attachment relationships may conduce to a self-critical fixation (Blatt & Homann, Reference Blatt and Homann1992; Dagnino et al., Reference Dagnino, Pérez, Gómez, Gloger and Krause2017; Reis & Grenyer, Reference Reis and Grenyer2002; Zuroff & Fitzpatrick, Reference Zuroff and Fitzpatrick1995). A body of research has concluded that early adverse stress might increase vulnerability to depression or related psychological problems by developing pathological personality styles, specifically self-criticism (Falgares et al., Reference Falgares, Marchetti, Manna, Musso, Oasi, Kopala-Sibley, De Santis and Verrocchio2018; Sachs-Ericsson et al., Reference Sachs-Ericsson, Verona, Joiner and Preacher2006). For instance, using a mental health survey representative of the United States, a study found that self-criticism mediated the association between verbal abuse and internalizing symptoms (e.g., depression) (Sachs-Ericsson et al., Reference Sachs-Ericsson, Verona, Joiner and Preacher2006). Relatedly, Falgares et al., found that the association between emotional neglect and abuse and suicidal risk was mediated by self-criticism in a sample of Italian higher education students (Falgares et al., Reference Falgares, Marchetti, Manna, Musso, Oasi, Kopala-Sibley, De Santis and Verrocchio2018).
Emotion regulation
Emotion regulation is the conscious or unconscious adjustment of emotional responses to environmental demands, changing the magnitude or type of emotional experiences (Aldao et al., Reference Aldao, Nolen-Hoeksema and Schweizer2010). Adaptive emotion regulation strategies include reappraisal (Gross, Reference Gross1998), problem-solving (Bell & D'Zurilla, Reference Bell and D’Zurilla2009), and acceptance (Hayes et al., Reference Hayes, Strosahl and Wilson1999). In contrast, maladaptive emotion regulation strategies include suppression (Gross, Reference Gross1998; Wenzlaff & Wegner, Reference Wenzlaff and Wegner2000), avoidance (Hayes et al., Reference Hayes, Strosahl and Wilson1999, Reference Hayes, Strosahl, Wilson, Bissett, Pistorello, Toarmino, Polusny, Dykstra, Batten, Bergan, Stewart, Zvolensky, Eifert, Bond, Forsyth, Karekla and McCurry2004), and rumination (Nolen-Hoeksema et al., Reference Nolen-Hoeksema, Wisco and Lyubomirsky2008; Watkins, Reference Watkins2008). Different emotion regulation strategies have been consistently linked to psychopathology, with rumination and avoidance robustly associated with depression (Aldao et al., Reference Aldao, Nolen-Hoeksema and Schweizer2010). Developmentally, the capacity for emotion regulation may be conceptualized as a component of the attachment system that can be seriously affected by emotionally abusive parenting, leading to severe difficulties in understanding and controlling complex emotions (Riggs, Reference Riggs2010). A few studies have been conducted on depressed patients exploring the mediating role of emotion dysregulation on the association between early adverse stress and depression (Hopfinger et al., Reference Hopfinger, Berking, Bockting and Ebert2016; Huh et al., Reference Huh, Kim, Lee and Chae2017; O'Mahen et al., Reference O’Mahen, Karl, Moberly and Fedock2015; Schierholz et al., Reference Schierholz, Krüger, Barenbrügge and Ehring2016). Although these studies have used different measurements of emotion regulation – making comparisons problematic – they have consistently stressed the critical role of these strategies (Hopfinger et al., Reference Hopfinger, Berking, Bockting and Ebert2016; Huh et al., Reference Huh, Kim, Lee and Chae2017; O'Mahen et al., Reference O’Mahen, Karl, Moberly and Fedock2015; Schierholz et al., Reference Schierholz, Krüger, Barenbrügge and Ehring2016). A single study provided evidence for a specific association between childhood trauma, emotion dysregulation, and depression: behavioral avoidance mediated the association between emotional neglect and depression, while rumination partially mediated the association between emotional abuse and depression (O'Mahen et al., Reference O’Mahen, Karl, Moberly and Fedock2015).
A hypothetical model
No empirical study has jointly explored the association between early adverse stress, the psychological mechanisms reviewed, and depression severity. We have built a simplified and hypothetical model grounded in the literature providing potential pathways for psychological mechanisms between early adverse stress and depression severity (Figure 1). Our hypothetical model proposes that the association between early adverse stress and depression severity would be fully mediated by attachment insecurity in adulthood – as an extension of attachment insecurity in childhood –, pathological personality styles, and difficulties in emotion regulation. Complementarily, pathological personality styles and difficulties in emotion regulation would partially mediate the association between attachment insecurity and depression severity. Finally, pathological personality styles and difficulties in emotion regulation would be directly associated with depression severity – that is, they would not be mediated by any other variable. Our study is a preliminary attempt at empirically testing this model in a sample of outpatients diagnosed with major depression. Owing to gaps in the literature, we were precluded from proposing more specific hypotheses a priori.

Figure 1. A simplified and hypothetical model for psychological mechanisms mediating the association between early adverse stress and depression severity.
Material and methods
Our report presents cross-sectional, secondary analyses of the baseline data from a longitudinal study entitled Profiles of depression and its relation to the therapeutic process, grant number 11170561, awarded by the Chilean National Fund for Scientific and Technological Development. The reported data came from a private research and mental health care institution in Santiago, Chile – Psicomedica, Clinical & Research Group. Psicomedica offers mental health outpatient care for middle-income urban populations.
Procedures
In Psicomedica, adults aged 18 years or older with probable depression who seek mental health care undergo a comprehensive clinical diagnostic interview with a psychiatrist or senior psychiatry resident to confirm the presence of a major depressive episode, according to the ICD-10 (World Health Organization, 1992). We recruited a convenience sample of these patients. Those agreeing to participate in the study signed an informed consent form, ensuring their confidentiality and voluntary participation. We excluded patients consulting for primary substance abuse, psychotic symptoms, cognitive dysfunction, or eating disorder based on the initial diagnostic interview. Participants answered the Patient Health Questionnaire-9 item (PHQ-9) before beginning their first psychological consultation. The other instruments: Childhood Trauma Questionnaire-Short Form, (CTQ-SF), Experience in Close Relationships Scale (ECR), Depressive Experience Questionnaire (DEQ), and Difficulties in Emotion Regulation Scale (DERS) were completed by the participants at home and returned to the researchers at the beginning of the second psychological consultation. This study was approved by the Alberto Hurtado University and Psicomedica research ethics committees.
Materials
Following a path analysis framework, we defined three variables: exogenous, endogenous mediators, and endogenous outcomes. In brief, exogenous variables do not depend on any other variables in the model, whereas endogenous models do depend on other variables included in the model (Hoyle, Reference Hoyle2012). We detail their measurement and further manipulations in this section.
Exogenous variables
The exogenous variable in our primary analyses was the compounded exposure to early adverse stress, represented by the total score of the CTQ-SF (ranging from 25 to 125 points). The CTQ-SF is a 28-item self-report scale for the comprehensive and retrospective assessment of early adverse stress in adults and adolescents (Bernstein et al., Reference Bernstein, Stein, Newcomb, Walker, Pogge, Ahluvalia, Stokes, Handelsman, Medrano, Desmond and Zule2003). It is based on the original and more extended version of the CTQ (Bernstein et al., Reference Bernstein, Fink, Handelsman, Foote, Lovejoy, Wenzel, Sapareto and Ruggiero1994). The CTQ-SF comprises five subscales assessing emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect (Bernstein et al., Reference Bernstein, Stein, Newcomb, Walker, Pogge, Ahluvalia, Stokes, Handelsman, Medrano, Desmond and Zule2003). Each subscale is represented by five items on a 5-point Likert-type scale, with responses ranging from “never” to “almost always” (Bernstein et al., Reference Bernstein, Stein, Newcomb, Walker, Pogge, Ahluvalia, Stokes, Handelsman, Medrano, Desmond and Zule2003). The five subscales have cutoff scores for different levels of exposure to early adverse stress, ranging from none to severe. The 5-dimensional factor structure, reported by Bernstein et al., has been consistently replicated in other studies (Spinhoven et al., Reference Spinhoven, Penninx, Hickendorff, van Hemert, Bernstein and Elzinga2014), including its Chilean validation (Behn et al., Reference Behn, Vöhringer, Martínez, Domínguez, González, Carrasco, Gloger, Behn, Vöhringer, Martínez, Domínguez, González, Carrasco and Gloger2020). Cronbach’s α coefficients for the subscales of the Chilean version of the CTQ-SF were: emotional abuse (.85), physical abuse (.87), sexual abuse (.93), emotional neglect (.79), and physical neglect (.41) (Behn et al., Reference Behn, Vöhringer, Martínez, Domínguez, González, Carrasco, Gloger, Behn, Vöhringer, Martínez, Domínguez, González, Carrasco and Gloger2020).
In secondary analyses, we treated the five subscales of the CTQ-SF (emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect, with scores ranging from 5 to 25 points) as exogenous variables. These secondary exogenous variables were separately tested and allowed us to gain further preliminary insights into the hypothetical associations between early adverse stress, psychological mechanisms, and depression. The sex and age of participants were included as exogenous covariates in all the analyses.
Endogenous mediator variables
The endogenous mediators were the measures of attachment insecurity as per the ECR, the pathological personality styles assessed with the DEQ, and the general difficulties in emotion regulation according to the DERS. Given the complexity of our hypothetical model (Figure 1), some of these variables intervened between two other endogenous variables. For instance, pathological personality styles were proposed to partially mediate the association between attachment insecurity and general difficulties in emotion regulation.
The ECR assesses the attachment style of individuals in their romantic relationships through 36 items, providing a solution to the heterogeneous measures of adolescent and adult romantic attachment orientations (Brennan et al., Reference Brennan, Clark and Shaver1998). In their large-scale validation study, Brennan et al., found two primary dimensions of insecure attachment: anxiety and avoidance (Brennan et al., Reference Brennan, Clark and Shaver1998). The ECR 35 items are rated on a 7-point Likert-type scale, with responses ranging from “disagree strongly” to “agree strongly” (Brennan et al., Reference Brennan, Clark and Shaver1998). The score for the ECR ranges from 35 to 245 points. The ECR has been used to measure adult attachment in Chilean samples, with reliability indexes of .84 for the anxiety scale and .83 for the avoidance scale (Guzmán & Contreras, Reference Guzmán and Contreras2012).
The DEQ is a 66-item self-report questionnaire focused on stable personality styles that would be determinant in the development of depression (Blatt et al., Reference Blatt, D’Afflitti and Quinlan1976). The original study of the DEQ yielded three orthogonal factors dependency, self-criticism, and efficacy (Blatt et al., Reference Blatt, D’Afflitti and Quinlan1976). Dependency and self-criticism are pathological personality styles, whereas efficacy reflects confidence regarding one self’s resources and capabilities (Blatt et al., Reference Blatt, D’Afflitti and Quinlan1976). The dependence factor of the DEQ investigates items referring to external interpersonal relationships. It contains themes such as abandonment, loneliness, helplessness, desires for attachment, closeness, dependence, preoccupation with rejecting, harming, and offending others, and difficulties handling aggression due to fear of loss. The second factor, self-criticism, consists of items related to internal relationships. It reflects guilt, emptiness, hopelessness, dissatisfaction, insecurity, fear of failure in the face of very high expectations and standards, and lack of capacity to assume responsibilities. The DEQ items are rated on a 7-point Likert-type scale, with responses ranging from “strongly disagree” to “strongly agree.” The range score of the DEQ goes from 66 to 462 points. The calculation of the subscales includes all items, and what changes between scales is the weight each item receives. The higher the score, the higher the presence of the corresponding factor. We used the Chilean adaptation of the DEQ by Rost and Dagnino (Reference Rost and Dagnino2011), which showed good internal consistency indices ranging from .66 to .89.
The DERS is a 36-item self-report questionnaire derived from a multidimensional conceptualization of emotion regulation (Gratz & Roemer, Reference Gratz and Roemer2004). The DERS measures the following interrelated dimensions in which difficulties in emotion regulation may occur: lack of awareness of emotional responses, lack of clarity of emotional responses, nonacceptance of emotional responses, limited access to emotion regulation strategies perceived as effective, difficulties controlling impulses when experiencing negative emotions, and difficulties engaging in goal-directed behaviors when experiencing negative emotions (Gratz & Roemer, Reference Gratz and Roemer2004). The DERS items are scored on a 5-point scale ranging from 1 “almost never” to 5 “almost always,” with higher scores indicating greater difficulties in emotion regulation (Gratz & Roemer, Reference Gratz and Roemer2004). We used the Chilean adaptation of the DERS by Guzmán-González et al. (Reference Guzmán-González, Trabucco, Urzúa M, Garrido and Leiva2014), which showed internal consistency indices ranging from 0.73 to 0.91. Keeping in mind the preliminary nature of our study, we did not analyze the six DERS subscales
Endogenous outcome variable
The endogenous outcome in our model was the severity of depressive symptoms assessed through the PHQ-9. The PHQ-9 is a widely employed nine-item questionnaire based on the DSM-IV, criteria for depressive episodes (Kroenke et al., Reference Kroenke, Spitzer and Williams2001). Each item is scored on a 4-point Likert-type scale, where higher scores represent higher symptom duration. The PHQ-9 has the following severity classification: no depression (0 to 4 points), mild depression (5 to 9 points), moderate depression (10 to 14 points), moderately severe depression (15 to 19 points), and severe depression (20 or more points) (Kroenke et al., Reference Kroenke, Spitzer and Williams2001). The validation study of the PHQ-9 found that a cutoff score of 10 points or more had a sensitivity and specificity of 88% for major depression (Kroenke et al., Reference Kroenke, Spitzer and Williams2001). A Spanish version of this instrument has been validated in the Chilean primary care population (Baader et al., Reference Baader M, Molina F, Venezian B, Rojas C, Farías S, Fierro-Freixenet, Backenstrass and Mundt2012).
Data analysis
We presented means and standard deviations (SD) for continuous variables and frequencies with percentages for categorical variables to describe our data. After data exploration, we noted a high proportion of missingness. Missing data ranged from 9.6% (sex) to 41.6% (the CTQ-SF subscale of emotional abuse). The extension of missingness made path analyses via the standard maximum likelihood estimation highly problematic. Such an estimation method would exclude an entire observation from calculations if a single value were missing (i.e., listwise deletion), being approximately unbiased under the untenable assumption of missing completely at random (Hoyle, Reference Hoyle2012). Instead, we relied on the full-information maximum likelihood (FIML) method to use all the available data. The FIML method is based on the assumption of missing at random – where missingness may be related to any other variable (included or not in our model) – and multivariate normality (Hoyle, Reference Hoyle2012).
After data exploration, we tested and confirmed the assumptions for our path model (Hoyle, Reference Hoyle2012). The normality of residuals was checked through visual observation of quantile-normal plots, and linearity was verified by plotting standardized residuals against predictor variables. The variance inflation factor was computed to establish the absence of multicollinearity with a mean variance inflation factor of 1.73. Finally, we demonstrated the multivariate normality of the endogenous variables using the Doornik-Hansen test (p > .1).
The FIML method was implemented through the maximum likelihood with missing values estimation procedure. Estimations with FIML were compared for consistency with the standard method to add confidence to our findings. Fit indices were computed, and R 2 was calculated to measure explained variance in the endogenous variables. We report standardized coefficients for direct, indirect, and total effects with corresponding 95% bias-corrected confidence intervals calculated by bootstrap resampling with 200 repetitions. These analyses were assisted by Stata 16.0.
Results
Sample characteristics
The total sample size for the study was 178 patients. Patients had a mean age of 36.9 years (SD = 13.7, range 18 to 74 years), and most identified themselves as females (69.6%). The mean total score for the CTQ-SF was 50.0 points (SD = 18.3). As per the CTQ-SF subscales, exposure to severe emotional abuse was considerably reported in the sample (36.5%), compared to severe physical abuse, sexual abuse, and emotional neglect, each referred by around 17%. Severe forms of physical neglect were reported only by 7.6% of the patients. Regarding the assessment of attachment insecurity (ECR scores), the sample tended towards avoidant (4.2 points, SD = 1.1) than anxious attachment (3.2, SD = 0.9). As for pathological personality styles (DEQ scores), the sample presented more self-criticism (0.7 points, SD = 0.9) than dependency (-0.1, SD = 0.9). The evaluation of difficulties in emotion regulation yielded an overall score of 113.9 (SD = 28.0) in the DERS, consistent with greater emotion dysregulation observed in clinical samples (Bjureberg et al., Reference Bjureberg, Ljótsson, Tull, Hedman, Sahlin, Lundh, Bjärehed, DiLillo, Messman-Moore, Gumpert and Gratz2016). Concerning the evaluation of depression severity, the mean PHQ-9 score was 17.8 (SD = 5.9) points. Nearly half of the patients were classified as severely depressed by the PHQ-9 (46.7%). Further details for the sample characteristics are reported in Table 1.
Table 1. Study sample characteristics

Notes. Data are mean and standard deviation for age, PHQ-9 scores, and the following classes of variables: early adverse stress, attachment insecurity, pathological personality styles, and difficulties in emotion regulation. Data are frequency and percentages otherwise. Depression severity levels are based on the PHQ-9. Our threshold score for the CTQ-SF was derived from the five CTQ-SF subscales. In our threshold score, individuals are assigned a point per CTQ-SF subscale falling into moderate or severe levels of exposure to early adverse stress.
SD: standard deviation; n: frequency; %: percentage; CTQ-SF: Childhood Trauma Questionnaire, Short Form; ECR: Experiences in Close Relationships; DEQ: Depressive Experience Questionnaire; DERS: Difficulties in Emotion Regulation Scale; PHQ-9: Patient Health Questionnaire-9 Items.
Testing of the hypothesized model
The results revealed that our hypothesized model tested no worse than a saturated model (χ2(2) = 2.738, p = .254). The root mean square error of approximation indicates a close-fitting model (root mean square error of approximation = .048, p = .387). The Tucker–Lewis and Comparative Fit indexes suggest a good overall fit to the data (Tucker–Lewis index = .955 and comparative fit index = 0.997, respectively).
In what follows, Table 2 depicts the detailed standardized effects (direct, indirect, and total) of the association between early adverse stress, the psychological mechanisms under study, and depression severity. We also provide a written description of the variance for each endogenous variable in the model (mediators and outcomes) and the statistically significant effects found. Finally, the statistically significant standardized direct effects from our model, after adjustment by sex and age, are summarized in Figure 2.

Figure 2. Direct effects for early adverse stress and psychological mechanisms associated with depression severity. Notes. Data presented are statistically significant standardized direct effects based on 95% bias-corrected confidence intervals. Model adjusted by sex and age (exogenous covariates). Early adverse stress was measured with the Childhood Trauma Questionnaire, Short Form. Avoidance and anxiety (attachment insecurity) were assessed with the Experiences in Close Relationships scale. Self-criticism and dependency (pathological personality styles) were evaluated with the Depressive Experience Questionnaire. Difficulties in emotion regulation were measured with the Difficulties in Emotion Regulation Scale. Depression severity was assessed with the Patient Health Questionnaire-9 Items.
Table 2. Standardized effects for the association between early adverse stress, psychological mechanisms, and depression severity (N = 164)
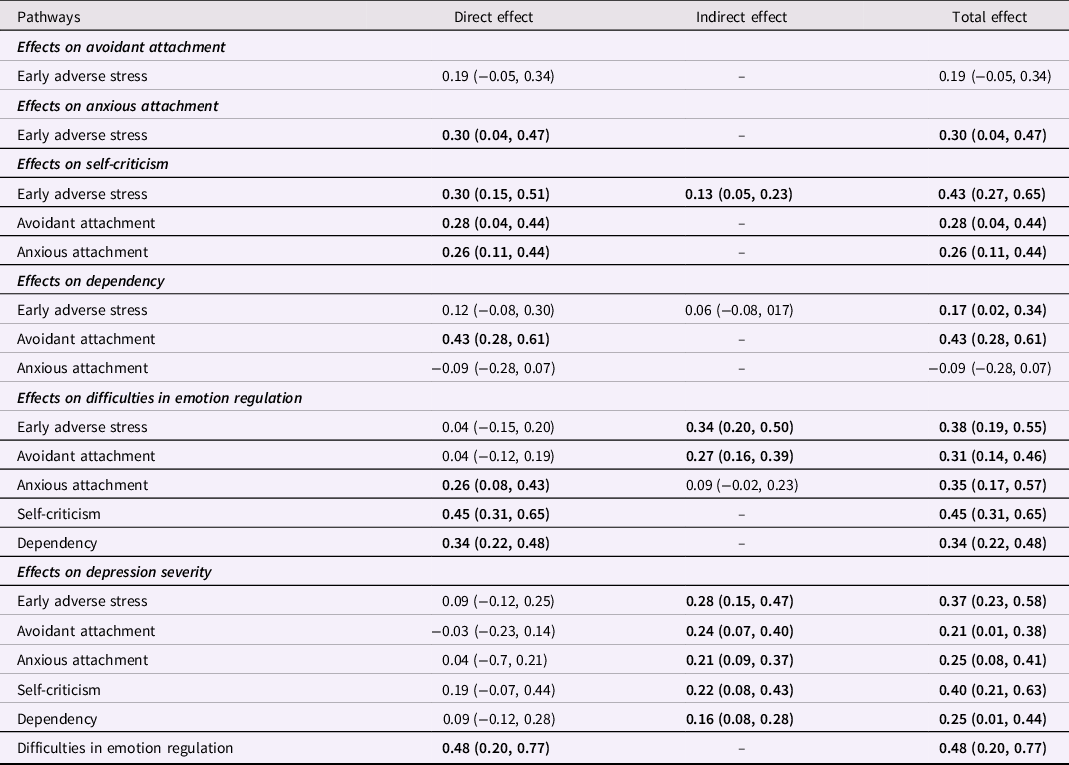
Notes. Data are standardized coefficients and their 95% bias-corrected confidence intervals. Model adjusted by sex and age (exogenous covariates). Statistically significant standardized effects are printed in bold. Early adverse stress was measured with the Childhood Trauma Questionnaire, Short Form. Avoidant and anxious attachment (attachment insecurity) were assessed with the Experiences in Close Relationships scale. Self-criticism and dependency (pathological personality styles) were evaluated with the Depressive Experience Questionnaire. Difficulties in emotion regulation were measured with the Difficulties in Emotion Regulation Scale. Depression severity was assessed with the Patient Health Questionnaire-9 Items.
As for attachment insecurity, our model explained 10.2% and 3.7% of the variance in anxious and avoidant attachment, respectively. Early adverse stress was statistically significantly associated with anxious attachment (β = 0.30, 95% bias-corrected confidence interval 0.04 to 0.47) but not with avoidant attachment (direct effects only). In summary, early adverse stress directly influenced anxious attachment.
Regarding pathological personality styles, the variance explained in our model was 42.8% for self-criticism and 26.4% for dependence. The direct effects of early adverse stress (β = 0.30, 95% bias-corrected confidence interval 0.15 to 0.51), avoidant attachment (β = 0.28, 95% bias-corrected confidence interval 0.04 to 0.44), and anxious attachment (β = 0.26, 95% bias-corrected confidence interval 0.11 to 0.44) on self-criticism were statistically significant. There was a statistically significant indirect effect of early adverse stress on self-criticism (β = 0.13, 95% bias-corrected confidence interval 0.05 to 0.23). The avoidant attachment was the only variable with a statistically significant and direct association with dependency (β = 0.43, 95% bias-corrected confidence interval 0.28 to 0.61). In summary, the effect of early adverse stress on self-criticism was partially mediated by attachment insecurity (i.e., both avoidant and anxious attachment styles), whereas only avoidant attachment was associated with dependency.
Our model explained 60.2% of the variance in difficulties in emotion regulation. The direct effects of anxious attachment (β = 0.26, 95% bias-corrected confidence interval 0.08 to 0.43), self-criticism (β = 0.45, 95% bias-corrected confidence interval 0.31 to 0.65), and dependency (β = 0.34, 95% bias-corrected confidence interval 0.22 to 0.48) on difficulties in emotion regulation were statistically significant. Whereas early adverse stress (β = 0.34, 95% bias-corrected confidence interval 0.20 to 0.50) and avoidant attachment (β = 0.27, 95% bias-corrected confidence interval 0.16 to 0.39) had statistically significant indirect effects on difficulties in emotion regulation. In summary, anxious attachment and pathological personality styles (i.e., dependency and self-criticism) were directly associated with difficulties in emotion regulation. In contrast, these variables fully mediated the effects of early adverse stress and avoidant attachment on difficulties in emotion regulation.
Finally, the variance explained in our model was 47.2% for depression severity. The only variable having a statistically significant direct effect on the severity of depressive symptoms was difficulties in emotion regulation (β = 0.48, 95% bias-corrected confidence interval 0.20 to 0.77). The indirect effects of early adverse stress (β = 0.28, 95% bias-corrected confidence interval 0.15 to 0.47), avoidant attachment (β = 0.24, 95% bias-corrected confidence interval 0.07 to 0.40), anxious attachment (β = 0.21, 95% bias-corrected confidence interval 0.09 to 0.37), self-criticism (β = 0.22, 95% bias-corrected confidence interval 0.08 to 0.43), and dependency (β = 0.16, 95% bias-corrected confidence interval 0.08 to 0.28) on depression severity, were statistically significant. In summary, difficulties in emotion regulation directly influenced depression severity, fully mediating the effects of early adverse stress, attachment insecurity, and pathological personality styles.
Standardized coefficients computed through the standard method were consistent with the estimations produced by the FIML method with overlapping 95% bias-corrected confidence intervals. The fit indices for our model and the comparison between estimation methods add confidence to the findings.
Discussion
In our pilot, cross-sectional and retrospective exploration of a sample of outpatients with major depression, we found that anxious attachment in adulthood and self-criticism mediated the association between early adverse stress and depression severity through their effects on difficulties in emotion regulation. In contrast, early adverse stress was not associated with avoidant attachment in adulthood or dependency, although the latter variables were indirectly associated with depression severity. We observed that difficulties in emotion regulation might play a pivotal role in explaining the severity of depressive symptoms, mediating the effects of all the preceding variables (including early adverse stress) and being the exclusive variable directly affecting depression severity.
Our results are preliminary but coherent with previous studies highlighting the relevance of anxious attachment in adulthood as a mediator for the association between early adverse stress and depression severity (Caldwell et al., Reference Caldwell, Shaver, Li and Minzenberg2011; Widom et al., Reference Widom, Czaja, Kozakowski and Chauhan2018). Abusive and neglectful parenting contributes to developing negative representations of the self (Hankin, Reference Hankin2005; Riggs, Reference Riggs2010). These negative internal working models (e.g., feelings of unworthiness) are typical in individuals with anxious attachment in adulthood (Caldwell et al., Reference Caldwell, Shaver, Li and Minzenberg2011), who also suffer from cognitive rumination and intense negative affect (Caldwell et al., Reference Caldwell, Shaver, Li and Minzenberg2011; Caldwell & Shaver, Reference Caldwell and Shaver2012; Mikulincer et al., Reference Mikulincer, Shaver and Pereg2003; Riggs, Reference Riggs2010), predisposing them to depression. Some of the characteristics of adults with anxious attachment, such as exaggerated emotions, dependency, and excessive care-seeking (Riggs, Reference Riggs2010), may expose them to future adverse life events, furthering their risk of elevated depressive symptoms (Hankin, Reference Hankin2005).
We could replicate a consistently observed finding: that self-criticism mediates the association between childhood maltreatment and psychopathology (specifically, internalizing symptoms and suicide-related behaviors) (Falgares et al., Reference Falgares, Marchetti, Manna, Musso, Oasi, Kopala-Sibley, De Santis and Verrocchio2018; Sachs-Ericsson et al., Reference Sachs-Ericsson, Verona, Joiner and Preacher2006). Experiences of hostility, humiliation, and rejection in parenting are a prominent risk factor for the development of a self-critical stance, as these maladaptive parenting behaviors directly provide children with negative representations of themselves (Campos et al., Reference Campos, Besser and Blatt2013; Falgares et al., Reference Falgares, Marchetti, Manna, Musso, Oasi, Kopala-Sibley, De Santis and Verrocchio2018; Lassri & Shahar, Reference Lassri and Shahar2012; Sachs-Ericsson et al., Reference Sachs-Ericsson, Verona, Joiner and Preacher2006). In turn, the core features of self-criticism, such as feelings of worthlessness, guilt, and a sense of failure (Blatt, Reference Blatt1974, Reference Blatt2004), related to maladaptive beliefs of the self, others, and the world, are serious risk factors for depression (Phillips et al., Reference Phillips, Hine and Thorsteinsson2010). Interestingly, some studies mentioned above have found that depressive symptoms directly mediate the relationship between self-criticism and suicide-related behaviors (Campos et al., Reference Campos, Besser and Blatt2013). The shared negative internal working models would explain the linkages between anxious attachment and self-criticism reported in our study (Blatt, Reference Blatt1974, Reference Blatt2004; Riggs, Reference Riggs2010).
The relevance of difficulties in emotion regulation as a critical psychological mechanism in the association of early adverse stress and depression severity is backed by a substantive body of empirical studies (Crow et al., Reference Crow, Cross, Powers and Bradley2014; Hopfinger et al., Reference Hopfinger, Berking, Bockting and Ebert2016; Huh et al., Reference Huh, Kim, Lee and Chae2017; O'Mahen et al., Reference O’Mahen, Karl, Moberly and Fedock2015; Raes & Hermans, Reference Raes and Hermans2008; Schierholz et al., Reference Schierholz, Krüger, Barenbrügge and Ehring2016; Spasojević & Alloy, Reference Spasojević and Alloy2002). Emotional abuse has been linked to the development of difficulties in emotion regulation, explicitly contributing to rumination and avoidance (Crow et al., Reference Crow, Cross, Powers and Bradley2014; Hopfinger et al., Reference Hopfinger, Berking, Bockting and Ebert2016; O'Mahen et al., Reference O’Mahen, Karl, Moberly and Fedock2015; Raes & Hermans, Reference Raes and Hermans2008; Spasojević & Alloy, Reference Spasojević and Alloy2002), which seem to play a central role in the etiology, maintenance, and severity of depression (Aldao et al., Reference Aldao, Nolen-Hoeksema and Schweizer2010; Visted et al., Reference Visted, Vøllestad, Nielsen and Schanche2018). Therefore, conceptualizing difficulties in emotion regulation as a proximal risk factor for depression severity or a fundamental feature of the depressive experience could explain its role as a pivotal mediator among all the psychological mechanisms studied.
Developmentally, adopting maladaptive emotion regulation strategies can be traced back to early adverse stress. Abusive parental behaviors elicit prolonged and dysregulated activation of the fight-or-flight mechanism; in turn, the resulting chronic arousal severely impairs children’s ability to experience and effectively regulate emotions consciously (Davies et al., Reference Davies, Winter and Cicchetti2006; Riggs, Reference Riggs2010). As a long-term consequence of child abuse and neglect, a limited sense of mastery or an environment perceived as threatening, with its accompanying intense negative emotions, might force individuals to retreat into nonconstructive and negative pondering (i.e., rumination) or to show an active unwillingness toward psychological experiences (i.e., avoidance) (Hopfinger et al., Reference Hopfinger, Berking, Bockting and Ebert2016; Huh et al., Reference Huh, Kim, Lee and Chae2017; Raes & Hermans, Reference Raes and Hermans2008; Spasojević & Alloy, Reference Spasojević and Alloy2002). The compounded action of maladaptive beliefs and difficulties in emotion regulation might contribute to a vicious cycle that furthers the risk of higher symptoms of depression (Huh et al., Reference Huh, Kim, Lee and Chae2017).
Although some studies conferred a role to adult avoidant attachment in the association between early adverse stress and more severe depression (Schierholz et al., Reference Schierholz, Krüger, Barenbrügge and Ehring2016), our study did not align with these findings. Caldwell et al. (Reference Caldwell, Shaver, Li and Minzenberg2011) stress that avoidant attachment, in contrast to anxious attachment, is not constituted by negative representations of the self or by consciously experiencing intense negative affect, offering a plausible reason for this null finding. Complementarily, we could not find the developmental linkages between adult avoidant attachment and self-criticism suggested in the literature (Blatt & Homann, Reference Blatt and Homann1992; Reis & Grenyer, Reference Reis and Grenyer2002; Zuroff & Fitzpatrick, Reference Zuroff and Fitzpatrick1995). On the contrary, we evidenced an association between anxious attachment and self-criticism, most likely tied to intense feelings of worthlessness common to attachment and personality styles (Blatt, Reference Blatt1974, Reference Blatt2004; Riggs, Reference Riggs2010).
Among the limitations of our study is the small sample size; such limitation decreases statistical power and the chances of detecting a true effect. Furthermore, testing a causal model with a cross-sectional design using retrospective measurements is a significant weakness in our study. Along the same line, using self-report instruments in conjunction with retrospective data collection may be susceptible to recall bias. However, we believe that our pilot study can serve as a proof of concept for future prospective studies. We are confident in the interim usefulness of our results because they were robust to different estimation methods, are theoretically plausible, and are consistent with the empirical literature.
We are not aware of another study that has simultaneously incorporated the variables considered in our pilot exploration. The integrative model we have proposed and empirically evaluated may extend the knowledge about the psychological mechanisms leading to more severe depression in adults exposed to early adverse stress. Our focus on severely depressed outpatients may increase the clinical relevance of our findings for this complex to treat population and promote the development of psychological interventions focused on early adverse stress (Gloger, Martínez et al., Reference Gloger, Martínez, Behn, Chacón, Cottin, Diez de Medina and Vöhringer2021). Notably, the central role of difficulties in emotional regulation should be considered in clinical practice with depressed adults exposed to early adverse stress.
Future studies should consider longitudinal designs with adequate sample sizes and evaluate the specific contribution of different types of early adverse stress and facets of emotional regulation difficulties. Other relevant mediators, both psychological and biological, should be incorporated to contribute to the development of psychological, pharmacological, and combined interventions. Forthcoming studies may expand our findings to other populations.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgements
The authors would like to thank Psicomedica, Clinical & Research Group’s administrative personnel, health providers, and patients.
Funding statement
Pablo Martínez and Paula Dagnino received support from the ANID – Millennium Science Initiative Program/Millennium Institute for Research on Depression and Personality-MIDAP ICS13_005. Additionally, Pablo Martínez was supported by the ANID – Millennium Science Initiative Program – NCS17_035. Paula Dagnino also received support from ANID/CONICYT Project No. 11170561. The supporting institutions had no role in the design and conduct of the study; analysis and interpretation of the data; or decision to submit the manuscript for publication.
Competing interests
None.







