Introduction
First-time mothers constitute a priority population for public mental health strategies (Leahy-Warren et al., Reference Leahy-Warren, McCarthy and Corcoran2012; Ong et al., Reference Ong, Ong, Ang, Vehviläinen-Julkunen and He2023; Wilkins, Reference Wilkins2006). Maternal depression in the first year postpartum can have serious consequences, including maternal morbidity and mortality as well as adverse infant outcomes (Arditi-Arbel et al., Reference Arditi-Arbel, Hamdan, Winterman and Gvion2023; Howard et al., Reference Howard, Molyneaux, Dennis, Rochat, Stein and Milgrom2014; Moreira et al., Reference Moreira, Moreira, Custódio, Dias, Rosa, Ferreira-Neto, Colombari, Costa, Fajemiroye and Pedrino2023; Rogers et al., Reference Rogers, Obst, Teague, Rossen, Spry, Macdonald, Sunderland, Olsson, Youssef and Hutchinson2020). Maternal postpartum depression (PDD) is defined as a major depressive disorder episode within one year of childbirth. It is marked by symptoms such as depressed mood, loss of interest, sleep disturbances, guilt, worthlessness, and suicidal ideation lasting over two weeks (Stewart and Vigod, Reference Stewart and Vigod2019). The risk factors for PDD may include perinatal depression and poor support from family, friends, or a partner. The prevalence of this condition is reported to be 17.8% within the first year after childbirth (Hahn-Holbrook et al., Reference Hahn-Holbrook, Cornwell-Hinrichs and Anaya2018). First-time mothers are more likely to report depressive symptoms than those who have already had children (Bradshaw et al., Reference Bradshaw, Riddle, Salimgaraev, Zhaunova and Payne2022), as their lack of experience with childbirth and childcare increases the psychosocial burden of their transition to motherhood (Ong et al., Reference Ong, Ong, Ang, Vehviläinen-Julkunen and He2023; Shorey et al., Reference Shorey, Chan, Chong and He2015; van Roode et al., Reference van Roode, Sharples, Dickson and Paul2017). A younger age at pregnancy may further increase transition challenges and the risk of postnatal depressive symptoms. Previous research on adversity during early pregnancy has primarily focused on teenage mothers; however, young adults aged 18–25 years also face unique challenges. These individuals are still in a stage of physical and psychological development, are not yet fully mature, and are subject to various psychosocial health disparities (Society for Adolescent Health and Medicine, 2017). Challenges specific to this age group include higher unemployment rates, economic instability, precarious housing conditions, and higher rates of unplanned pregnancies; this necessitates increased awareness of their vulnerability to postpartum depression compared to older first-time mothers (Harron et al., Reference Harron, Gilbert, Fagg, Guttmann and van der Meulen2021; Ong et al., Reference Ong, Ong, Ang, Vehviläinen-Julkunen and He2023; van Roode et al., Reference van Roode, Sharples, Dickson and Paul2017; Zasloff et al., Reference Zasloff, Schytt and Waldenström2007).
We defined ‘interpersonal support’ as individuals who can be genuinely relied upon when assistance is needed. Having a reliable person to turn to in times of need positively affects mental health in general adolescent and adult populations (Brugha et al., Reference Brugha, Weich, Singleton, Lewis, Bebbington, Jenkins and Meltzer2005; Nishida et al., Reference Nishida, Foo, Yamaguchi, Togo, Shimodera, Nishida, Okazaki and Sasaki2024). Social support during pregnancy, especially emotional support from close individuals such as partners and family members, is crucial to reducing the risk of postpartum depressive symptoms (Cankorur et al., Reference Cankorur, Abas, Berksun and Stewart2015; Cho et al., Reference Cho, Lee, Choi, Cho, Park, Suh, Rhee and Choi2022; Faleschini et al., Reference Faleschini, Millar, Rifas-Shiman, Skouteris, Hivert and Oken2019; Milgrom et al., Reference Milgrom, Hirshler, Reece, Holt and Gemmill2019; Morikawa et al., Reference Morikawa, Okada, Ando, Aleksic, Kunimoto, Nakamura, Kubota, Uno, Tamaji, Hayakawa, Furumura, Shiino, Morita, Ishikawa, Ohoka, Usui, Banno, Murase, Goto, Kanai, Masuda and Ozaki2015; Razurel et al., Reference Razurel, Kaiser, Antonietti, Epiney and Sellenet2017; Taylor et al., Reference Taylor, Nath, Sokolova, Lewis, Howard, Johnson and Sweeney2022; Wickramaratne et al., Reference Wickramaratne, Yangchen, Lepow, Patra, Glicksburg, Talati, Adekkanattu, Ryu, Biernacka, Charney, Mann, Pathak, Olfson and Weissman2022). However, pregnant women sometimes experience reduced accessibility to friends and family as support (De Sousa Machado et al., Reference De Sousa Machado, Chur-Hansen and Due2020). The number of close friends and neighbours an individual had during pregnancy had a greater impact on postpartum mental health than the quality of support (Martín-Vázquez et al., Reference Martín-Vázquez, Urchaga-Litago, García-Fernández, Calvo-Ayuso, Quiroga-Sánchez and Liébana-Presa2024; Matsumura et al., Reference Matsumura, Morozumi, Hamazaki, Tsuchida and Inadera2023) or satisfaction with the relationship (Morikawa et al., Reference Morikawa, Okada, Ando, Aleksic, Kunimoto, Nakamura, Kubota, Uno, Tamaji, Hayakawa, Furumura, Shiino, Morita, Ishikawa, Ohoka, Usui, Banno, Murase, Goto, Kanai, Masuda and Ozaki2015). Therefore, understanding the number of such supportive relationships is vital for designing effective support interventions. As young first-time mothers are particularly more likely to be isolated and depressed, they require robust interpersonal support beginning in early pregnancy (Henderson and Redshaw, Reference Henderson and Redshaw2016). Therefore, they should be considered a priority group for public mental health strategies to provide access to interpersonal support (Estrin et al., Reference Estrin, Ryan, Trevillion, Demilew, Bick, Pickles and Howard2019; Kim et al., Reference Kim, Connolly and Tamim2014). Identifying groups with a high need for interpersonal support and who are likely to experience positive changes through such support is important for the optimal use of limited resources (Nakamura et al., Reference Nakamura, Sutter-Dallay, El-Khoury Lesueur, Thierry, Gressier, Melchior and van der Waerden2020). Additionally, identifying the approaches to increase interpersonal support must establish a clear minimum threshold to ensure effective implementation, as practitioners and first-time mothers may struggle to take practical action without this clarity (Palmer, Reference Palmer2011). However, to our knowledge, no existing research has clarified the minimum number of interpersonal supporters associated with lower postpartum depressive symptoms.
This study aimed to examine the minimal number of interpersonal supporters during pregnancy associated with lower levels of postpartum depressive symptoms among first-time mothers.
Methods
Study setting
This population-based Mother–Infant/Newborn Tokyo Cohort (MINT cohort) study was commissioned by the Tokyo Metropolitan Government and conducted in four municipalities in Tokyo, Japan.
Populations
The study recruited first-time mothers aged ≥ 16 years who submitted a notification of pregnancy to their municipal office in July 2022. Because the proportion of first-time mothers aged 16–25 years in the population was small, they were over-sampled to increase the number of subjects (November 2021–July 2022). Eligible individuals received a face-to-face explanation from a public health nurse regarding the web-based survey, which would be conducted for up to one year after delivery. Pregnant women who agreed to participate completed the consent procedure online and then proceeded to the first online survey. Inclusion criteria for the study were as follows: at least 16 years of age, first-time mothers, registered residents in the target municipality with no immediate plans to move out, pregnancy at earlier than 30 weeks gestation, and the ability to understand the Japanese language. During the period, 461 pregnant women who had registered their pregnancies in the target municipalities were eligible for this study. All 461 women were approached through face-to-face interactions, and 11 declined to participate, resulting in 441 participants (95.7%). Of the 441 participants, 12 did not report their age in the surveys. After excluding these 12 participants, 429 pregnant women (97.3% of those who consented) were included in the analysis.
Data collection procedure
This study of first-time mothers comprised five waves of web-based surveys conducted at different stages: the first at the time of pregnancy notification (Wave 1, W1), the second at 20 weeks gestation (W2), the third at 1-month postpartum (W3), the fourth at 6 months postpartum (W4), and the fifth at 12 months postpartum (W5). During pregnancy (W1 and W2), data were collected on maternal demographics, mental health (using the World Health Organization-Five Well-Being Index [WHO-5] Well-Being Index), self-esteem, and social support (measured with the SSQ6). In the postpartum period (W3, W4, and W5), the surveys were expanded to include additional topics such as childbirth-related information, child health, mother–child attachment, and postpartum depression assessed using the Edinburgh Postnatal Depression Scale (EPDS), alongside items measured during pregnancy. The present analysis used data from the first (W1) and the third (W3) surveys, as postpartum depression most commonly occurs within the first 3 months after childbirth (Hutchens and Kearney, Reference Hutchens and Kearney2020; Iwata et al., Reference Iwata, Mori, Sakajo, Aoki, Maehara and Tamakoshi2016). Additionally, we stratified the sample into two age groups—25 years and young adults aged 18–25 years. Previous research on adversity during early pregnancy has primarily focused on teenage mothers; however, young adults aged 18–25 years also face unique challenges (Aitken et al., Reference Aitken, Hewitt, Keogh, LaMontagne, Bentley and Kavanagh2016). These individuals are still in a stage of physical and psychological development in extended adolescence (Sawyer et al., Reference Sawyer, Azzopardi, Wickremarathne and Patton2018), are not yet fully mature, and are subject to various psychosocial health disparities (Society for Adolescent Health and Medicine, 2017).
Measurements
Maternal postpartum depressive symptoms
Postpartum depressive symptoms were assessed using the Japanese version of the EPDS (Okano et al., Reference Okano, Murata, Masuji, Tamaki, Nomura, Miyaoka and Kitamura1996). The EPDS was developed to assess postpartum depressive symptoms after childbirth (Cox et al., Reference Cox, Holden and Sagovsky1987). It is a 10-item scale that assesses a woman’s mood during the past week, with each item scored on a four-point Likert scale ranging from 0 to 3. A total score ranging from 0 to 30 was calculated, with higher scores indicating more severe depressive symptoms. The Japanese version of the EPDS has satisfactory psychometric properties, including good internal consistency, with a cutoff score of ≥ 9 indicating a diagnosis of depression (Cronbach’s alpha = 0.78; Okano et al., Reference Okano, Murata, Masuji, Tamaki, Nomura, Miyaoka and Kitamura1996). For our analysis, we used the EPDS as a continuous variable rather than a binary variable based on the cutoff point. While the EPDS can also be used during pregnancy (Park and Kim, Reference Park and Kim2023), the WHO-5 Well-Being Index, which consists of positively framed questions, was used instead at W1 to minimise the invasiveness of the initial survey.
Interpersonal support in pregnancy
The number of interpersonal supporters in early pregnancy (at approximately 20 weeks gestation) was measured using the first item of the Japanese version of the Social Support Questionnaire, ‘Whom can you really count on to be dependable when you need help?’ and had seven answer options: 1. ‘None’, 2. ‘One’, 3. ‘Two’, 4. ‘Three’, 5. ‘Four’, 6. ‘Five’, 7. ‘Six or more’ (Furukawa et al., Reference Furukawa, Harai, Hirai, Kitamura and Takahashi1999; Sarason, Levine, et al., Reference Sarason, Levine, Basham and Sarason1983; Sarason et al., Reference Sarason, Sarason, Shearin and Pierce1987). In this study, our objective was to estimate the number of interpersonal supporters associated with lower postpartum depressive symptoms in first time mothers rather than to use a composite measure of social support. Therefore, we selected a single item from the scale that was the most closely aligned with the questions used in previous studies suggesting the relationship between better mental health and greater number of supporters (Brugha et al., Reference Brugha, Weich, Singleton, Lewis, Bebbington, Jenkins and Meltzer2005; Nishida et al., Reference Nishida, Foo, Yamaguchi, Togo, Shimodera, Nishida, Okazaki and Sasaki2024). Given that the correlation between the first item and the summary score of the remaining five items in our survey was 0.67, we assumed that this first item preserved consistency with the scale. A prior study found that Japanese pregnant women had an average of 4.6 interpersonal supporters (Morikawa et al., Reference Morikawa, Okada, Ando, Aleksic, Kunimoto, Nakamura, Kubota, Uno, Tamaji, Hayakawa, Furumura, Shiino, Morita, Ishikawa, Ohoka, Usui, Banno, Murase, Goto, Kanai, Masuda and Ozaki2015).
Covariates
Depressive symptoms during pregnancy were assessed using the Japanese version of the WHO-5 (Awata et al., Reference Awata, Bech, Yoshida, Hirai, Suzuki, Yamashita, Ohara, Hinokio, Matsuoka and Oka2007; Topp et al., Reference Topp, Østergaard, Søndergaard and Bech2015). Symptoms during pregnancy have often been reported as a critical risk factor for postpartum depression (Cruise et al., Reference Cruise, Layte, Stevenson and O’Reilly2018; Howard et al., Reference Howard, Molyneaux, Dennis, Rochat, Stein and Milgrom2014) and were included as a covariate in the analysis.
Statistical analysis
We compared demographic characteristics, depressive symptoms, and the number of interpersonal supporters between younger mothers (≤ 25 years) and older mothers (≥ 26 years). We conducted chi-square tests for categorical variables (educational attainment, marital status, employment status, prenatal and postnatal number of interpersonal supporters, prevalences of cases exceeding cutoff for depression [EPDS scores ≥ 9]) and t-tests for continuous variables (age at the first survey and prenatal and postnatal depressive symptom scores). We conducted a segment regression analysis to test whether there was a threshold at which the strength of the association between the number of interpersonal supporters and postpartum depressive symptoms changed. First, we conducted the analysis with the total sample without covariates. Second, we performed the analysis stratified by the younger and older age groups. We then repeated the analyses, adjusting for prenatal depressive symptoms, with the total sample and stratified by the age groups. The significance level was set at α = 0.05. These analyses were conducted using R version 4.4.0 with the segmented package.
Results
Descriptive statistics
A total of 429 first-time mothers from four municipalities in Tokyo participated in this study. The mean age was 29.0 years (SD = 5.7). The proportion of pregnant women with an education degree of less than a high school education (29.7%) and living alone (7.6%) was higher among the younger than older pregnant women (Table 1). The mean antenatal WHO-5 score was 15.2 (SD = 4.9), with no significant difference between younger and older pregnant women (P = 0.416; Table 2). The mean postpartum EPDS score was 6.2 (SD = 4.7), with 26.4% of pregnant women showing possible PDD. These findings are largely consistent with previous research, which reported a prevalence of 22.5% (Nakamura et al., Reference Nakamura, Sutter-Dallay, El-Khoury Lesueur, Thierry, Gressier, Melchior and van der Waerden2020). There was no significant difference in postnatal depressive symptom rates between young and older pregnant women (P = 0.648; Table 2). The average number of interpersonal supporters was 3.9 (SD = 1.6) during pregnancy and 3.7 (SD = 1.6) postpartum (Table 2), indicating a significant difference between the prenatal and postnatal periods (paired t-test: P = 0.005).
Table 1. Demographic characteristics of participants (N = 429)

a P-values derived from the chi-square or t-test.
Table 2. Number of interpersonal supporters during the prenatal period, prenatal depressive symptoms, and postnatal depressive symptoms (N = 429)
a P-values derived from the chi-square or t-test.
b Interpersonal social support was measured using the first item of the Japanese version of the Social Support Questionnaire: ‘Whom can you really count on to be dependable when you need help?’
c Depression was measured using the five-item version of the World Health Organization Mental Well-Being Index.
d EPDS = Edinburgh Postnatal Depression Scale.
Segmented regression analysis
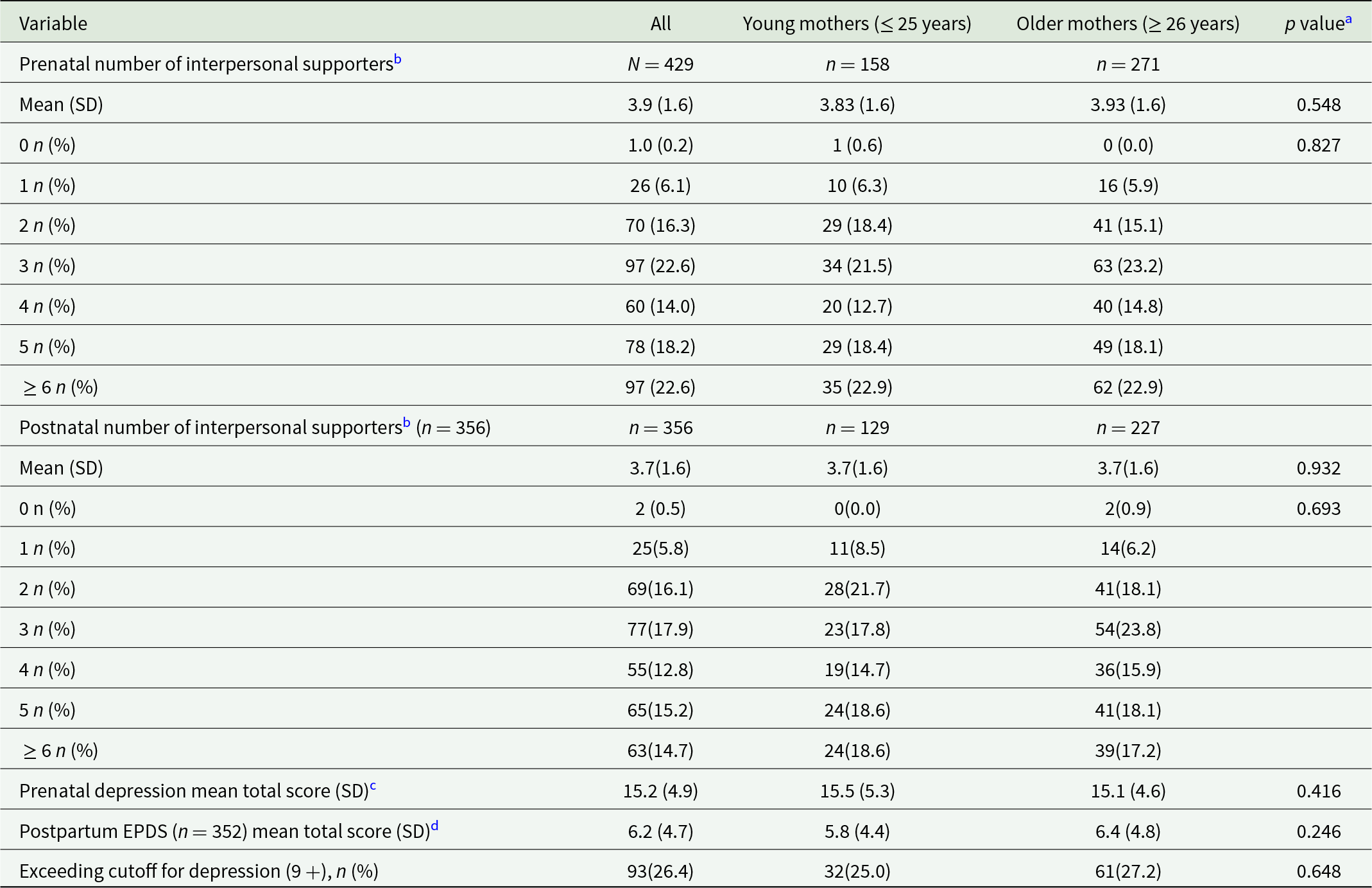
Figure 1 shows that in the segmented regression analysis, the regression line remained stable around 6.9 points for the EPDS score (range 0–30) for zero to three interpersonal supporters (β = − 0.035, P = 0.976), while it significantly decreased from 6.9 points to 5.6 points when the number of interpersonal supporters exceeded three (β = − 0.590, P = 0.013). Those with three or fewer interpersonal supporters showed higher EPDS scores than those with four or more interpersonal supporters (means of total EPDS scores: 6.92 vs. 5.58, respectively; P = 0.007). The results showed that the breakpoint at which the strength of the association between the number of interpersonal supporters during pregnancy and postpartum depressive symptoms changed was 3.0 (Fig. 1). These association patterns were similar even after adjusting for depressive symptoms during pregnancy (breakpoint = 3.0; the regression coefficients when the number of interpersonal supporters ≤ 3.0: β = − 0.007, P = .995, the number of interpersonal supporters > 3.0: β = − 0.516, P = 0.029). Additionally, the segmented regression analysis results among young mothers aged ≤ 25 years showed a breakpoint of 5.3 (Fig. 2). First-time mothers with five or fewer interpersonal supporters showed higher EPDS scores than those with six or more interpersonal supporters (means of total EPDS scores: 6.3 vs. 4.3, respectively; P= 0.029). In contrast, a breakpoint was not found among mothers aged ≥ 26 years (Fig. 3). These association patterns were similar even after adjusting for depressive symptoms during pregnancy.
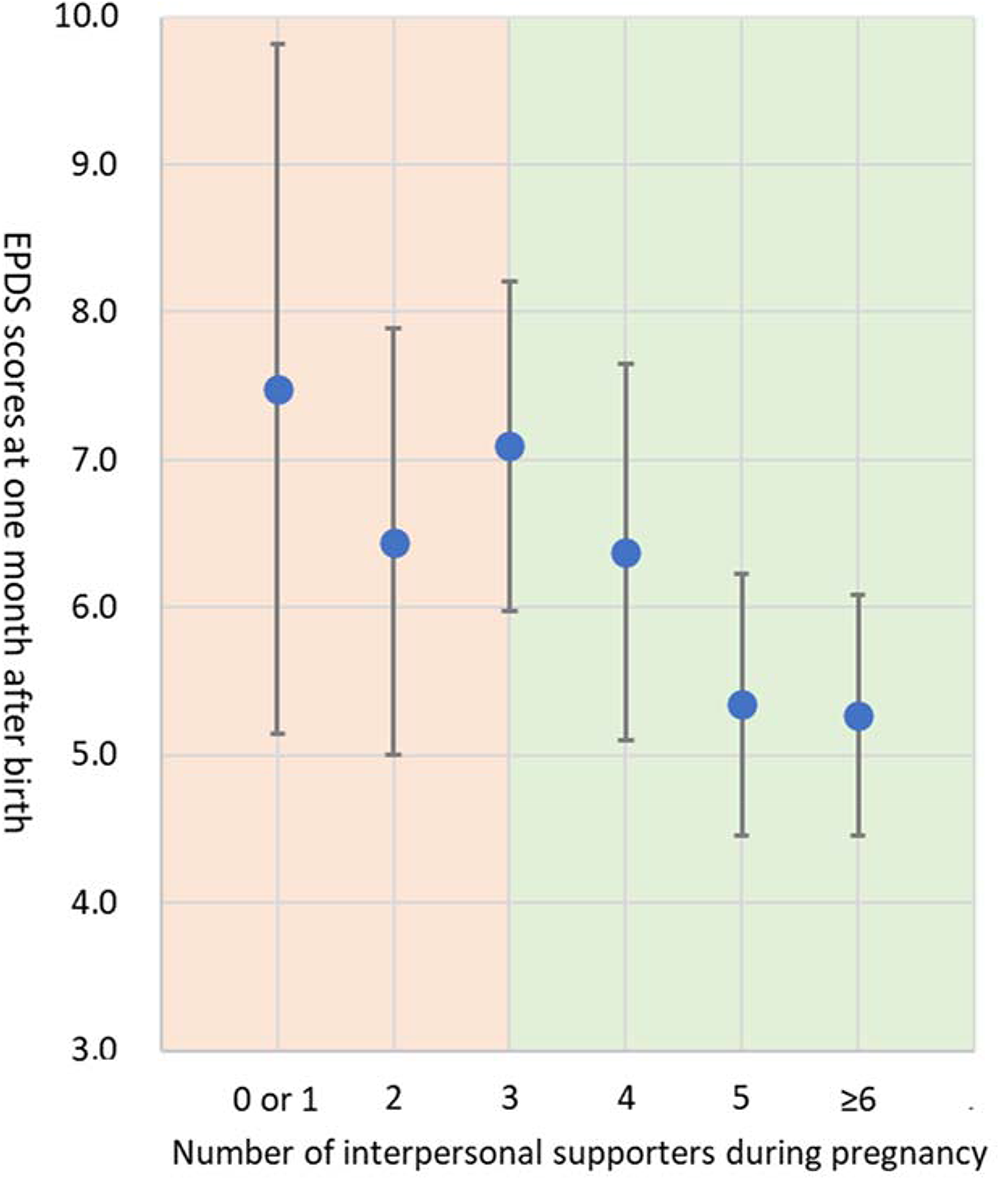
Figure 1. Association between the number of maternal interpersonal supporters during pregnancy and postpartum depressive symptoms 1 month after childbirth.
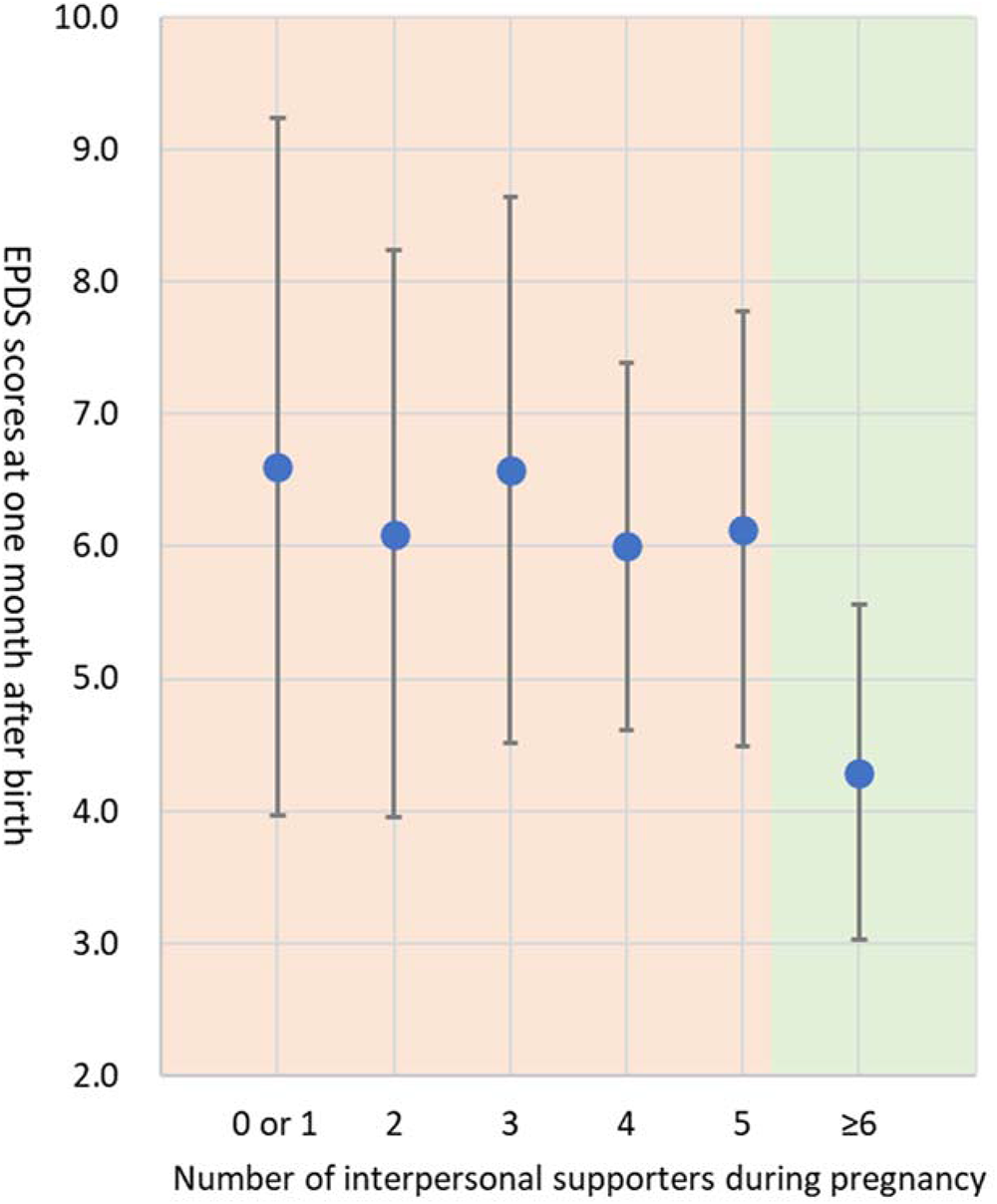
Figure 2. Association between the number of maternal interpersonal supporters during pregnancy and postpartum depressive symptoms one month after childbirth among young mothers ≤ 25 years-old.
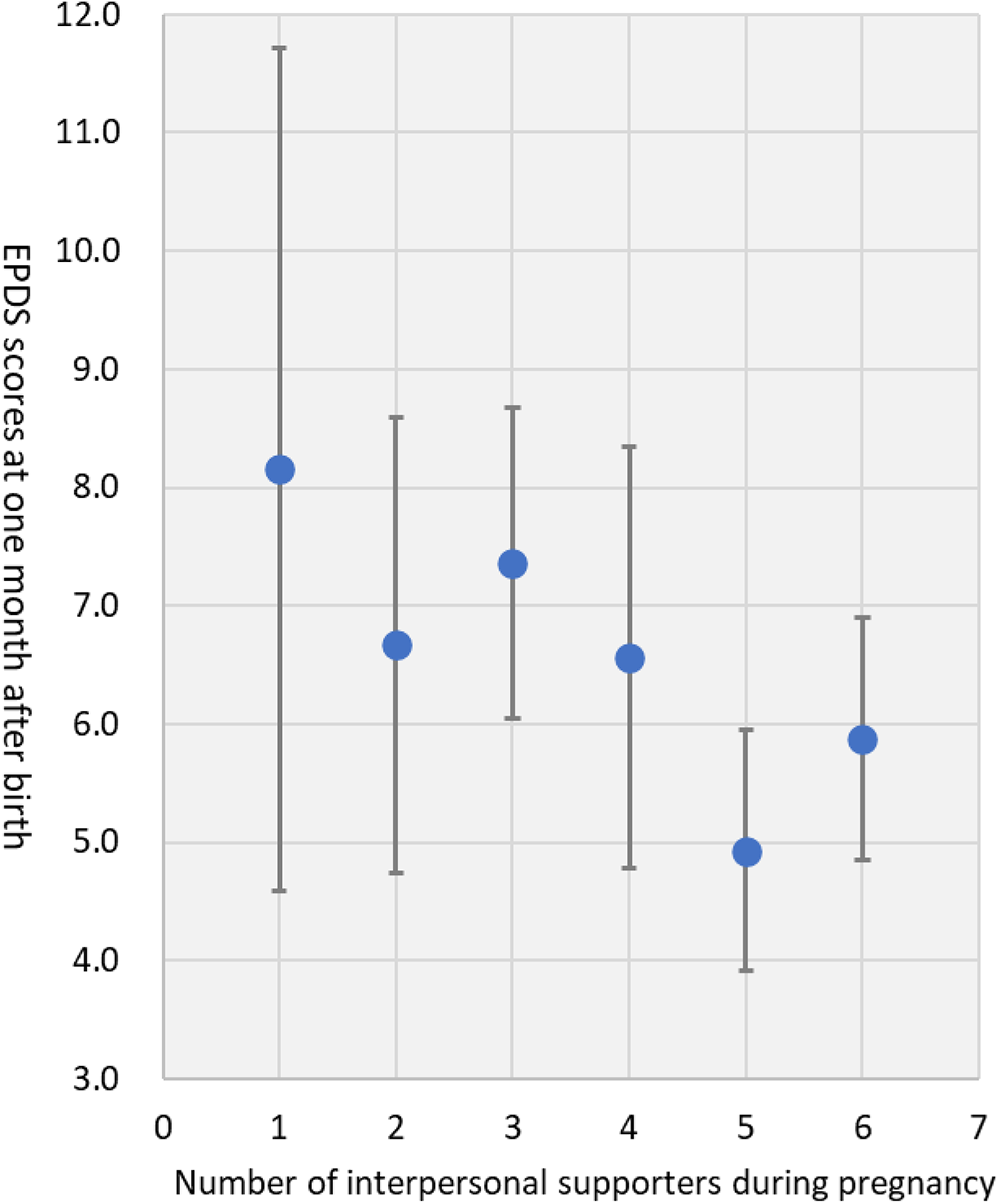
Figure 3. Association between the number of maternal interpersonal supporters during pregnancy and postpartum depressive symptoms 1 month after childbirth among mothers ≥ 26 years-old.
Discussion
This study explored the minimal number of interpersonal supporters in early pregnancy that was associated with lower postpartum depressive symptoms in a cohort of first-time mothers recruited from four municipalities in Tokyo. The results demonstrated that within the range of having zero to three supportive individuals during early pregnancy, the number of supporters was not associated with postpartum depression symptoms. However, when the number of supportive individuals was four or more, it was noted that higher numbers were associated with lower postpartum depression symptoms. Age-stratified analysis showed a linear relationship among first-time mothers aged ≥ 26 years, with the number of supportive individuals negatively associated with postpartum depressive symptoms. Conversely, among first-time mothers aged ≤ 25 years, the effects on postpartum depressive symptoms were non-significant unless they had six or more supportive individuals during early pregnancy. These findings remained consistent even after adjusting for antenatal depression.
Our findings resonate with previous studies highlighting the protective role of social support in reducing postpartum depression (Morikawa et al., Reference Morikawa, Okada, Ando, Aleksic, Kunimoto, Nakamura, Kubota, Uno, Tamaji, Hayakawa, Furumura, Shiino, Morita, Ishikawa, Ohoka, Usui, Banno, Murase, Goto, Kanai, Masuda and Ozaki2015; Taylor et al., Reference Taylor, Nath, Sokolova, Lewis, Howard, Johnson and Sweeney2022). Furthermore, this study extends the literature and addresses a key gap in evidence by quantifying a minimum number of interpersonal supporters associated with lower depressive symptoms. Previous research focused on the quality of support (Cankorur et al., Reference Cankorur, Abas, Berksun and Stewart2015; Razurel et al., Reference Razurel, Kaiser, Antonietti, Epiney and Sellenet2017); our findings suggest that, at least during pregnancy, the number of reliable supporters should be considered as another key element of interpersonal support associated with lower postpartum depression.
Additionally, our study suggests that the minimum number of interpersonal supporters during pregnancy may differ according to the age at first-time pregnancy. A younger age (≤ 25 years) was associated with a need for two additional interpersonal supporters to be associated with lower postpartum depressive symptoms. Notably, many participants reported fewer supporters than the suggested threshold: only 54.8% of all first-time mothers and 22.9% of young first-time mothers met the threshold (see Table 2). Furthermore, our findings indicate that the number of interpersonal supporters reported in our study was lower than in a previous study that included multiparous women and non-nuclear families (Morikawa et al., Reference Morikawa, Okada, Ando, Aleksic, Kunimoto, Nakamura, Kubota, Uno, Tamaji, Hayakawa, Furumura, Shiino, Morita, Ishikawa, Ohoka, Usui, Banno, Murase, Goto, Kanai, Masuda and Ozaki2015). The number of interpersonal supporters declined from pregnancy to postpartum assessment, suggesting that first-time mothers may be at greater risk of social isolation during pregnancy and after childbirth (Adlington et al., Reference Adlington, Vasquez, Pearce, Wilson, Nowland, Taylor, Spring and Johnson2023; Seymour-Smith et al., Reference Seymour-Smith, Cruwys and Haslam2021). Identifying individuals with particularly low interpersonal support in early pregnancy may help enhance mental health support for mothers postpartum.
Contrary to the findings of previous studies (Harron et al., Reference Harron, Gilbert, Fagg, Guttmann and van der Meulen2021), we found that the mean depressive symptoms of first-time mothers aged ≤ 25 years were lower than those of first-time mothers aged ≥ 26 years. Young mothers may have fewer challenges during pregnancy than older mothers due to being physically fit and having greater flexibility in working arrangements in the early career stages. Therefore, the risk of postpartum depressive symptoms among young mothers may reflect their complex underlying needs, which necessitate intensive resource investment, interpersonal support, and multifaceted life support, including financial, educational, and career development support.
This study had several limitations. First, we used the number of trusted persons in early pregnancy to investigate the minimum number of interpersonal supporters associated with lower postpartum depressive symptoms. Previous studies have shown that sources of support influence maternal mental health, and the perceived benefit of interpersonal support depends on the social contexts of pregnant women and their families (Wickramaratne et al., Reference Wickramaratne, Yangchen, Lepow, Patra, Glicksburg, Talati, Adekkanattu, Ryu, Biernacka, Charney, Mann, Pathak, Olfson and Weissman2022). We have not addressed these aspects in this study. However, to our knowledge, this longitudinal study with segmented regression analysis is the first to examine the minimum number of interpersonal supporters associated with lower postpartum depressive symptoms. Second, the data employed in the present study were derived from self-report questionnaires, which may have resulted in an underestimation of depressive symptoms. Third, our data focused on urban-dwelling first-time mothers. Future studies need to be conducted to expand the target group to include multiple pregnancies and rural dwellers. Therefore, the representativeness of our findings should be interpreted with caution. Fourth, the number of subjects in this study is relatively small; thus, caution should be exercised when generalising the results.
Conclusion
Our results suggest that having three or more interpersonal supporters in early pregnancy is associated with lower postpartum depressive symptoms among first-time mothers. Additionally, having six or more supporters appears to be associated with decreased postpartum depressive symptoms among young mothers. These findings suggest that tailored strategies to increase supporters around first-time pregnant women might be practical, depending on their age. Future research should consider expanding the sample size and conducting intervention studies to further explore the association between the number of interpersonal supporters during pregnancy and postpartum depression.
Availability of data and materials
The datasets generated during and/or analysed in the current study are available from the corresponding author on reasonable request.
Acknowledgements
The authors would like to thank the women who participated in the survey.
Author contributions
J.N. and M.N. contributed equally to this work.
Financial support
This work was supported by the Tokyo Metropolitan Government under the Prevention for Child Maltreatment project, JSPS KAKENHI (grant numbers JP18K10375, JP20H01777, JP20H03951, JP21H05171, JP21H05173, JP21H05174, JP21K10487, JP22K17509, JP23H03174, and JP24K14025), JST-Mirai Program (grant number JPMJMI21J3), and JST-RISTEX (grant number JPMJRS24K1).
Competing interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000. The Institutional Review Board of the Ethics Committee of the Tokyo Metropolitan Institute of Medical Science approved the research protocol and information statements, and all elements of consent were included (approval number: 21-39).







