Introduction
Suicide is a significant global health challenge and a leading cause of death worldwide (World Health Organization, 2021). Each instance of suicide profoundly impacts a broad network of people (Andriessen et al., Reference Andriessen, Mowll, Lobb, Draper, Dudley and Mitchell2017; Cerel et al., Reference Cerel, Fristad, Weller and Weller1999). Exposure to suicide, defined as having a personal connection to someone who has died by suicide (Andriessen et al., Reference Andriessen, Mowll, Lobb, Draper, Dudley and Mitchell2017), includes individuals who have lost someone close to them, such as a family member or friend, and are significantly affected by the death. These individuals are referred to as suicide loss survivors. Adolescents are particularly vulnerable to the psychological aftermath of suicide loss due to their unique developmental stage (Brent et al., Reference Brent, Melhem, Masten, Porta and Payne2012; Melhem et al., Reference Melhem, Day, Shear, Day, Reynolds and Brent2004). Accordingly, in the current study we aimed to examine extended (24-year) longitudinal trajectories of depressive symptoms in adolescents after suicide bereavement and to identify predictors of these pathways. The extended 24-year timeframe of this study is particularly significant, as it allows us to track the long-term impacts of suicide bereavement across the developmental period from adolescence through adulthood. This extensive longitudinal perspective is crucial for understanding how the effects of suicide loss during this critical developmental period may manifest and evolve over time, potentially influencing life trajectories and major life transitions.
Approximately 4.6% of adolescents lose someone to suicide in a given year, and about 18% experience such a loss before reaching adulthood (Andriessen et al., Reference Andriessen, Mowll, Lobb, Draper, Dudley and Mitchell2017). Moreover, a national cohort study from Sweden found that approximately 3.7% of adolescents lose a parent before the age of 18 due to various causes including natural causes, accidents, substance abuse, and suicide (Rostila et al., Reference Rostila, Berg, Arat, Vinnerljung and Hjern2016). The adverse effects of the loss of a loved one, such as parent, sibling, or friend, to suicide can be particularly pronounced during adolescence compared to losses from natural deaths (Andriessen et al., Reference Andriessen, Mowll, Lobb, Draper, Dudley and Mitchell2017; Balk Reference Balk1991; Brent et al., Reference Brent, Moritz, Bridge, Perper and Canobbio1996; Robin & Omar, Reference Robin and Omar2014). Suicide bereavement can affect various facets of an adolescent’s life, including self-perception, identity formation, interpersonal relationships, academic performance, and mental health (Robin & Omar, Reference Robin and Omar2014).
Grief during this pivotal developmental stage can obstruct the achievement of milestones and pose obstacles to normal transitions into adulthood. Research underscores the profound psychological impact on adolescent suicide survivors, indicating an increased risk for depression, post-traumatic stress disorder, anxiety, and suicidal behaviors (Brent et al., Reference Brent, Perper, Moritz, Allman, Friend, Roth, Schweers, Balach and Baugher1993; Andriessen et al., Reference Andriessen, Mowll, Lobb, Draper, Dudley and Mitchell2017; Cerel et al., Reference Cerel, Fristad, Weller and Weller1999; Pfeffer et al., Reference Pfeffer, Jiang, Kakuma, Hwang and Metsch2002). The impact of suicide loss can be due to several factors. The sudden and often unexpected nature of the loss can be deeply shocking and disruptive. Bereaved adolescents may grapple with intense feelings of guilt, self-blame, or perceived responsibility for the death (Robin & Omar, Reference Robin and Omar2014). The stigma often associated with suicide can lead to social isolation or difficulties in seeking support, further complicating the grieving process (Cerel et al., Reference Cerel, Fristad, Weller and Weller1999). Additionally, the distressing and potentially traumatic circumstances surrounding the death can have lasting psychological effects (Cerel et al., Reference Cerel, Fristad, Weller and Weller1999; Pfeffer et al., Reference Pfeffer, Jiang, Kakuma, Hwang and Metsch2002). Finally, the loss represents the absence of a potentially significant role model or source of support during a critical developmental period, which can have far-reaching implications for the adolescent’s growth and future (Robin & Omar, Reference Robin and Omar2014).
The impact of suicide loss may not be limited to the immediate aftermath but can also have long-term, downstream effects (Brent et al., Reference Brent, Melhem, Masten, Porta and Payne2012). For example, the absence of an important figure during crucial developmental stages can lead to disruptions in attachment patterns, potentially affecting future relationships. Adolescents might face challenges in identity formation and self-concept development, as they navigate their formative years without a significant role model (Robin & Omar, Reference Robin and Omar2014). The loss may also result in difficulties with emotional regulation and the development of effective coping strategies. Furthermore, the impact of the loss may alter educational and career trajectories, as the absence of guidance and support during critical decision-making periods can influence life choices. Lastly, the cumulative effect of these challenges can contribute to an increased vulnerability to mental health issues in adulthood, underscoring the long-lasting nature of suicide bereavement’s impact on adolescent development.
Bailey et al. (Reference Bailey, Kral and Dunham1999) suggested that not all individuals navigate the aftermath of a suicide loss in the same manner, highlighting the need to explore factors that predict these diverse responses. Previous research has identified several potential predictors of differential trajectories of depressive symptoms among adolescents who have experienced suicide loss, encompassing both individual and environmental factors that may influence the broader developmental process and psychological outcomes.
At the individual level, demographic characteristics may influence adolescents’ experiences following suicide bereavement. For example, younger adolescents tend to report higher levels of emotional distress compared to older adolescents (Hanschmidt et al., Reference Hanschmidt, Lehnig, Riedel-Heller, Kersting and van Wouwe2016; Haw et al., Reference Haw, Hawton, Niedzwiedz and Platt2013). Regarding gender, several studies have indicated that female adolescents are at greater risk for prolonged grief and depressive symptoms as they are more likely to report stigma and shame related to the suicide loss of a loved one (Hanschmidt et al., Reference Hanschmidt, Lehnig, Riedel-Heller, Kersting and van Wouwe2016). Additionally, Rivart et al. (Reference Rivart, Wainwright, Flynn, Hunt, Shaw, Smith, McGale and McDonnell2021) found that bereaved individuals from various racial backgrounds may encounter higher levels of stigma within their communities, which can hinder help-seeking behavior. This stigma is compounded by perceived external discrimination and mistrust of formal support services. Furthermore, a significant number of participants from different racial backgrounds in the study reported a lack of culturally sensitive support and difficulties accessing appropriate mental health services. The findings indicate that while grieving processes may not fundamentally differ between ethnic groups, minority adolescents may experience additional barriers, such as cultural taboos surrounding suicide and limited community-based support, making them more vulnerable to adverse psychological outcomes (Rivart et al., Reference Rivart, Wainwright, Flynn, Hunt, Shaw, Smith, McGale and McDonnell2021 ). Personality traits, such as neuroticism, have been linked to an increased vulnerability to depression in the context of stressful life events, including bereavement (Kendler et al., Reference Kendler, Kuhn and Prescott2004; Ormel et al., Reference Ormel, Oldehinkel and Brilman2001). Sleep quality has also emerged as a potentially important predictor, with sleep disturbances being common in the aftermath of a significant loss and associated with an increased risk of developing depression (Kaplow et al., Reference Kaplow, Saunders, Angold and Costello2010).
While individual factors play a crucial role, it is equally important to consider the broader context in which adolescents experience and process a loss. Environmental factors, including family, school, and community contexts, have also been implicated in shaping the trajectories of depressive symptoms among bereaved adolescents. The quality of the parent-child relationship, as perceived by both the adolescent and the parent, has been found to influence the adolescent’s ability to cope with the loss and adapt to the new reality (Sandler et al., Reference Sandler, Ayers, Tein, Wolchik, Millsap, Khoo, Kaplan, Ma, Luecken, Schoenfelder and Coxe2010; Shapiro et al., Reference Shapiro, Howell and Kaplow2014). Similarly, a sense of connection to school and satisfaction with one’s neighborhood have been identified as potential protective factors that may promote resilience in the face of adversity (Andriessen et al., Reference Andriessen, Draper, Dudley and Mitchell2015). Access to mental health and substance use treatment is another crucial environmental factor that may impact the trajectories of depressive symptoms among bereaved adolescents, with the availability and utilization of these services providing much-needed support and facilitating the healing process (Kersting et al., Reference Kersting, Brähler, Glaesmer and Wagner2011; Melhem et al., Reference Melhem, Porta, Payne and Brent2013).
Despite the acknowledged impact of suicide loss, there remains a notable gap in targeted, age-specific research focusing on adolescents (Pitman et al., Reference Pitman, Osborn, Rantell and King2016). Research with both youth (Haag et al., Reference Haag, Bonanno, Chen, Herd and Strong-Jones2023) and adults (Galatzer-Levy et al., Reference Galatzer-Levy, Huang and Bonanno2018) facing aversive circumstances has consistently revealed heterogenous trajectories of outcome. However, research on adolescent suicide loss has largely overlooked the spectrum of possible trajectory patterns. A recent study by Liu and Wang (Reference Liu and Wang2024) addressed some of these gaps by examining how exposure to suicide attempts by friends and family members during adolescence impacts long-term outcomes. Their findings demonstrated that both friends’ and family members’ suicide attempts were significant risk factors for suicidal ideation and attempts from adolescence through young adulthood (Liu and Wang, Reference Liu and Wang2024). The study also revealed that depressive symptoms served as an important mechanism linking this exposure to later suicidal thoughts and behaviors, with higher levels of depressive symptoms mediating the relationship between suicide exposure and subsequent suicidal ideation and attempts (Liu and Wang, Reference Liu and Wang2024). While Liu and Wang’s study provides valuable insights into how exposure to suicide attempts impacts later suicidal behaviors through depressive symptoms, their study did not investigate the trajectories of depressive symptoms that may emerge following suicide loss. Although their study spanned multiple years, they did not examine how different subgroups of adolescents might show varying patterns of depressive symptoms over time following suicide bereavement, nor did they explore early psychosocial indicators that might help identify adolescents at risk for different long-term adjustment trajectories. Addressing these gaps through trajectory-based analyses is crucial for developing more targeted and effective interventions that account for the heterogeneous nature of bereavement responses among adolescents.
To address these research gaps, we aimed to identify long-term trajectories of depressive symptoms following the suicide loss of a close one among adolescents using Latent Growth Mixture Modeling (LGMM). This method allows for the identification of latent subgroups that follow similar patterns of change (Muthén & Muthén, Reference Muthén and Muthén2012). Previous research on depressive symptoms trajectories after bereavement has consistently highlighted the heterogeneity in outcomes. For example, Galatzer-Levy and Bonanno (Reference Galatzer-Levy and Bonanno2012) have described four trajectories: resilient (66.3%, little or no depressive symptoms), chronic grief (9.1%, sustained depressive symptoms after loss), depressed-improved (10.1%, high pre-loss depressive symptoms that declines post-loss), and pre-existing chronic depression (14.5%, consistently high levels of depressive symptoms before and after loss). Similarly, Maccallum et al. (Reference Maccallum, Galatzer-Levy and Bonanno2015) found comparable trajectories following both spousal and child bereavement: resilience (68.2%), chronic grief (13.2%), depressed-improved (11.2%), and pre-existing chronic depression (7.4%). More recently, Djelantik et al. (Reference Djelantik, Robinaugh and Boelen2022) identified three distinct trajectories—resilient (66.4%), chronic (25.1%), and acute recovery (8.4%, elevated grief in the first months after the loss that recover during the first year)—among bereaved individuals over the first 27 months post-loss. Given this body of work, the specific objectives of the current study are twofold: (1) To examine whether the prototypical patterns observed in other forms of loss and adversity are also present in the long-term following adolescents suicide bereavement. Specifically, this analysis will examine trajectories of depressive symptoms over an extended period, 24 years, among adolescents who have experienced the loss of a family member or friend due to suicide within 12 months of the baseline (Wave 1) data collection. (2) to explore a set of baseline psychosocial variables as early indicators that may differentiate these long-term developmental trajectories.
Methods
Data and sample
This study utilized public-use data from the National Longitudinal Study of Adolescent to Adult Health (Add Health), a longitudinal study employing a multistage stratified cluster design to recruit a nationally representative sample of 20,745 adolescents in grades 7–12 from 132 schools across the USA in 1994–1995. The participants were followed through five survey waves. Add Health used a school-based sampling design, selecting 80 high schools across urban, suburban, and rural areas with probability proportional to size, as well as 52 middle schools paired with the high schools as feeder schools. Schools were stratified by region, urbanicity, school type (public, private, parochial), ethnic mix, and size. Response rates for the Add Health study were as follows: Wave I (79.0%, n = 20,745), Wave II (88.6%, n = 14,738), Wave III (77.4%, n = 15,197), Wave IV (80.3%, n = 15,701), and Wave V (71.8%, n = 12,300).
The analytic sample for this study (n = 236) included participants who answered “yes” to the question “Have any of your family members or friends succeeded in committing suicide in the past 12 months?” at Wave I. Additionally, these participants completed the in-home interviews across Waves I (1994–1995, ages 11–19 years), II (1996, ages 12–20 years), III (2001–2002, ages 18–26 years), IV (2007–2008, ages 24–32 years), and V (2016-2018, ages 33–43 years) (Chen & Harris, Reference Chen and Harris2020).
Procedure
The public-use data for this study was obtained from the Add Health study website for analysis. To protect participant privacy, the Add Health data do not contain respondent identifiers. Prior to data collection, written informed consent was obtained from the respondents’ parents for those aged 18 years and younger, and directly from respondents older than 18 years. The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of the University of North Carolina at Chapel Hill (Harris et al., Reference Harris, Udry and Bearman2019). Surveys were administered privately using two methods: Computer-Assisted Personal Interview (CAPI) and Audio Computer-Assisted Self-Interview (ACASI). CAPI involves an interviewer reading questions aloud to the respondent and entering their responses into a computer, while ACASI allows respondents to read questions on a computer screen and enter their responses directly, providing an additional layer of privacy for sensitive topics (Harris et al., Reference Harris, Udry and Bearman2019). The use of these computer-assisted methods helps to ensure the consistency and quality of the data collected across multiple survey waves and interviewers (Chen & Harris, Reference Chen and Harris2020). The Add Health study employed a variety of measures to maintain high response rates and data quality throughout the longitudinal data collection process. These included locating and recruiting respondents using a combination of mail, telephone, and field contacts; providing incentives for participation; and offering make-up interviews for missed appointments (Harris et al., Reference Harris, Udry and Bearman2019).
Measurements
Depressive symptoms
Depressive symptoms experienced over the past week were evaluated using a modified, three-item version of the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, Reference Radloff1977). This shortened scale required participants to rate their experiences on a four-point Likert scale: 0 (‘rarely or none of the time’), 1 (‘sometimes’), 2 (‘a lot of the time’), and 3 (‘most or all of the time’). The specific items queried included: “you felt that you could not shake off the blues, even with help from your family and your friends”, “you felt depressed”, and “you felt sad”. Mean scores were calculated to quantify the severity of depressive symptoms for each study wave. Internal consistency reliability analyses across the five waves demonstrated good to very good reliability (DeVellis, Reference DeVellis2016): Wave 1 (α = .73), Wave 2 (α = .78), Wave 3 (α = .74), Wave 4 (α = .82), and Wave 5 (α = .83). Mean scores across waves ranged from 1.51 to 2.23 (SDs = 1.94-2.20), with scores ranging from 0 to 9.
Predictors
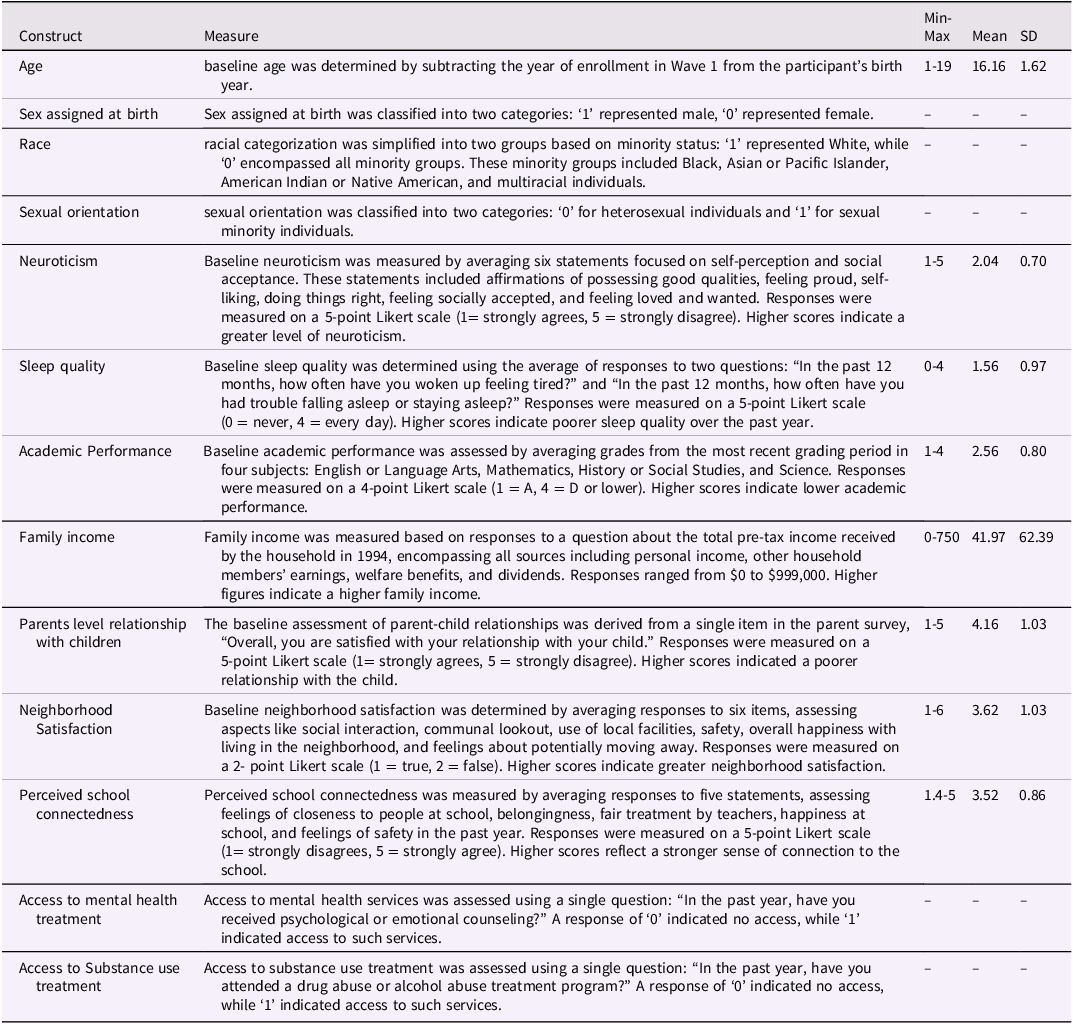
Baseline person-level and context-level predictors were included in the analyses. Person-level predictors consisted of age, race, sexuality, neuroticism, sleep quality, and academic performance. Context-level predictors included household income, parents’ perceived relationship with children, neighborhood satisfaction, school connection, access to mental health treatment, and access to substance use treatment. All predictors used in the prediction analyses, along with their descriptive statistics, are presented in Table 1.
Table 1. Personal level and context level predictors used in the multinomial logistic regression analyses
Analytic plan
Statistical analyses were conducted using Mplus Version 7.4 and R Version 4.0.4 (Muthén & Muthén, Reference Muthén and Muthén2012; R Core Team, 2021). Latent Growth Mixture Modeling (LGMM), a form of unsupervised machine learning, was employed to identify distinct trajectories of depressive symptoms over time. The model accounted for the unequal time intervals between waves, with measurement time points specified at 0, 1, 6, 13, and 23 years. This approach ensured that the irregular spacing of assessments across the 24-year period was accurately represented in the analysis. Missing data were handled using Full Information Maximum Likelihood estimation, which assumes data are missing at random and uses all available information to estimate model parameters without excluding cases with incomplete data.
The analysis began by fitting a single-class latent growth model. The single-class model had a significant intercept (2.03, p < .001), and a marginally significant negative slope (−0.02, p = .062). We observed significant variance in both the intercept (1.71, p < .001) and slope (0.01, p = .011). When we attempted to freely estimate both the intercept and slope variances in subsequent multi-class models, convergence issues emerged. Based on the initial model results, the intercept was allowed to vary freely, while the slope was fixed in the final model to aid convergence. Subsequently, we evaluated LGMM models with 1 to 4 latent classes. Fit indices, including Akaike Information Criteria (AIC), Sample-Size Adjusted Bayesian Information Criteria (SSABIC), Entropy, Bootstrap Likelihood Ratio Test (BLRT), and adjusted Likelihood Ratio Test (LRT). The optimal model was selected based on: (1) lower AIC and SSABIC values indicating better fit, (2) entropy values above 0.80 indicating clear class separation, (3) significant BLRT and LRT (p < .05) improved model fit relative to the pervious class solution, and (4) class sizes exceeding 5% of the sample to ensure stability. Models with classes comprising fewer than 5% of the total sample were excluded to ensure stability and replicability (Nylund-Gibson & Choi, Reference Nylund-Gibson and Choi2018). The final model was selected based on statistical fit, theoretical coherence, and explanatory relevance.
Depressive symptoms scores were relatively stable across waves (Wave 1: M = 2.23; Wave 2: M = 1.97; Wave 3: M = 1.51; Wave 4: M = 1.86; Wave 5: M = 1.74), with near-complete data at baseline (99.6% available) and varying completion rates in subsequent waves (Wave 2: 75.8%; Wave 3: 72.5%; Wave 4: 79.7%; Wave 5: 61.9%).
After identifying the optimal trajectory solution, we conducted a multinomial logistic regression analysis to examine predictors of trajectory group membership using Mplus Version 7.4. The predictors included in the model were age, sex assigned at birth, race, sexuality, family income, academic performance, neuroticism, sleep quality, parental report of relationship with children, school connection, neighborhood satisfaction, access to mental health services, and access to substance use treatment. All predictors were entered simultaneously in the model, with membership in the resilient trajectory group used as the reference category for comparison. We tested for multicollinearity by examining the correlation between predictors. Correlations between predictors were all below 0.5, indicating no serious multicollinearity concerns. Missing data in predictor variables were handled using Monte Carlo integration method in Mplus to obtain parameter estimates. This method accommodates missing data under the assumption that data are missing at random (MAR), ensuring that all available information is used in the analysis without excluding participants with incomplete data. Maximum likelihood estimation was used, and results are presented as odds ratios with 95% confidence intervals to indicate the relative likelihood of membership in each trajectory group compared to the reference group (resilient trajectory), given a one-unit increase in each predictor while controlling for all other variables in the model.
Results
Sample characteristics
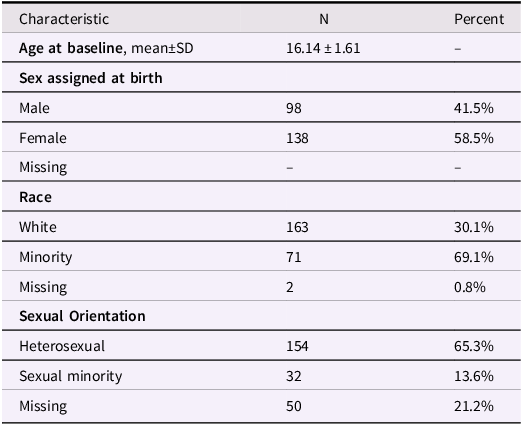
Our sample consisted of 236 adolescents who experienced the suicide of a family member or friend in the 12 months prior to Wave I (Table 2). Compared to the complete sample, the bereaved subsample had a higher proportion of females (58.5% vs 51.6%) and White participants (69.1% vs 64.2%), though these differences were not statistically significant (p = 0.116 and p = 0.194, respectively). The mean age at baseline was 16.16 years (SD = 1.62, range: 13–20 years), similar to the complete sample (M = 16.04, SD = 1.77, p = 0.286). Among those who reported sexual orientation (78.8% of the sample), 154 (82.8%) identified as heterosexual and 32 (17.2%) as sexual minorities. This distribution was comparable to the complete sample (86.2% heterosexual, 13.8% sexual minorities; p = 0.386), with similar rates of missing data (bereaved: 21.2%, complete: 22.1%).
Table 2. Participant demographics
Regarding participation across waves, retention rates remained relatively high through the first four waves, with 75.8% (n = 179) participating in Wave 2, 72.5% (n = 171) in Wave 3, and 79.7% (n = 188) in Wave 4. There was some attrition by Wave 5, with 61.9% (n = 146) of the original sample participating. The pattern of missingness showed fluctuation rather than a steady decline, suggesting that dropout was not entirely systematic.
Latent growth mixture modeling (LGMM)
We conducted a series of one- to four-class LGMMs to identify distinct trajectories of depressive symptoms over time (Table 3). The Akaike Information Criteria (AIC), Bayesian Information Criteria (BIC), and Sample-Size Adjusted Bayesian Information Criteria (SSABIC) consistently decreased from one to four classes, indicating improved model fit. Both the Bootstrap Likelihood Ratio Test (BLRT) and adjusted Likelihood Ratio Test (LRT), which compare n-class solution with (n − 1) class solutions, showed significant results up to three classes (p < .001). Entropy for each solution was high (>.80), indicating clear separation between classes (Celeux & Soromenho, Reference Celeux and Soromenho1996), while class prevalences were adequate (>5%). Based on these indices, the three-class model was clearly the optimal solution (Figure 1). The most prominent trajectory (77.5%) was characterized by stable low depressive symptoms, followed by a trajectory (16.9%) of initially high depressive symptoms that declined to sustained moderate depressive symptoms (recovery-moderate depressive symptoms), and a trajectory (5.5%) of initially low but gradually increasing symptoms (delayed depressive symptoms).
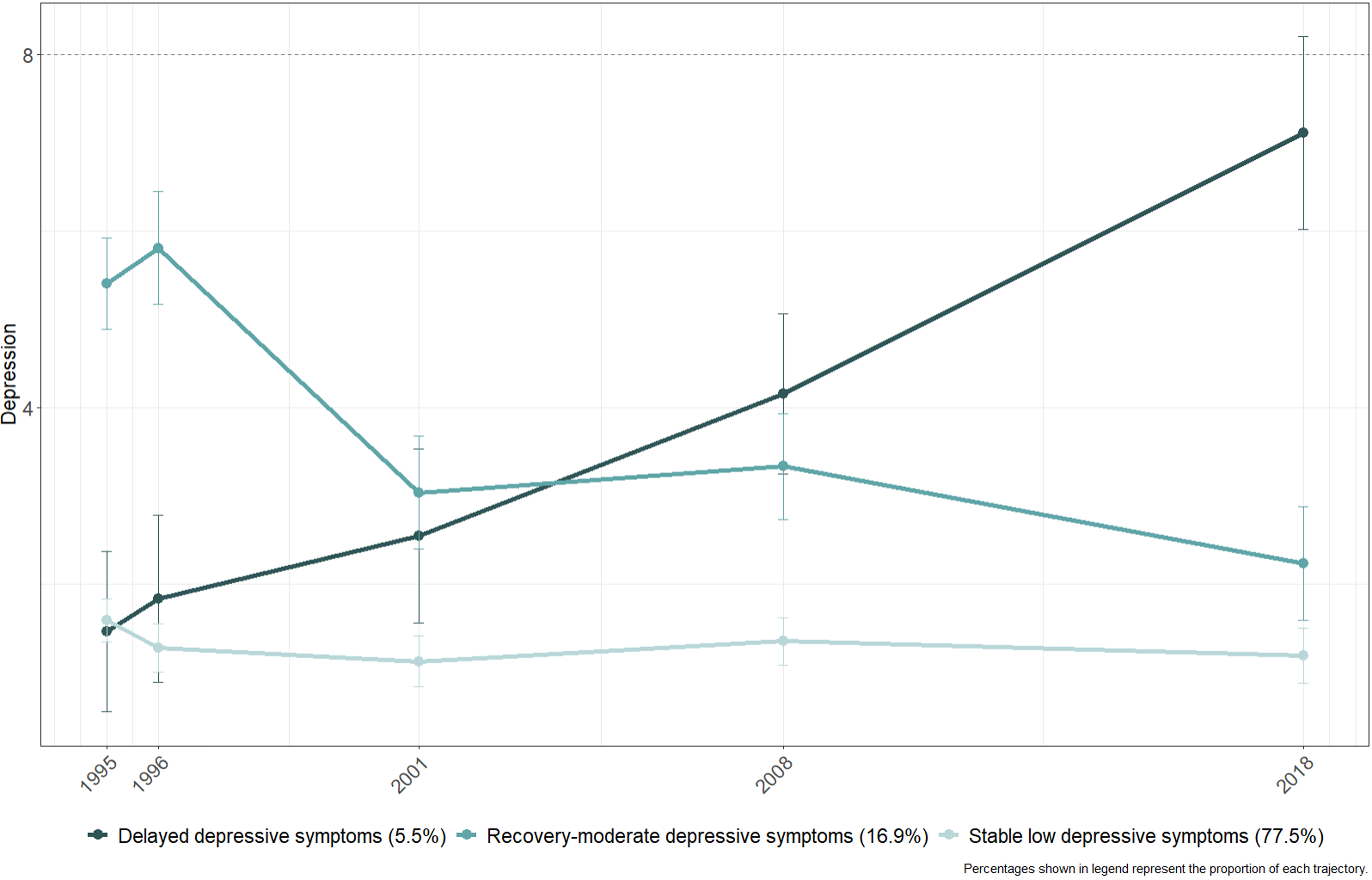
Figure 1. Depression trajectories.
Table 3. Fit indices for latent growth mixture models (LGMM) for depressive symptoms
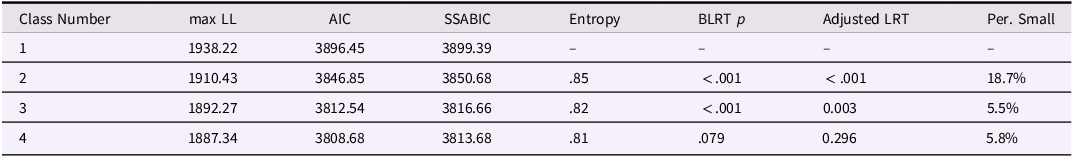
Note. max LL = maximized log likelihood value. AIC = Akaike Information Criterion. SSABIC = Sample-size adjusted Bayesian Information Criterion. BLRT = Parametric Bootstrapped likelihood ratio test. Per. Small = Percentage of participants in the smallest group. Adjusted LRT = Adjusted Likelihood Ratio Test.
Predictors of trajectory group membership
We next conducted a multinomial logistic regression to identify predictors of trajectory group membership (Table 4). The predictors included in the model were age, sex, race, sexuality, family income, academic performance, neuroticism, sleep quality, parental report relationship with adolescents, school connection, neighborhood satisfaction, access to mental health, and access to substance use treatment program. Among key predictor variables, missing data rates varied: Academic Performance (28.39%), and Income (20.76%). Several important variables had high completion rates, including School Connectedness (97.46% complete), Neighborhood Satisfaction (98.31% complete), and demographic variables such as age and sex (100% complete).
Table 4. Multinomial logistic regression results predicting trajectory membership
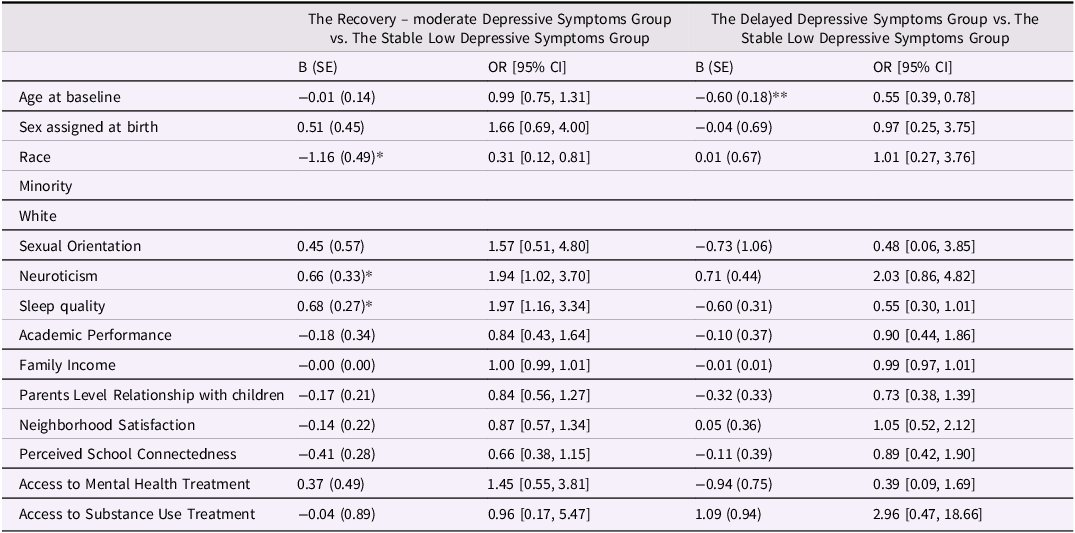
Note: B = unstandardized regression coefficient; SE = standard error; OR = odds ratio; CI = confidence interval. *p < .05. **p < .01.
When comparing the recovery-moderate depressive symptoms group to the stable low depressive symptoms group, race (B = −1.161, SE = 0.488, p = .017), neuroticism (B = 0.664, SE = 0.330, p = .044), and sleep quality (B = 0.678, SE = 0.271, p = .012) were significant predictors. Specifically, individuals who identified as white had lower odds of being in the recovery-moderate depressive symptoms group compared to the stable low depressive symptoms group (OR = 0.313), while those with greater neuroticism and poorer sleep quality had higher odds of being in the recovery -moderate depressive symptoms group (OR = 1.943 and OR = 1.971, respectively). In the comparison between the delayed depressive symptoms group and the stable low depressive symptoms group, age (B = −0.597, SE = 0.179, p = .001) was the only significant predictor. Older individuals were less likely to be in the delayed depressive symptoms group compared to the stable low depressive symptoms group (OR = 0.551). Other variables in the model did not significantly predict membership in either the recovery-moderate depressive symptoms group or the delayed depressive symptoms group compared to the stable low depressive symptoms group.
Discussions
The present study aimed to identify 24-year trajectories of depressive symptoms following adolescents who experienced the loss of a family member or friend due to suicide and to investigate a range of baseline psychosocial variables that may differentiate these trajectories. By employing a person-centered approach across several decades, we sought to capture the heterogeneity in depressive symptoms across a wide developmental phase and shed light on the factors that might contribute to different trajectories of adaptation following suicide bereavement.
Our analysis identified three distinct trajectories of depressive symptoms: stable low depressive symptoms, initially high depressive symptoms that declined to sustained moderate depressive symptoms (recovery-moderate depressive symptoms), and initially low but gradually increasing symptoms (delayed depressive symptoms). The prevalence of stable low depressive symptoms (77.5%) among adolescents bereaved by suicide aligns with the considerable literature documenting resilience patterns in both youth and adults (Bonanno et al., Reference Bonanno, Chen and Galatzer-Levy2023; Bonanno, Reference Bonanno2004; Djelantik et al., Reference Djelantik, Robinaugh and Boelen2022; Galatzer-Levy & Bonanno, Reference Galatzer-Levy and Bonanno2012; Galatzer-Levy et al., Reference Galatzer-Levy, Huang and Bonanno2018; Maccallum et al., Reference Maccallum, Galatzer-Levy and Bonanno2015). Our findings extend this literature by demonstrating the stability of the resilience pattern from adolescence to well into adulthood.
Particularly noteworthy, however, we also observed a delayed increase in depressive symptoms trajectory (5.5%) in this sample. Individuals categorized in this trajectory pattern had low symptoms at the first measurement, seemingly identical with the stable low depressive symptoms group. Their depressive symptom levels increased only slightly by two years of bereavement, and then increased steadily in the years afterwards. Nine years after the loss, their depressive symptoms were considerably greater but still relatively moderate. They continued to increase, however, by 14 years after the loss, and then climbed even more steeply, reaching the highest level of any group in the sample, 24 years after the loss. While our shortened version of the CES-D prevents us from determining whether these elevated symptoms reached clinical thresholds, the identification of this long-term trajectory is significant give that the majority of previous studies on adolescent bereavement have focused on the immediate aftermath of the loss or have employed cross-sectional designs (Brent et al., Reference Brent, Perper, Moritz, Allman, Friend, Roth, Schweers, Balach and Baugher1993; Balk, Reference Balk1991), limiting our understanding of long-term trajectories of depressive symptoms. Our study addresses this gap by utilizing a longitudinal design spanning over two decades, allowing us to capture the long-term developmental consequences years downstream from the loss. Importantly, while we identified this distinctive trajectory pattern, the mechanisms underlying this delayed increase are not clear. While it could represent a delayed reaction to the loss, it might also reflect responses to changes in life circumstances that emerged as a consequence of the loss (e.g., the absence of the deceased in important life roles), or factors unrelated to the bereavement itself. Our data cannot definitively determine which of these explanations is most accurate.
The extensive longitudinal perspective provided several key insights. It suggested a persistence of the impact of suicide loss well into adulthood, at least for a small subset of bereaved youth, highlighting the enduring nature of this experience. Our findings aligned with recent research by Liu and Wang (Reference Liu and Wang2024), who also utilized the Add Health dataset to examine long-term effects of suicide exposure on adolescents. While their study focused on the impact of friends’ and family members’ suicide attempts on suicidal ideation and attempts, rather than completed suicides, they examined depressive symptoms as a mediator rather than tracking distinct trajectories as we did in our study. Notably, both our study and Liu and Wang’s (Reference Liu and Wang2024) highlighted the importance of long-term monitoring and support for adolescents exposed to suicide, as the psychological impact may not be immediately apparent and can persist well into adulthood. However, our study’s focus on completed suicides provided unique insights into the specific challenges faced by bereaved adolescents, complementing Liu and Wang’s findings on the impact of suicide attempts. Additionally, it allowed for the identification of long-term delayed-onset depression, a pattern that would be missed in shorter-term studies. Specifically, our trajectory analyses revealed that some participants experienced increases in depressive symptoms during key life transitions such as entering college/workforce (around Wave III, ages 18–26) and establishing long-term relationships and careers (Wave IV, ages 24–32). This suggests that these developmental transitions may act as potential periods of vulnerability for bereaved individuals. Furthermore, it offered insights into the long-term resilience of the majority of bereaved adolescents, demonstrating the human capacity for adaptation even in the face of profound loss.
The delayed onset of depressive symptoms is likely related to a complex interplay of developmental challenges, residual grief, and cascading consequences of the loss. Adolescence is a period marked by significant cognitive, emotional, and social changes, and the experience of suicide loss may disrupt these developmental processes (Robin & Omar, Reference Robin and Omar2014). As adolescents navigate the challenges of identity formation, autonomy seeking, and peer relationships, the full impact of the loss may not be immediately apparent. Over time, as they confront new developmental milestones and stressors, the impact of grief and/or the absence of the lost relationship may become more salient, leading to the emergence of depressive symptoms (Balk, Reference Balk1991). Delayed depressive symptoms may reflect the gradual depletion of coping resources and support systems over time. Initially, adolescents may rely on the support of family, friends, and the broader community to cope with the loss. However, as time passes, these support systems can become less available or less attuned to the evolving needs of the bereaved adolescent (Andriessen et al., Reference Andriessen, Draper, Dudley and Mitchell2015). The deterioration of social support, combined with the accumulated stress of navigating developmental challenges, can potentially contribute to an increase in the risk of depressive symptoms in adolescents who have experienced loss. Conversely, the trajectory showing decreasing depressive symptoms over time likely reflects successful adaptation and recovery processes. This pattern suggests that many bereaved adolescents are able to effectively utilize initial support systems, develop adaptive coping strategies, and gradually integrate their loss experience into their life narrative. The decrease in symptoms may also indicate the development of resilience through the grieving process, where individuals learn to maintain meaningful connections with the deceased while engaging in healthy developmental progression (Stroebe & Schut, Reference Stroebe and Schut2010).
To address our second research question, we identified several noteworthy predictors of trajectory group membership. Race, neuroticism, and sleep quality were associated with the recovery -moderate depressive symptoms trajectory, while age distinguished the delayed depressive symptoms trajectory from the stable low depressive symptoms trajectory. These findings are consistent with previous research that has identified demographic characteristics, personality traits, and sleep disturbances as potential risk factors for adverse psychological outcomes following suicide bereavement (Brent et al., Reference Brent, Perper, Moritz, Allman, Friend, Roth, Schweers, Balach and Baugher1993; Kaplow et al., Reference Kaplow, Saunders, Angold and Costello2010; Melhem et al., Reference Melhem, Day, Shear, Day, Reynolds and Brent2004). Our results indicated that individuals who identified as white and were older were significantly more likely to be in the stable low depressive symptoms group, suggesting that these demographic factors may confer some protection against the development of depressive symptoms following suicide loss. This finding aligns with previous studies that have reported differential vulnerability to depression based on age and race (Brent et al., Reference Brent, Perper, Moritz, Allman, Friend, Roth, Schweers, Balach and Baugher1993; Melhem et al., Reference Melhem, Day, Shear, Day, Reynolds and Brent2004). However, further research is needed to elucidate the underlying mechanisms and potential confounding factors that may contribute to these associations, with implications for developing tailored intervention strategies for different depression trajectory groups.
A notable strength of this study is the use of a nationally representative sample of adolescents from the Add Health dataset, which allowed for the examination of extended developmental trajectories of depressive symptoms following suicide loss and the exploration of a wide range of potential predictors. While our subsample of bereaved adolescents showed slightly higher proportions of females (58.5% vs 51.6%) and White participants (69.1% vs 64.2%) compared to the complete Add Health sample, these differences were not statistically significant. Similarly, the age distribution (M = 16.16 years) and sexual orientation composition were comparable to the complete sample, suggesting our findings may be reasonably generalizable. However, the moderate attrition by Wave 5 (61.9% retention) should be considered when interpreting long-term trajectories. The longitudinal design and the inclusion of multiple waves of data spanning more than two decades provide a unique opportunity to investigate the enduring impact of suicide loss on adolescents’ mental health. Our identification of the delayed depressive symptoms trajectory is a unique contribution of this study, as it sheds light on a subgroup of adolescents who may not initially exhibit significant depressive symptoms but are at risk of developing them over time. This finding underscores the importance of long-term monitoring and support for bereaved adolescents, as the psychological and practical impacts of suicide loss may not be immediately apparent. The likely complex interplay of developmental challenges and emerging impacts of the loss highlight the need for targeted interventions that can address the evolving needs of adolescents as they navigate their developmental journey into adulthood.
Our study is not without limitations. First, the measurement of depressive symptoms relied on a modified, three-item version of the CES-D scale, which may not fully capture the complexity of depressive symptomatology. Future studies may benefit from using more comprehensive assessments of depression and other relevant mental health outcomes. Second, the study did not include a measure of grief per se, which is a central component of the experience of suicide loss. Incorporating validated measures of grief severity and persistence could provide valuable insights into the interplay of and possible unique causes and impacts of grief and depressive symptoms among bereaved adolescents. Third, a significant limitation is that our data did not distinguish between the loss of family members versus friends, as participants only responded to a general question about suicide loss of “family members or friends.” This prevents us from examining potentially different psychological impacts based on relationship closeness or type, particularly regarding parental loss which has been shown to have distinct developmental implications. Fourth, the unequal time intervals between measurements (0, 1, 6, 13, and 23 years) create differential sensitivity to changes in depressive symptoms across the study period. While the early measurements (years 0–1) provide detailed capture of short-term changes, the longer intervals in later years may miss intermediate fluctuations in depressive symptoms, potentially affecting our ability to detect more nuanced patterns of change over time. Finally, the presence of missing data in our dataset may have affected the representativeness of our findings.
These limitations notwithstanding, our findings have important clinical implications. By identifying distinct trajectories of depressive symptoms and their associated predictors, our research highlights the need for personalized interventions that cater to the diverse needs of adolescents bereaved by suicide. Moreover, the study underscores the importance of considering the broader family, school, and community contexts in supporting bereaved adolescents. Interventions that promote resilience and coping skills, enhance social support networks, and address potential barriers to accessing mental health services may be particularly beneficial in mitigating the long-term impact of suicide loss on adolescents’ mental health. By illuminating the diverse trajectories of adaptation following suicide loss, this study paves the way for future research and clinical efforts aimed at promoting resilience and mitigating the long-term mental health consequences of suicide bereavement among adolescents. Ultimately, these insights can inform the development of more effective support systems and interventions, potentially improving long-term outcomes for this vulnerable population.
Acknowledgements
We would like to express our gratitude to Kathleen Mullan Harris and J. Richard Udry for making the longitudinal data available to the public, as well as to all the participants in the original study (Harris et al., Reference Harris, Udry and Bearman2019). This research relies on data from the Add Health study, which was supported by grant P01 HD31921 (Harris) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, along with contributions from 23 other federal agencies and foundations. The Add Health study was developed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill.
Author contribution
All authors have approved the final article. XP: Conceptualization, Formal analysis, Data interpretation, Writing – Original Draft; KB: Conceptualization, Formal analysis, Data interpretation, Writing – Review & Editing; RM: Data interpretation, Writing – Review & Editing; MC: Conceptualization, Data interpretation, Supervision, Writing - Review & Editing; GAB: Conceptualization, Methodology, Formal analysis, Writing – Review & Editing, Supervision.
Funding statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The authors declare that they conducted this research and analysis using their own resources. The study utilized a publicly available dataset that is freely accessible, and the authors have no financial or other relationships with the providers of this dataset. All authors confirm they received no payment or compensation related to this research.








