Introduction
According to the United Nations High Commissioner for Refugees (UNHCR), the number of forcibly displaced individuals reached 110 million by mid-2023, marking a 1% rise from the end of 2022 (UNHCR, 2024). In response to evolving global needs since World War II, Australia’shumanitarian programme has expanded to offer permanent resettlement opportunities, with 17,875 placements offered in 2022–2023 and an intake of 20,000 places planned for both 2023–2024 and 2024–2025 (Australian Government Department of Home Affairs, 2024; Karlsen et al., Reference Karlsen, Phillips and Koleth2010). Humanitarian migrants are displaced persons who have been granted protection in the resettled country or have been resettled through programmes outside the asylum procedure (Bîrgău, Reference Bîrgău2022).
Humanitarian migrants often face numerous challenges during and after their migration process, including trauma, persecution, and difficulties establishing a new life in the countries of resettlement (Australian Government Department of Home Affairs, 2023; Jenkinson et al., Reference Jenkinson, Silbert, De Maio and Edwards2016). These hardships are not unique to Australia; similar experiences are observed in other high-income host nations (Sigvardsdotter et al., Reference Sigvardsdotter, Vaez, Hedman and Saboonchi2016). Many humanitarian migrants are at increased risk of mental health issues due to their past experiences and ongoing stressors, such as limited access to mental health services (Handiso et al., Reference Handiso, Paul, Boyle, Shawyer, Meadows and Enticott2024; Sarría-Santamera et al., Reference Sarría-Santamera, Hijas-Gómez, Carmona and Gimeno-Feliú2016; Silver et al., Reference Silver, Williams and Forty2023), discrimination, lack of social support (Alegría et al., Reference Alegría, Álvarez and DiMarzio2017; Handiso et al., Reference Handiso, Paul, Boyle, Shawyer, Meadows and Enticott2024) and financial hardship (Handiso et al., Reference Handiso, Paul, Boyle, Shawyer, Meadows and Enticott2024; Schenker, Reference Schenker2010). Furthermore, humanitarian migrants may be more vulnerable to elevated psychological distress (EPD) than host populations due to unique and compounding risk factors such as family separation, cultural shock, language barriers and social exclusion, which intensify post-migration stress and hinder social integration (Jurado et al., Reference Jurado, Alarcón, Martínez-Ortega, Mendieta-Marichal, Gutiérrez-Rojas and Gurpegui2017; Miller et al., Reference Miller, Hess, Bybee and Goodkind2018; Naseh et al., Reference Naseh, Zeng, Ahn, Cohen and Rfat2024; Nguyen et al., Reference Nguyen, Slewa-Younan and Rioseco2024). EPD, characterised by emotional suffering with symptoms such as depression and anxiety, is common among humanitarian migrants and often exacerbated by the compounding effects of pre- and post-migration adversities (Keramat et al., Reference Keramat, ComansT, Bailey, D and Dissanayaka2024; Mirowsky and Ross, Reference Mirowsky and Ross2002).
However, research comparing the mental health status of humanitarian migrants with that of host populations has produced conflicting findings. Some studies show higher levels of EPD among humanitarian migrants, while others indicate higher levels among the host population or no significant differences (Giacco et al., Reference Giacco, Laxhman and Priebe2018; Priebe et al., Reference Priebe, Giacco and El-Nagib2016). For instance, some studies have reported EPD of over 20–35%% among humanitarian migrants (Walther et al., Reference Walther, Kröger, Tibubos, Ta, Von Scheve, Schupp, Hahn and Bajbouj2020), while others have found similar or even higher rates among host populations, ranging from 20% to 35%, highlighting the inconsistency in findings and the need for further comparative research (Giuliani et al., Reference Giuliani, Palumbo, Giordano, Perrottelli, Pezzella, Caporusso, Bucci, Corrivetti, Storti and Piras2023; Lindert et al., Reference Lindert, von Ehrenstein Os, Priebe, Mielck and Brähler2009). Methodological limitations such as non-comparable datasets, small or non-representative samples, inconsistent mental health measures and limited use of matching methods reduce the utility of these findings for policymakers and programme planners (Minas et al., Reference Minas, Kakuma, Too, Vayani, Orapeleng, Prasad-Ildes, Turner, Procter and Oehm2013; Watson and Wooden, Reference Watson and Wooden2002).
This study addressed these gaps by employing a high-quality dataset, advanced matching approaches, a validated data collection tool and a representative sample from both the Australian-born group and humanitarian migrants, to compare EPD. We aimed to provide robust evidence on the patterns and predictors of EPD in these two groups and to explore whether demographic, social and socio-economic factors account for any observed disparities. By doing so, we hope to inform more targeted and effective mental health interventions and policies for humanitarian migrants.
Methods
Data source and samples
Our study used two data sets to compare EPD among humanitarian migrants and Australian-born adults: humanitarian migrants’ data were from the fifth wave of the Building a New Life in Australia (BNLA) survey conducted in 2017/18, and the nationally representative Australian National Health Survey (ANHS) conducted in 2017/18. Using data sources from the same year allowed us to compare the humanitarian migrants and Australian-born populations directly. The response rates for the Australian-born database and the humanitarian migrant’s database were approximately 76.1% and 81.0%, respectively (Australian Bureau of Statistics, 2018; Australian Government: Department of Social Services, 2022).
The BNLA dataset was a longitudinal survey of 2,399 humanitarian migrants. It provides a nationally representative sample of individuals from diverse cultural backgrounds. These participants arrived in Australia and received permanent protection visas through the country’s humanitarian programmes between May and December 2013 (Australian Government: Department of Social Services, 2022). Data collectors obtained a list of all eligible participants from the Australian Government’s Department of Immigration and Border Protection, and study participants provided consent to participate in the survey before data collection commenced. The survey tool was checked for internal consistency and translated into 19 languages to ensure that most participants could respond in their primary language (Australian Government: Department of Social Services, 2022).
The ANHS was an ongoing national health survey designed to collect a comprehensive range of information about the health of the Australian population, including data on the prevalence of various health conditions and mental well-being. The 2018 survey data were accessed through the public use microdata file platform, and then a sample consisting solely of Australian-born individuals were extracted for the matched analysis (Australian Bureau of Statistics, 2021). This comparison group was used to avoid mixing Australian-born individuals with other migrants. The sample included a 1:2 ratio of humanitarian migrants and Australian-born participants. To maintain this proportional representation, we randomly selected two Australian-born participants for every one humanitarian migrant included in the analysis. Matching variables were selected based on relevance to outcome variables and their availability and comparability across both datasets, comprising age, gender and remoteness/location (Figure 1).
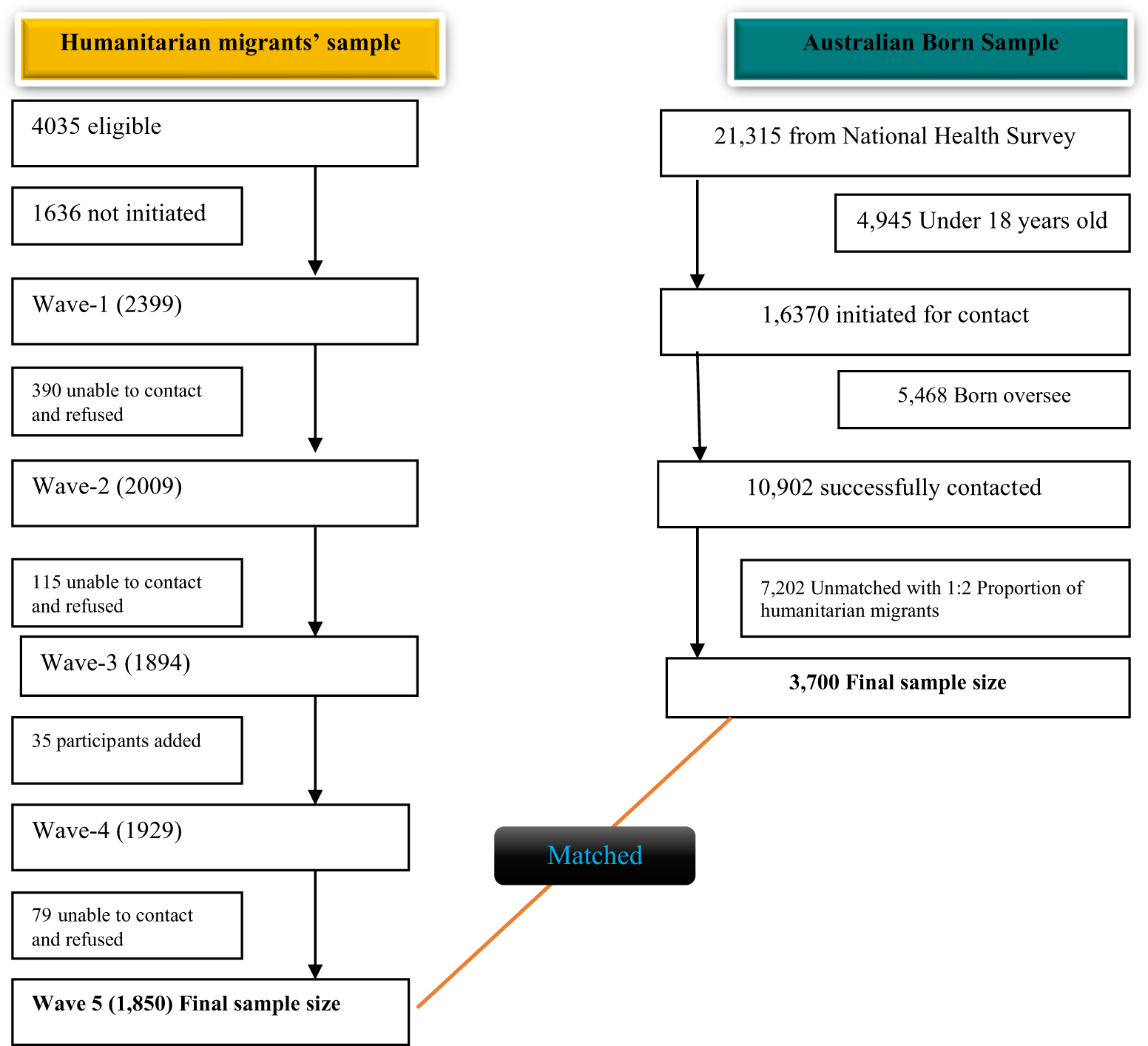
Figure 1. Flow chart for selecting and matching study participants from humanitarian migrants and the Australian-born population.
Outcome measures
The ANHS reported the EPD ratings for each of the 10 items in the 10-item Kessler Psychological Distress scale (K10) (Kessler et al., 2002). However, the BNLA dataset had only six of these same items, called the 6-item Kessler scale (K6). Therefore, we examined the K6 items in both surveys. K6 scale scores (Australian scoring) range from 6 to 30. The Australian Bureau of Statistics (ABS) recommends, in dichotomous analysis, the use of a score of 19 or higher to define EPD (Kessler et al., Reference Kessler, Green, Gruber, Sampson, Bromet, Cuitan, Furukawa, Gureje, Hinkov, Hu, Lara, Lee, Mneimneh, Myer, Oakley-Browne, Posada-Villa, Sagar, Viana and Zaslavsky2010) and is indicative of probable serious mental illness (Australian Bureau of Statistics, 2021). These scores (≥19) will here be described as ‘EPD’ (Australian Bureau of Statistics, 2012; Harvard University, 2010).
Independent variables
The following covariates were investigated in both datasets. Sex was asked as a binary of male and female. Age by years was categorised into the following groups: 18–24 years, 25–34 years, 35–44 years, 45–54 years, 55–64 years and 65+ years. Educational status was asked as highest level completed then classified according to the International Standard Classification of Education (ISCED) (Australian Bureau of Statistics, 2015) as High education ([Levels 5–8]: ISCED 5: Short-cycle tertiary education; ISCED 6: Bachelor’s or equivalent level; ISCED 7: Master’s or equivalent level; ISCED 8: Doctoral or equivalent level); Medium education ([Levels 3 and 4]: ISCED 3: Upper secondary education; ISCED 4: Post-secondary non-tertiary education); and Low education ([Levels 0–2]: ISCED 0: Early childhood education [‘less than primary’ for educational attainment]; ISCED 1: Primary education; ISCED 2: Lower secondary education). Self-rated health condition (excellent, very good, good, fair, poor), income Quintile (Quintile 1–5) and employment included full-time/part-time/casual (yes/no).
Two area covariates were also investigated: (1) Location/remoteness was classified as major cities, inner regional, and outer/other regional based on the Australian Bureau of Statistics (21), and (2) Index of Relative Socio-economic Disadvantage (IRSD) (Quintile 1–5), also determined by the ABS using a variety of area-based information such that IRSD Quintile 1 represents the most disadvantaged areas.
Statistical analyses
Statistical analysis was performed using Stata version 18 (StataCorp, 2023) to investigate the relationship between EPD and the characteristics of humanitarian migrants and Australian-born. A modified Poisson regression model with robust variance was used to identify predictors of EPD for both groups. Univariable and multivariable analyses were conducted to determine the associations between covariates and outcome variables. Crude and adjusted relative risks (aRR) with 95% confidence intervals were presented for predictor variables with P-values <0.05. The variable selection process for the final model employed adaptive Least Absolute Shrinkage and Selection Operator (LASSO) methods. Cross-validation was used to determine the optimal alpha hyperparameter to ensure the best performance of the LASSO regression. The final model included variables such as self-rated health condition, location/remoteness, employment status, Index of Relative Socio-economic Disadvantage (IRSD) for the area, income, educational status, age categories and sex. The Hosmer–Lemeshow statistic and omnibus tests assessed the goodness of fit. We tested interaction effects for the outcome variables; however, a significant interaction was observed only between sex and self-rated health in the final step of the model. Additionally, we estimated marginal effects to measure changes in the likelihood of EPD given self-rated health conditions, age, income level, and IRSD quintile for both humanitarian migrants and the Australian-born. We followed the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) (Cooper et al., Reference Cooper, Enticott, Shawyer and Meadows2019) guidelines in reporting this study. Missing data were handled using multiple imputation by chained equations (MICE), following StataCorp’s recommendations. This process involved constructing imputation models for all explanatory variables with missing values. The Stata commands ‘mi impute’ and ‘mi estimate’ were then used to generate, combine and analyse data across 20 imputed datasets (StataCorp, 2023).
Results
Characteristics of study participants
The main analysis included 5,550 participants, comprising 1,850 humanitarian migrants and 3,700 matched (by age, sex and location/remoteness) individuals born in Australia. Table 1 displays the characteristics of the humanitarian migrant and Australian-born study participants across various socio-demographic, educational and socio-economic variables. In both samples, most participants were male (52.6%) and aged between 18 and 44 (64.1%). Most of the female (69.2%) and male (64.1%) humanitarian migrants had low education levels, whereas the largest proportion of Australian-born women had a high level of education (46.9%), and in men, the largest proportion had a medium level of education (47.7%). Employment status differs significantly between humanitarian migrants and the Australian-born group. Most humanitarian migrants resided in the most disadvantaged IRSD areas, 61.1% (n = 1131), compared to the Australian-born counter sample; household income showed a similar trend (Table 1).
Table 1. Socio-demographic characteristics of Australian-born and humanitarian migrant study participants, n (%)
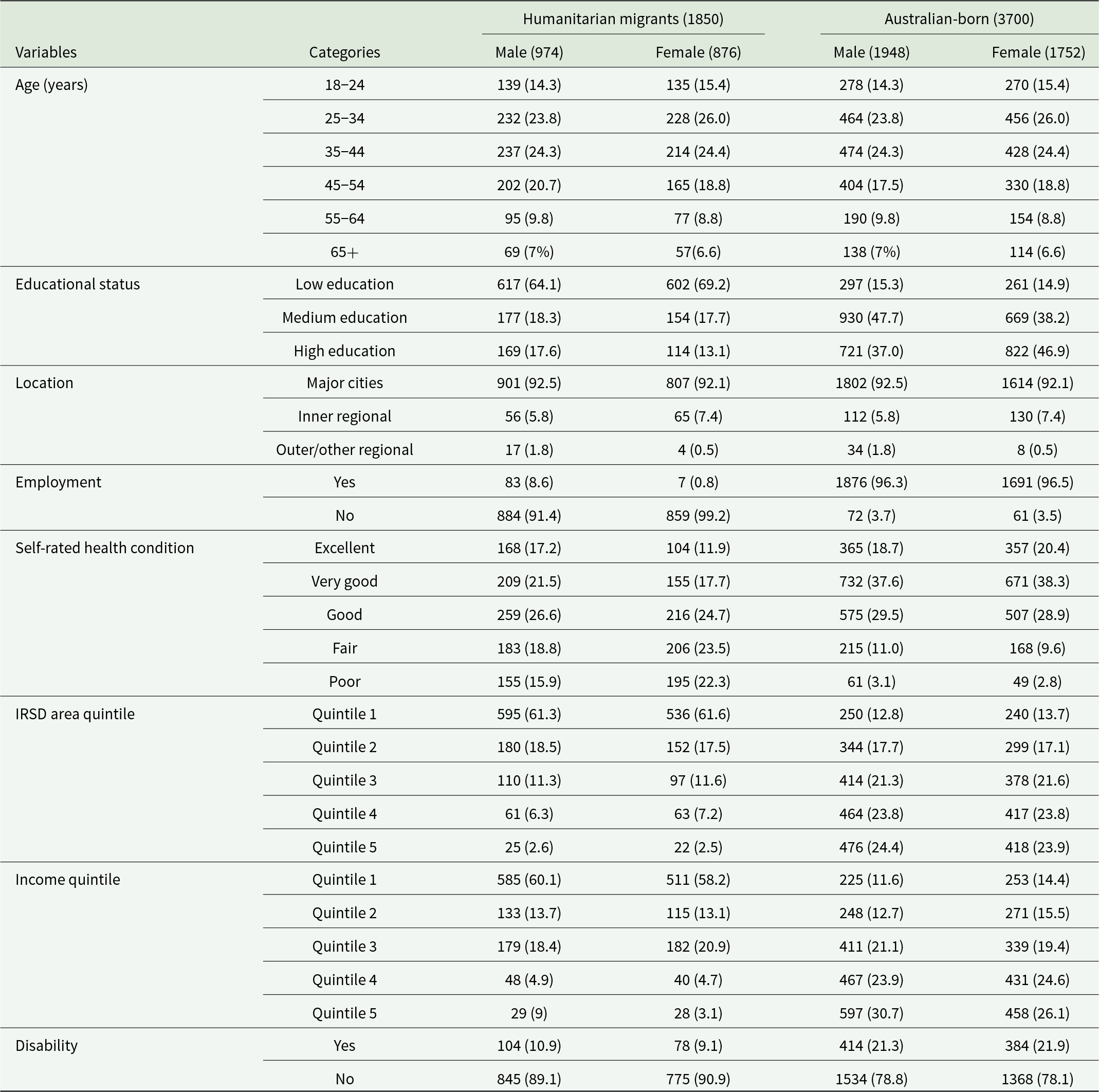
IRSD: Index of Relative Socio-economic Disadvantage for areas, IRSD Quintile 1 represents the most disadvantaged areas.
Comparison of EPD between humanitarian migrants and Australian-born
The overall prevalence of EPD was higher among humanitarian migrants (17.2%, 95% CI: 15.5, 18.9) compared to Australian-born adults (14.5%, 95% CI: 13.3, 15.6), and this occurred for both females and males (Fig. 2).
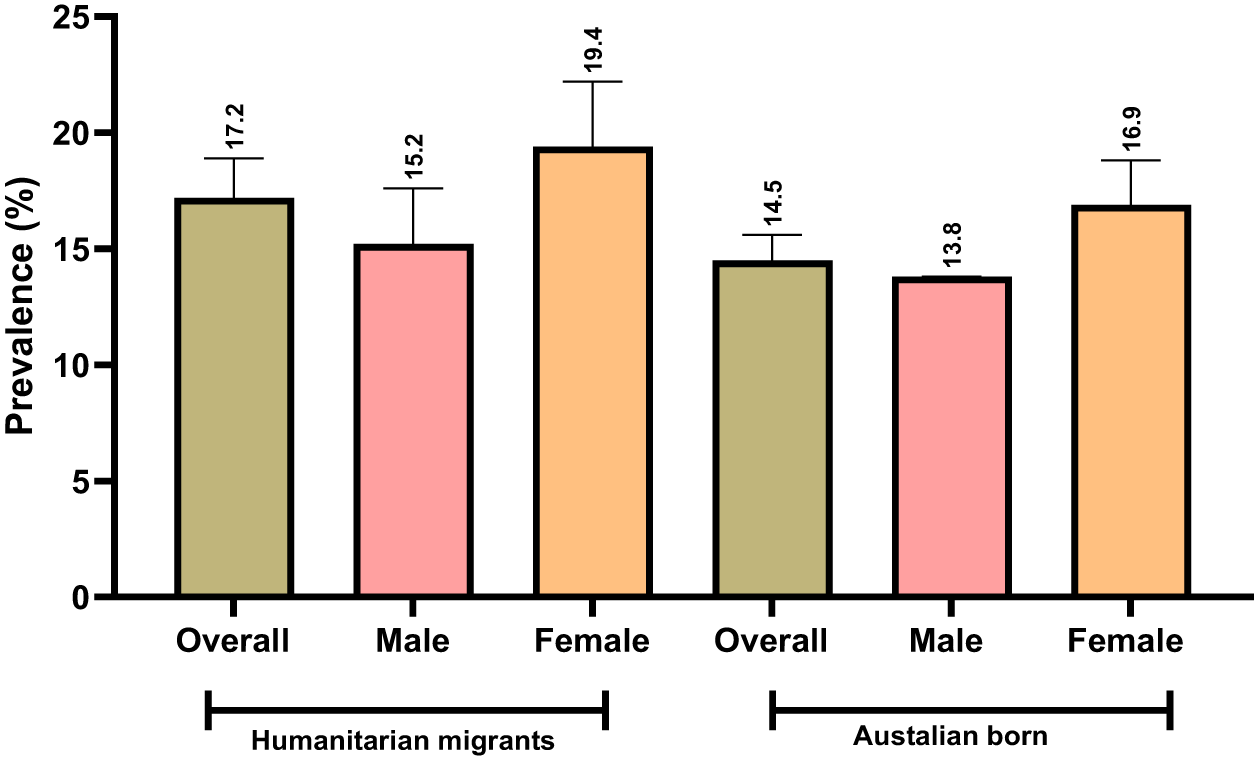
Figure 2. Prevalence of EPD in humanitarian migrants and matched Australian-born study participants (95% confidence interval).
A higher proportion of Australian-born females (23.3%) and males (16.2%) in the youngest age group (18–24) reported EPD compared with 8.9% and 9.4% of female and male humanitarian migrants, respectively. For individuals with low educational status, EPD was observed in 14.6% (n = 90) male and 19.3% (n = 116) female humanitarian migrants, compared to 22.6% (n = 67) male and 23.4% (n = 61) female individuals in the Australian-born. A greater proportion of Australian-born adults reported EPD if they self-reported fair or poor health. For those with fair health, EPD levels were 8.8% and 20.7% higher in Australian-born males and females, respectively, compared to humanitarian migrants. For those with poor health, EPD was 11.9% higher in males and 19.2% higher in females among the Australian-born population (Table 2).
Table 2. Prevalence of EPD between humanitarian migrants and Australian-born, stratified by gender across various factors
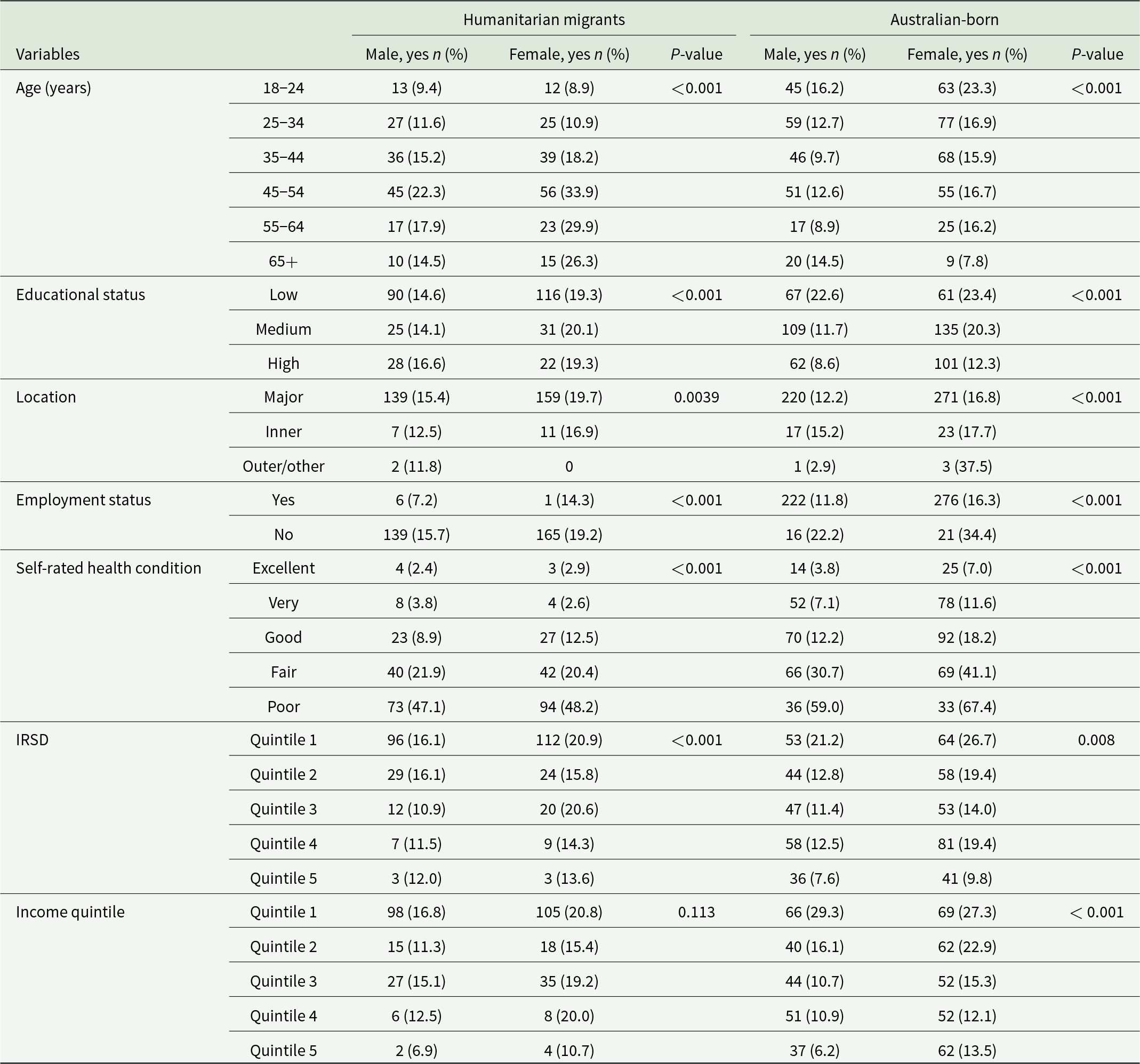
IRSD: Index of Relative Socio-economic Disadvantage for areas; IRSD Quintile 1 represents the most disadvantaged areas.
Humanitarian migrants residing in IRSD Quintile 1 reported EPD in 16.1% (n = 96) males and 20.9% (n = 112) females. In comparison, the Australian-born showed distress in 21.2% (n = 53) males and 26.7% (n = 64) females, indicating a 5.1% and 5.8% higher distress in Australian-born males and females, respectively. In Quintile 2, EPD was 3.3% higher in humanitarian migrant males, while it was 3.6% higher in females from the Australian-born (Table 2).
Predictors of EPD in humanitarian migrant and Australian-born
After adjusting for socio-demographic factors, self-rated health condition, gender and age category emerged as key determinants of EPD in both Australian-born individuals and humanitarian migrants (Table 3). However, remoteness, income and IRSD area quintiles were determinant factors exclusively for the Australian-born population.
Table 3. Crude relative risk estimates in comparing EPD between humanitarian migrants and a matched Australian-born group
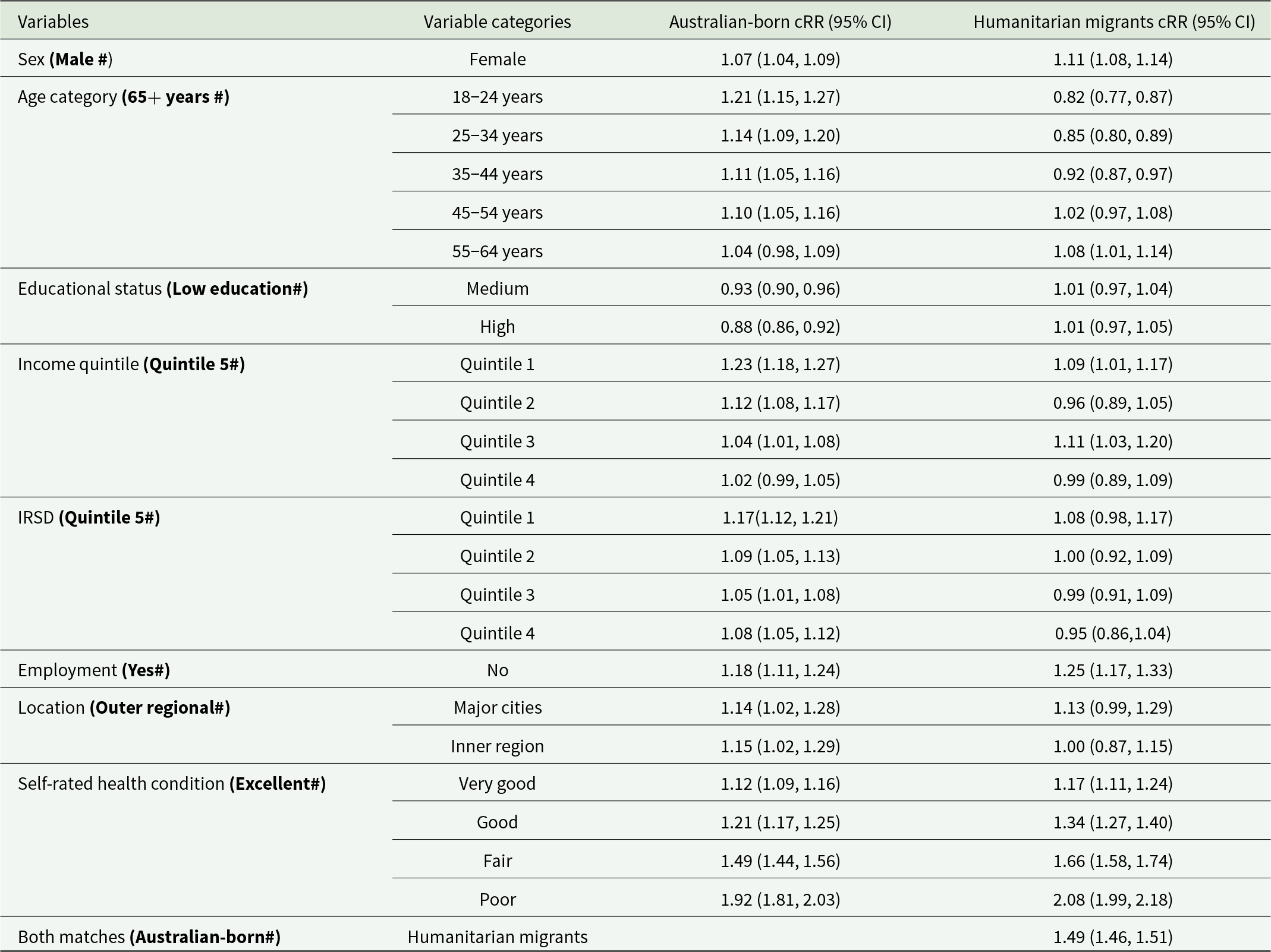
cRR: Crude Relative Risk; IRSD: Index of Relative Socio-economic Disadvantage for areas; IRSD Quintile 1 represents the most disadvantaged areas.
Overall, humanitarian migrants experienced a 16% higher relative risk of EPD compared to Australian-born individuals (aRR: 1.16, 95% CI: 1.11–1.21). In both the Australian-born and humanitarian migrants, females had a greater relative risk of distress compared to males, and the magnitude of this effect appeared similar in the two groups: females exhibited a 6% increased relative risk of EPD compared to males among Australian-born individuals (aRR: 1.06, 95% CI: 1.04–1.08) and 4% higher relative risk among humanitarian migrants (aRR: 1.04, 95% CI: 1.02–1.07). However, the distress effect size for age was more significant in the Australian-born compared to humanitarian migrants, as compared to the 65+ age group, the youngest group of 18–24 years had a relative risk of 1.36 for Australian-born and 1.19 for humanitarian migrants (aRR: 1.36; 95% CI: 1.28–1.43) and (aRR: 1.19; 95% CI: 1.12–1.27) respectively. Australian-born individuals, those aged 25–34 and 35–44, have a 1.29 (aRR: 1.29; 95% CI: 1.23–1.37) and 1.25 (aRR: 1.25; 95% CI: 1.19–1.32) times higher relative risk, respectively, whereas humanitarian migrants in these same age groups have a comparatively lower relative risk, with aRRs of 1.11 (95% CI: 1.05–1.18) for ages 25–34 and 1.12 (95% CI: 1.06–1.19) for ages 35–44, relative to those over 65 (Fig. 3). However, the marginal effect indicates that humanitarian migrants consistently experience higher levels of EPD than Australian-born individuals across all age categories. Although distress levels decrease slightly with age, the gap between the two groups remains significant (Fig. 4).
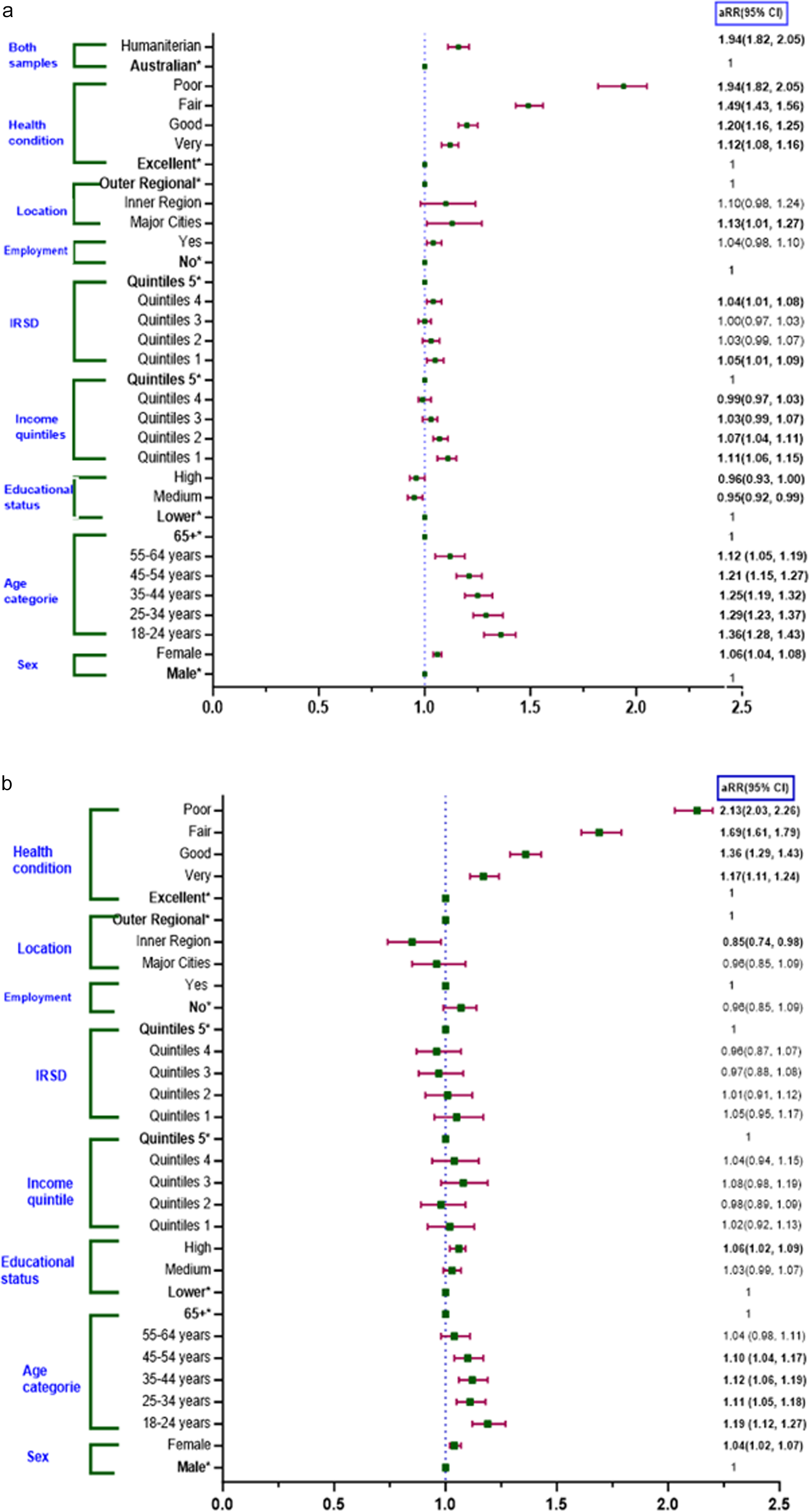
Figure 3. Relative risk estimates comparing EPD between Australian-born (a) and a matched humanitarian migrants (b). IRSD: index of relative socio-economic disadvantage for areas (IRSD Quintile 1 represents the most disadvantaged areas); aRR: adjusted risk ratio (adjusted for self-rated health, age, sex, employment status and location). Note: * indicates the reference categories.
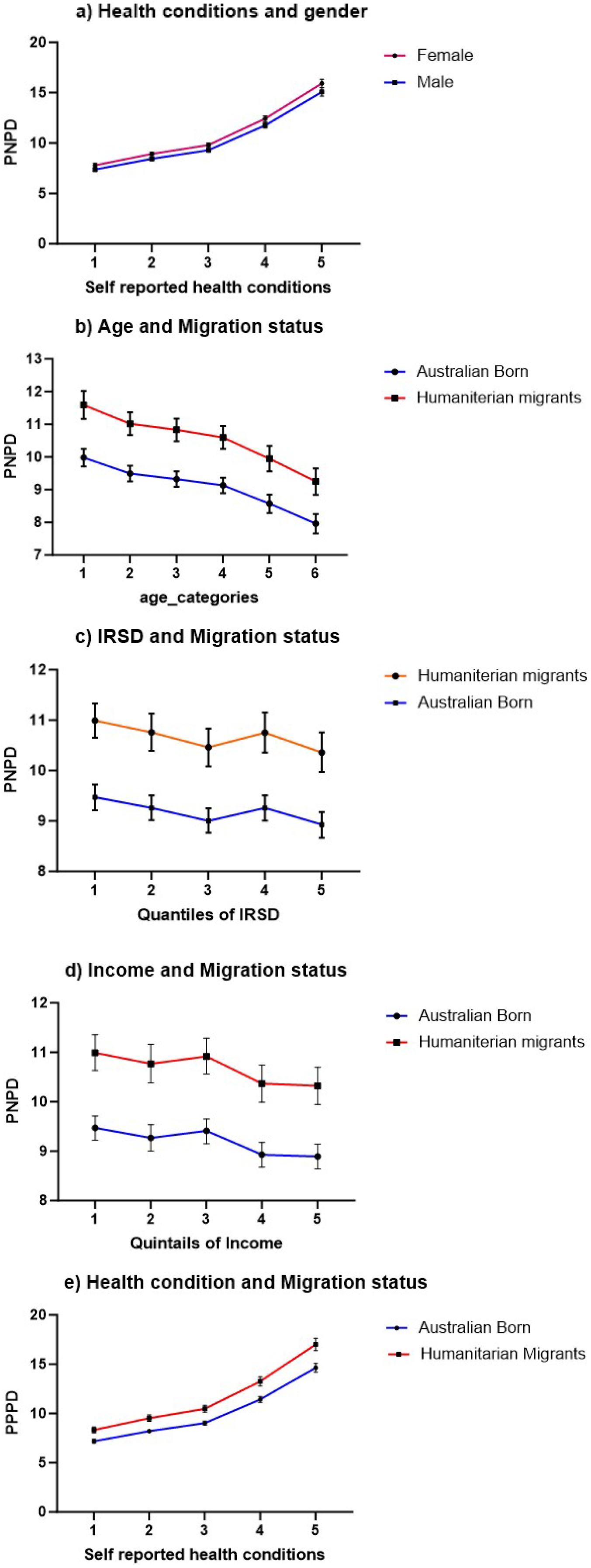
Figure 4. Marginal effects on EPD score of humanitarian migrants and Australian-born. (a) Margin effect of gender and self-rated health conditions; (b) margin effect between age and migration status; (c) margin effect of IRSD quintile and migration status; (d) margin effect of income level and migration status; (e) margin effect of self-rated health condition and migration status.
In an Australian-born study, participants with lower income quintiles were associated with an increased relative risk of EPD compared to the fifth quintile, particularly in Quintiles 1 and 2, which had 1.11- and 1.07-times higher relative risk of EPD, respectively (aRR: 1.11; 95% CI: 1.06–1.15 and aRR: 1.07; 95% CI: 1.04–1.11). Australian-born individuals residing in IRSD Quintile 1 had a 5% higher relative risk, and those in Quintile 4 had a 4% higher relative risk of EPD compared to those in the Quintile 5 (aRR: 1.05; 95% CI: 1.01–1.09 and aRR: 1.04; 95% CI: 1.01–1.08). For Australian-born individuals, medium levels of education were associated with a 5% lower relative risk of EPD compared to lower education levels (aRR: 0.95; 95% CI: 0.92–0.99). In contrast, humanitarian migrants with higher education face a 6% higher relative risk of EPD compared to those with lower education levels (aRR: 1.06; 95% CI: 1.02–1.09). Among Australian-born individuals, those living in major cities were at 1.13 times higher relative risk of EPD compared to those residing in outer regions (aRR: 1.13; 95% CI: 1.01–1.27) (Fig. 3).
The effect size for EPD was higher among humanitarian migrants than Australian-born individuals, particularly when self-rated health was considered. Humanitarian migrants who rated their health as poor and fair had a 2.13- and 1.69-times higher relative risk of experiencing EPD, respectively, compared to those reporting excellent health (aRR: 2.13; 95% CI: 2.03–2.26 and aRR: 1.69; 95% CI: 1.61–1.79) (Fig. 3). Marginal effects further indicate that humanitarian migrants consistently experience higher EPD across various health conditions (Fig. 4).
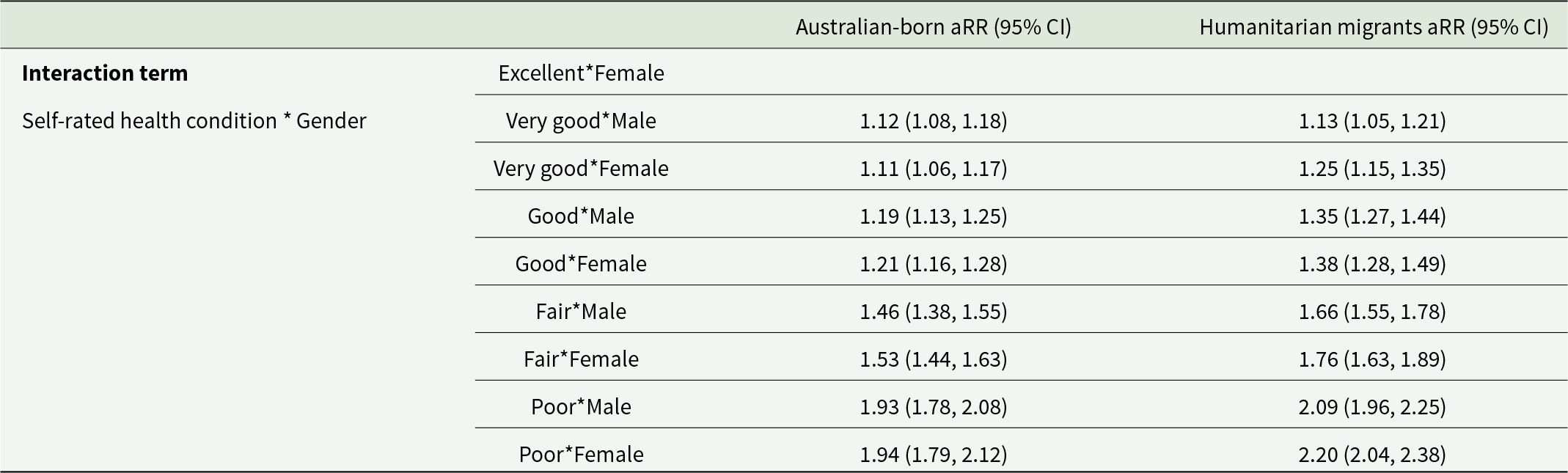
Additionally, we examined the relative risk of EPD by considering the interaction between self-rated health and gender for both Australian-born individuals and humanitarian migrants. In both groups, poorer self-rated health was associated with higher aRR across genders. For Australian-born individuals, males with poor health have an aRR of 1.93, while females have an aRR of 1.94. Humanitarian migrants show even higher aRRs, with males at 2.09 and females at 2.20. Humanitarian migrants experience higher aRRs than Australian-born individuals (Table 4).
Table 4. Interaction term for self-rated health condition and gender in Australian and humanitarian migrants
Discussion
The study revealed that humanitarian migrants (17.2%) experienced higher levels of EPD compared to Australian-born adults (14.5%), with a 1.16 times higher relative risk (aRR) after adjusting for factors such as self-rated health condition, age, gender, employment status and location. In both groups, females exhibited a higher risk of EPD than males, with comparable effect sizes. However, age played a more substantial role in EPD among Australian-born individuals, with younger adults demonstrating higher aRRs than older adults. Poor and fair self-rated health conditions had a higher impact on distress among humanitarian migrants compared to Australian-born individuals. Additionally, among Australian-born individuals, those in the lowest income quintiles exhibited significantly higher distress risks than those in the highest income quintile, while no significant income-related effects were observed for humanitarian migrants.
Younger study participants and women in both groups exhibited more EPD compared to older participants and males; this observation aligns with a study from the United States and another study conducted in Australia (Jarallah and Baxter, Reference Jarallah and Baxter2019; Li and Anderson, Reference Li and Anderson2016). The higher distress experienced by migrants in the younger age group may be at least partially attributable to stresses associated with displacement, including difficulties in acclimating to a newly resettled country, social isolation, pressure to adapt rapidly to a new culture and identity struggles (Cooper et al., Reference Cooper, Enticott, Shawyer and Meadows2019; Guskovict and Potocky, Reference Guskovict and Potocky2018; Handiso et al., Reference Handiso, Paul, Boyle, Shawyer, Meadows and Enticott2024). The increased distress observed in women and younger persons from both groups may be ascribed to their heightened susceptibility (Yuan et al., Reference Yuan, Luo, Yan, Meng, Yu and Li2009). Among Australian-born individuals, the relative risk of EPD was lower with moderate education relative to lower education levels, consistent with established knowledge, as elevated educational attainment is often associated with enhanced access to resources, superior socio-economic status, and more effective coping mechanisms (Ouwehand et al., Reference Ouwehand, Ridder and Bensing2009; Roohafza et al., Reference Roohafza, Sadeghi, Shirani, Bahonar, Mackie and Sarafzadegan2009). Education may offer a sense of agency and stability, mitigating the effects of stressors (Brännlund and Hammarström, Reference Brännlund and Hammarström2014; Mandemakers and Monden, Reference Mandemakers and Monden2010). In terms of self-assessed health, Australians in poor health had the highest levels of EPD relative to humanitarian migrants, perhaps attributable to elevated expectations and perceived inequities in healthcare access (Brijnath et al., Reference Brijnath, Antoniades and Temple2020).
Lower income level was also correlated with increased EPD in both groups. Low-income individuals face financial hardship as well as limited access to healthcare, which can exacerbate EPD (Fukuda and Hiyoshi, Reference Fukuda and Hiyoshi2012; Isaacs et al., Reference Isaacs, Enticott, Meadows and Inder2018). Nevertheless, Australian-born individuals in lower-income quintiles exhibited higher EPD than humanitarian migrants, possibly due to greater expectations and perceived disparities in socio-economic status and access to resources (Brijnath et al., Reference Brijnath, Antoniades and Temple2020). Although the host population often have more stable living conditions, access to mental health services varies substantially with socio-economic disadvantage in the general population (Dawadi et al., Reference Dawadi, Shawyer, Callander, Patten, Johnson, Rosenberg, Lakra, Lin, Teede and Meadows2024). In some settings, humanitarian and non-governmental support may enhance service availability for migrants (Steel et al., Reference Steel, Silove, Giao, Phan, Chey, Whelan, Bauman and Bryant2009). As well, humanitarian migrants may have developed resilience from overcoming past adversities, which might buffer against EPD despite lower socio-economic conditions (Majumder,Reference Majumder2016).
Australian-born adults with fair or poor self-rated health conditions had higher EPD than humanitarian migrants. These discrepancies could result from better healthcare access in the host population, leading to higher detection and disclosure of EPD (Selkirk et al., Reference Selkirk, Quayle and Rothwell2014). In contrast, humanitarian migrants face barriers to accessing healthcare services, stigma and cultural differences, which have been found to result in lower reported distress levels (Jarallah and Baxter, Reference Jarallah and Baxter2019; Priebe et al., Reference Priebe, Giacco and El-Nagib2016). The host population may also have more chronic health conditions due to prolonged exposure to risk factors, contributing to a higher risk of EPD (Debnar et al., Reference Debnar, Carrard, Morselli, Michel, Bachmann and Peter2020).
Finally, EPD in Australian-born decreased with age. The oldest age group (65+) and those aged 55–64 had lower relative risk compared to younger groups, supported by other studies in Australia (Jorm et al., Reference Jorm, Windsor, Dear, Anstey, Christensen and Rodgers2005) but contrasting with others (Kilkkinen et al., Reference Kilkkinen, Kao‐Philpot, O’Neil, Philpot, Reddy, Bunker and Dunbar2007). Younger people experience more transitions, social pressures and uncertainties, contributing to higher distress levels than older individuals (Matud et al., Reference Matud, Díaz, Bethencourt and Ibáñez2020).
Policy implication
Humanitarian migrants experience 16% higher EPD compared to the Australian-born population, making targeted mental health services and support systems essential, including early identification using screening and diagnostic tools in clinical visits (Shawyer et al., Reference Shawyer, Enticott, Block, Cheng and Meadows2017, Reference Shawyer, Enticott, Doherty, Block, Cheng, Wahidi and Meadows2014). Policymakers should ensure these services are accessible to this group. Implementing community-based mental health programmes, improving access to culturally familiar support systems, and expanding transcultural mental health services can further enhance outcomes. In addition, addressing the identified disparities in education between humanitarian migrants and Australians is critical. Programmes promoting educational attainment and vocational training can empower individuals, alleviate financial stress and reduce EPD. For Australian-born individuals, particularly those in lower-income levels, providing financial assistance and social support services can help mitigate the impact of financial strain on mental health. Additionally, policies should focus on the specific stressors faced by young people and women, as these were the identified groups with higher EPD.
Strengths and limitations of the study
A major strength of this study was the utilisation of two high-quality, nationally representative data sources that were collected by the ABS and the Australian Government Department of Social Services, with the aim of informing health and social policies in Australia. Moreover, this study used a matched comparison group and advanced statistical approaches, and the matching methodology is novel (building on the methodology derived by JE (Shawyer et al., Reference Shawyer, Enticott, Doherty, Block, Cheng, Wahidi and Meadows2014) and provides an exemplar for other researchers to extract policy information from existing large data assets. Our study addressed the existing inconsistencies in the prevalence of EPD between humanitarian migrants and the host population using a large sample of study participants.
Despite these strengths, it has a few limitations. Although the response rates for both surveys were within acceptable ranges for large-scale population surveys, non-response bias remains a potential concern. This may limit the generalisability of the findings and could lead to underestimation or overestimation of the true prevalence of EPD. Future studies should consider implementing strategies to adjust for non-response bias. The reliance on self-report data more generally can also impact comparability since self-rated health may be influenced by cultural norms and individual perceptions. The final limitations relate to the K6, which was used instead of the K10 resulting in a potential loss of some information and a more constrained screening of mental illness (Furukawa et al., Reference Furukawa, Kessler, Slade and Andrews2003). There was also no confirmation of clinical diagnosis so the use of K6 alone as a screening tool has the potential to result in misclassification and inflate prevalence estimates (Shawyer et al., Reference Shawyer, Enticott, Block, Cheng and Meadows2017). Finally, this study employed a categorical cut-off (K6 ≥ 19) to define EPD, which is a common method but may limit sensitivity to variation in distress levels. Categorical thresholds can be somewhat arbitrary and may obscure more subtle gradients in mental health conditions. Future studies could benefit from examining continuous K6 scores to enhance the robustness of findings and better capture the full range of psychological distress.
Conclusion
This study found that EPD was more prevalent among humanitarian migrants compared to the Australian-born population, and this difference increased when self-rated health was considered. These results highlight the need to prioritise both physical and mental health interventions for this group. The findings point to significant disparities in EPD related to education levels, suggesting that these factors play a critical role in the mental health of both groups. Interestingly, income disparities were a prominent factor in EPD for the Australian-born sample, but not the humanitarian migrants. Overall, these findings indicate the necessity of routine screening for EPD among humanitarian migrants, as early identification can help prevent the progression to more serious mental disorders. Moreover, early and culturally appropriate screening, diagnosis and intervention are not only more effective but also more cost-efficient than addressing mental health complications at the resettlement phase of migrants, minimising long-term healthcare and social expenses.
Availability of data and materials
Data from the Building a New Life in Australia (BNLA) study are available to authorised users through the National Centre for Longitudinal Data, and data from the Australian National Health Survey (ANHS) are accessible via the Australian Bureau of Statistics website.
Acknowledgements
The authors sincerely thank all study participants, including humanitarian migrants and Australian-born individuals, for their time and contributions. The authors also acknowledge the Australian Government Department of Social Services and the Australian Bureau of Statistics for granting permission to use the data.
Financial support
Not applicable.
Competing interests
All authors declare no competing interests.
Ethical standards
Ethical clearance was not required to use the ANHS dataset because the data were provided in a non-identifiable format, meeting the criteria specified in Section 5.1.22 of the National Statement on Ethical Conduct in Human Research. The BNLA data was accessible to authorised researchers who had obtained permission from the Australian Government Department of Social Services. The Australian Institute of Family Studies Ethics Committee approved the data registered with the National Health and Medical Research Council. Measures to ensure the accuracy of responses to the government-administered survey included fostering trust, maintaining confidentiality and anonymity, and providing assurances against data misuse. Additionally, informed consent was obtained from all BNLA study participants by the data collectors at the Australian Institute of Family Studies. De-identified data was provided to researchers after a data usage and confidentiality deed was signed. The first and sixth authors obtained permission to use the dataset. The Monash University Human Research Ethics Committee advised that a separate ethics application was unnecessary, as this secondary data analysis within the BNLA programme had already received approval (2017-8041-8528).









