Introduction
COVID-19 was declared a pandemic by the WHO on 11th March 2020 (Perumal et al. Reference Perumal, Curran and Hunter2020). Older adults are at a higher risk of developing a severe form of COVID-19, often requiring hospitalization (Zhou et al. Reference Zhou, Yu, Du, Fan, Liu, Liu, Xiang, Wang, Song, Gu, Guan, Wei, Li, Wu, Xu, Tu, Zhang, Chen and Cao2020). COVID-19 infection is associated with a high incidence of delirium and is more likely to present with atypical symptoms in older adults (ISARIC Clinical Characterisation Group et al. Reference Abdukahil, Abe, Abel, Absil and Acker2021).
Delirium is an acute neuropsychiatric syndrome commonly associated with respiratory infections (Magny et al. Reference Magny, Le Petitcorps, Pociumban, Bouksani-Kacher, Pautas, Belmin, Bastuji-Garin and Lafuente-Lafuente2018). Classical risk factors for delirium have been categorized as predisposing and precipitating factors. Older adults often harbor more predisposing factors and experience delirium because of precipitants that may not affect younger adults (Marcantonio, Reference Marcantonio2017). Delirium is common in hospitalized older adults and is strongly associated with a poor prognosis and negative outcomes (Marengoni et al. Reference Marengoni, Zucchelli, Grande, Fratiglioni and Rizzuto2020).
The primary aim of this study was to investigate the risk factors of delirium in hospitalized older adults with COVID-19 by exploring the characteristics of patients with and without delirium. A secondary aim was to evaluate whether delirium is a predictor of mortality in this cohort of patients, independent of frailty and the burden of co-morbidities.
Methods
St. James’sHospital (SJH) in Dublin is an 865-bed university hospital with multiple specialist tertiary services. A cross-sectional cohort study was designed to collect data from inpatients at St James Hospital between March 2020–March 2021. Ethical approval for the study was granted by the St James Hospital and Tallaght University Hospital (SJH/TUH) Joint Research and Ethics Committee under the STTAR Bioresource for the COVID-19 project (O’Doherty et al. Reference O’Doherty, Hendricken Phelan, Wood, O’Brien, Sui and Mangan2022). The STTAR Bioresource study Project ID is JREC 2020-05 List 19 and further data protection impact assessment and review was performed by the SJH Research and Innovation Office (R&I no. 6949).
The inclusion criteria for our study were hospitalized adults, aged 65 years or older, who tested positive for SARS-CoV-2 infection on throat and/or high nasal swab by polymerase chain reaction (PCR) at any point during their admission. Patients aged 65 years or older were reviewed by the Psychiatry of Elderly Liaison Service; therefore, this was chosen as the age threshold. Data were collected through a retrospective clinical chart review by two senior psychiatry trainees (N. M. and E. M.), and variables were recorded and analyzed using IBM SPSS Statistics (Version 26). The electronic health record for each patient was reviewed by only one trainee as the data collection process was shared by the trainees. Data was pseudo-anonymised and recorded on a password protected spreadsheet, stored in a password protected hospital desktop computer with only limited access. Consent was not sought from the patients as it was not deemed necessary by the ethics committee for the study.
Sociodemographic data included age, sex, ethnicity, and living arrangements (i.e., community or nursing homes). Information about the admitting team, location of the first positive PCR test, and probable source of infection were also recorded. For the purpose of the study delirium was identified from the medical records by 4AT score of 4 or greater and/or when documented in the clinical notes based on the judgment of a senior clinician (consultant or senior registrar). The 4AT is a brief screening tool for delirium and is scored from 0 to 12 (www.the4AT.com) . 4AT is the preferred tool for delirium detection in COVID-19 patients due to its high sensitivity (83–100%), moderate specificity (70–99%), brevity, and ease of administration (Meagher et al. Reference Meagher, Adamis, Timmons, O’Regan, O’Keeffe, Kennelly, Corby, Meaney, Reynolds, Mohamad, Glynn and O’Sullivan2021).
The presence of preexisting (predisposing) risk factors for delirium was recorded: pre-existing cognitive impairment, history of major mental illness, use of anticholinergic medications by recording the anticholinergic cognitive burden (ACB) score, polypharmacy on admission (defined as being on ≥ 5 medications), smoking status, and clinical frailty score on admission using the Rockwood Clinical Frailty Scale (CFS). Pre-existing cognitive impairment was recorded from admission notes as mild cognitive impairment or dementia (specifying the type where known). Also if assessments were undertaken at the hospital memory clinic or geriatric clinic prior to admission they were available in the electronic health record for review for confirmation of pre-existing cognitive impairment. Older adults are more likely to be prescribed anticholinergic medications, and given their association with untoward effects, it is useful to quantify the anticholinergic burden when assessing relative risks. The ACB score was calculated using the Anticholinergic Cognitive Burden Scale (Boustani et al. Reference Boustani, Campbell, Munger, Maidment and Fox2008). CFS is a nine-point scale representing different levels of frailty (Rockwood, Reference Rockwood2005). It was also recommended by the National Institute for Health and Care Excellence guidance NG 159, the COVID-19 rapid guideline: critical care in adults to inform clinical decisions about escalation of care. If CFS was not recorded in the medical notes on admission, it was retrospectively determined by the researchers based on information about pre-morbid functioning two weeks before admission. The Charlson Co-morbidity index (CCI) was used to quantify the burden of medical comorbidity. CCI is a validated tool that calculates a score using a predefined list of comorbidities that can also be adjusted for age and predicts the risk of death within one year of hospitalization (Charlson et al. Reference Charlson, Szatrowski, Peterson and Gold1994; Charlson et al. Reference Charlson, Pompei, Ales and MacKenzie1987).
Laboratory parameters, such as CRP, lymphocyte, and neutrophil levels, were also noted. Extreme values were recorded within the first week of infection. Patients were admitted at different points during the course of infection; therefore, it was not possible to obtain the parameters for all patients on the same day of infection. Prescription of psychotropic medications and referral to the Psychiatry for the Elderly Liaison Service were used as proxy indicators for delirium severity. Past psychiatric history was recorded for all patients as stated on the admission notes, irrespective of referral to Psychiatry for the Elderly Liaison Service. It is likely that this data is incomplete as not all patients had their past psychiatric history detailed in their admission notes, and not all patients were seen by the Psychiatry for the Elderly Liaison Service. Data on the requirement for oxygen, ventilator use, need for steroids, and clinical outcomes, including length of hospital stay, mortality, and discharge destination, were also recorded.
Statistical analysis
Demographic and clinical variables of the study participants were summarized using descriptive statistics. Continuous variables are presented as median or mean± standard deviation, and categorical variables as absolute numbers or proportions. Predisposing determinants of delirium between patients with and without delirium were assessed using the chi-square test or independent samples t-test, according to the variable type. Statistical significance was defined at a level of 95%, with a p-value of <0.05. Logistic regression was used to test the association between the independent variables and the dependent variable (in-hospital mortality).
Results
Characteristics of patients
There were 9246 patients, aged 65 years or older, who were admitted to St James Hospital during the study time period. A total of 261 patients met the inclusion criteria for the study during the defined period. The mean age of the participants was 77.1 years. 51.3% (n = 134) were male and 98.8% of the study population was of white ethnic origin. 71.6% (n = 187) of the patients were admitted under the care of a medical team, 20.3% (n = 53) under a dedicated medical ‘COVID-19 team’ and 8.0% (n = 21) were under surgical teams. Most patients were residing at home (93.5%, n = 244) prior to admission, with only 3.8% (n = 10) residing in a nursing home and 1.5% (n = 4) in sheltered housing. Very few patients (7.28%, n = 19) were current smokers at admission. In most cases (70.5%, n = 184), the location of the first positive PCR for SARS-CoV-2 was at St James’s Hospital, 25.7% of the participants (n = 67) tested positive in the community prior to admission, and 2.67% (n = 7) of the patients tested positive for SARS-CoV-2 in a convalescence unit or nursing home prior to admission to SJH. The source of infection was deemed as hospital acquired in 40.6% (n = 106) of the cases, community acquired in 54.8% (n = 143) of the cases, and acquired from a nursing home in 3.8% (n = 10) of the cases. More than half of the patients (55.17%, n = 144) were prescribed 5 or more medications at the time of admission.
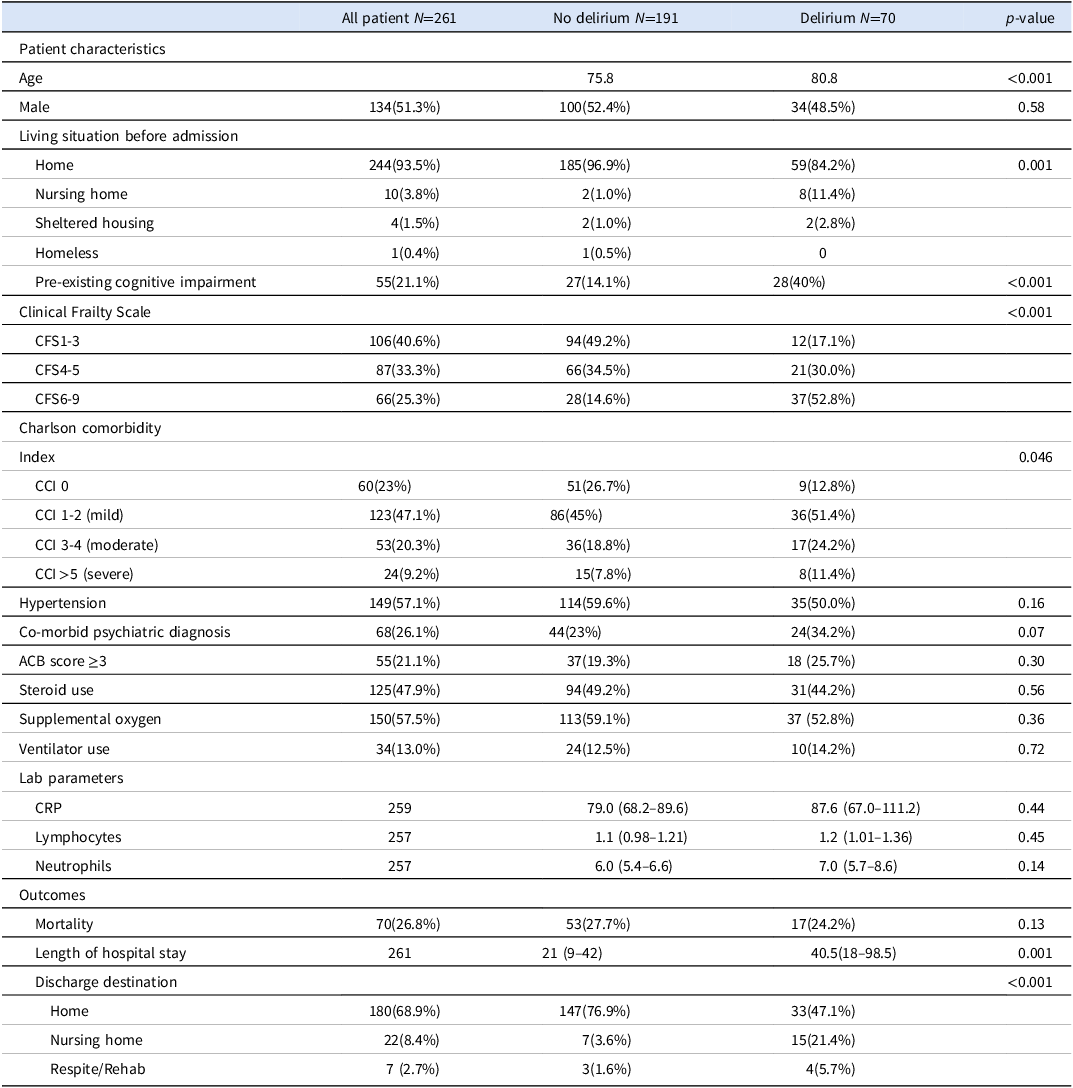
Delirium was detected in 70 patients (26.8%) in our cohort during hospitalization. Only 6.5% of records (n = 17) had 4AT completed. Table 1 shows the risk factors for delirium during hospitalization. Patients who developed delirium were older (80.8 v. 75.8 years, p < 0.001), more likely to have pre-existing cognitive impairment (OR = 3.97 [95% CI 2.11–7.46], p < 0.001), and more likely to reside in a nursing home prior to admission (OR = 12.32 [95% CI 2.54–59.62], p = 0.0018). The cohort of patients who developed delirium had a higher CFS score (mean 5.31 v. 3.67, p < 0.001) and higher CCI (mean 2.38 v. 1.82, p = .046) compared to patients who did not develop delirium during hospitalization. Fig 1. shows the prevalence of various co-morbid illnesses in the participants. Hypertension was the most common comorbid illness followed by chronic obstructive pulmonary disease and diabetes. None of the listed comorbidities significantly increased the odds of delirium in our patient cohort.
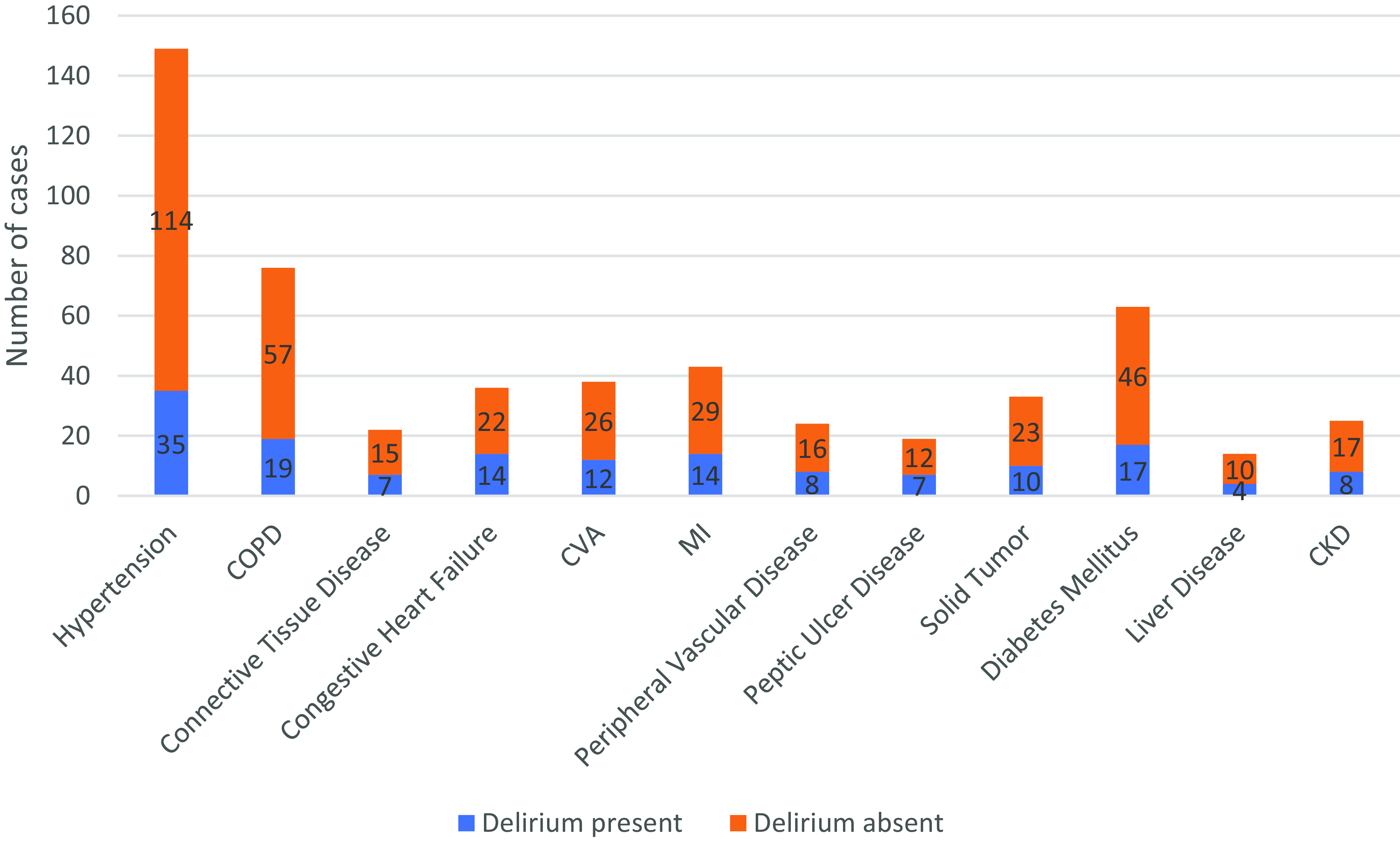
Figure 1. Bar chart showing the prevalence of comorbid illnesses in the participants.
Table 1. Characteristics and outcomes of participants with and without delirium
Outcomes
The association between delirium and in-hospital outcomes is presented in Table 1. There was no significant association between in-hospital mortality and delirium in our patient cohort (p = 0.13). However, the median length of hospital stay was significantly longer in patients who developed delirium than patients without delirium (40.5 days v. 21 days, P = 0.001). The occurrence of delirium was also significantly associated with discharge destination, as patients with delirium were more likely to be discharged to nursing homes or convalescence instead of home (OR = 8.46 [95% CI 3.60–19.88], p < 0.001).
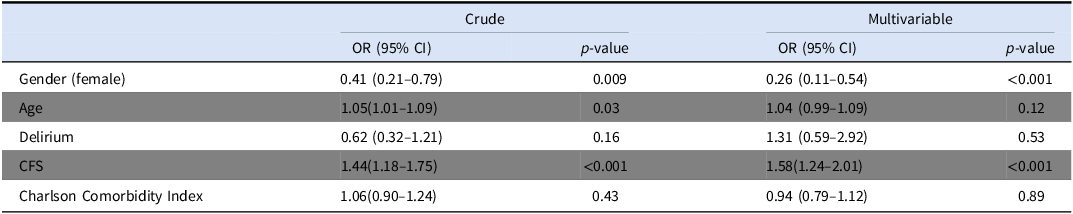
In the univariate analysis, older age (OR = 1.05, p = 0.03) and high CFS (OR = 1.42, p < 0.001) were associated with in-hospital mortality. In the multivariate analysis, only higher CFS (OR = 1.6, p < 0.001) was associated with in-hospital mortality, whereas older age was not as detailed in Table 2. Female gender was associated with decreased mortality in both univariate (OR = 0.41, p = 0.009) and multivariate analysis (OR = 0.26, p < 0.001).
Table 2. Multivariable logistic regression analyses of determinants of in hospital mortality
Discussion
Only 2.6% of the total admissions, aged 65 years or older, tested COVID-19 positive during the study period. This seems a low number considering the data collection period was at the height of the pandemic. The STTAR bioresource collected data on all inpatients with PCR confirmed COVID-19 during the study time period. This data was collected directly from the virology laboratory results over that time period. As all hospitalized patients would have had COVID-19 screening on admission and during admission, if they developed suspicious symptoms, it seems likely that the dataset included all the cases. It is difficult to explain the low number, however, the hospital introduced stringent infection control measures very early in the pandemic so outbreaks were minimized. We found a delirium prevalence of 26.8% in our study population, which is similar to the rates described in other COVID-19 studies. A meta-analysis by (Shao et al. Reference Shao, Lai, Chen, Chen, Hung and Liao2021) concluded the prevalence rate of delirium in COVID-19 patients aged >65 years was 28.2%. Our findings on the predisposing determinants of delirium partially align with those of recent studies on COVID-19 and delirium. Older adults are more likely to be frail, have a higher burden of co-morbidities, and are more likely to suffer from delirium with COVID-19 infection (Kennedy et al. Reference Kennedy, Helfand, Gou, Gartaganis, Webb and Moccia2020). Older adults are more likely to present with delirium with COVID-19 infection in the absence of respiratory symptoms, effectively disguising the underlying etiology of delirium to clinicians (Tyson et al. Reference Tyson, Shahein, Erdodi, Tyson, Tyson, Ghomi and Agarwal2022).
Frailty is described as a multidimensional health state that increases exponentially with age and is linked to adverse health outcomes in the context of COVID-19 (Gale et al. Reference Gale, Cooper and Aihie Sayer2015). Frailty is associated with increased odds of delirium and higher mortality in COVID-19 patients, which was corroborated by the results of our study (Dumitrascu et al. Reference Dumitrascu, Branje, Hladkowicz, Lalu and McIsaac2021). Frailty was the only risk factor identified in our study population associated with an increased likelihood of delirium and in-hospital mortality. Furthermore, its effect on mortality was independent of delirium occurrence.
Pre-existing cognitive impairment has consistently been shown to increase the odds of delirium in COVID-19 patients (Munawar et al. Reference Munawar, Syed, Costello, Robinson, Bergin and Greene2023). This finding was replicated in our cohort, in which patients with pre-existing cognitive impairment were four times more likely to develop delirium. A higher CCI score is associated with an increased risk of severe disease and death in COVID-19 patients (Tuty Kuswardhani et al. Reference Tuty Kuswardhani, Henrina, Pranata, Anthonius Lim, Lawrensia and Suastika2020). In our study population, a higher CCI score was associated with an increased risk of delirium but not in-hospital mortality.
The results of our study highlight that the risk factors for delirium in COVID-19 are more strongly substrate-related (frailty, cognitive impairment, higher CCI score) than the severity of illness. Patients with severe disease were more likely to require steroids and supplemental oxygen. These variables were not associated with the increased prevalence of delirium in our cohort. Steroids are known to cause neuropsychiatric problems and have been linked to increased rates of delirium in COVID-19 (Martinotti et al. Reference Martinotti, Bonanni, Barlati, Miuli, Sepede, Prestia, Trabucco, Palumbo, Massaro, Olcese, D’Ardes, Cipollone, Amore, Bondi, Russo, Carrarini, Onofrj, Sensi, Vita and Di Giannantonio2021; Woolley, Reference Woolley2021). Unlike in some studies (Pun et al. Reference Pun, Badenes, Heras La Calle, Orun, Chen and Raman2021), invasive mechanical ventilation was not associated with an increased risk of delirium in our cohort. The low rates of delirium in mechanically ventilated patients in our study may be due to the inclusion of only cases of delirium that occurred prior to receiving any muscle relaxant and sedative medications for invasive ventilation.
We postulated that patients taking medications with a cumulative anticholinergic cognitive burden≥3 as measured by the ACB scale would be more likely to suffer from delirium (Lisibach et al. Reference Lisibach, Gallucci, Benelli, Kälin, Schulthess, Beeler, Csajka and Lutters2022). However, we were unable to confirm these results. This may be partly due to the inadequate sample size. Only 21.1% (n = 55) of our cohort were on a combination of medications with an ACB score of ≥3 on admission.
Preexisting psychiatric disorders did not increase the risk of delirium in our cohort. Anxiety and depression were the most common psychiatric co-morbidities in this study population. Of the patients (n = 60) who required Psychiatry of Elderly Liaison (PsychEL) input, less than 50% (n = 27) had a comorbid psychiatric illness on admission.
Delirium was not associated with increased in-hospital mortality in our cohort. A growing body of evidence suggests that other factors such as frailty are better predictors of mortality in COVID-19 (Dumitrascu et al. Reference Dumitrascu, Branje, Hladkowicz, Lalu and McIsaac2021). In our cohort, being female was associated with decreased risk of mortality that is consistent with the current evidence that shows that men are more likely to die from COVID-19 infection (Ya’qoub et al. Reference Ya’qoub, Elgendy and Pepine2021). Our data show that delirium is associated with a significantly increased length of stay and increased likelihood of discharge to long-term care or convalescence, which signals functional decline. The implications are significant in the context of the demand for inpatient beds.
The results of our study should be interpreted in light of its strengths and limitations. The strengths include the cohort of PCR confirmed COVID-19 positive inpatients, consecutively admitted at the start of the pandemic. The electronic medical record system ensured that all patients, irrespective of their location in the hospital (ED, ICU, or general wards), were included and all medical and allied health professional documentation was available for review. This study has several limitations. First, it was a retrospective chart review, and data were collected from routine notes in the patients’ medical records, resulting in potential bias. Second, cases of delirium may be underreported, as formal delirium assessment and documentation is inconsistent. Moreover, patients who presented in a critical state may not have undergone delirium assessment. Finally, the study sample was from a single hospital and included an ethnically homogenous group (predominantly Caucasian).
Conclusion and implications
We found that over a quarter of inpatients with COVID-19 experienced delirium, resulting in prolonged admission and functional decline, requiring increased support for discharge. Alternate care pathways involving early recognition and transfer of the vulnerable group of patients to ‘delirium friendly’ wards may help improve inpatient turnover and outcomes for these patients. The effectiveness of prevention and early recognition of delirium leading to early intervention is well described. Good examples of this are the Hospital Elder Life Program (HELP) and the Recognizing Acute Delirium As part of your Routine (RADAR) program (Inouye et al. Reference Inouye, Bogardus, Charpentier, Leo-Summers, Acampora, Holford and Cooney1999; Voyer et al. Reference Voyer, Champoux, Desrosiers, Landreville, McCusker, Monette, Savoie, Richard and Carmichael2015). They have proved effective for delirium recognition and improving outcomes for hospitalized older adults (Hshieh et al. Reference Hshieh, Yang, Gartaganis, Yue and Inouye2018). The effectiveness of delirium friendly wards is less well described, but the cohorting of these vulnerable patients allows more focused non-pharmacological interventions to be provided as shown by Chong et al. Reference Chong, Chan, Tay and Ding(2014). Frail older adults with pre-existing cognitive impairment are at the highest risk of developing delirium and may benefit from care by specially trained staff with the utilization of preventive measures early in the course of illness. This can lead to substantially reduced costs for both acute and long term care services as our findings show that delirium is associated with increased length of hospital stay and greater likelihood of being discharged to a long term care facility or convalescence. Implementation of integrated care pathways for delirium prevention and intervention, while initially costly to set up from a manpower perspective, have consistently proved to be beneficial in improving healthcare quality, patient satisfaction and reducing healthcare costs.
Acknowledgements
We would like to thank the St James’s Hospital, Tallaght University Hospital, Trinity College Dublin Allied Researchers’ (STTAR) Bioresource COVID-19 team for their collaboration.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interests
The authors declare none.
Ethical standard
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The authors assert that ethical approval for publication of this study was granted by the St James Hospital and Tallaght University Hospital (SJH/TUH) Joint Research and Ethics Committee under the STTAR Bioresource for the COVID-19 project. The STTAR Bioresource study Project ID is JREC 2020-05 List 19 and further data protection impact assessment and review was performed by the SJH Research and Innovation Office (R&I no. 6949).
Description of author’s roles
N. Munawar: conceptualization, methodology, data curation, software, formal analysis, writing-original draft, project administration.
E. Mohamed: data curation, writing-review and editing.
C. Ni Cheallaigh, C. Bergin: data curation, editing.
E. Greene: conceptualization, project administration, writing-review and editing, supervision.





