Disclaimer: The views expressed in this publication are those of invited contributors and not necessarily those of the Institute and Faculty of Actuaries. The Institute and Faculty of Actuaries do not endorse any of the views stated, nor any claims or representations made in this publication and accept no responsibility or liability to any person for loss or damage suffered as a consequence of their placing reliance upon any view, claim or representation made in this publication. The information and expressions of opinion contained in this publication are not intended to be a comprehensive study, nor to provide actuarial advice or advice of any nature and should not be treated as a substitute for specific advice concerning individual situations. On no account may any part of this publication be reproduced without the written permission of the Institute and Faculty of Actuaries.
1. Introduction
The imperative for holistic healthcare management, encompassing early detection, proactive primary care, and integrated hospital and post-hospital support, is undeniable. Fragmented healthcare systems globally, particularly in India’s complex landscape of public and private schemes, lead to suboptimal patient outcomes and rising costs. This paper presents a pioneering programme within India’s organised corporate sector, a strategic source of data on behavioural change and health.
Traditionally, Indian corporations have emphasised inpatient (IPD) insurance, neglecting the essential role of primary care (OPD). Through collaborative engagement with corporations, HR leaders, insurers, and health technology companies, we identified a critical need to enhance OPD access via an innovative, insurance-led model. By aligning stakeholder objectives around employee benefits, we generated data-driven insights to facilitate a paradigm shift: inverting the traditional healthcare pyramid by prioritising robust primary care as the foundation, followed by appropriate IPD. This shift is crucial to alleviate the strain on secondary and tertiary care facilities and establish a more sustainable, cost-effective healthcare delivery system.
This study examines the synergistic relationship between robust outpatient (OPD) platforms, strategically funded by insurance investments, and their impact on inpatient (IPD) utilisation. We hypothesised that improved and consistent access to high-quality OPD care would lead to earlier disease detection and more effective management, thereby reducing the frequency and duration of hospital stays, and subsequently lowering costs. Our programme’s evidence-based findings support this hypothesis, demonstrating a crucial synergy. Specifically, we observed a 7% improvement in workforce productivity, directly attributable to an 11% reduction in hospitalisation days among employees utilising OPD benefits compared to those who did not. While we noted an initial increase in the incidence of IPD claims due to earlier interventions, the severity and cost per claim decreased by 13% for OPD users, resulting in an overall 9% cost saving on the IPD programme through strategic investment in OPD insurance programmes.
Furthermore, this research explores the transformative role of Artificial Intelligence (AI) and Machine Learning (ML) in proactively influencing individual patient behaviour through personalised nudges and interventions, and in creating dynamic, personalised health and wellness indices. We analyse the potential applications of these indices to support various societal needs, such as streamlined pre-approval processes for personal loans and more accurate pre-underwriting assessments for health and life insurance products, highlighting the broader economic and social implications of this integrated healthcare model. Our findings provide a compelling argument for a fundamental restructuring of healthcare delivery within the Indian corporate sector, emphasising the pivotal role of primary care within a synergistic, insurance-driven framework that benefits both individuals and the healthcare system as a whole. We conclude by outlining key recommendations for implementing and scaling this model across diverse corporate settings.
2. Methodology
This study employs a mixed-methods approach, which is a research strategy that integrates both quantitative and qualitative data to provide a more holistic understanding of the integration of outpatient and inpatient care. By combining these two methodologies, the study aims to capture a comprehensive view of how these care models interact and affect patient outcomes, healthcare utilisation, and costs. The methodology consists of several key components:
-
Quantitative data: We collected data from 300 organisations offering company-sponsored outpatient care and inpatient hospitalisation insurance policies to their employees in India. The data spans three renewal periods from 2021 to 2024, focusing on healthcare utilisation patterns, patient outcomes, and cost implications.
-
Healthcare utilisation patterns: This involves examining how often employees utilise outpatient services compared to inpatient services, identifying trends in service usage, and understanding the factors that influence these patterns using descriptive statistics.
-
Patient outcomes: The study assesses the health outcomes of patients who engage with both outpatient and inpatient services, looking at metrics such as hospital length of stay, claim incidence and severity of ailment.
-
Cost implications: An analysis of the financial aspects of care integration is conducted, including the costs associated with outpatient visits versus inpatient stays, and how these costs impact both the organisations providing insurance and the employees utilising the services.
-
Qualitative analysis: Surveys and interviews were conducted with 6 healthcare providers and 8 insurance providers to gather insights on the effectiveness of integrated care models. The qualitative data were used to identify common perceptions and experiences related to outpatient and inpatient care.
3. Literature Review
The integration of outpatient and inpatient care has been a topic of interest in health policy research for several decades. A review of the literature reveals several key themes:
-
Importance of coordination: Effective coordination between outpatient and inpatient services is essential for improving patient outcomes. Berry-Millett and Bodenheimer (Reference Berry-Millett and Bodenheimer2009) emphasise that coordinated care can lead to better management of chronic conditions and reduced hospital admissions.
-
Cost implications: Research indicates that integrated care models can result in significant cost savings. Schurrer et al. (Reference Schurrer, O’Malley, Wilson, McCall and Jain2017) found that organisations implementing coordinated care strategies experienced lower overall healthcare expenditures due to reduced hospitalisations and emergency department visits.
-
Patient-centred care: The shift towards patient-centred care highlights the need for seamless transitions between outpatient and inpatient services. Studies show that patients who receive coordinated care report higher satisfaction levels and better health outcomes (Bodenheimer, Reference Bodenheimer2008).
-
Barriers to integration: Despite the benefits, several barriers hinder the effective integration of outpatient and inpatient care. These include misaligned incentives, lack of communication between providers, and fragmented healthcare systems (Bodenheimer & Pham, Reference Bodenheimer and Pham2010).
-
Risk prediction for Cardiovascular disease (CVD): By analysing data from the Framingham Heart Study, Pencina et al. (Reference Pencina, D’Agostino, Larson, Massaro and Vasan2009) has created a model that estimates an individual’s risk of developing CVD over a 30-year period. This predictive capability is crucial for clinicians, enabling them to stratify patients based on their risk levels and tailor interventions accordingly.
-
Blood pressure prediction using machine learning: Golino et al. (Reference Golino, de Brito Amaral, Duarte, Gomes, de Jesus Soares, dos Reis and Santos2014) underscore the potential of machine learning techniques to revolutionise blood pressure prediction and management. By leveraging advanced algorithms and large datasets, healthcare providers can enhance the accuracy of BP assessments and develop personalised treatment strategies.
4. Results
4.1. Integrating Outpatient and Inpatient Care: Revolutionising Workforce Health Management
The last two years have witnessed a significant shift in how India Inc. approach Outpatient Department (OPD) coverage for their employees.
Improved employee wellbeing and productivity is one of the key objectives for organisations to offer OPD Insurance solutions. We saw that nearly half of the organisations offered OPD benefits, but mainly through self-funded models, and with a fragmented approach. Designing an appropriate funding mechanism became a critical ask with a clear need to re-allocate the sporadic benefits spend into a single structured OPD Insurance framework.
Introducing OPD insurance adds value to both the employees and the organisation. Employee retention, competitive edge and return on investment through timely health risk management are a few of the many advantages a well-curated OPD Insurance Program brings to the table.
The advantage of doing so is two-fold: for employees, it is an additional offering to the employee benefits package; for organisations, they now have a defined budget and visibility on the utilisation patterns and employee health risk.
Today, more than 1 in 3 organisations offer OPD insurance to their employees, representing a substantial increase towards insured programmes.
OPD Insurance is being looked at as the first port of call for all healthcare needs. It is being considered not just from an insurance perspective, but organisations are looking at it as an integrated health and wellbeing solution, focusing on the overall health of an individual. It encompasses a wide range of services, including preventive care such as health checks and vaccines, doctor consultation and diagnostic testing, and management of chronic diseases.
When it comes to designing a robust OPD Insurance Program, certain pre-requisites are particularly important. Most corporates felt a need for a wider cashless OPD network, preferably with their existing insurer. For a successful programme, communication and employee awareness is key. Customisation of products, lower operational and administrative challenges and appropriate budgeting are some of the other ways to make the OPD Insurance Program sustainable in the long-term.
4.2. Benefit Wise Utilisation
The success of any OPD programme depends on employee awareness and utilisation. The data depicts a positive picture, with a substantial 61% of unique employees availing of one or more OPD benefits. This high number signifies a strong level of awareness and active engagement amongst the workforce.
To understand how employees are leveraging OPD offerings, we analysed utilisation patterns across various services covered under OPD insurance programmes (see Figure 1). The way the services are being utilised also showcases an ideal patient journey for any individual. The journey starts from a preventive care solution through annual health checks, followed by doctor consultation on the findings of the health check report with additional diagnostic tests being recommended and medications. The journey is also essentially starting from consulting a doctor for any health condition one may have and continue the cycle.
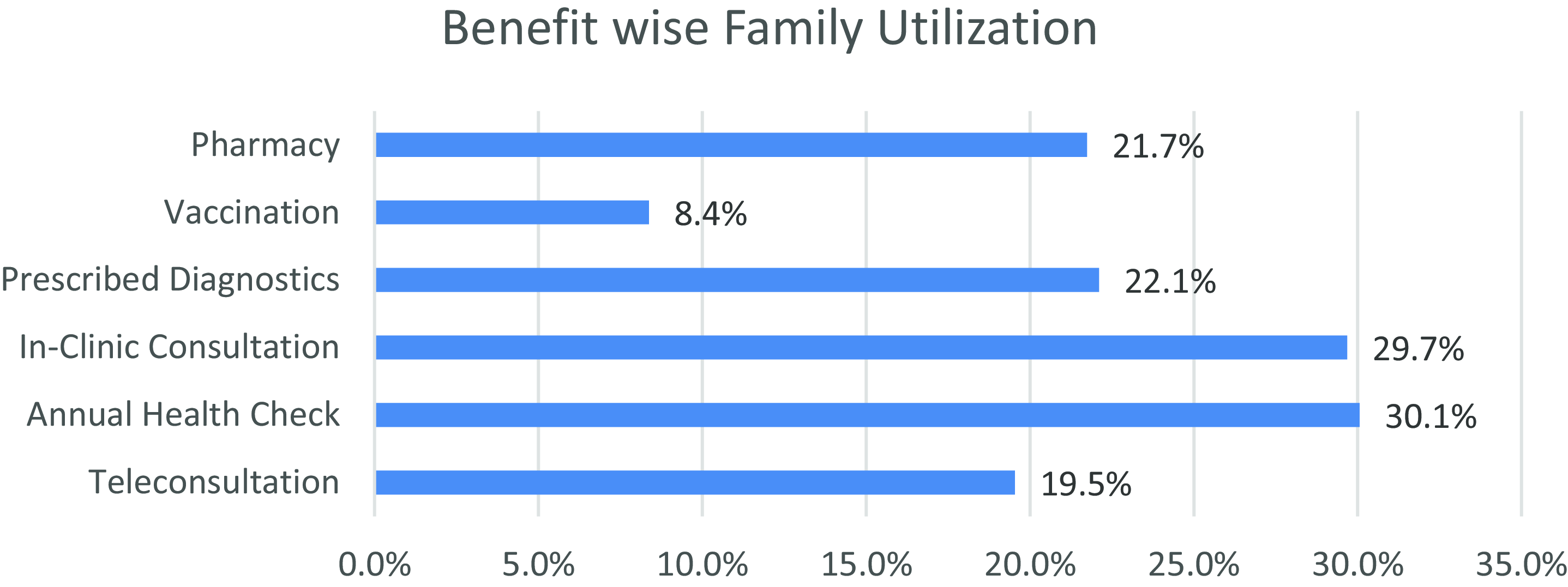
Figure 1. Benefit wise family utilisation.
Based on the mix of claims counts (see Figure 2), we see that 1 in 2 doctor consultations leads to a prescribed diagnostic test and almost every doctor consultation results in a prescribed pharmacy.
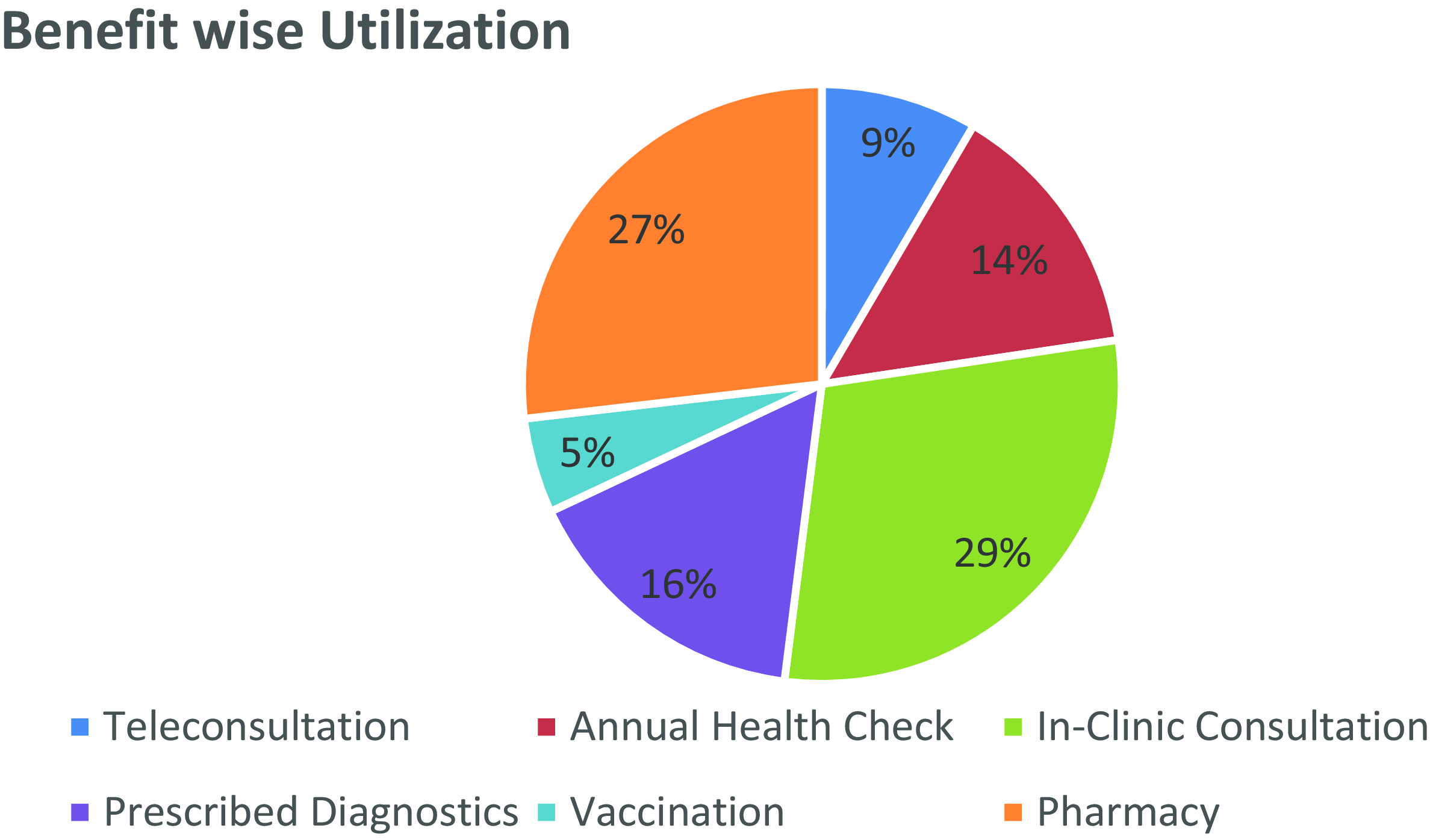
Figure 2. Benefit-wise utilisation in terms of claims count.
4.3. Findings
The role of outpatient care in reducing hospitalisations cannot be overstated. By providing timely interventions and ongoing management, outpatient services can prevent the escalation of health issues that may require hospitalisation.
Inpatient care is critical for managing acute health conditions that necessitate intensive medical attention. Hospitals provide essential services such as surgeries, emergency care, and specialised treatments that cannot be delivered in an outpatient setting. However, the high costs associated with inpatient care underscore the need for effective management and prevention strategies to minimise unnecessary admissions.
The analysis bifurcates the IPD claims data into two cohorts: IPD claims experience for those who have availed themselves of OPD benefits and IPD claims experience for those who have not availed themselves of OPD benefits.
This analysis excludes maternity, COVID and cataract claims.
The findings present various statistics that illustrate the positive effects of utilising outpatient services on inpatient hospitalisation, employee health and organisational costs.
-
Decreased IPD utilisation (See Figure 3 and Figure 4): Employees who availed themselves of OPD benefits showed a significant decline in IPD claims contribution to overall healthcare expenditure. This decrease is evident in both the number of claims (73% in 2022 to 57% in 2024) and the total claims incurred amount spent (67% in 2022 to 52% in 2024).

Figure 3. IPD claims count distribution with basis OPD benefits utilisation.

Figure 4. IPD incurred claims outgo distribution with basis OPD benefits utilisation.
-
Reduced hospital stays (See Figure 5): Individuals utilising OPD benefits consistently had shorter hospital stays compared to those who didn’t (0.28-0.52 days shorter across years). Close to 11% reduction was seen in the average length of stay in hospital by the third year of a continuous OPD Insurance engagement programme.

Figure 5. Hospital length of stay with basis OPD benefits utilisation.
-
Increased early intervention: The significant decrease in the ratio of unique IPD claimants who utilised OPD benefits (2:1 in 2022 to 1:1 in 2024) suggests a rise in early intervention through OPD services. It is observed that, on account of early disease management, the IPD incidence has been seen to increase by 4%. This potentially prevented minor health issues from escalating into hospitalisation needs.
-
Reduced severity (See Figure 6): It was observed that a 13% reduction in average per claim cost amongst users utilising OPD versus those not utilising OPD. The year-on-year (YoY) increase for cost per claim is higher for those not utilising OPD (2.6% year 1, 8.1% year 2) versus those utilising OPD services (1.7% year 1, 7.5% year 2).

Figure 6. Cost per claim with basis OPD benefits utilisation.
This analysis provides strong evidence that OPD benefit utilisation positively impacts IPD utilisation and overall healthcare costs.
Key challenge: The results differ across organisations depending on the programme design and offerings, coverages offered, demography of the organisation and the utilisation and engagement of the programme.
4.4. Insurer view and Healthcare Provider View
Insurers are designing OPD programmes and making them available on both a company-sponsored and voluntary basis. Insurers have further widened their network reach by empanelling clinics, diagnostic centres and local pharmacies making the OPD Insurance Program a viable solution for the end-users.
The majority of the insurers believe that a well-structured, comprehensive and sustainable OPD insurance plan will bring savings in group medical insurance plans in the long run. By promoting early intervention, chronic disease management, and preventive care, OPD programmes can contribute to a healthier workforce and significant cost savings for the company.
On the other hand, healthcare providers are also open and ready to integrate their outpatient services with TPA/Insurer platform for seamless user experience. Their multi-fold strategy includes:
-
Integration of services with claims processing platforms.
-
Co-creation of Group OPD products with insurers.
-
Digitisation and access to outpatient services.
-
Gamification of benefits.
The focus is on primary and preventive care aspects such as doctor consultation, diagnostics, mental health services, daily health & wellness management for employees and their families, with customisations possible at an individual employee level. With multiple service providers in the market, it represents a very competitive environment, which is driving innovation at affordable prices. Industry is now more open to new-age players with tech-enabled platforms, artificial intelligence and data analytics, stitching the health ecosystem together.
4.5. Strategies for Building Synergies between Outpatient and Inpatient Care
To build synergies between outpatient and inpatient care, healthcare systems must focus on several key strategies:
-
Enhanced communication: Establishing effective communication channels between outpatient and inpatient providers is essential for ensuring continuity of care. This includes sharing patient information, treatment plans and follow-up care instructions.
-
Integrated care models: Implementing integrated care models that facilitate collaboration between outpatient and inpatient services can lead to improved patient outcomes. For example, care coordinators can help manage transitions between care settings, ensuring that patients receive appropriate follow-up care after hospitalisation.
-
Patient education and engagement: Educating patients about their health conditions and the importance of outpatient care can empower them to take an active role in managing their health. Engaged patients are more likely to adhere to treatment plans and attend follow-up appointments, reducing the likelihood of hospitalisation.
-
Data-driven decision-making: Utilising data analytics to monitor healthcare utilisation patterns and outcomes can inform decision-making and resource allocation. By identifying trends and areas for improvement, healthcare organisations can implement targeted interventions to enhance care integration.
4.6. The Importance of Integration
4.6.1. Continuity of care
Continuity of care is a critical component of effective healthcare delivery. It ensures that patients receive consistent and coordinated care throughout their treatment journey. When outpatient and inpatient services are well-integrated, healthcare providers can share information, track patient progress, and make informed decisions about treatment plans. This continuity reduces the risk of fragmented care, which can lead to adverse outcomes, including medication errors, misdiagnoses, and unnecessary hospitalisations.
4.6.2. Improved patient outcomes
Research has shown that integrated care models can lead to improved patient outcomes. For instance, patients with chronic conditions who receive coordinated care between outpatient and inpatient settings experience fewer complications and hospital readmissions. By fostering synergies, healthcare providers can better manage patients’ needs, leading to enhanced health outcomes and increased patient satisfaction.
4.6.3. Cost efficiency
Integrating outpatient and inpatient care can also result in significant cost savings for healthcare systems. By reducing unnecessary hospitalisations and readmissions, healthcare providers can lower overall healthcare costs. Additionally, effective outpatient management can prevent the escalation of health issues that require more intensive inpatient care, ultimately leading to a more efficient allocation of resources.
4.7. Challenges to Integration
4.7.1. Fragmented healthcare delivery
One of the primary challenges to building synergies between outpatient and inpatient care is the fragmented nature of the healthcare system. Different providers often use disparate electronic health record systems, making it difficult to share patient information. This lack of interoperability can hinder communication and coordination, leading to gaps in care.
4.7.2. Provider resistance
Healthcare providers may be resistant to change, particularly if they are accustomed to traditional models of care. Integrating outpatient and inpatient services requires a shift in mindset and practice, which can be met with scepticism. Overcoming this resistance is essential for fostering collaboration and achieving successful integration.
4.7.3. Financial barriers
Financial incentives in the healthcare system often favour inpatient care over outpatient services. This misalignment can discourage providers from investing in outpatient care initiatives that promote integration. Addressing these financial barriers is crucial for creating a sustainable model of care that prioritises patient outcomes.
As healthcare systems continue to evolve, prioritising the integration of outpatient and inpatient services will be crucial for enhancing patient experiences, reducing costs, and ultimately improving health outcomes.
Future research should focus on identifying best practices for implementing integrated care models and exploring the long-term impacts on patient health and system efficiency. By fostering collaboration between outpatient and inpatient care, healthcare organisations can create a more cohesive and effective healthcare system that meets the needs of patients and providers alike.
5. Future Research on ‘Wellbeing Rating’
The early detection of lifestyle-related disorders and diseases has proven invaluable in guiding individual health management and preventing the onset of major chronic illnesses, including diabetes, hypertension, and cardiovascular diseases. These conditions, often insidious in their development, can be significantly mitigated through timely interventions informed by accurate health assessments. However, current health assessment models often fall short, failing to provide a readily accessible and comprehensive index that encapsulates the multifaceted nature of individual well-being. Existing tools may focus on isolated metrics or rely on infrequent, point-in-time assessments, neglecting the dynamic interplay of factors that contribute to overall health.
The proposed model will be grounded in a rich dataset of utilisation trends emerging out of OPD insurance covers – encompassing:
-
Annual health check-ups: Regular preventive screenings provide a baseline understanding of an individual’s health status and identify potential risk factors. Analysing trends in these check-ups over time can reveal patterns and changes in health.
-
Diagnostic services: Utilisation of diagnostic services, including laboratory tests and imaging, offers insights into specific health concerns and the progression of any existing conditions. Tracking the frequency and types of diagnostic procedures can contribute to a more nuanced health assessment.
-
Teleconsultations: The increasing adoption of telehealth provides valuable data on an individual’s engagement with healthcare providers, including their choice of doctors and specialists. Analysing teleconsultation trends can reveal patterns in seeking medical advice and managing health issues.
-
Pharmacy data: Prescribed medications, accessed through pharmacy claims, offer a direct indication of the medical conditions being managed and the adherence to prescribed treatments. Analysing medication fills and refills can provide insights into treatment efficacy and patient compliance.
-
Lifestyle questionnaire: A carefully designed questionnaire, encompassing lifestyle behaviours (e.g., diet, exercise, smoking habits), family medical history, and basic vital signs (e.g., blood pressure, weight), will supplement the utilisation data with crucial contextual information.
The central hypothesis is that by integrating these diverse data points, a more holistic and dynamic health score can be generated. Furthermore, aggregating these individual scores across a population can provide a valuable measure of community health, enabling targeted public health interventions and resource allocation.
Beyond simply generating a health index, this system aims to empower individuals and groups with actionable insights. By analysing the contribution of each parameter to the overall health score, the system can provide personalised recommendations for improvement. This feedback loop can motivate individuals to adopt healthier behaviours and make informed decisions about their healthcare. For example, the system might highlight the impact of regular exercise on cardiovascular health or the importance of medication adherence in managing chronic conditions. This personalised and actionable approach has the potential to significantly improve health outcomes and promote proactive health management.
Quantifying health status offers significant advantages for both individuals and communities, providing a baseline for health assessment, highlighting underlying risks, and informing targeted interventions. At the individual level, health quantification raises awareness of chronic disease risks, empowering individuals to take proactive steps towards prevention and management. For communities, it enables corporations to design tailored wellness programmes for their employees, assists insurance companies in pricing premiums more accurately, and informs the development of effective government health policies. These benefits underscore the importance of developing robust and reliable health quantification methodologies.
Health risk conditions can be broadly categorised as chronic or acute. This proposal focuses on the most prevalent chronic conditions: the risk of diabetes, hypertension, and cardiovascular disease (CVD). These risks are ideally assessed using actual physiological data, specifically blood glucose and blood pressure values. However, access to this data may be limited, particularly for individuals who are unaware of their current health status. Therefore, the proposed model will leverage the power of AI and machine learning (ML) to predict these risks based on existing data. This predictive component will utilise relevant attributes contributing to chronic disease risk, such as demographics, lifestyle factors, family history, and potentially even proxy measures derived from OPD utilisation patterns. This approach allows for risk stratification even in the absence of direct physiological measurements.
The core objective is to construct a multi-level health index/score, applicable at the individual, community, and corporate levels. This index will integrate physiological data (where available) with OPD insurance utilisation trends, categorised into the three target chronic disorders: diabetes, hypertension and CVD. The synthesis of these data sources will generate a single, comprehensive health score for each individual. Critically, the high frequency of claims within OPD insurance offers the potential for a near real-time health index. This dynamic score can reflect an individual’s current health status based on their latest OPD utilisation and health assessment results, providing a more responsive and personalised health management tool. This real-time capability distinguishes this approach from traditional static health assessments and opens up exciting possibilities for proactive interventions and personalised health recommendations.
5.1. Data Requirements
Required data are:
-
Lifestyle and family medical history data (while utilising the OPD insurance benefits/at the enrolment stage itself).
-
Digital medical locker - historic medical report and latest medical data.
-
OPD insurance benefits utilisation data - data cuts/patterns of OPD insurance utilisation trends.
5.2. Methodology
The objective of the Health Index/Score is to assign a single score to an individual/community/organisation/cohort which would represent overall health. Health Index/Score to eventually be utilised as a novel approach for arriving at this score by taking minimum number of already known/easily available data points yet covering all the major health risks that are relevant to majority of the key demographic population. This will eventually get built as a major aggregated data base which would be used for various segments of key and essential services in and around Health Index/Score.
5.3. Major Reference Point: Framingham Study & Idea Way forward
The Framingham Heart Study, a cornerstone of cardiovascular disease (CVD) epidemiology, has provided invaluable insights into the factors contributing to cardiovascular risk. Its widely used risk prediction equation incorporates key parameters such as age, gender, body mass index (BMI), lipid levels, smoking status, hypertension treatment, diabetes status and systolic blood pressure. While the Framingham equation provides a robust framework for assessing CVD risk, translating this complex information into a readily understandable metric is crucial for effective communication and individual engagement.
Therefore, it is proposed to develop a user-friendly, easily interpretable score derived from the Framingham equation (or potentially other advanced risk prediction models). Critically, this score should be framed as a “Wellbeing Rating” rather than a “Risk Rating.” This shift in terminology is essential for promoting a positive and proactive approach to health management, emphasising well-being and encouraging positive lifestyle changes, rather than solely focusing on potential risks.
This Wellbeing Rating will have broad applicability across multiple stakeholders:
-
Individuals: The rating will provide a readily accessible and personalised snapshot of their cardiovascular health, empowering them to understand their current status and make informed decisions about their lifestyle and healthcare.
-
Communities: Aggregated Wellbeing Ratings can provide a valuable measure of community health, enabling targeted public health interventions and resource allocation to address specific needs.
-
Corporates: Businesses can utilise aggregated Wellbeing Ratings to design and implement tailored employee wellness programmes, promoting a healthier workforce and potentially reducing healthcare costs.
-
Insurance companies: The Wellbeing Rating can serve as a valuable tool for risk assessment and underwriting in various insurance products, including hospitalisation and life insurance. This can lead to more personalised premium pricing based on individual health status.
-
Banks and financial institutions: Long-term loan products, such as mortgages, could potentially leverage Wellbeing Ratings to assess an individual’s long-term health prospects, informing lending decisions and potentially offering preferential rates to individuals with higher wellbeing scores.
The vision is for this Wellbeing Rating to become a widely recognised and trusted metric, like a credit score (e.g., CIBIL Score *). Its widespread adoption would facilitate better communication about health status, empower individuals to take control of their well-being, and enable various sectors to make more informed decisions based on a reliable and easily interpretable health metric. Further research and development will be necessary to refine the model, ensure its accuracy and validity, and explore the optimal ways to communicate and utilise the Wellbeing Rating across different contexts.
Preliminary work has begun to expand upon this foundation, but further development and broader accessibility are crucial. The current focus on promoting OPD insurance is strategically linked to the development of a robust Wellbeing Rating. Systematic analysis of OPD utilisation data trends, combined with key factors influencing major chronic risks like hypertension and diabetes, will provide the necessary data to refine and solidify this rating. This integrated approach allows for a more holistic and data-driven assessment of individual well-being. The Wellbeing Rating model will be further refined by incorporating specific risk factors for each condition:
Hypertension risk factorsFootnote *
-
Age
-
Gender
-
Body mass index (BMI)
-
Systolic blood pressure
-
Diastolic blood pressure
-
Smoking status (current, former, never)
-
Parental history of hypertension (yes/no)
-
Current use of hypertension medication (yes/no)
Diabetes risk factors
-
Age
-
Gender
-
Systolic blood pressure
-
Body mass index (BMI)
-
Waist circumference or waist-to-hip ratio
-
High-density lipoprotein cholesterol levels
-
Triglyceride levels
-
Current use of hypertension medication (yes/no)
-
Current use of diabetes medication (yes/no)
-
Fasting blood glucose levels
-
Parental history of diabetes (yes/no)
By incorporating these specific factors, the Wellbeing Rating will provide a more granular and accurate assessment of an individual’s risk profile for these critical chronic conditions. This detailed information will empower individuals to better understand their health status and work with healthcare professionals to develop personalised prevention and management strategies. Furthermore, the data collected through OPD utilisation and the Wellbeing Rating system can contribute to valuable research on the prevalence and trends of these conditions, informing public health initiatives and resource allocation. Future development of this model may include incorporating additional risk factors, refining the weighting of different parameters, and exploring the use of advanced analytics and machine learning techniques to further enhance the accuracy and predictive power of the Wellbeing Rating.
Acknowledgements
The authors would like to thank Marsh India for their continued support in backing the thought leadership work through this paper.












