Background
Opioid use disorder (OUD) is a medical condition characterized by the problematic use of opioids that leads to significant distress or impairment (Bergeria and Strain, Reference Bergeria and Strain2022; Taylor and Samet, Reference Taylor and Samet2022). It includes both the compulsive use of opioids and the inability to control opioid use, which is shown as craving and dependence, despite negative consequences in personal, social or professional life (Strang et al., Reference Strang, Volkow, Degenhardt, Hickman, Johnson, Koob, Marshall, Tyndall and Walsh2020). The disorder contributes to a substantial disease burden and high mortality rates (Degenhardt and Hall, Reference Degenhardt and Hall2012; Degenhardt et al., Reference Degenhardt, Whiteford, Ferrari, Baxter, Charlson, Hall, Freedman, Burstein, Johns, Engell, Flaxman, Murray and Vos2013). In 2010, an estimated 15.5 million people globally suffered from opioid dependence (Degenhardt et al., Reference Degenhardt, Charlson, Mathers, Hall, Flaxman, Johns and Vos2014), and by 2016, this number had surged to 26.8 million (GBD 2016 Alcohol and Drug Use Collaborators 2018). The sharp increase in OUD cases can be attributed to several factors, including the increased misuse of prescription opioids, proliferation of illicit opioids and deficiencies in public health policy. These issues are particularly pronounced in high-income countries, where OUD is closely tied to the alarming rise in opioid overdose deaths and burden (Ellis et al., Reference Ellis, Dunn and Huhn2024; The US Burden of Disease Collaborators, 2018).
Previous studies, notably from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD), highlighted OUD’s regional disparities. GBD 2010 identified high burdens in North America, Eastern Europe and sub-Saharan Africa (Degenhardt et al., Reference Degenhardt, Charlson, Mathers, Hall, Flaxman, Johns and Vos2014), while GBD 2019 focused on South America, revealing distinct drug use patterns (Castaldelli-Maia et al., Reference Castaldelli-Maia, Wang, Brunoni, Faro, Guimarães, Lucchetti, Martorell, Moreira, Pacheco-Barrios, Rodriguez, Roever, Silva, Tovani-Palone, Valdez, Zimmermann, Culbreth, Hay, Murray and Bensenor2023). However, systematic evaluations of OUD’s global burden have been limited since GBD 2010. The COVID-19 pandemic likely exacerbated OUD prevalence due to healthcare shifts and socio-economic changes, yet its impact remains under-assessed (Alexander et al., Reference Alexander, Stoller, Haffajee and Saloner2020; Haley and Saitz, Reference Haley and Saitz2020).
This study addresses these gaps by analysing OUD burden at global, regional and national levels using GBD 2021 data (1990–2021), stratified by sex, age and the socio-demographic index (SDI). This analysis aims to reveal the unobserved conditions and provide a scientific basis for developing effective prevention and treatment strategies, particularly to address the opioid crisis.
Methods
Overview
The data used in this study was extracted from the GBD 2021 study (GBD 2021 Diseases and Injuries Collaborators 2024). The University of Washington Institutional Review Board waived the requirement for informed consent to access the GBD data. The research adhered to the Guidelines for Accurate and Transparent Health Estimates Reporting (Stevens et al., Reference Stevens, Alkema, Black, Boerma, Collins, Ezzati, Grove, Hogan, Hogan, Horton, Lawn, Marušić, Mathers, Murray, Rudan, Salomon, Simpson, Vos and Welch2016).
Data source
The GBD 2021 data on OUD is available from the Global Health Data Exchange (GHDx) system. Additionally, the GBD population forecasts for 2017–2100 (Institute for Health Metrics and Evaluation (IHME), 2020) were obtained to predict the burden of OUD from 2022 to 2040. Furthermore, the SDI is a crucial metric in the GBD study, which is used to quantify the level of socio-economic development across countries and regions (GBD 2021 Diseases and Injuries Collaborators 2024; GBD 2021 Lower Respiratory Infections and Antimicrobial Resistance Collaborators 2024). The SDI is constructed based on data from three core dimensions: fertility rate, educational attainment and per capita income. By integrating statistical data from these three dimensions, the GBD study classifies countries and regions worldwide into five SDI categories: low, low-middle, middle, middle-high and high SDI. This classification enables researchers to better analyse the relationship between socio-economic development and the burden of OUD. Individuals were assessed for OUD using the International Classification of Diseases version 10 codes. OUD is defined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition as a ‘pattern of opioid use that results in clinically significant impairment or distress, as evidenced by the presence of at least two of eleven specified criteria’ (American Psychiatric Association, 2013).
Statistical analyses
The details of the methods, including the data estimation framework and the interpretation of the model, are provided in the Supplementary Methods section. Metrics of the OUD burden included prevalence, incidence, mortality and disability-adjusted life years (DALYs), all of which refer to age-standardized rates unless otherwise specified. Uncertainty intervals (UIs) are used to quantify uncertainty in disease burden estimates (GBD 2021 Risk Factors Collaborators 2024).
The age-standardized rate per 100,000 population is obtained by summing the products of the age-specific rates and the number of persons (or weight) in the same age subgroup of the chosen reference standard population, and then dividing by the sum of the standard population weights. The formula is expressed as follows:
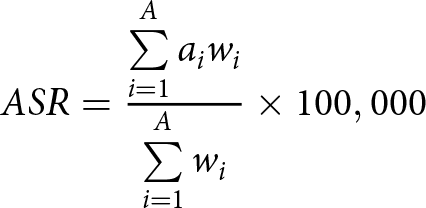 \begin{equation*}ASR = \frac{{\sum\limits_{i = 1}^A {{a_i}{w_i}} }}{{\sum\limits_{i = 1}^A {{w_i}} }} \times 100,000\end{equation*}
\begin{equation*}ASR = \frac{{\sum\limits_{i = 1}^A {{a_i}{w_i}} }}{{\sum\limits_{i = 1}^A {{w_i}} }} \times 100,000\end{equation*}where ai is the age-specific rate for the i age group; wi is the number of persons or weight in the ith age group of the standard population; and A is the total number of age groups.
The average annual percentage change (AAPC) is used to describe the average rate of change of a variable over a specific time period, helping to determine the trend in the OUD burden (Kim et al., Reference Kim, Fay, Feuer and Midthune2000). The AAPC was performed using Joinpoint software (Version 5.3.0). If the 95% confidence interval (CI) of the AAPC estimate is greater than 0, the age-standardized indicator shows an increasing trend during the study period; if it is less than 0, it indicates a decreasing trend; and if it includes 0, it suggests no significant change. Spearman’s correlation is used to assess the relationship between SDI and the age-standardized rates of OUD (Li et al., Reference Li, Kong, Yang, Cheng, Lv, Guo and Liu2024).
The age-period-cohort model was used to evaluate the effects of age, period and cohort on the burden of OUD (Li et al., Reference Li, Ning, Shen, Shi, Song, Fang and Ding2023). The age effect refers to the impact of individual ageing on health outcomes. The period effect reflects the influence of social, economic or environmental factors in different time periods on all age groups. The cohort effect captures the specific health risks or behavioural patterns of people born in similar historical or social contexts due to shared life experiences. The log-linear regression model is as follows: log(Ya ,p) = μ + αa + βp + γc + εa ,p, where Ya ,p is the observed value for age a in period p, μ is the intercept, and α, β and γ are the coefficients for age, period and cohort, respectively. εa ,p denotes the residual term. The intrinsic estimator method integrated into the age-period-cohort model was used to obtain the net effects of the three dimensions. Additionally, the Bayesian age-period-cohort model with integrated nested Laplace approximations was employed to predict future trends in OUD burden from 2022 to 2040 due to its superior coverage and precision (Knoll et al., Reference Knoll, Furkel, Debus, Abdollahi, Karch and Stock2020; Wu et al., Reference Wu, Li, Shi, Zhang, Lai, Cui, Bai, Xiang, Geng, Liu, Jiao, Wu, Yang, Zhang, Liu, Tian and Li2024). The statistical analyses were conducted using R software (Version 4.4.1). A p-value of <0.05 was considered statistically significant.
Results
Global level
The global burden of OUD has shown a consistent increase from 1990 to 2021. In 2021, the global burden of OUD reached approximately 16,164,876 cases (95% UI: 14,133,120–18,431,510). The prevalence increased from 154.59 per 100,000 (95% UI: 131.06–181.26) in 1990 to 198.49 per 100,000 (95% UI: 173.42–227.22) in 2021, at an AAPC of 0.80% (95% CI: 0.71%–0.90%). The global incidence reached 1,942,525 cases (95% UI: 1,643,342–2,328,363), and the global mortality reached 99,555 deaths (95% UI: 92,948–108,050), with DALYs amounting to 11,218,519 (95% UI: 9,188,658–13,159,551) (Table 1, Fig. 1). These trends showed a significant increase, especially from 2015 to 2018 (all p < 0.05). However, starting in 2019, the prevalence growth began to slow down, while incidence showed a downward trend (all p < 0.05), but mortality accelerated after 2017 (all p < 0.05). The temporal trend of DALYs closely resembles that of prevalence (all p < 0.05) (Supplementary Fig. S1–S4).
Table 1. Global and regional trends in the burden of opioid use disorder across five SDI levels: prevalence, incidence, mortality and disability-adjusted life years (1990–2021)
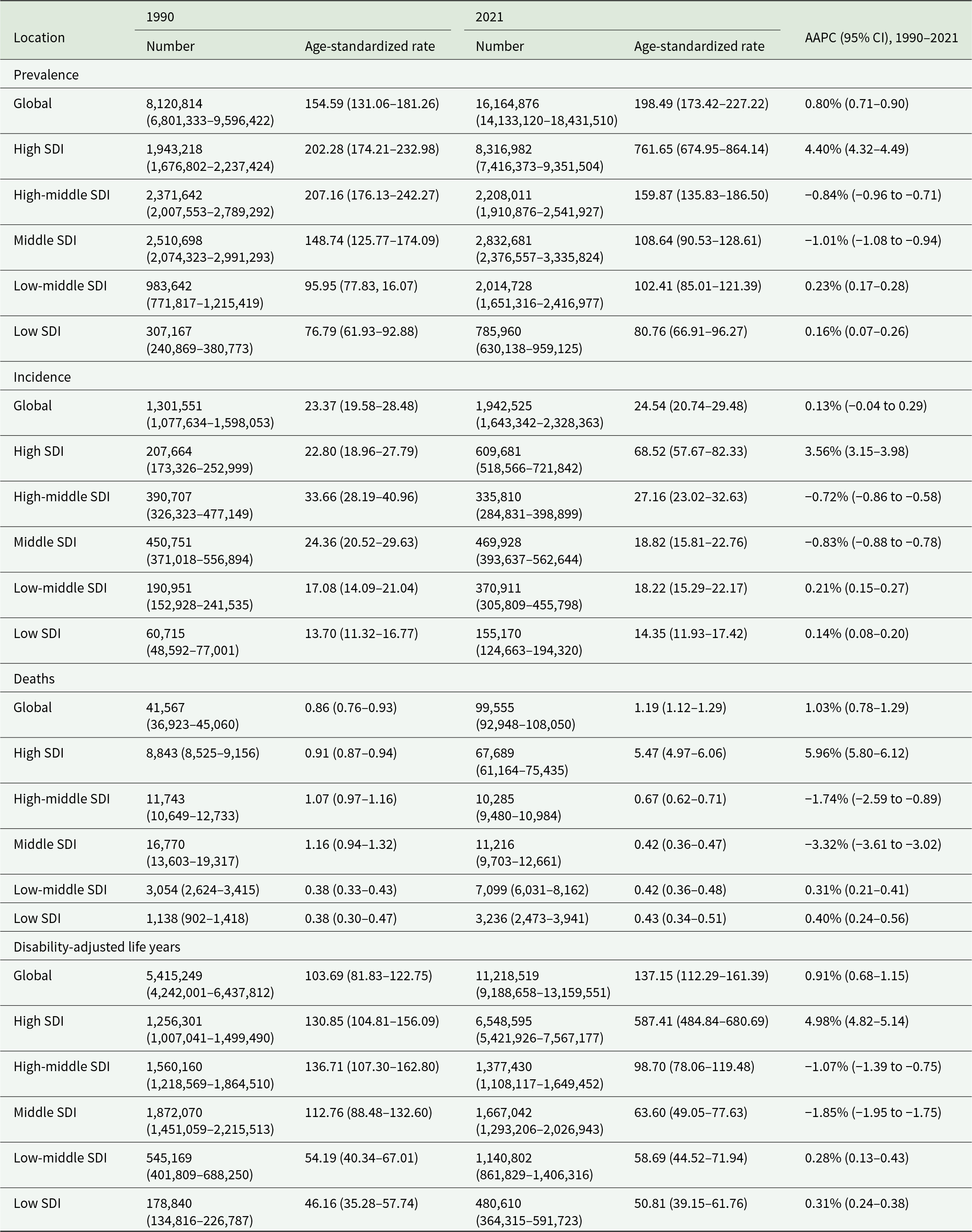
AAPC, average annual percentage change; SDI, socio-demographic index.
Values in parentheses are 95% uncertainty intervals.
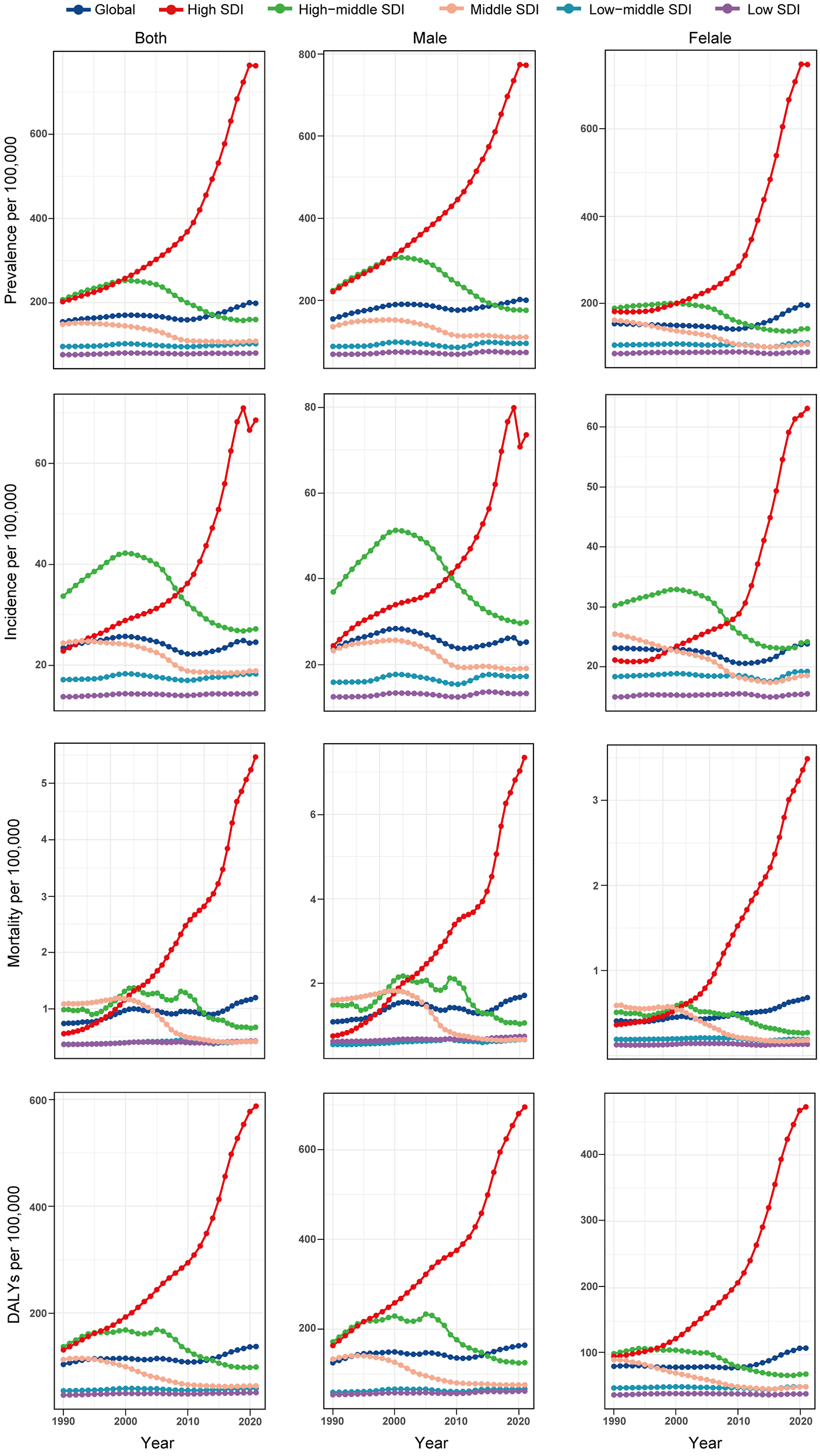
Figure 1. Burden of opioid use disorder for age-standardized prevalence, incidence, mortality and disability-adjusted life years from 1990 to 2021.
Regional level
The burden of OUD varies significantly across different SDI levels, with the main burden progressively transitioning from high-middle and middle SDI regions to high SDI regions for prevalence, incidence, mortality and DALYs from 1990 to 2021 (Fig. 2, Supplementary Figs S5–S6). From 1990 to 2019, these four indicators exhibited rapid growth (all p < 0.05). However, from 2019 to 2021, the growth in prevalence, mortality and DALYs began to slow, with incidence notably showing a decline (all p < 0.05) (Supplementary Figs S1–S4). In 2021, high SDI regions faced the highest prevalence of 761.65 per 100,000 (95% UI: 674.95–864.14) and an AAPC of 4.40% (95% CI: 4.32%–4.49%) (Table 1, Fig. 1). In addition, incidence, mortality and DALYs showed the highest values in high SDI regions (Table 1, Fig. 1). Given the chronic nature of OUD, we analysed the correlation between the indicators of prevalence and DALYs with SDI from 1990 to 2021. Globally, there is a moderate positive correlation between prevalence and SDI (Spearman’s rho = 0.553, p < 0.001), with a similar pattern for DALYs (rho = 0.543, p < 0.001) from 1990 to 2021 in GBD regions (Supplementary Fig. S7). These situations indicate that regions with high SDI generally face a greater burden of OUD.
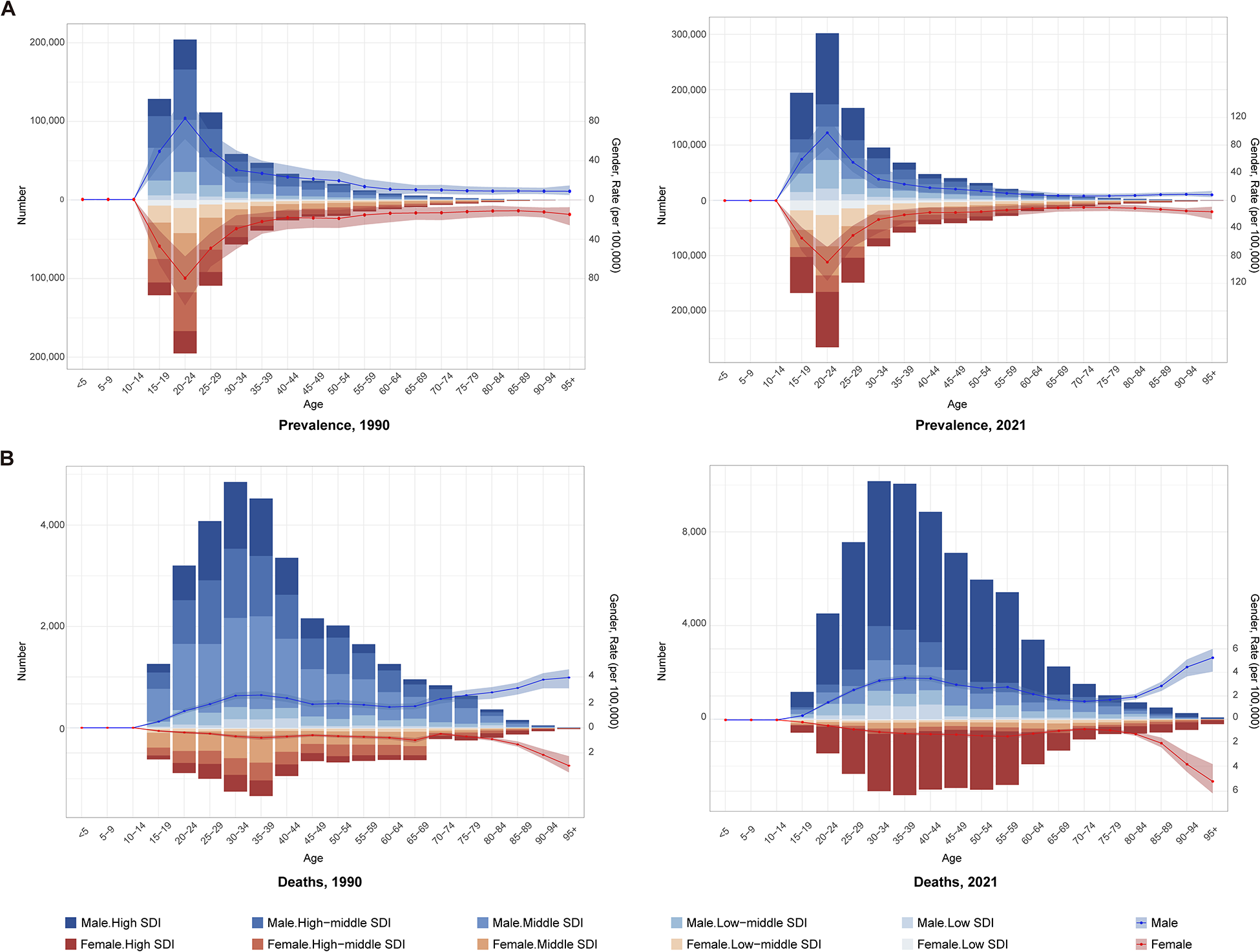
Figure 2. Prevalent cases and crude prevalence (a), deaths cases and crude mortality (b) of opioid use disorder by sex and SDI regions in 1990 and 2021. SDI, socio-demographic index.
For GBD regions, the High-income North America region exhibits the highest global burden of OUD, with a prevalence of 1890.26 per 100,000 (95% UI: 1659.84–2156.24), incidence (144.24 per 100,000, 95% UI: 120.13–174.95), mortality (14.5 per 100,000, 95% UI: 12.92–16.30), DALYs (1502.44 per 100,000, 95% UI: 1235.96–1740.10) in 2021. Moreover, all four of the above indicators exhibit the highest AAPC (all > 5%), which reflects rapid increases largely attributed to the opioid crisis, overprescription and misuse. For Latin American regions, although having generally low prevalence and incidence, its mortality displays a rapid rise, especially in Tropical Latin America (AAPC: 4.25%, 95% CI: 3.75%–4.76%) and Southern Latin America (AAPC: 3.59%, 95% CI: 1.91%–5.31%), suggesting an escalating future burden. The burden of OUD for 21 GBD regions is shown in the Supplementary Table S1.
National level
At the national level, the United States, which belongs to both the high SDI region and the High-income North America Region, bears the highest prevalence (2014.62 per 100,000; 95% UI: 1761.65–2308.32), incidence (151.84 per 100,000; 95% UI: 125.79–184.96), mortality (15.37 per 100,000; 95% UI: 13.62–17.33) and DALYs (1594.63 per 100,000; 95% UI: 1308.06–1849.82) (Supplementary Tables S2–S5, Fig. 3, Supplementary Fig. S8). Additionally, the United States has the most rapid AAPC (all > 5%) increase across all four metrics (Supplementary Fig. S9). Second, as the other representative of High-income North America, Canada ranks the third position in prevalence (771.61 per 100,000; 95% UI: 717.18–826.73) and second in both mortality (6.92 per 100,000; 95% UI: 6.32–7.51) and DALYs (681.03 per 100,000; 95% UI: 590.51–775.86) (Supplementary Tables S2–S5, Fig. 3, Supplementary Fig. S8). Canada also shows significant growth in mortality (AAPC: 6.38%, 95% CI: 5.57%–7.18%) and DALYs (AAPC: 3.57%, 95% CI: 3.13%–4.01%), following the United States (Supplementary Fig. S9). In contrast, Switzerland and China exhibit declining trends. Switzerland, as a high SDI country, has the largest decrease in prevalence (AAPC: −2.72%, 95% CI: −2.83% to −2.61%) and incidence (AAPC: −3.35%, 95% CI: −3.80% to −2.89%). China shows the most notable declines in mortality (AAPC: −5.32%, 95% CI: −5.67% to −4.96%) and DALYs (AAPC: −3.41%, 95% CI: −3.65% to −3.16%) (Supplementary Tables S2–S5). Detailed national burden and AAPC are available in Supplementary Tables S2–S5.
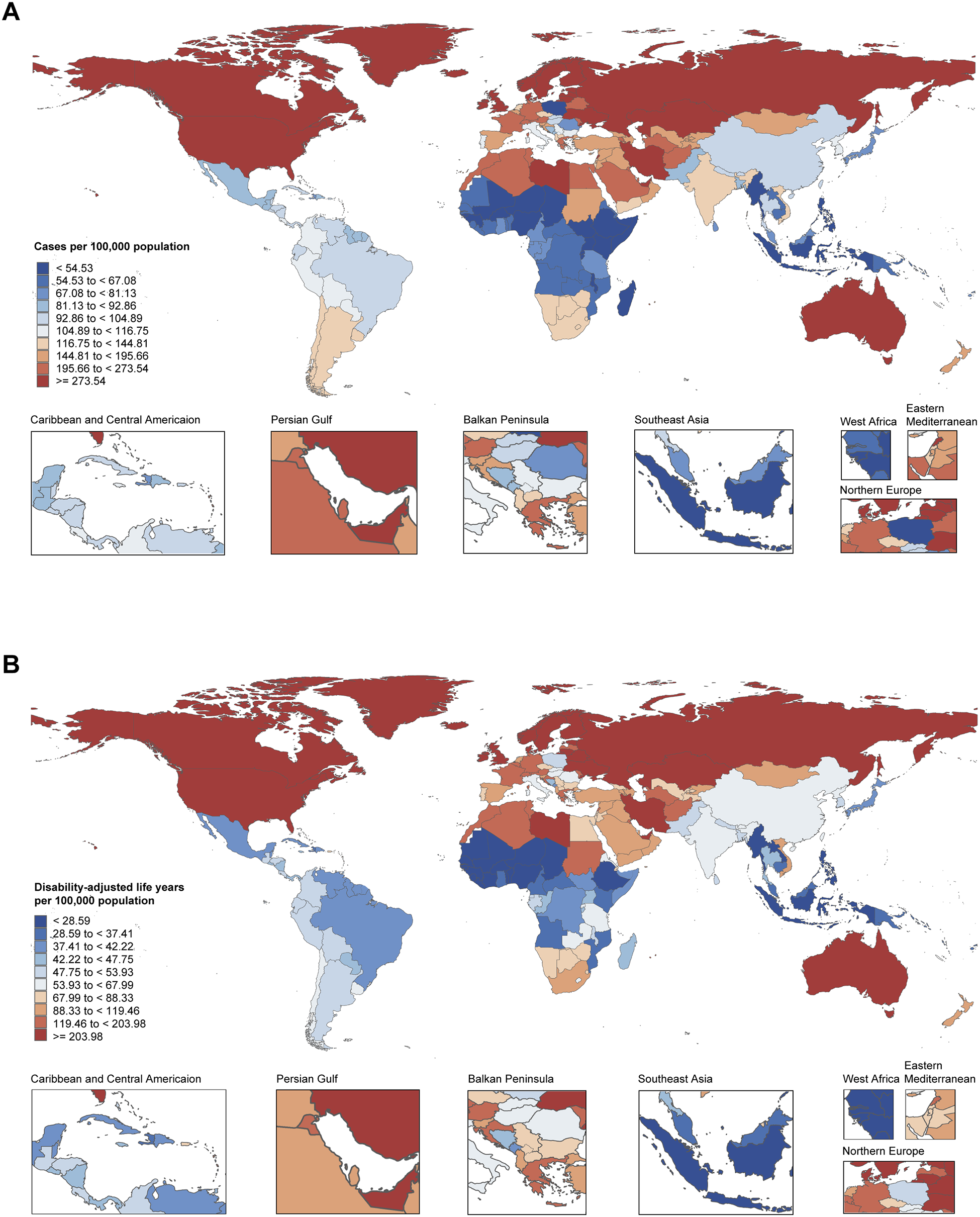
Figure 3. Global maps of opioid use disorder prevalence (a) and disability-adjusted life years (b) rates across all ages in 2021.
Age and sex patterns
Overall, the prevalence, incidence, mortality and DALYs show differences across age and sex, with a peak observed between the ages of 20 and 39 years in 2021. The burden of OUD appears to be higher in males than females for the four indicators. The age-period-cohort model also suggested that age effects were the main influencing factor on the burden of OUDs. Figure 4 and Supplementary Fig. S10 illustrate the age-period-cohort effects of OUD prevalence and DALYs, with both indicators showing similar trends. The prevalence and DALYs peak in the 25–29 age group, followed by a gradual decline. After controlling for period and cohort effects, the age effects of prevalence in the 25–29 age group is 7.17 times that of the 15–19 age group (exp((αage(25–29) − αmean) − (αage(15–19) −αmean)) = exp(αage(25–29) −αage(15–19)) = 1.700/0.237), while DALYs are 5.83 times. Although the burden tends to decrease with age, a considerable health burden remains in the middle-aged and elderly populations. Both indicators show an increase in the population over 80 years of age. The period effect has a non-significant impact on both prevalence (relative risk [RR]: 0.93–1.10) and DALYs (RR: 0.95–1.15) from 1990 to 2021. The cohort effect for both prevalence (RR: 1.03–1.31) and DALYs (RR: 1.07–1.46) shows an early increase in cohorts born in earlier years, a mid-term decline, followed by a late-term rise from 1990 to 2021.
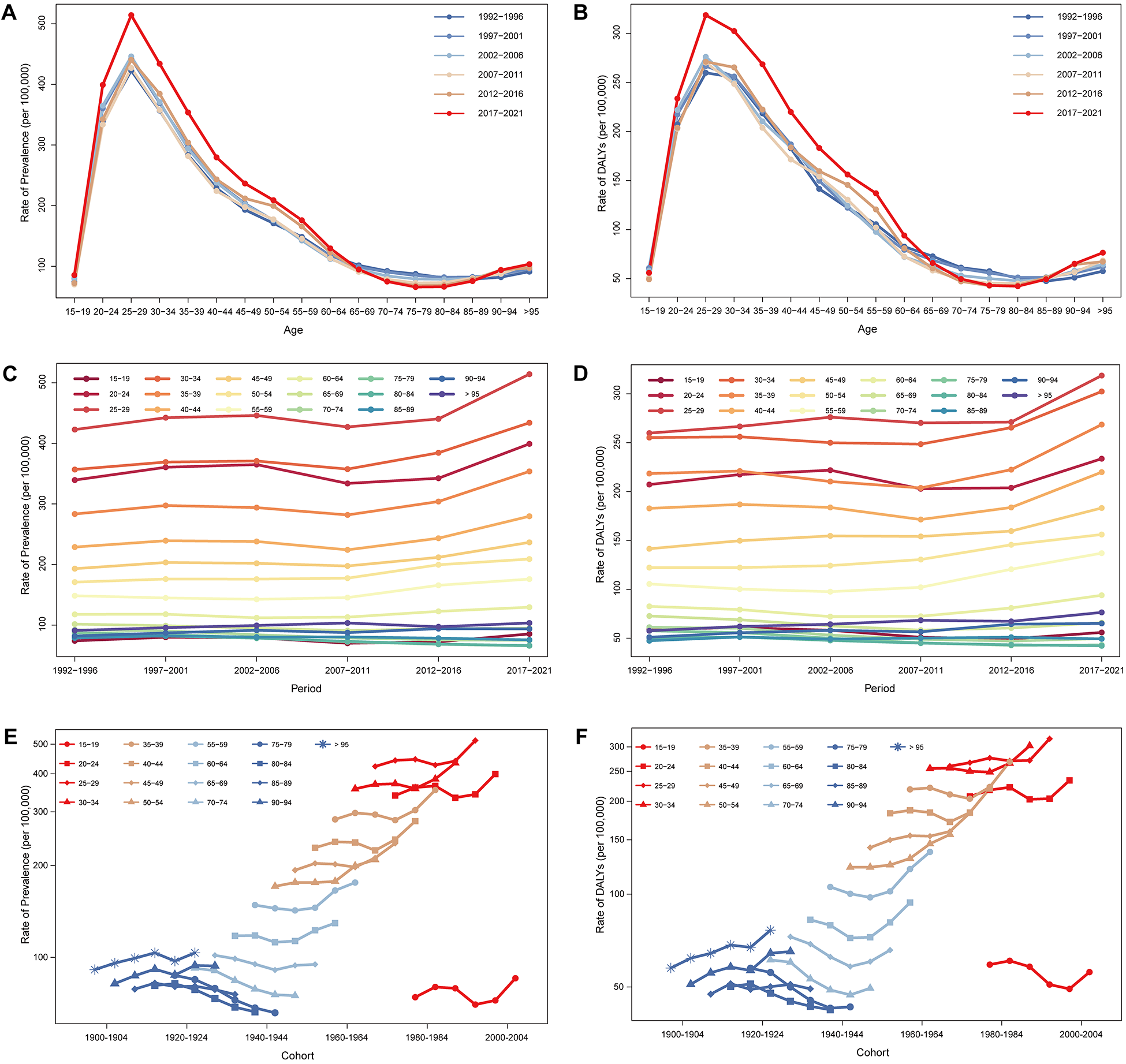
Figure 4. Global trends of age-specific, period-based and cohort-based effects on opioid use disorder prevalence (a, c, e) and DALYs (b, d, f). DALYs, disability-adjusted life years.
Future forecasts
From 2021 to 2040, the Bayesian age-period-cohort model predicts a significant global increase in the burden of OUD, with a particularly notable rise among females (Fig. 5). The prevalence for both genders is projected to increase from 278.33 per 100,000 in 2021 to 347.43 per 100,000 in 2040, an approximate rise of 25%. The prevalence for females is more pronounced, from 274.98 per 100,000 to 382.13 per 100,000, a growth of about 39%. A similar trend is observed in the incidence, with the combined incidence for both genders rising by about 30% (44.96 per 100,000) and increasing by approximately 49% (49.76 per 100,000) for females in 2040. The mortality is expected to grow by 30% (2.17 per 100,000) globally in 2040. The DALYs will increase from 192.24 per 100,000 to 222.28 per 100,000. These data highlight the significant impact of gender differences on the burden of OUD.
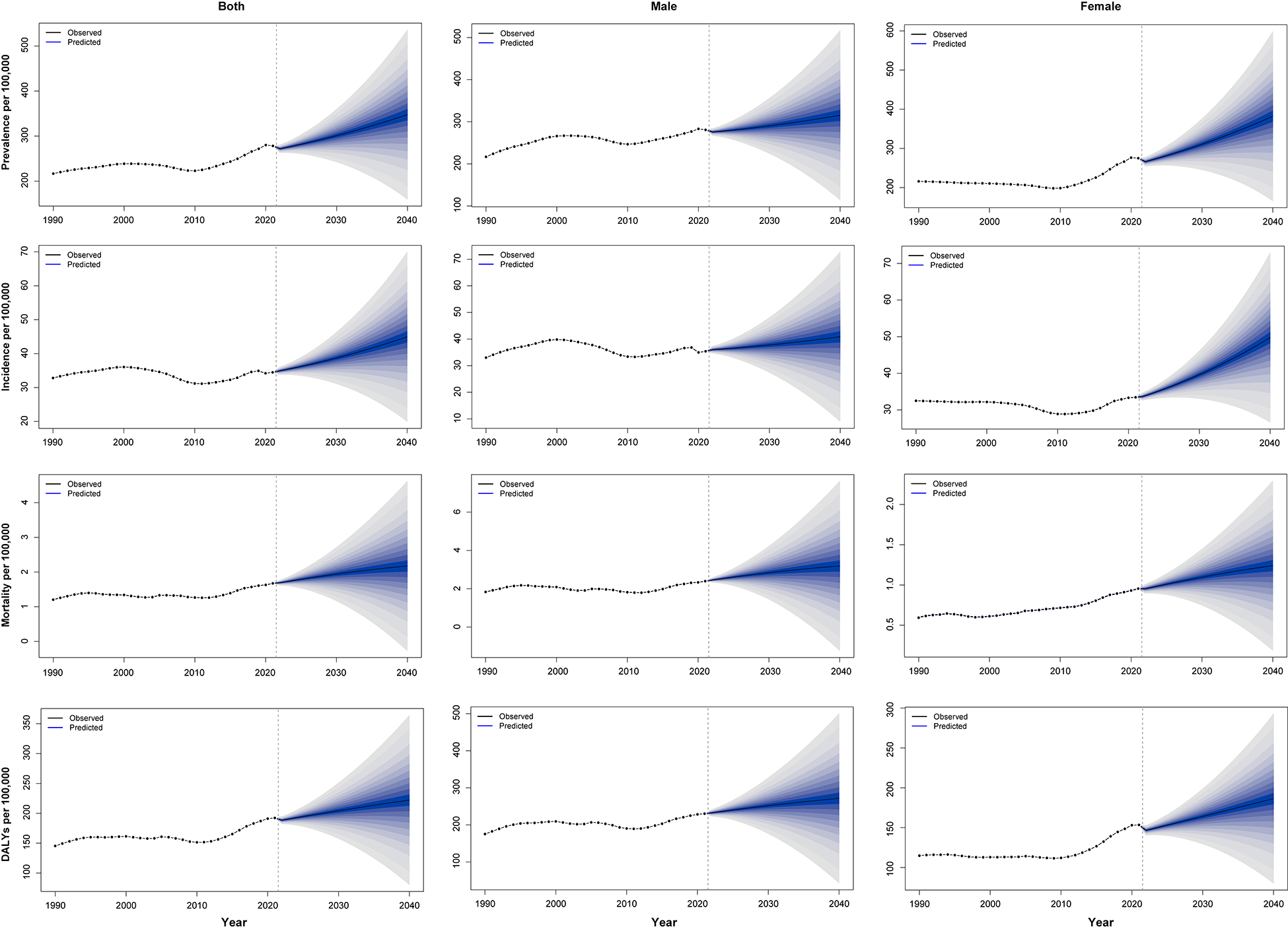
Figure 5. Future forecasts of global opioid use disorder burden for age-standardized prevalence, incidence, mortality and disability-adjusted life years.
Discussion
This study systematically analysed the global burden of OUD and confirmed a consistent increase from 1990 to 2021. The burden shows significant variation across regions and countries. The United States bears the heaviest burden and largest increase, followed by Canada, which consistently belongs to the high SDI group and the High-income North America region. In contrast, changes in global and most regional areas outside High-income North America are relatively small (with most AAPCs below 1%), suggesting slower progression of the opioid crisis. However, in Latin America, although mortality remains low compared to High-income North America, the growth rate is notable, particularly in the Tropical and South Latin regions, which are geographically close. Therefore, we may assume the root causes of these differences involve a combination of socio-economic factors, drug policies, healthcare resources and drug management strategies, which may influence one another between neighbouring countries.
A striking feature in high-SDI countries is the stronger correlation between OUD and SDI within countries. A higher SDI typically reflects better socio-economic support and more comprehensive healthcare, which, while improving medical resources and treatment access, may also increase the risk of opioid misuse. In high-income and high-SDI regions, opioid use is more prevalent due to easier access, particularly in areas with less stringent regulation, such as the United States (Friedman et al., Reference Friedman, Nguemeni Tiako and Hansen2024). Therefore, improvements in medical resources and access should be accompanied by compatible regulatory and supervisory policies from the outset. If no scrutinizing system is in place, medical access to opioids should be more conservative, as various non-opioid analgesics are available. Moreover, the uneven distribution of healthcare resources within high-SDI countries may further exacerbate this burden (Bounthavong and Yip, Reference Bounthavong and Yip2024). Regions with more healthcare services show a more pronounced OUD problem, highlighting the role of medical access in driving the opioid crisis. Overall, multiple factors contribute to OUD, but medical source access should receive the most attention for future management.
Although the OUD crisis in High-income North America primarily stems from the over-prescription of opioids since the 1990s, along with subsequent misuse and addiction problems, illicitly manufactured opioids have worsened this problem (Dhalla et al., Reference Dhalla, Persaud and Juurlink2011; The Lancet, 2022). Therefore, even though delayed public health policies have been credited with addressing this crisis (Dasgupta et al., Reference Dasgupta, Beletsky and Ciccarone2018), such as Prescription Drug Monitoring Programs, the prevalence, mortality and DALYs in these regions are still rising (Dowell et al., Reference Dowell, Brown, Gyawali, Hoenig, Ko, Mikosz, Ussery, Baldwin, Jones, Olsen, Tomoyasu, Han, Compton and Volkow2024). Based on the data from the Centers for Disease Control and Prevention in the United States, approximately 72,000 overdose deaths were reported involving illicitly manufactured fentanyls, accounting for 70% of all drug-related overdose deaths in 2023 (Tanz et al., Reference Tanz, Stewart, Gladden, Ko, Owens and O’Donnell2024). Furthermore, carfentanil-related overdose deaths increased sevenfold in the first half of 2024. This evidence strongly emphasizes the potential shift of OUD from medical prescriptions to the illicit market, which might contribute to the rapid rise in Latin American regions and should also be addressed as quickly as possible. Therefore, future public health strategies should not only actively supervise medical access to opioids, but also swiftly and strictly eliminate the illicit drug market.
The Latin American region also requires attention. Although the current burden of OUD is less prevalent than amphetamines, cannabis and cocaine use disorders, OUD accounts for the largest burden in this region, particularly in years lived with disability (Castaldelli-Maia et al., Reference Castaldelli-Maia, Wang, Brunoni, Faro, Guimarães, Lucchetti, Martorell, Moreira, Pacheco-Barrios, Rodriguez, Roever, Silva, Tovani-Palone, Valdez, Zimmermann, Culbreth, Hay, Murray and Bensenor2023). Some Latin American countries, especially in tropical and southern regions, show rapid increases in mortality and DALYs. The expansion of drug access channels, such as overprescription and the illicit drug market, and insufficient healthcare resources for overdose rescue mean these countries may face greater future challenges. For example, Brazil showed a significant increase in prescribed opioid sales, especially oxycodone, from 2009 to 2015, reflecting generous opioid prescribing (Krawczyk et al., Reference Krawczyk, Greene, Zorzanelli and Bastos2018). Heroin use among Peru’s younger population has gradually increased, while Uruguay was identified as having an emerging opioid misuse problem in 2020 (Castaldelli-Maia et al., Reference Castaldelli-Maia, Wang, Brunoni, Faro, Guimarães, Lucchetti, Martorell, Moreira, Pacheco-Barrios, Rodriguez, Roever, Silva, Tovani-Palone, Valdez, Zimmermann, Culbreth, Hay, Murray and Bensenor2023). Although opioid misuse became a public health concern in Uruguay in 2020, there is still limited information on the effectiveness of public interventions targeting opioid-related harm. Delayed and insufficient actions could result in a problematic situation, as seen in the United States.
Overall, there are clear regional variations and disparities in the global burden of OUD. However, we can observe that high SDI and income may lead to an early ‘onset’ of OUD. The global shift in causes and the expansion of opioid access worldwide would involve more countries in the opioid crisis. Learning from the opioid history of countries with a high OUD burden, early intervention and strict control can be highly beneficial. Effective global strategies must also be tailored to the specific circumstances of each region.
The burden of OUD varies across age and gender. Unlike chronic diseases that typically affect the elderly, OUD is most prevalent among young adults aged 20–39 years, particularly males, consistent with previous studies (GBD 2016 Alcohol and Drug Use Collaborators 2018; Pan et al., Reference Pan, Zhang, Cheng, Bu, Li, Deng, Zhou, Dai and Lyu2020). This age group should be the focus of future intervention. Additionally, the burden among older populations (aged above 65 years) has increased in recent years, especially among those aged 80 years and above. In contrast to younger individuals, long-term opioid prescriptions for chronic pain appear to be the main cause among the elderly (Degenhardt and Hall, Reference Degenhardt and Hall2012). Furthermore, the burden of disease affects both incidence and health outcomes more directly than in other conditions, where DALYs typically lag behind prevalence (Degenhardt et al., Reference Degenhardt, Whiteford, Ferrari, Baxter, Charlson, Hall, Freedman, Burstein, Johns, Engell, Flaxman, Murray and Vos2013); The US Burden of Disease Collaborators. These findings suggest that these groups are in an early stage of drug-related health issues, highlighting the need for earlier intervention. Although the overall burden is higher in males, studies indicate that females may face a greater risk of drug dependence due to psychological and social pressures (Castaldelli-Maia et al., Reference Castaldelli-Maia, Wang, Brunoni, Faro, Guimarães, Lucchetti, Martorell, Moreira, Pacheco-Barrios, Rodriguez, Roever, Silva, Tovani-Palone, Valdez, Zimmermann, Culbreth, Hay, Murray and Bensenor2023; Pan et al., Reference Pan, Zhang, Cheng, Bu, Li, Deng, Zhou, Dai and Lyu2020). The Bayesian age-period-cohort model further predicts that the burden for females will increase significantly over the next 20 years. Overall, young males and the elderly are current key groups of concern, while females may face a severe burden in the future. To address this, key strategies include enhancing opioid education for women, improving treatment access, considering psychological and physiological factors and strengthening social support and policy protections.
The COVID-19 pandemic had a complex impact on the global burden of OUD. A marked shift in the prevalence and incidence of OUD has been closely related to the effects of the COVID-19 pandemic. First, the COVID-19 pandemic led to disruptions in healthcare services worldwide, with the diagnosis and treatment of non-acute conditions being delayed, and OUD patients were no exception. OUD patients who should have been diagnosed did not receive timely evaluation. Thus, the decline in ASIR during the pandemic may not fully reflect the actual incidence trend, likely due to underdiagnosis and patients avoiding medical care (Haley and Saitz, Reference Haley and Saitz2020). Second, the pandemic’s potential impacts, such as mental health issues and racial inequalities, led more people to rely on opioids, particularly illicit drugs, especially in high SDI countries. In 2020, the proportion of Black patients seeking treatment for opioid-related overdoses increased significantly in Virginia (Ochalek et al., Reference Ochalek, Cumpston, Wills, Gal and Moeller2020). Additionally, the supply of illicit fentanyl in the United States increased, contributing to a resurgence of opioid misuse (Wainwright et al., Reference Wainwright, Mikre, Whitley, Dawson, Huskey, Lukowiak and Giroir2020). The use of these illicit synthetic opioids reflects the worsening trend of misuse in the post-pandemic period. These factors may explain the rebound in ASIR seen in Fig. 1 in late 2020. Overall, COVID-19 caused complex changes in the OUD burden in 2020, and there is a need to remain vigilant regarding further rebound in the OUD burden in the post-pandemic period.
Regarding the limitations and future research directions, this study has three limitations. First, the quality and completeness of the GBD database vary across countries and regions, particularly in low-income areas where underreporting, underdiagnosis, and data gaps may lead to an underestimation of the burden of OUD (Degenhardt et al., Reference Degenhardt, Whiteford, Ferrari, Baxter, Charlson, Hall, Freedman, Burstein, Johns, Engell, Flaxman, Murray and Vos2013). To address this, efforts should enhance data collection and reporting mechanisms in low-income regions, such as improving local healthcare information systems and promoting international collaborations. Second, the GBD models for estimating disease burden rely on assumptions and statistical estimations, which may introduce uncertainties. Future research could benefit from multicentre prospective studies to validate predictive models and supplement GBD estimates. Finally, although the GBD database provides the best available estimates, these limitations highlight the need for caution in interpreting results and underscore the importance of efforts to update and refine global burden estimates (GBD 2021 Diseases and Injuries Collaborators 2024). Future studies should explore the relationship between disease burden and socio-economic factors, drug policies and healthcare resources.
Conclusions
The global burden of OUD has shown a consistent increase from 1990 to 2021. There are marked disparities across regions, countries and SDI levels. The changes in the global burden and in most regions, other than the High-income North America region, are relatively small. High-income North America, particularly the United States, bears the heaviest burden and the largest increase, even though multiple but delayed policies have been implemented. Regions from non-high SDI regions, such as Latin America, are experiencing a rapidly rising burden, albeit from a low baseline. Meanwhile, opioid sources have expanded from overprescription to illicit market. Young males (aged 20–39 years) are the most affected group, while the elderly suffer increasingly. Moreover, the burden among females is expected to rise sharply over the next 20 years. Therefore region-, source- and population-targeted interventions are urgently needed to mitigate the growing challenges posed by OUD worldwide.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796025100085.
Availability of data and materials
GBD study 2021 data resources were available online from the GHDx query tool (http://ghdx.healthdata.org/gbd-results-tool).
Acknowledgements
We sincerely thank the contributors of the Global Burden of Diseases, Injuries, and Risk Factors Study 2021 and the Institute for Health Metrics and Evaluation for providing the GBD data for this research.
Financial support
This work was supported by the National High Level Hospital Clinical Research Funding (No. 2022-PUMCH-B-006), the National Natural Science Foundation of China (No. 82071252), the Peking Union Medical College Hospital Talent Cultivation Program (Category D, No. UHB12233) and the Japan–China Sasakawa Medical Fellowship.
Competing interests
The authors declare no conflict of interest.








