Introduction
Even in the world’s more developed countries, a considerable number of households struggle to make ends meet (Gornick & Jäntti, Reference Gornick, Jäntti, Kamerman, Phipps and Ben-Arieh2010). Although the exact circumstances that characterize poverty differ per region, around twenty percent of the children in high- and middle-income countries live in poverty based on their household income (UNICEF Office of Research, 2017). The mental health of individuals is partly shaped by their environment and childhood poverty is considered a major determinant of emotional and behavioral development (Duncan et al., Reference Duncan, Magnuson, Kalil and Ziol-Guest2012; Saitadze & Lalayants, Reference Saitadze and Lalayants2021). This highlights the importance of understanding how childhood poverty affects children’s well-being today.
Associations between low income and poor mental health have consistently been reported in studies across diverse populations (Costello et al., Reference Costello, Compton, Keeler and Angold2003; Knifton & Inglis, Reference Knifton and Inglis2020; Raphael, Reference Raphael2011). Growing up in a poor family or a family with low socioeconomic status has been related to a 2–4 times higher degree of psychopathology in children (Amone-P’Olak et al., Reference Amone-P’Olak, Burger, Ormel, Huisman, Verhulst and Oldehinkel2009; Dashiff et al., Reference Dashiff, DiMicco, Myers and Sheppard2009; Dearing et al., Reference Dearing, McCartney and Taylor2006; Gutman et al., Reference Gutman, Joshi, Parsonage and Schoon2015; Kinge et al., Reference Kinge, Øverland, Flatø, Dieleman, Røgeberg, Magnus and Torvik2021; Murali & Oyebode, Reference Murali and Oyebode2004; Peverill et al., Reference Peverill, Dirks, Narvaja, Herts, Comer and McLaughlin2021; Reiss, Reference Reiss2013), including higher rates of depression and anxiety symptoms (Kinge et al., Reference Kinge, Øverland, Flatø, Dieleman, Røgeberg, Magnus and Torvik2021; Melchior et al., Reference Melchior, Chastang, Walburg, Arseneault, Galéra and Fombonne2010), suicidal behavior (Fergusson et al., Reference Fergusson, Woodward and Horwood2000), attention-deficit hyperactivity disorder (Kinge et al., Reference Kinge, Øverland, Flatø, Dieleman, Røgeberg, Magnus and Torvik2021), and behavioral problems (Garratt et al., Reference Garratt, Chandola, Purdam and Wood2017). Experiencing mental health problems can lead to difficulties attending school or work, negatively affecting performance in these areas (Bubonya et al., Reference Bubonya, Cobb-Clark and Wooden2017; DeSocio & Hootman, Reference DeSocio and Hootman2004; Suldo et al., Reference Suldo, Thalji and Ferron2011). This often results in adverse socioeconomic outcomes later in life, such as being out of education or employment (Ringbom et al., Reference Ringbom, Suvisaari, Kääriälä, Sourander, Gissler, Ristikari and Gyllenberg2022; Veldman et al., Reference Veldman, Reijneveld, Almansa Ortiz, Verhulst and Bültmann2015) and lower income (Andersen & Gunes, Reference Andersen and Gunes2018; Evensen et al., Reference Evensen, Lyngstad, Melkevik, Reneflot and Mykletun2017; Philipson et al., Reference Philipson, Alaie, Ssegonja, Imberg, Copeland, Möller, Hagberg and Jonsson2020). Theories concerning socioeconomic status (SES, frequently assessed through income) can helpexplain these findings. Initially, the social causation hypothesis,which suggests that low SES leads to poorer health outcomes (Kröger et al., Reference Kröger, Pakpahan and Hoffmann2015), is likely applicable in childhood, since the child generally does not determine the family’s SES (Wadsworth & Achenbach, Reference Wadsworth and Achenbach2005). Next, when transitioning into adulthood, the health selection hypothesis may also become relevant, which posits that individuals with poor health may be more prone to lower future SES (Kröger et al., Reference Kröger, Pakpahan and Hoffmann2015).When considering the relation between childhood poverty and mental health, parental psychopathology can also play an important role. This may determine the family’s SES in accordance with the health selection hypothesis, while simultaneously increasing the risk for mental health problems in their offspring (Leijdesdorff et al., Reference Leijdesdorff, van Doesum, Popma, Klaassen and van Amelsvoort2017; Rasic et al., Reference Rasic, Hajek, Alda and Uher2013; Reiss, Reference Reiss2013). Taken together, these mechanisms are fueling a vicious circle between low income and mental health problems (Mossakowski, Reference Mossakowski, Cockerham, Dingwall and Quah2014), potentially shaping long-term health trajectories.
Adolescence is a critical phase for the development of physical, cognitive, and social-emotional functioning (Choudhury et al., Reference Choudhury, Blakemore and Charman2006; Nelson et al., Reference Nelson, Leibenluft, McClure and Pine2005; Sawyer et al., Reference Sawyer, Azzopardi, Wickremarathne and Patton2018; Steinberg, Reference Steinberg2005) and is also the period in which mental disorders often have their onset (Kessler et al., Reference Kessler, Berglund, Demler, Jin and Walters2005; Paus et al., Reference Paus, Keshavan and Giedd2008; Solmi et al., Reference Solmi, Radua, Olivola, Croce, Soardo, Salazar de Pablo, Il Shin, Kirkbride, Jones, Kim, Kim, Carvalho, Seeman, Correll and Fusar-Poli2022; Walker, Reference Walker2002). Adolescence is marked by the process of identity formation (Erikson, 1986), making adolescents especially vulnerable to poverty-related social processes, such as social disintegration (Böhnke, Reference Böhnke2008), and more family conflicts (Conger et al., Reference Conger, Ge, Elder, Lorenz and Simons1994).This may thus be a particularly informative stage for examining the relation between household income and mental health. Therefore, an integral test of the possible underlying mechanisms for the risk of poor mental health in adolescents from low-income households is warranted.
Research focussing on low income specifically or SES more generally has provided some insight into potential underlying mechanisms between household income and adolescent mental health, by describing potential mediating factors. Mediating factors may include characteristics related to the individual adolescent, such as cognitive abilities that may not fully develop under the pressure of poverty (Hair et al., Reference Hair, Hanson, Wolfe and Pollak2015; Mani et al., Reference Mani, Mullainathan, Shafir and Zhao2013), which may impact mental health (Melby et al., Reference Melby, Indredavik, Løhaugen, Brubakk, Skranes and Vik2020). Furthermore, children from low-income families experience less social support (Böhnke, Reference Böhnke2008) and more adverse childhood experiences (Walsh et al., Reference Walsh, McCartney, Smith and Armour2019), both being a risk factor for developing psychopathology (Chang et al., Reference Chang, Peng, Guo, Cai and Yip2020; Hughes et al., Reference Hughes, Bellis, Hardcastle, Sethi, Butchart, Mikton, Jones and Dunne2017; Rueger et al., Reference Rueger, Malecki, Pyun, Aycock and Coyle2016). Physical health also tends to be worse in adolescents from low-income households (Poulain et al., Reference Poulain, Vogel and Kiess2020; Spencer et al., Reference Spencer, Thanh and Louise2013), which can affect mental health (McCloughen et al., Reference McCloughen, Foster, Huws-Thomas and Delgado2012; Ohrnberger et al., Reference Ohrnberger, Fichera and Sutton2017).Mediators can also include parent-related factors, such as parenting practices (Bradley & Corwyn, Reference Bradley and Corwyn2002; Devenish et al., Reference Devenish, Hooley and Mellor2017; Letourneau et al., Reference Letourneau, Duffett-Leger, Levac, Watson and Young-Morris2013). Following the health selection theory, parental mental health may initially act as a confounding factor, in which it leads to both low family income and psychopathology in their offspring. Additionally, following the social causation theory, it also has the potential to act as a mediating factor, as demonstrated in previous studies regarding SES (Devenish et al., Reference Devenish, Hooley and Mellor2017; Letourneau et al., Reference Letourneau, Duffett-Leger, Levac, Watson and Young-Morris2013; Reiss, Reference Reiss2013). These studies suggest that low family income increases the risk of parental mental health problems, which in turn may negatively impact the mental health of their children. Next to individual and parental factors, neighborhood characteristics, for example neighborhood safety, may also serve as a mediator (Letourneau et al., Reference Letourneau, Duffett-Leger, Levac, Watson and Young-Morris2013). Besides mediating factors, variables such as ethnic background and parental IQ may serve only as confounders in the relation between income and adolescent mental health. These factors may influence both household income and mental health outcomes, but they do not necessarily represent causal mechanisms within this relation. For instance, ethnic background is linked to both SES and mental health problems (McLaughlin et al., Reference McLaughlin, Hilt and Nolen-Hoeksema2007; Williams et al., Reference Williams, Mohammed, Leavell and Collins2010). Consequently, adolescents from minority ethnic groups may be more likely to experience socioeconomic disadvantage, while also facing an increased risk of mental health problems. This dual vulnerability could confound the observed relation between low household income and mental health problems.
The current study aimed to examine the relation between household income and mental health in a contemporary population-based cohort of adolescents at risk for developing psychopathology. Drawing on existing theories related to SES, we hypothesized that low household income would be associated with higher rates of both internalizing (e.g., anxiety, depression) and externalizing (e.g., aggression, conduct problems) mental health issues in adolescents. We further hypothesized that this relationship would be explained or mediated by a range of factors:(1) adolescent characteristics including ethnic background, IQ score, perceived social support, adverse life events, and physical health concerns, which have been shown to be related to socioeconomic factors and to affect mental health; (2) parental characteristics including psychopathology, IQ score, and parent-child interaction problems, which have also been shown to be related to socioeconomic factors and to affect adolescent mental health;and (3) neighborhood characteristics including violent and sexual crime rates and unemployment rate, which may serve as contextual factors mediating the relation between income and mental health. This framework aligns with the social causation hypothesis, as well as the health selection hypothesis. In light of the complexity of the relation, it is essential to consider not only the direct effects of household income on adolescent mental health but also the roles that these additional variables play in the association. Therefore, despite employing a cross-sectional design, we tested whether some of these factors mediate the relation between low household income and adolescent mental health problems for exploratory purposes. Figure 1 presents a simplified directed acyclic graph (DAG) illustrating the hypothesized relations among key variables. Although these are tested cross-sectionally, based on previous studies, a likely direction of causality is indicated. Supporting references for each pathway depicted in the DAG are provided in the Supplementary Material. By integrating these factors, we aim to elucidate the mechanisms through which household income and related hardships impact adolescent mental health, thereby contributing to the development of more targeted and effective interventions.
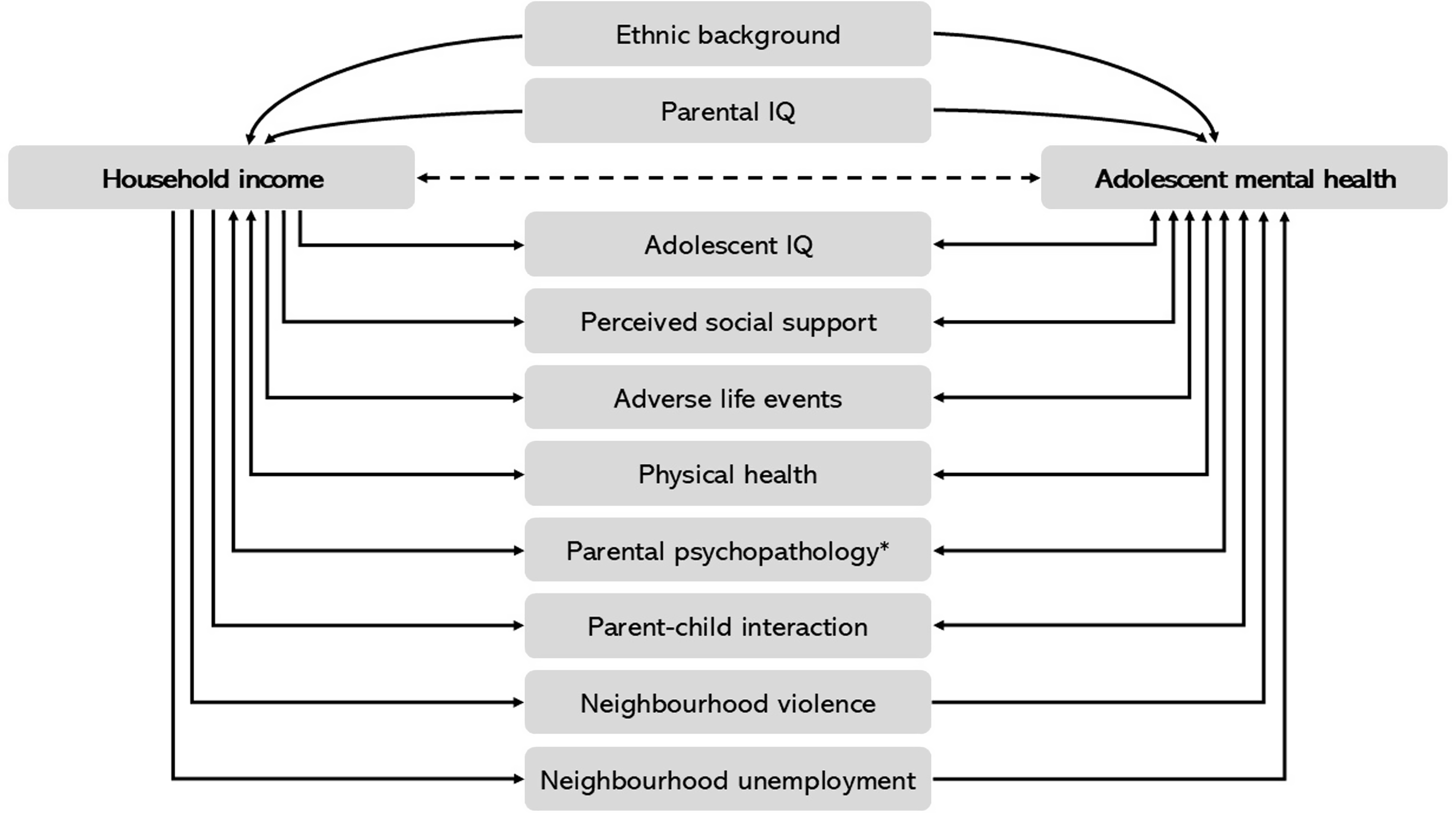
Figure 1. A simplified direct acyclic graph illustrating the tested relations between household income and adolescent mental health, including proposed third variables in the top and proposed mediating factors at the bottom. Note. the directions of the associations are based on previous literature (see Supplementary Material) but could not be formally tested due to the cross-sectional nature of our study. *Parental psychopathology may initially function as a confounding variable, influencing both household income and adolescent mental health problems.
Methods
Procedure and participants
The current study is embedded in the iBerry (Investigating Behavioral and Emotional Risk in Rotterdam Youth) Study, a population-based longitudinal cohort study to investigate determinants of psychopathology in youth. Details of the study design, sampling procedure, and study sample have been described in Grootendorst et al. (Reference Grootendorst-van Mil, Bouter, Hoogendijk, van Jaarsveld, Tiemeier, Mulder and Roza2021). Adolescents from the general population have been oversampled based on their risk for developing psychopathology using the Strengths and Difficulties Questionnaire-Youth (SDQ-Y) (van Widenfelt et al., Reference van Widenfelt, Goedhart, Treffers and Goodman2003). The SDQ-Y was administered to adolescents in their first year of high school as part of a routine health measurement. The SDQ-Y questionnaires of 16,736 adolescents were screened. Eligible adolescents scoring in the top 15% on the SDQ-Y and a random sample from the remaining 85% were invited to participate in the iBerry Study. This recruitment strategy targeted 1895 adolescents and their parents, ultimately resulting in the final cohort comprising 1022 adolescents (53.9% response rate [54.9% in the high-risk group, 51.7% in the low-risk group], mean age 15.0 years). Adolescents with high SDQ-Y scores were intentionally oversampled at a 2.5:1 ratio.
Participating adolescents and an accompanying parent were invited for a visit to the research center between 2015 and 2019. The other parent was asked to complete a set of questionnaires about themselves and the adolescent. Written informed consent was provided by the adolescent and their parents or legal guardian(s). The study protocol has been approved by the Medical Ethics Review Committee of the Erasmus MC, University Medical Center, Rotterdam.
Participants of the iBerry Study were recruited in the greater Rotterdam area of the Netherlands, which is considered a high-income country. However, 13.2% of the Dutch families were living below the national poverty line in 2019 (Statistics Netherlands, 2019c). In 2018, 8.1% of underage children lived in a low-income family (Statistics Netherlands, 2019b). Despite its relatively small country size, poverty rates differ greatly per region. In the Rotterdam region, child poverty rates are more than double the national average, with 17.5% of young people residing in low-income households (Statistics Netherlands, 2019b).
Instruments
Household income
The accompanying parent provided information on the household income, which was defined as the total net monthly income, excluding money from (holiday) bonuses and (housing or child) benefits. The parent could select one of 11 answer options ranging from <800 euros to ≥4400 euros, with each answer option increasing by 400 euros. The cut-off for low income was set at the 20th percentile, <2000 euros, which closely corresponds with the percentage of Rotterdam youth living below the poverty line (Statistics Netherlands, 2019b) and the Dutch national poverty line for a couple with two children (1960 euros) (Statistics Netherlands, 2019a). For sensitivity analysis, alternative cut-offs were set at the 12th (<1600 euro) and 28th (<2400 euro) percentiles.
Adolescent internalizing and externalizing problems
Two questionnaires of the Achenbach System of Empirically Based Assessment (ASEBA) instruments were used to determine adolescent internalizing and externalizing problems (Achenbach & Rescorla, Reference Achenbach and Rescorla2001; Verhulst & van der Ende, Reference Verhulst and van der Ende2013). The Youth Self-Report (YSR) assessed self-reported problems and the Child Behavior Checklist (CBCL/6-18) was completed by the accompanying parent. Both consisted of 112 items about the adolescent’s behavior over the past six months that were answered on a 3-point scale ranging from not true (0) to very often or often true (2). The subscales Internalizing Problems and Externalizing Problems were computed separately for the YSR and the CBCL, with higher scores indicating more problems.
Adolescent individual characteristics
Demographic characteristics
Several sociodemographic characteristics were assessed, including the adolescent’s sex and age. The accompanying parent provided information on the adolescent’s ethnic background, categorized as Dutch (both the adolescent and their parents born in the Netherlands) or non-Dutch (at least one born abroad), based on the country of birth.
IQ score
Two subscales of the Snijders-Oomen Nonverbal Intelligence Test (SON-R 6-40) (Tellegen & Laros, Reference Tellegen and Laros2011) were administered to obtain an indication of the IQ score for the adolescent. The administered subtests Categories and Analogies both have a strong correlation with the sum of the other categories and highly correlate with other IQ measures like the WISC-III/IV (Tellegen & Laros, Reference Tellegen and Laros2011). The combined score of the subtests was multiplied by two to obtain a total IQ score indication. IQ scores were adjusted for the Flynn effect (Pietschnig & Voracek, Reference Pietschnig and Voracek2015; Trahan et al., Reference Trahan, Stuebing, Fletcher and Hiscock2014).
Perceived social support
Perceived social support was measured using the Multidimensional Scale of Perceived Social Support (Zimet et al., Reference Zimet, Dahlem, Zimet and Farley1988). This self-report questionnaire consists of 12 items about the perceived social support of family, friends, and significant others. The total score was used to obtain a measure of perceived social support, with higher scores indicating better perceived social support.
Adverse life events
The accompanying parent was asked to report about adverse life events experienced by their child during a structured interview based on the stressful life events questionnaire used in the TRAILS study (Amone-P’olak et al., Reference Amone-P’Olak, Burger, Ormel, Huisman, Verhulst and Oldehinkel2009; Oldehinkel & Hartman, Reference Oldehinkel and Hartman2003). Among the 13 assessed events were physical and sexual violence, severe illness or death of close relatives or friends, hospitalization of parents, divorce/separation of parents, living elsewhere for an extensive period, hospitalization, repeating classes, and changing schools. Each event was coded as present or not present during the adolescent’s life. The total number of different experienced adverse life events was computed.
Physical health
The general physical health of the adolescent was rated by the accompanying parent as excellent, very good, good, moderate, or poor. They were also asked to indicate whether their child suffered a chronic illness and, if so, which disease. Based on criteria compiled by the Verwey-Jonker Institute, a physician evaluated the responses to determine whether they met the criteria for a physical chronic condition (van Hal et al., Reference van Hal, Tierolf, van Rooijen and van der Hof2019). Answers were combined into a single indicator with two categories: “no physical health concerns” (no physical chronic condition and health rated as excellent, very good, or good) and “physical health concerns” (physical chronic condition and/or health rated as moderate or poor).
Parental characteristics
IQ score
The SON-R-40 (Tellegen & Laros, Reference Tellegen and Laros2011) was administered to the accompanying parent in the same way as it was to the adolescent.
Parental psychopathology
The Brief Symptom Inventory measured parental psychopathology through 53 items about the past week, covering nine symptom dimensions (De Beurs, Reference De Beurs2004). For both parents, the mean item score was calculated to obtain the Global Severity Index, with higher scores indicating a higher degree of parental psychopathology.
Parent-child interaction
The Parent-Child Interaction Questionnaire-Revised (OKIV-R) child version was filled in by the adolescent separately about their mother and their father (Lange et al., Reference Lange, Evers and Jansen2000). The 25 items asked about their perceived interaction with that specific parent. Total scores were computed independently for the perceived quality of interaction with the mother and with the father, with higher scores indicating better quality.
Neighborhood characteristics
We matched publicly available neighborhood data from Statistics Netherlands (CBS) (Bresters, Reference Bresters2019; Statistics Netherlands) to the adolescent’s home address:
Percentage out of labor force
Neighborhood inhabitants who, based on their age, belong to the labor force but do not gain their main income from labor or owning a business as a percentage of the total labor force.
Relative number of crimes
This number comprised all yearly registered violent and sexual crimes in the neighborhood per 1,000 inhabitants.
Statistical analyses
Data were analyzed using IBM SPSS Statistics Version 28.0.1.0 (IBM Corp., 2021). Differences in sociodemographic characteristics and psychopathology scores between adolescents from low-income and higher-income households were assessed. Chi-square tests were performed for categorical characteristics and t-tests for continuous variables. Pearson correlations were computed for continuous adolescent individual, parental, and neighborhood factors, point biserial correlations for dichotomous factors with continuous factors, and Phi coefficients for correlations between dichotomous factors.
Hierarchical multiple linear regression analyses were performed for the different outcome measures: YSR Internalizing Problems, YSR Externalizing Problems, CBCL Internalizing Problems, and CBCL Externalizing Problems. Model 1 included household income, adolescent sex, and age to determine the crude effect estimate of household income. In model 2, adolescent ethnicity, IQ score, perceived social support, adverse life events, and physical health were added to determine the additional effect of adolescent individual characteristics. In model 3, IQ score of the accompanying parent, parental psychopathology, and parent-child interaction were added to model 1 to determine the effects of parental characteristics. In model 4, the percentage out of labor force and the relative number of crimes were added to model 1 to establish the effect of neighborhood characteristics. The complete model included all of the previously mentioned factors. A p-value of < .05 was considered significant. To resolve the violated normality and homoscedasticity assumptions, a square root transformation of the outcome measures (YSR and CBCL) was used.
To verify the robustness of the observed associations, analyses were repeated with the 12th and 28th percentile cut-off for low household income as a sensitivity analysis.
For exploratory analyses, we performed mediation models using the PROCESS macro version 4.1 (Hayes, Reference Hayes2022) (5000 bootstraps), adjusting for sex and age. This allowed us to test whether the proposed potential mediating characteristics that were significant covariates in the linear regression models could indeed serve as mediating factors. Since mediation analyses cannot be performed with dichotomous variables, we used the general physical health score instead of physical health problems.
Missing data
Adolescents with missing data on household income or psychopathology were excluded from analyses (n = 150). Most missingness occurred because there was no participating parent, and therefore data on household income were lacking. We compared the excluded participants with the included participants on available characteristics and internalizing and externalizing scores (see Supplementary Table S1). Excluded participants were slightly older (t (187.24) = 6.70, p < .001) and lived more often in an urban environment (χ2 (2, N = 1022) = 10.23, p = .006). Excluded participants did not differ from the included participants based on sex, ethnic background, education level, or self- or parent-reported internalizing and externalizing problems. The intentional oversampling of high SDQ-Y scores at a 2.5:1 ratio was retained in the current study sample.
For the instruments used, if up to 25% of items were missing, these were corrected using the participant’s mean item score on the relevant subscale. Multiple imputation using the Markov chain Monte Carlo method and Predictive Mean Matching was used to correct for missing data in the covariates (number of imputations = 15, maximum iterations = 30). Covariates with missing data included ethnic background (0.3% missing), adolescent IQ score (5.5%), perceived social support (10.6%), adverse life events (5.6%), physical health concerns (8.5%), parental IQ-score (6.0%), maternal psychopathology (9.5%), paternal psychopathology (33.5%), mother-child interaction problems (29.4%), father-child interaction problems (31.7%), neighborhood percentage out of labor force (1.1%), and neighborhood crimes (0.5%). Auxiliary variables included sex of the parent, parental education level, adolescent scores on the Parent-Child Conflict Tactics Scale (Jansen et al., Reference Jansen, Raat, Mackenbach, Hofman, Jaddoe, Bakermans-Kranenburg and Tiemeier2012; Straus et al., Reference Straus, Hamby, Finkelhor, Moore and Runyan1998) separately for mother and father, and neighborhood address density. For the exploratory mediation analyses, the original, non-imputed data were used.
Results
Demographic characteristics and internalizing and externalizing problems of the 872 adolescents included in the current study are presented in Table 1. The mean adolescent age was 14.93 years (SD = 0.88) and 50.7% of the sample was female. A net monthly household income below 2000 euros was reported by 19.8% of the parents.
Table 1. Sociodemographic characteristics and psychopathology scores of the adolescents
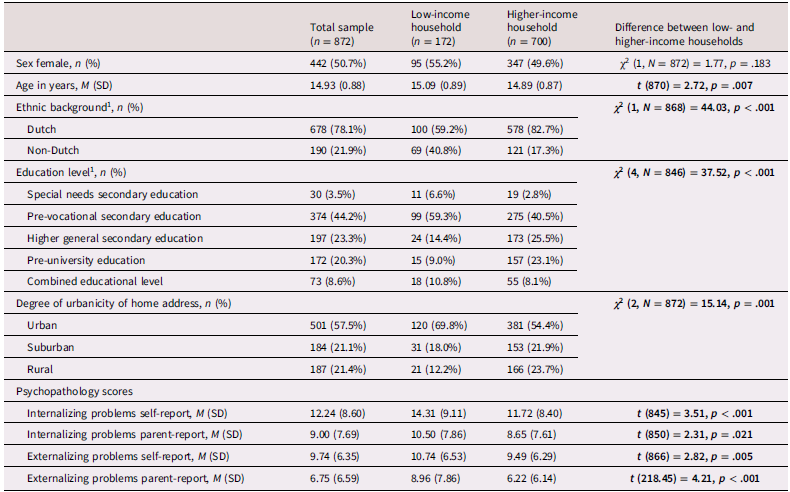
1Ethnic background was missing for 4 adolescents, education level was missing for 26 adolescents.
A slightly higher age, non-Dutch background, lower education level, and an urban living environment were more common in adolescents in the low-income group compared to peers from higher-income households. Additionally, the adolescents from low-income households had higher levels of self- and parent-reported internalizing and externalizing problems, compared to peers from higher-income households.
Absolute correlations between characteristics ranged between .007 and .366 (see Supplementary Table S2).
Adolescent internalizing problems
Table 2 provides an overview of the association between low household income and self- or parent-reported internalizing problems adjusted for the different characteristics. Adolescents from low-income households showed increased self- and parent-reported internalizing problems compared to those from higher-income households when adjusting only for adolescent age and sex. However, this relation disappeared after adding other individual characteristics in the second model, or after adding parental characteristics in model 3, and in the full model adjusting for all covariates. Adding only neighborhood characteristics to the model (model 4) did not explain the relation between low income and internalizing problems.
Table 2. Linear regression coefficients on the relationship between low household income and adolescent internalizing problems (n = 847 for self-report and n = 868 for parent-report)
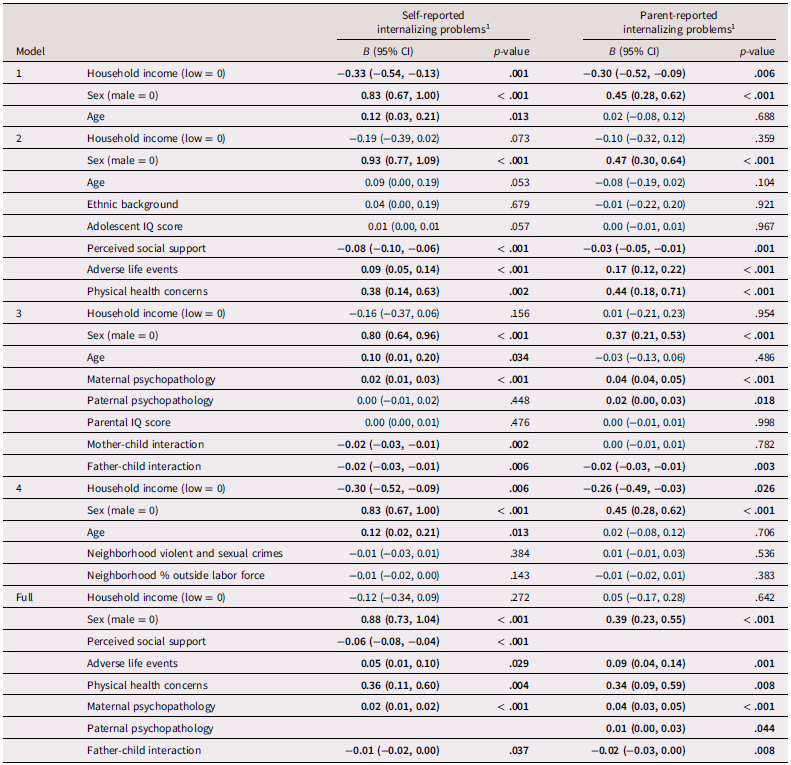
Note. In the full model, only covariates that were significantly related to self- or parent-reported internalizing problems are reported. Significant associations are printed in bold.
1 Square root transformation
The full models, including all covariates, showed that the relation between low income and internalizing problems could be explained by more adverse life events, the presence of physical health concerns, higher levels of maternal psychopathology, and worse father-child interaction. Depending on the informant of adolescent internalizing problems, this also included lower perceived social support (self-reported internalizing problems), and higher levels of paternal psychopathology (parent-reported internalizing problems). Mother-child interaction did explain the relation between low income and self-reported internalizing problems within the model with only parental factors (model 3), but not in the full model. The same applied to perceived social support and parent-reported internalizing problems, which were significant in the model with only individual factors, but not in the full model.
Adolescent externalizing problems
Table 3 provides an overview of the association between low household income and self- or parent-reported externalizing problems. For externalizing problems, we observed a similar pattern in the relation with low income. Adolescents from low-income households had increased self- and parent-reported externalizing problems compared to those from higher-income households, when adjusting only for adolescent sex and age. After including individual characteristics in model 2, the relation between low income and self-reported externalizing problems was no longer significant and was also absent after adding parental characteristics in model 3, and in the full model. Adding only neighborhood characteristics to the model (model 4) did not explain the relation between low income and externalizing problems. For parent-reported externalizing problems, low income was still related to more parent-reported externalizing problems in adolescents when adjusting for other individual characteristics in model 2 or neighborhood factors in model 4. After adding parental characteristics in the third model, there was no longer a significant effect, and the effect was also absent in the full model.
Table 3. Linear regression coefficients on the relationship between low household income and adolescent externalizing problems (n = 852 for self-report and n = 867 for parent-report)
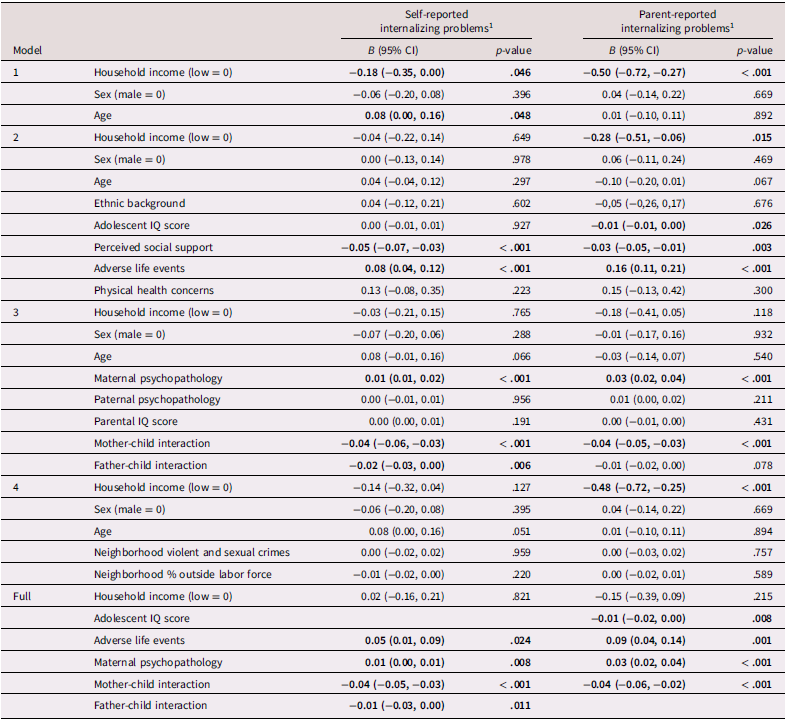
Note. In the full model, only covariates that were significantly related to self- or parent-reported externalizing problems are reported. Significant associations are printed in bold.
1 Square root transformation
The full models, including all covariates, showed more adverse life events, higher levels of maternal psychopathology, and worse mother-child interaction to better explain the association between low-income and adolescent externalizing problems. For self-reported externalizing problems, this also included worse father-child interaction. For parent-reported externalizing problems, this also concerned lower IQ score of the adolescent. Perceived social support explained the relation between low income and externalizing problems within the models that included only individual factors (model 3). However, this relation was not explained by perceived social support in the full models that included all covariates.
Sensitivity analyses
Sensitivity analyses using the 12th and 28th percentiles as alternative low-income cut-offs yielded minimal differences in estimated coefficients and p-values, especially in the full model (see Supplementary Tables S3-S4). The direction of significant associations did not change. However, when using the 28th percentile, low income was still associated with self- and parent-reported internalizing problems after adding individual factors (model 2) and with self-reported internalizing problems after adding parental factors (model 3). For parent-reported internalizing problems, the relation with household income was no longer observed after adjusting for neighborhood factors (model 4) when using the 12th percentile, despite none of the neighborhood factors being related.
Furthermore, when using the 12th and 28th percentiles, we found no association at all between self-reported externalizing problems and low income. For parent-reported externalizing problems, using the 12th percentile, the relation with income became non-significant after adding individual characteristics (model 2). Using the 28th percentile, low income was still significantly related to more parent-reported externalizing problems when adjusting for parental characteristics and the full model, adjusting for individual, parental and neighborhood characteristics.
Exploratory mediation analyses
The significant proposed mediating factors were analyzed as potential mediators (see Supplementary Table S5 for the indirect effects). The results indicated that perceived social support, number of adverse life events, maternal psychopathology, and father-child interaction could serve as potential mediators between low household income and adolescent internalizing and externalizing problems. Physical health condition was a potential mediator for internalizing problems, paternal psychopathology for parent-reported internalizing problems, and adolescent IQ score for parent-reported externalizing problems. Mother-child interaction does not seem to be a mediator in the relation between low income and adolescent internalizing and externalizing problems.
Discussion
The current study aimed to further clarify the relation between household income and adolescent mental health in a contemporary cohort. Low household income was related to higher levels of self- and parent-reported internalizing and externalizing problems in adolescents. In line with our hypothesis, we observed that several adolescent and parental factors underlie this relation. Neighborhood characteristics did not account for this association. Although our results highlight the need for a nuanced understanding of how poverty affects different types of mental health issues, they also underscore the urgency of addressing these challenges. Given the robust evidence supporting the multifaceted effects of poverty on mental health, it is crucial to develop and implement interventions that target these underlying socioeconomic factors.
In particular, adverse life events, maternal psychopathology, and parent-child interaction problems seem to be important factors in the association between low household income and adolescent internalizing and externalizing problems. For internalizing problems, physical health concerns contributed to the outcome as well. Other underlying factors were the IQ score of the adolescent, perceived social support, and paternal psychopathology, although explanatory power differed depending on the type of problems (internalizing versus externalizing) and the informant. Exploratory cross-sectional analyses suggested a mediating role for all of these factors except for mother-child interaction. Contrary to our hypotheses, neighborhood characteristics - specifically crime rates and the percentage of unemployed individuals - did not clarify the relation between low household income and adolescent mental health. One possibility is that adolescents at this age engage in a variety of social, sports, and educational activities outside their direct neighborhood, allowing them to interact with different communities. Furthermore, it could be that other neighborhood factors than those used in the current study, i.e. number of crimes and number of people out of the labor force, are relevant for the income-mental health relation in adolescents. For example, the subjective feeling of unsafety may be more pertinent (Austin et al., Reference Austin, Furr and Spine2002; Baba & Austin, Reference Baba and Austin1989).
These results are mostly in line with previous reviews and meta-analyses, which have shown a relation between low socioeconomic status (mainly defined by income) and adolescent internalizing and externalizing problems (Peverill et al., Reference Peverill, Dirks, Narvaja, Herts, Comer and McLaughlin2021; Reiss, Reference Reiss2013). Importantly, our study showed that the effect of low income could be explained by other factors. Theories of social causation and health selection provide useful frameworks for understanding the mechanisms behind these associations. The factors included in our study likely act as mediators in the causal pathway between low income and adolescent mental health. For example, the relation between low income and mental health could be mediated by father-child interaction problems, where the stress faced by families with low incomes could impact family dynamics and, in turn, contribute to mental health difficulties in adolescents. Nevertheless, the question of causality remains complex. While the health selection theory suggests that families with pre-existing mental health conditions are more likely to experience financial hardship, and the social selection theory proposes that low family SES makes them vulnerable to mental health problems, the cross-sectional design of our study limits our ability to establish (the direction of) causality. The relation between low income and poor mental health in general may be bidirectional. As we specifically considered family SES and adolescent mental health, this relation is even more complex, as household poverty may cause or exacerbate mental health problems in adolescents, which in turn may constrain their own future economic opportunities, creating a cycle of disadvantage.
In addition to identifying explanatory factors in the relation between low income and adolescent mental health, we also provided insight into how different thresholds of low income can influence results. Our 20th percentile cut-off aligned with national data. Nonetheless, there is an ongoing societal debate regarding the most appropriate cut-off. While directions of associations remained consistent across the different income cut-offs we used, magnitude and significance varied in some cases. Overall, associations between low income and internalizing and externalizing problems tended to be more robust when applying a higher cut-off for defining low income. Differences in significant results can partly be attributed to increased statistical power when applying a higher cut-off and decreased power when using a lower cut-off, as the size of the low-income group changes. Another explanation might be that adolescents from families with incomes just above the nationally defined low-income line may suffer from similar or even additional problems as those below the poverty line. Families whose incomes slightly exceed the nationally defined poverty line might not benefit as much from measures aimed at supporting the poorest, such as benefits and allowances, potentially resulting in less disposable income (Netherlands Institute for Social Research, 2024).
Additionally, we observed differences in associations with internalizing and externalizing problems. More factors seem involved in the relation with internalizing than with externalizing problems. Specifically in the relation with internalizing problems, physical health problems consistently served as an explanatory factor. The relation between low income and parent-reported externalizing problems seemed to be mainly explained by including parental factors in the model, while for the other associations (i.e. with internalizing problems and self-reported externalizing problems)individual factors could also fully explain the effect. The well-known Great Smoky Mountains Study (Costello et al., Reference Costello, Compton, Keeler and Angold2003) also underscores this distinction in the differential effects of low income on internalizing versus externalizing problems. The study found that when families moved out of poverty, there was a significant reduction in externalizing behaviors like aggression, which are more directly influenced by the stressors associated with economic hardship. These behaviors are often more observable and linked to immediate environmental stressors, making them more responsive to changes in family income. In contrast, internalizing problems such as anxiety and depression were not as quickly alleviated by the same economic relief. This could be due to the more complex, enduring nature of internalizing issues, which, as our findings indicate, can also be connected to physical health problems.
Given the complex relation between income and health, we have accounted for a variety of factors that were often not simultaneously captured in previous studies. Furthermore, the influence of low income on young people can vary among countries due to differences in social welfare policies and programs. While higher-income countries such as the Netherlands may have preventive interventions to alleviate the impact of poverty, it is important to recognize that poverty exists and persists across all nations, even among the wealthiest. In the Netherlands, a relatively egalitarian country, this disparity is notably illustrated by the fact that the average life expectancy is eight years shorter for women and nine years shorter for men in the lowest 20% income bracket, compared to those in the highest 20% income bracket (Statistics Netherlands, 2022). These recent figures, along with the current findings from our temporary population-based cohort, vividly illustrate the disparities in health outcomes within a high-income country that persist up to this day. Our cohort of adolescents from the general population with oversampling on high risk of developing psychopathology made it possible to investigate a variety of factors that potentially underlie the relation between income and mental health. Previous studies adjusting for only a few covariates do not do justice to the very complex relations we are looking at in reality (Reiss, Reference Reiss2013). With our comprehensive approach, we aimed for a more accurate understanding of how multiple individual, social, and parental factors interact to influence adolescent mental health in the context of income disparities. We observed important changes in associations when adjustments were made, and we identified potential mediators, resulting in a more nuanced view of the income-mental health relation in adolescents. Another strength of the study is the use of both adolescent and parental instruments to assess adolescent mental health problems. Different informants may provide unique perspectives and insights into the adolescent’s behavior, emotions, and functioning, resulting in a more balanced and reliable assessment.
One important limitation of our study is the cross-sectional design, we were therefore unable to test the causal relation, and the mediation outcomes should be interpreted in a suggestive manner only. Nonetheless, our results do provide important insights for future longitudinal studies which aim to determine the direction of causality and mediating pathways. There seem to be important adolescent and parental characteristics that should be included in analyses as they could act as confounding or mediating variables in the causal pathway between income and mental health, which can be of high clinical importance. Additionally, the use of a high-risk sample may limit the generalizability of the findings to the broader adolescent population. However, this design enabled us to achieve sufficient power to detect small effects while minimizing sample size requirements. Importantly, prior research suggests that the bias introduced by oversampling is minimal and does not typically compomrise the validity of behavioral research results (Hauner et al., Reference Hauner, Zinbarg and Revelle2014). Another limitation is that there was no formal, well-defined cut-off for low income available and only income data provided by one parent was used. However, the prevalence of low income, 19.8% in our sample, and the cut-off amount of 2000 euros align well with regional or national figures (Statistics 2019b, Netherlands, 2019a). Sensitivity analyses using other cut-off points showed only minor deviations, suggesting the robustness of our findings. Additionally, adolescents were excluded from the current study if they participated solely, as income data was provided by the parent. Nonetheless, we could compare the included and excluded groups based on sociodemographic characteristics and internalizing and externalizing problems. The excluded adolescents more often lived in an urban environment, suggesting that caution is necessary when generalizing results to this subgroup. Lastly, caution should also be warranted when generalizing results to other countries. The definition of low income in this study was relative to other households from the same region and country. Although differences exist, the Netherlands has comparable poverty risks and similar mental healthcare systems to other European countries, such as Belgium, France, and Austria (Eurostat, 2019; OECD, 2021). Results from our study might be more applicable to these countries compared to other countries, particularly low-income countries, where the impact of living in a low-income family could vary significantly. This variation underscores the importance of contextual factors when interpreting the relation between income and mental health across diverse settings.
The current study provides leads for future research. It has shown the importance of including various types of covariates and using multi-informant assessments. Both can impact the results and conclusions drawn from them. One should consider the possibility that these factors play a mediating role in the causal pathway. While the direct relation between income and adolescent mental health may not be apparent when considering these factors, the clinical relevance of household income should not be overlooked. Lower income levels can be associated with multiple factors that adversely affect an adolescent’s mental health, indicating broader challenges within a family. Future research should explore the interactions and contributions of these variables to adolescent mental health outcomes. Understanding these interrelations can inform the development of more effective interventions and support for families experiencing financial hardship.
Our findings have elucidated that low income can serve as a comprehensive risk indicator, embodying numerous factors that can serve as determinants of adolescent mental health. This underscores the necessity of a comprehensive, multi-faceted approach to address the impact of poverty on adolescent mental health. The research suggests potential pathways for preventive interventions, targeting factors such as physical health, parental psychopathology, parent-child interaction problems, adverse life events, and social support, while taking into account adolescent IQ level. Programs providing social and emotional support, mental health resources for parents, and initiatives promoting physical health and intellectual development in adolescents can address the broader implications of poverty on mental health. Recently, various initiatives worldwide have already taken steps to support low-income families, such as local governments providing direct cash payments or offering debt relief programs to low-income residents (Conway, Reference Conway2021; Kamphuis, Reference Kamphuis2024; Kangas et al., Reference Kangas, Jauhiainen, Simanainen and Ylikännö2019). Ideally, these initiatives would be accompanied by family assistance targeting related problem areas, and standardized measures of internalizing and externalizing mental health problems would be used before and after the intervention to assess changes.
Conclusion
Our study sheds light on the relation between low household income and adolescent mental health within a contemporary Dutch cohort. Increased internalizing and externalizing problems can be attributed to individual and parental characteristics, but not to neighborhood factors. These findings highlight the need to address childhood poverty, which remains prevalent even in developed nations and is linked to multiple problem domains. The complex interplay of factors related to poverty may ultimately result in mental health problems in adolescents, perpetuating a vicious circle of inequality throughout their lives.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579425100266.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions. Other researchers are welcome to collaborate with researchers in the iBerry Study group and to request access to the data. Proposals to collaborate will be assessed by the iBerry Study group with respect to quality, feasibility, and potential overlap with planned or published publications.
Acknowledgments
We thank the iBerry research team, including master’s students, research assistants, PhD students, managers, and collaborating clinicians, for their assistance with the data collection.
Author contribution
Conceptualization: all authors; Data curation: DB; Formal analysis: SR; Investigation: SR, DB, NdN-E; Methodology: SR, NG-vM; Project administration: SR, DB, NdN-E, NG-vM; Supervision: WH, NG-vM; Writing - original draft: SR; Writing - review & editing: all authors.
Funding statement
The iBerry Study is funded by the Erasmus MC, Erasmus University Medical Center and the following institutes of mental health care (GGz): Parnassia Psychiatric Institute Antes, GGzBreburg, GGzDelfland, GGzWestelijk Noord-Brabant and Yulius. All funding organizations participate in the Epidemiological and Social Psychiatric Research Institute (ESPRi), a consortium of academic and non-academic research groups. The current study is also funded by StichtingtotSteun VCVGZ (NG-vM, SR, grant number 280).
Competing interests
The authors declare that they have no conflict of interest.
Ethics approval
This study was conducted in accordance with the guidelines of the World Medical Associations Declaration of Helsinki and was approved by the Medical Ethics Committee of the Erasmus MC, Erasmus University Medical Center, Rotterdam. Procedures were fully explained to the participants. Both adolescents and their parent(s) or legal guardians gave written informed consent to participate in the study.







