Introduction
Hypertensive disorders of pregnancy (HDP) and postpartum depression (PPD) are two major public health concerns that pose significant risks to maternal and child well-being. HDPs, encompassing conditions like pre-eclampsia, gestational hypertension, and chronic hypertension, complicate up to 10% of pregnancies worldwide, with a significant impact in low- to middle-income countries (LMICs) (Abalos et al., Reference Abalos, Cuesta, Grosso, Chou and Say2013; Duley, Reference Duley2009). They are particularly dangerous in LMICs, contributing substantially to maternal mortality (Say et al., Reference Say, Chou, Gemmill, Tunçalp, Moller and Daniels2014).
These conditions are characterized by high blood pressure and often involve issues with the blood vessels throughout the body. This can result in adverse effects such as damage to the mothers’ organs, complications during birth, and stunted foetal growth. The combination of experiencing a life-threatening complication and its management may culminate in psychological trauma.
Despite global efforts, complications from HDP remain a major public health issue, especially in LMICs like Ghana. The incidence of HDP has increased globally, from 16.30 million cases in 1990 to 18.08 million in 2019, highlighting the growing concern (Wang et al., Reference Wang, Xie, Yuan, Wang, Zhao and Zhou2021). In Ghana, the maternal mortality ratio remains high at 263 per 100,000 live births, with HDPs cited as the second leading cause after postpartum haemorrhage, HDPs are a significant cause of maternal mortality, accounting for 30.0 to 31.7% of maternal deaths in Ghanaian tertiary hospitals (Adu-Bonsaffoh et al., Reference Adu-Bonsaffoh, Oppong, Binlinla and Obed2013). These disorders also lead to severe perinatal outcomes, including stillbirth, early neonatal death, and low birth weight.
Perinatal mental health (PMH) disorders occur during pregnancy and postpartum, impacting maternal well-being and family dynamics. These include postpartum blues, depression, psychosis, and anxiety disorders (COPE., 2017; Cook et al., Reference Cook2023). Globally, PMH problems pose a significant public health challenge. Approximately 10% of pregnant women and 13% of postpartum women encounter a mental disorder, primarily depression (WHO., 2019). In developing countries, these rates are even higher, reaching 15.6% during pregnancy and 19.8% after childbirth (Miafo et al., Reference Miafo, Woks, Nzebou, Tchaptchet, Delene, Tchidje, Ndzodo, Siewe Kamga and Assumpta2023). In severe instances, mothers may experience such intense suffering that it could lead to suicidal tendencies. Moreover, affected mothers may struggle to function adequately, potentially impacting the growth and development of their children negatively. It is essential to note that maternal mental disorders are treatable, and effective interventions can be administered by well-trained non-specialist health providers.
While the physiological and medical aspects of HDP have been extensively studied, there is growing recognition of the potential impact of these disorders on maternal mental health. Pregnancy itself is a period of significant physiological and psychological changes, and the presence of a medical complication like hypertensive disorders could potentially exacerbate stress and anxiety levels among pregnant women. While evidence indicates the potential development of major depressive disorders during the perinatal period, mental illness during this time is frequently underestimated, overlooked in assessments, undiagnosed, and consequently left untreated (Apter et al., Reference Apter, Devouche and Gratier2011).
PPD usually begins within a few weeks of childbirth, but symptoms can emerge up to a year later as well (Nakić Radoš et al., Reference Nakić Radoš, Kömürcü Akik, Žutić, Rodriguez-Muñoz, Uriko and Motrico2024). PPD is common, affecting 10%–20% of new mothers globally, with reported prevalence ranging from 4% to 36% in Ghana (Noonan et al., Reference Noonan, Jomeen, Galvin and Doody2018).
The exact causes of PPD are still being researched but are believed to involve a combination of hormonal factors, genetics, physiological stress from childbirth, and environmental/social triggers. Research conducted by Beck, Reference Beck2006 suggests that a substantial portion of new mothers experiencing PPD go undiagnosed. Left untreated, PPD can adversely impact maternal-infant bonding and child development. Fortunately, there are effective treatments for PPD. Many women benefit from a combination of antidepressant medication and psychotherapy approaches like cognitive behavioural therapy or interpersonal counselling (Milgrom et al., Reference Milgrom, Gemmill, Ericksen, Burrows, Buist and Reece2015). With various treatment options available, the prognosis for women with postpartum depression is generally good.
Understanding the potential associations between hypertensive pregnancy disorders and perinatal mental health is crucial for several reasons. Unfortunately, the exact nature and extent of these associations, and their subsequent impact on postnatal psychological health in LMICs, have not been comprehensively explored, resulting in an evidence gap that hinders the provision of appropriate care for these women. While some individual studies have hinted at potential connections between HDP and maternal mental health in LMICs, a systematic literature review is warranted to provide a comprehensive and evidence-based understanding of these associations. Given the potential effects on the health of the mother, the unborn child, and the entire family, establishing a connection between HDP and negative mental health outcomes for mothers could significantly impact how healthcare professionals manage and care for pregnant individuals.
Most studies examining the relationship between HDPs and PPD have been conducted in high-income countries, leaving a gap in evidence from sub-Saharan Africa, particularly Ghana. Although some studies have assessed the prevalence of PPD in Ghana, no research has specifically investigated the connection between HDP and PPD, underscoring the need for more focused research. To address this gap, the present study conducted a systematic review and meta-analysis to determine the association between HDP and PPD in LMICs. Furthermore, semi-structured qualitative interviews were conducted with Ghanaian healthcare professionals to gain insights into their perspectives and experiences regarding this association within the local context.
By identifying and addressing these links, healthcare professionals can develop interventions and support systems, especially for women in LMICs who are at risk of developing HDP. This, in turn, will contribute to improved pregnancy outcomes. The insights provided in this review can serve as a resource for healthcare professionals, researchers, and policymakers looking to guide future healthcare strategies and develop targeted interventions that address the psychological needs of pregnant individuals dealing with HDP, as well as mothers of newborns, to enhance maternal well-being during the perinatal period in Ghana.
Methods
First, this study used systematic literature and Meta-analysis tools to generate research hypotheses. Then qualitative interviews were conducted to confirm the logical associations between HDP and PPD. It was aimed to provide a holistic understanding of the relationship between HDP and PPD, particularly within the unique sociocultural context of Ghana. The pluralistic approach offered new perspectives and triangulated insights into this critical maternal health issue.
A systematic review was performed based on a pre-established protocol (S1 Text. Protocol), adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist (S2 Text. PRISMA Checklist). The protocol was registered with PROSPERO under reference number CRD42023464675 and is accessible at https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023464675 . Selected studies underwent systematic data collection, encompassing study characteristics, participant demographics, and outcome measures pertaining to HDP and PPD. The methodological quality of these studies was evaluated to uphold the reliability and validity of results. Data synthesis consolidated findings, identifying key patterns across studies.
In this meta-analysis, a random effects model is the primary statistical methodology. The analysis utilized the odds ratio as the outcome measure. The Q-test for heterogeneity (Cochran, Reference Cochran1954) and the
![]() ${I^2}$
statistic (Higgins & Thompson, Reference Higgins and Thompson2002) were reported to assess variability. Studentized residuals and Cook’s distances were used to identify potential outliers and influential studies within the model. Funnel plots were employed to detect biases, with visual inspections for asymmetry and consideration of p-values. The analysis was performed using R (version 4.3.1) (R Core Team, 2020) and the Metafor package (version 4.2.0) due to their robustness and computational efficiency (Viechtbauer, Reference Viechtbauer2010).
${I^2}$
statistic (Higgins & Thompson, Reference Higgins and Thompson2002) were reported to assess variability. Studentized residuals and Cook’s distances were used to identify potential outliers and influential studies within the model. Funnel plots were employed to detect biases, with visual inspections for asymmetry and consideration of p-values. The analysis was performed using R (version 4.3.1) (R Core Team, 2020) and the Metafor package (version 4.2.0) due to their robustness and computational efficiency (Viechtbauer, Reference Viechtbauer2010).
The qualitative study was conducted at the University of Ghana Medical Centre LTD (UGMC), a leading medical and research institution in Ghana and West Africa. UGMC was chosen for its prominence in advancing clinical practice and research. Semi-structured interviews were used to gather focused yet flexible insights from frontline maternal health experts at UGMC, aiming to understand the relationship between hypertensive disorders and postpartum depression. After obtaining ethical clearance from the UGMC institutional review board, ten participants (five female medical doctors and five midwives) with a minimum of five years of experience in maternal healthcare were interviewed to ensure data saturation and a comprehensive understanding of the research questions. The all-female participant group was chosen to foster a comfortable environment for discussing sensitive maternal health issues. Participants were provided with detailed information about the study and consent forms prior to scheduling interviews via Microsoft Teams. The interviews, lasting 20–30 minutes, were recorded and transcribed verbatim. The semi-structured format allowed for gathering targeted information while enabling participants to share their observations and perspectives on hypertension, depression, and maternal health. Braun and Clarke’s six-step thematic analysis method was employed to analyse the data (Braun & Clarke, Reference Braun and Clarke2021). This approach aimed to provide a thorough understanding of the complex health issues affecting Ghanaian mothers.
Inclusion and exclusion criteria
The review focused on articles that included women residing in LMICs who either have experienced HDPs or are currently dealing with the aftermath of such conditions. Included articles were peer-reviewed original articles with abstracts in English. However, conference presentations, opinion articles, books, and dissertations are excluded. Non-English studies, studies conducted on animals, incomplete studies where required data is inaccessible/unavailable, studies without primary data, and studies that were not conducted in LMICs were excluded. No limitations were placed on the years of publication.
Outcome variables
The outcomes of this review focused on studies that assessed postpartum depression among women with HDP. To evaluate postpartum depression, the Edinburgh Postnatal Depression Scale (EPDS) was employed. The EPDS is a widely recognized and validated screening tool specifically designed to identify depressive symptoms in the postpartum period.
This allowed for a robust examination of the psychological impact of HDP on postpartum women. By using this standardized tool, the study ensured the reliability and comparability of the findings with existing research. This approach not only facilitated a detailed analysis of the prevalence and severity of postpartum depression but also contributed to the broader understanding of maternal mental health in the context of hypertensive disorders during pregnancy.
Search strategy and study selection
The following key databases and register were meticulously explored from inception to August 19, 2023: Academic Search Elite (ASE), APA PsycINFO, CINAHL, Cochrane Central Register of Controlled Trials (CRCT), Cochrane Database of Systematic Reviews (CDSR), Embase, Maternity and Infant Care Database (MICD), MEDLINE, PubMed, and Scopus. All searches were conducted using the same search techniques, with unique modifications made to each database’s requirements. All databases were subject to restrictions, which included only studies published in English. However, certain databases also had additional filters, as shown in Table 1, such as peer review status, subjects related to humans, women, and pregnancy, among others. Screening of the reference list of included articles for the likelihood of relevant articles was conducted.
Table 1. Summary of Databases Used in the Review
CINAHL: Cumulated Index to Nursing and Allied Health Literature, MEDLINE: Medical Literature Analysis and Retrieval System Online, APA: American Psychological Association, ASE: Academic Search Elite, MICD: Maternal and Infant Care Database, CCRCT: Cochrane Central Register of Controlled Trials, CDSR: Cochrane Database of Systematic Reviews.
The details of the search in specific databases are given in this study (S3 Text. Search Strategy). The databases were initially searched without applying any filters. After reviewing the initial hits, filters were applied to align the results with the study objectives. The cumulative outcome of these searches, totalling 1444 results, was then exported to RefWorks referencing software manager.
Duplicates within the reference collection, identified by identical titles, authors, and publication years from the same journal, were subjected to a de-duplication process. This process utilized Digital Object Identifier (DOI), International Standard Book Number (ISBN), and International Standard Serial Number (ISSN) to ensure thorough identification and removal of redundant entries. Upon completing the de-duplication process, 17 redundant articles were successfully eliminated, resulting in 1427 articles remaining for screening.
Title and abstract screening were conducted using the RefWorks referencing software manager. The initial screening of titles and abstracts of all articles was performed by the first reviewer (KMA). To ensure comprehensive coverage, a random 10% of all references were reviewed by the second reviewer (HK). KMA and HK independently screened the full texts, resolving any discrepancies through discussion and input from the third reviewer (MO).
The most suitable data were selected from multiple studies within the same dataset. From the initial search, 44 studies were identified as potentially relevant based on research questions and the Population, Exposure and Outcome (PEO) criteria. However, full-text access could not be obtained for 9 of these studies, resulting in 35 studies being available for comprehensive full-text review. These studies were then rigorously assessed against the established inclusion criteria.
The review aimed to include studies exploring the impact of HDP on perinatal mental health (PMH) in LMICs. Suitable study designs included Cross-Sectional studies, Cohort studies, and Case-Control studies. Exclusion criteria ruled out non-English studies, animal studies, review articles, opinion pieces, case reports, incomplete studies, and studies outside LMICs or lacking primary data.
After a thorough review of the 35 full-text articles, 5 studies were selected for critical appraisal. Exclusions were primarily due to the studies not being conducted within LMICs or their reported outcomes not aligning with the specific variables under investigation. Additionally, two studies were omitted because of concerns about the suitability of their research designs.
The meta-analysis expanded on the systematic review, maintaining the same search strategy, screening and selection methods, and critical appraisal process. Two studies were excluded from the review - one by Abedian et al. (2015) and another by Mbarak et al. (Reference Mbarak, Kilewo and Kuganda2019) - due to the absence of dichotomous data. These studies lacked a control group, preventing direct comparisons and the extraction of necessary binary data for statistical analyses. A rigorous evaluation was conducted to ensure the integrity and relevance of the selected articles. A PRISMA flow diagram (Fig 1) is included to detail the study selection decisions.
Figure 1. PRISMA flow diagram.
Critical appraisal
A rigorous quality assessment was conducted using the Joanna Briggs Institute (JBI) critical appraisal checklist, tailored to the specific study designs under consideration (S4 Text. Cohort, S5 Text. Cross Sectional & S6 Text. Case Control). Each item in the checklist was scored numerically: ‘Yes’ received 1 point, ‘No’ received 0 points, and ‘Unclear’ or ‘Not applicable’ also received 0 points. The total score varied by study type, with 11 points for cohort studies, 10 for case-control studies, and 8 for cross-sectional studies. The selected studies were graded as poor, moderate, or good based on the critical appraisal scale presented in Table 2.
Table 2. Critical Appraisal Scale
Upon evaluation, four out of five studies received a good-quality rating, indicating strong methodological rigor. One study received a moderate-quality rating. The limitations observed were primarily related to addressing confounding factors and the statistical tools used. Specifically, four studies lacked documented strategies for mitigating the influence of potential confounders. In one study, there was uncertainty about whether participants were free of the outcome variable at the start. Although data collection began at the study’s inception, there was no clear mention of participants’ baseline status regarding the outcome variable. Despite these limitations, all five studies were included in the subsequent data extraction phase of the review process as detailed in Table 3.
Table 3. Grading of Selected Studies
Data extraction
Systematic review
The extraction of data was conducted simultaneously with full-text searching. The relevant information was extracted from each article included and recorded immediately in the data extraction file (S7 Text. Extracted Data). Five studies were identified for data extraction under the following key categories: study details: authors, publication, year, population characteristics: study design, setting, duration and follow-up, type of recruitment, sample size, inclusion criteria, exclusion criteria, independent variable: exposed variable, measurement of the exposed variable, dependent variable: outcome variable, measurement of the outcome variable, statistical techniques, results, and limitations.
Meta-analysis
Three studies were identified for data extraction, focusing on key variables including the author, year, and categories denoted as ‘a’, ‘b’, ‘c’, ‘d’, ‘n1’, and ‘n2’. These variables were defined as follows: ‘a’ represented the count of individuals with HDP who experienced PPD, ‘b’ represented the count of individuals with HDP who did not experience PPD, ‘c’ represented the count of individuals without HDP who experienced PPD, and ‘d’ represented the count of individuals without HDP who did not experience PPD. ‘n1’ and ‘n2’ indicated the total number of study participants with and without HDP, respectively. The data was manually extracted and recorded in Table 4.
Table 4. Extracted Data for Meta-Analysis
a: Count of individuals with HDP who experienced PPD; b: Count of individuals with HDP who did not experience PPD; c: Count of individuals without HDP who experienced PPD; d: Count of individuals without HDP who did not experience PPD; n1: Total number of study participants with HDP; n2: Total number of study participants without HDP.
Results
Systematic review
The studies reviewed were authored by Abedian et al, 2015; Chen et al, Reference Chen, Wang, Ding, Shan and Qi2019; Sarosh et al, 2022; Strapasson et al, Reference Strapasson, Ferreira and Ramos2018 and Mbarak et al, Reference Mbarak, Kilewo and Kuganda2019. Abedian and his colleagues conducted their study in Iran, employing a cohort design with specific inclusion criteria including women aged at least 18 years, gestational age of ≥ 36 weeks, and diagnosed with preeclampsia. Exclusion criteria covered various medical conditions and mental health history. They conducted their research in a hospital setting from June 2012 to November 2012 and again from June 2013 to October 2013. Convenience sampling was used, resulting in a sample size of 122 participants. Their study found significant differences in depression, state anxiety, and trait anxiety scores between admission and six weeks postpartum. While preeclampsia was not significantly associated with depression, state anxiety, or trait anxiety, it was identified as a potential risk factor for PPD, with a higher incidence in preeclamptic women. The changes in depression and anxiety over time were independent of the severity of preeclampsia. Statistically, depression (F = 3.8, p < 0.001), state anxiety (F = 1.52, p < 0.001), and trait anxiety (F = 1.5, p < 0.001) showed significant changes from admission to postpartum, with no significant interaction between time and preeclampsia severity for depression, state anxiety, and trait anxiety.
Chen’s research team carried out their retrospective study in China. They included individuals diagnosed with preeclampsia based on American College of Obstetricians and Gynaecologists (ACOG) guidelines, with ages between 20 and 40 years and gestational age of at least 28 weeks. Obstetric complications other than preeclampsia and certain medical histories were adopted as the exclusion criteria. The study spanned from January 1, 2017, to August 30, 2018, in a hospital setting, with a recruitment procedure that combines two methods. Although controls were assigned randomly, the method employed for recruiting cases was not explicitly specified. The researchers likely employed either convenience or purposive sampling methods for case recruitment. Their study included a sample size of 180 participants, evenly divided between those with preeclampsia (90 individuals) and those without the condition (90 individuals). This study reported no significant association between preeclampsia severity and state anxiety, trait anxiety, or depression. However, there was a higher incidence of PPD among women with preeclampsia compared to those without, making preeclampsia a significant risk factor for PPD, especially with severe preeclampsia increasing the risk further. The EPDS scores were significantly higher in preeclamptic women. Statistically, preeclampsia significantly increased the odds of PPD (AOR = 2.753, 95% CI: 1.056–7.178), with severe preeclampsia further elevating the risk (AOR = 4.540, 95% CI: 1.194–17.255).
Sarosh and colleagues conducted a cross-sectional study in Pakistan. They included women with varying degrees of hypertensive disorders in pregnancy and a control group of women without such disorders. Participants delivered after 28 weeks of gestation, either by caesarean section or vaginal delivery, and had living infants at the time of the study. Exclusion criteria involved psychiatric illnesses and other specific conditions. The study occurred between June 2020 and December 2021, and participants were followed in a postpartum clinic around six weeks after delivery. The recruitment procedure was unclear, with a combined sample of 220 participants (110 with hypertensive disorders and 110 with normal pregnant controls). The research team observed a higher incidence of PPD among women with preeclampsia, with the risk of PPD increasing with the severity of preeclampsia. The prevalence of PPD was 27% among women with hypertensive disorders, compared to 13% in normotensive women. Higher incidence rates of PPD were found in subgroups such as gestational hypertension, preeclampsia, pregnancy-induced hypertension (PIH) with superimposed preeclampsia, and eclampsia. Statistically, there was a significant association between hypertensive disorders and PPD (30/45 vs. 80/175, p = 0.015).
Strapasson’s research team conducted a prospective descriptive cross-sectional study in Brazil. They included women who had recently delivered, either with or without hypertensive disorders of pregnancy (HDP). Women with HDP were further categorized based on disease severity. Exclusion criteria included maternal age younger than 18 years, foetal malformation, foetal death, and psychiatric disease. The study took place from January 15, 2015, to January 15, 2017, in a hospital setting. The recruitment procedure used convenience sampling, with samples matched by pregnancy duration. The study involved 160 women (40 with preeclampsia and 120 without). The team found a higher prevalence of depressive symptoms in women with hypertensive disorders during pregnancy (HDP). Depressive symptoms correlated with factors such as parity, spontaneous abortions, and diastolic blood pressure, and there were higher NICU admission rates for newborns of women with depressive symptoms. Statistically, there were significant correlations between HDP and postpartum depressive symptoms (rs = 0.219, p = 0.004).
Mbarak and colleagues conducted a cross-sectional study in Tanzania, but detailed inclusion and exclusion criteria were not provided. The study occurred from July 2016 to January 2017 in a hospital setting. Convenience sampling was used, resulting in a sample of 386 participants. This team found a 20.5% prevalence of PPD in their study cohort, with higher rates among women with eclampsia and severe preeclampsia. Significant predictors of PPD included younger age, single status, lower education, perinatal death, lack of family support, and stressful events during pregnancy. Statistically, significant predictors of PPD included age (AOR 10.19 for < 20 years), single status (AOR 3.18), lower education (AOR 3.83), perinatal death (AOR 5.14), lack of family support (AOR 7.06), and stressful events during pregnancy (AOR 15.14).
Overall, the studies highlighted a consistent finding: preeclampsia and other hypertensive disorders during pregnancy are significant risk factors for postpartum depression. While the severity of preeclampsia did not always correlate directly with anxiety or depression scores, severe preeclampsia consistently showed a higher risk for PPD. The presence of preeclampsia significantly increased the odds of PPD, and this risk was further elevated in cases of severe preeclampsia. Additionally, factors such as age, marital status, education level, perinatal death, lack of family support, and stress during pregnancy emerged as important predictors of PPD.
Meta-analysis
According to the Q-test, there was no significant amount of heterogeneity in the true outcomes
![]() $Q\left( 2 \right)=0.0746,\;p=0.9634,\;{I^2}=0.0000\%, \;{\hat \tau ^2}=0.0000)$
. The estimated average log odds ratio (pooled estimate) based on the random effects model was 0.8757 (95%, CI: 0.4467 to 1.3047, SE=0.2189). Therefore, the average outcome differed significantly from zero (
$Q\left( 2 \right)=0.0746,\;p=0.9634,\;{I^2}=0.0000\%, \;{\hat \tau ^2}=0.0000)$
. The estimated average log odds ratio (pooled estimate) based on the random effects model was 0.8757 (95%, CI: 0.4467 to 1.3047, SE=0.2189). Therefore, the average outcome differed significantly from zero (
![]() $z=4.0010,\;p \lt 0.0001)$
(See Fig 2).
$z=4.0010,\;p \lt 0.0001)$
(See Fig 2).
Figure 2. Results of the Random-Effects Model Legend: The Random-Effects Model, comprising three studies (k=3), revealed an estimated
![]() $\;\;{\hat \tau ^2}$
of 0 using Restricted Maximum Likelihood (REML) method, a total heterogeneity/total variability (I2) of 0.00% and a total variability/sampling variability (H²) of 1.00. The test for heterogeneity (Q = 0.0746, with two degrees of freedom) yielded a p-value of 0.9634. The estimated effect size was 0.8757, with a standard error (SE) of 0.2189, resulting in a z-value of 4.0010 and a p-value < 0.0001. The 95% confidence interval (CI) ranged from 0.4467 to 1.3047.
$\;\;{\hat \tau ^2}$
of 0 using Restricted Maximum Likelihood (REML) method, a total heterogeneity/total variability (I2) of 0.00% and a total variability/sampling variability (H²) of 1.00. The test for heterogeneity (Q = 0.0746, with two degrees of freedom) yielded a p-value of 0.9634. The estimated effect size was 0.8757, with a standard error (SE) of 0.2189, resulting in a z-value of 4.0010 and a p-value < 0.0001. The 95% confidence interval (CI) ranged from 0.4467 to 1.3047.
An evaluation of the studentized residuals indicated that none of the studies exhibited a value exceeding ±2.3940, signifying the absence of outliers within the framework of this model. Similarly, based on the Cook’s distances, none of the studies appeared to exert excessive influence (see Fig 3).
Figure 3. Studentized Residuals and Cook’s Distances Legend: rstudent: Studentized Residuals, cook.d: Cook’s Distances.
The individual weights assigned to the included studies were determined to be 30%, 39%, and 31% for the studies conducted by Chen et al., Reference Chen, Wang, Ding, Shan and Qi2019, Sarosh et al., 2024, and Strapasson et al., Reference Strapasson, Ferreira and Ramos2018 respectively (see Fig 4). These weights signify the relative contributions of each study to the overall analysis, with higher weights indicating greater influence on the estimated effect size. The odds ratios from each study indicated estimated effect sizes of 2.61, 2.38, and 2.24, respectively, highlighting the magnitude of the association between HDP and PPD. The p-values for the studies by Chen et al., Reference Chen, Wang, Ding, Shan and Qi2019, Sarosh et al., 2024, and Strapasson et al., Reference Strapasson, Ferreira and Ramos2018 were 0.0165, 0.0137, and 0.0391, respectively.
Figure 4. Individual Contribution of Each Study in the Analysis.
Additionally, the observed log odds ratios, depicted in Figure 5, ranged from 0.81 to 0.96. All estimates were positive, indicating a consistent positive association between HDP and PPD across the studies analysed.
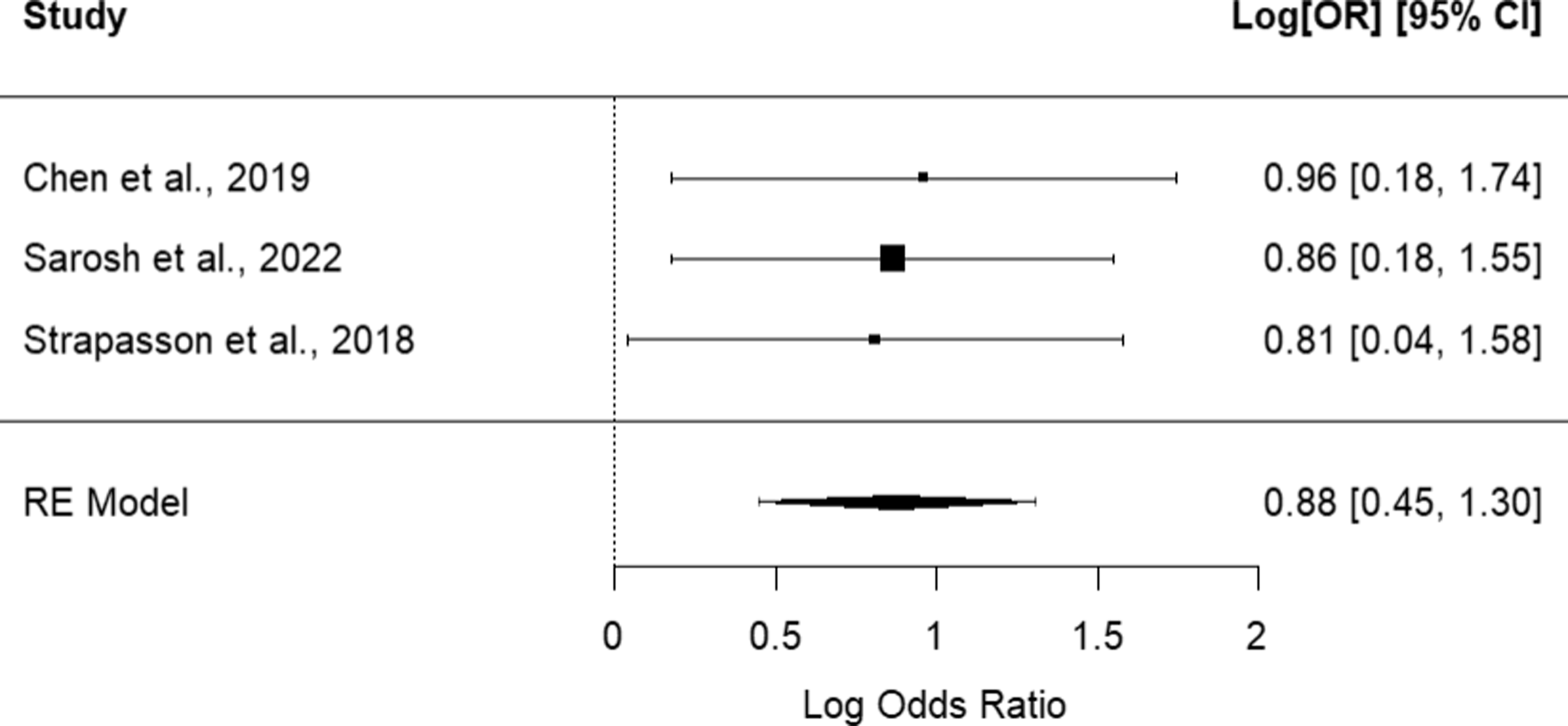
Figure 5. Log Odds Ratio of the Random-Effects (RE) Model.
Overall, the analysis yielded a predicted pooled effect size of 2.40, with a 95% confidence interval ranging from 1.56 to 3.69 and the corresponding p-value of 0.00006 highlights the statistical significance of this association (See Summary section of Fig 4). This effect size indicates a strong and positive association between HDP and PPD across the studies included in the analysis.
A cumulative meta-analysis was performed for different models and measures to understand how the available evidence evolved over time, assess the robustness of the findings, and detect potential biases. Findings from a range of studies consistently confirmed a significant association between HDP and PPD. The cumulative meta-analysis, as presented in Fig 6 demonstrated a trend towards consistent findings across studies, indicating a robust effect of the intervention under investigation. The evidence presented suggested a trend of consistency, with findings strengthening over time. Across different models and measures, the studies consistently showed similar trends and estimates, indicating robustness in the evidence. Specifically, as newer studies, such as Sarosh et al., 2022 were included, the estimates remained largely in line with those from earlier studies, like Strapasson et al., Reference Strapasson, Ferreira and Ramos2018, albeit with potentially more precise estimates and lower p-values, indicating increasing confidence in the results. This suggests a progressive accumulation and refinement of evidence over time, contributing to a clearer understanding of the phenomenon under investigation. The consistent findings across studies underscore the reliability of the observed effects.
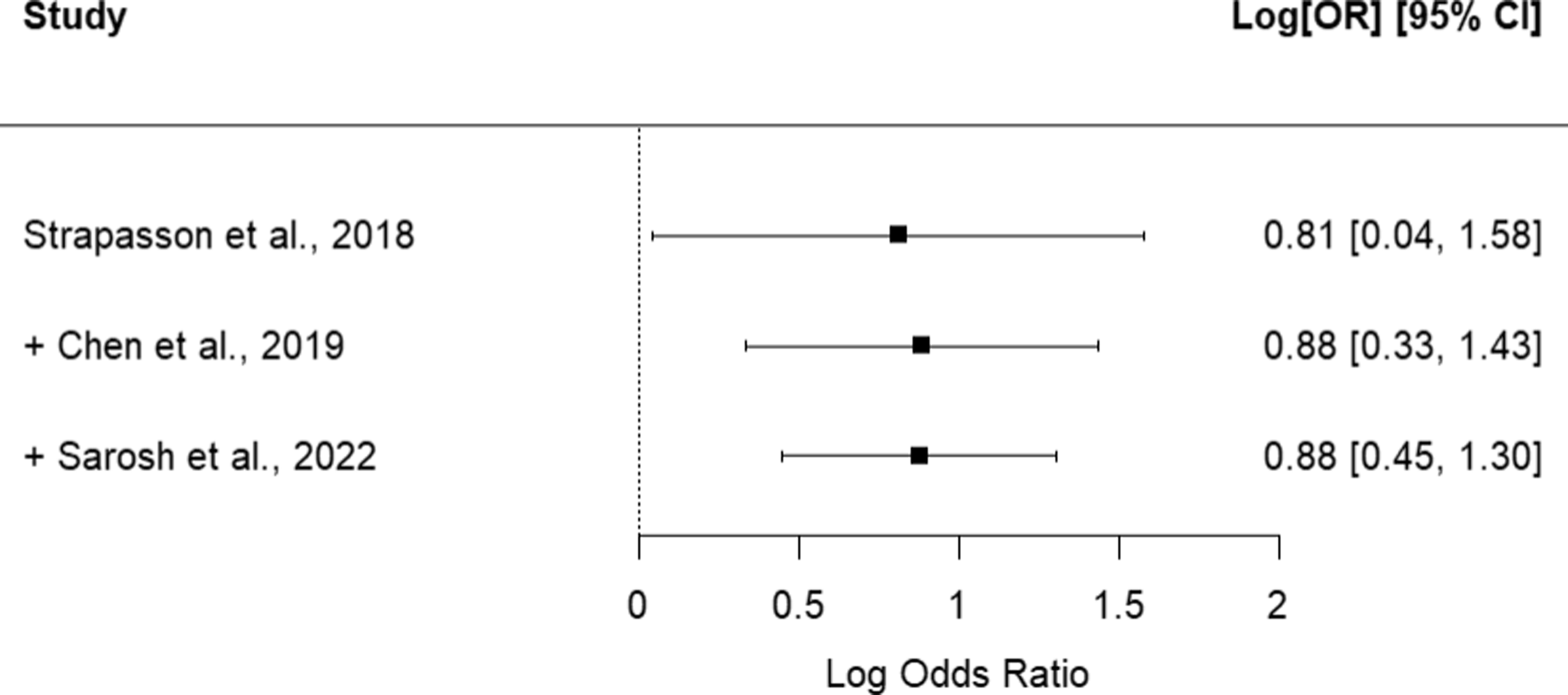
Figure 6. Cumulative Meta-Analysis of the Selected Studies.
Funnel plot asymmetry was examined using the rank correlation test and the regression test using the standard error of the observed outcomes as a predictor across different models and measures. Despite differences in the models, the p-values remained remarkably consistent. Both the rank correlation and regression tests consistently failed to detect any significant asymmetry in the funnel plot. The high p-values (1.000 for the rank correlation test and 0.9369 for the regression test) exceeded the 0.05 threshold, indicating no substantial evidence of publication bias across the models or effect measures examined.
Upon visual examination of the plots, a symmetrical pattern is evident, with points evenly dispersed around the central line, as illustrated in Fig 7. The associated p-values are significant for all the studies, as shown in Fig 8. This absence of unevenness in the distribution of points indicates no apparent publication bias in the study. The consistent lack of indications of publication bias across a range of models and effect measures enhances the overall reliability of the meta-analysis findings.
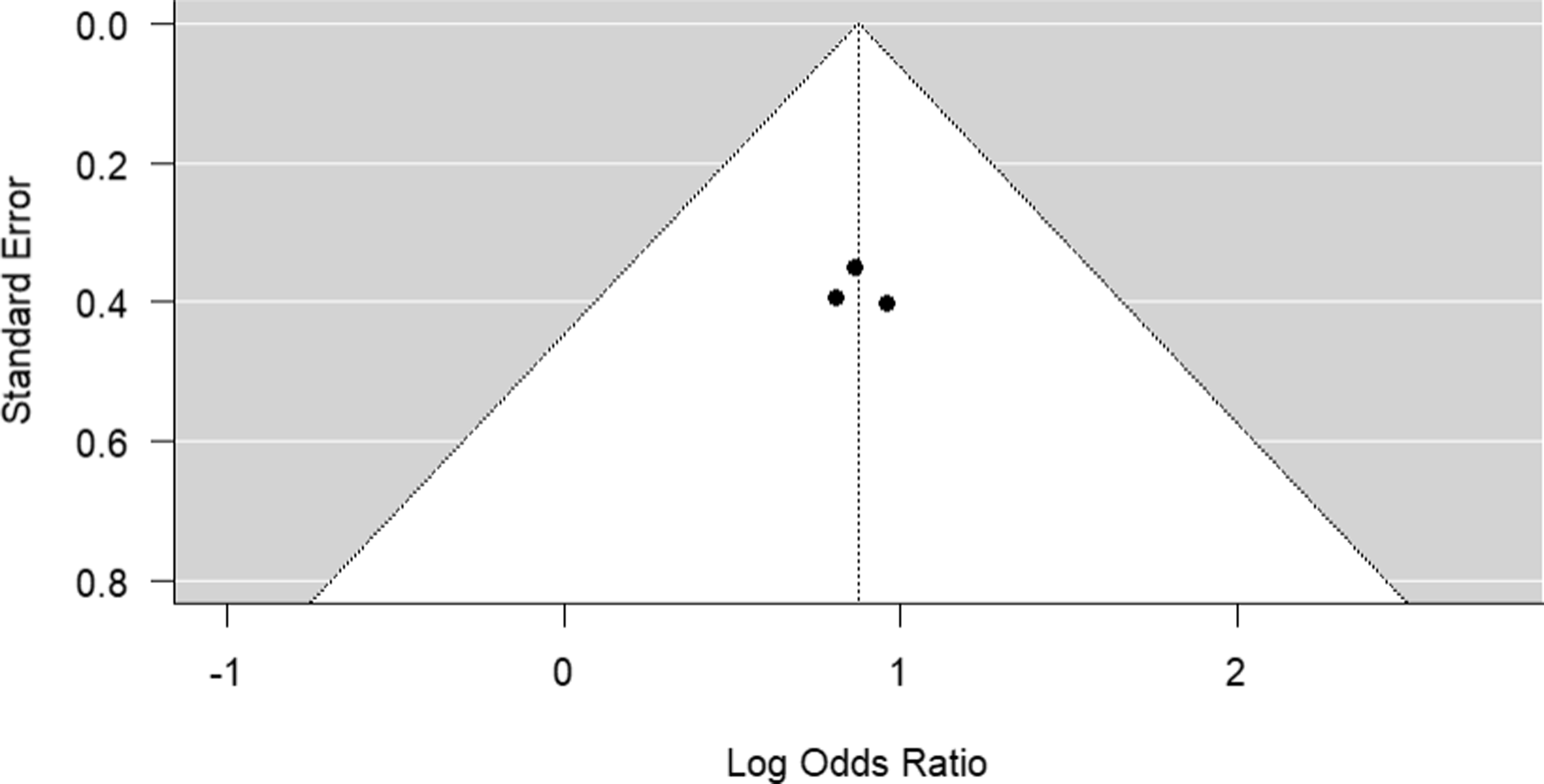
Figure 7. Test of Publication Bias using a Funnel Plot.
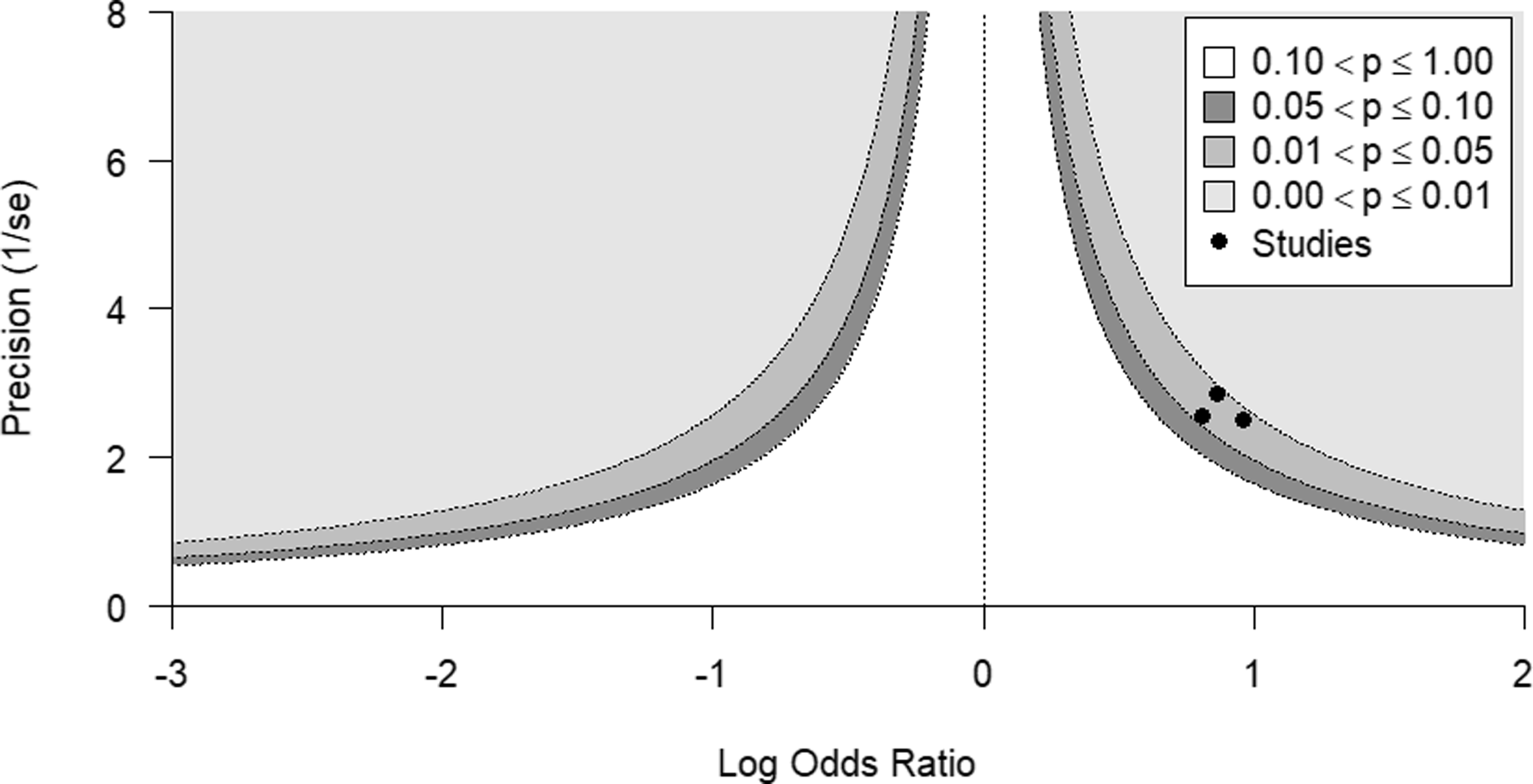
Figure 8. Publication Bias using Contour-Enhanced Funnel Plot.
Semi-structured interviews
The participants in the study included doctors and midwives who have worked with pregnant women across various regions, providing a comprehensive and varied perspective (see Table 5). The interviews involved healthcare professionals of diverse ranks and years of practice, collectively covering extensive experience across 75% of Ghana’s regions. This geographical diversity strengthened the external validity of the qualitative findings, ensuring that the experiences and insights reflected the diverse contexts within the country.
Table 5. Participants’ Ranks, Years of Experience, and Regions of Practice

Key findings from the interviews illuminated the intricate association between HDP and PPD. The frequency of HDP cases observed by healthcare providers varied, with estimates ranging from 5 to 100 cases per month. Healthcare professionals reported a substantial number of hypertensive pregnancies, emphasizing the critical health priority that HDP represents in pregnancy.
‘Maybe 100 per month. It is quite a lot.’- Participant D1
‘That should be about 20 a month.’- Participant M4
‘I will say, my facility where I work, about 15 women’ – Participant M5
‘Between 5 to 10 per month.’-Participant D3
The prevalence of PPD was varied, with estimates ranging from 2% to 5%.
‘Maybe 2%.’ - Participant M1
‘I will keep it at 5%. It’s not much that I have come of across.- Participant M5
‘I will say like 3%.’ – Participant M3
They highlighted a co-occurrence of PPD among HDP patients, with estimates ranging from 2% to 50%. More severe variants of HDP, such as severe preeclampsia and eclampsia, were associated with the highest likelihood of experiencing PPD.
‘About 50%.’ - Participant M4
‘About 30% of hypertensive patients also have postpartum depression.’ – Participant D3
‘Maybe about half of them. About 50%.’ – Participant D1
‘Between 25 to 30%.’- Participant D4
Healthcare providers reported varying trends in the frequency of HDP and PPD. While some observed stability or a decline, others identified an increase, reflecting differences in their awareness of these trends.
‘I will think it is increasing more likely to the fact that ourare now keener on maternal mental health.’- Participant D5
‘I think it is rather decreasing because those I have encountered.’ – Participant M2
‘I will go for remaining stable.’ – Participant M5
‘Well, I think it’s increasing. Depression and mental health, in general, are areas of health that have really been neglected. For most of the women I cared for, the few I encountered with such issues, follow-up care was very poor. After discharge, they return to their communities and often do not come back. We also fail to follow up because we don’t really see depression or mental health as a serious health challenge. People are developing mental health conditions, but we tend to trivialize them. As a result, we haven’t put measures in place to follow up on these issues. Since we are not following up, we are not collecting data on them. I feel mental health issues are increasing, but because we have trivialized them, there isn’t data to support this increase.’ - Participant M3
Factors contributing to these trends included increased awareness of maternal mental health issues, stress and the socio-economic status of patients.
‘Increasing awareness of maternal mental health issues contributes to rising rates.’- Participant D5
‘Mainly due to stress among patients with varying reasons, whether it is in life events or due to being hypertensive and its related health issues and the strain it puts on them financially, emotionally, physically.’- Participant D4
‘The common thing I have noticed with such women is mostly with their socio-economic background. I worked in a rural area, where most of the women were farmers, helping their husbands on the farms. Many of them came in during the intrapartum period with limited resources. Some couldn’t afford the items needed for delivery, and some even struggled to pay for transportation to access antenatal services. A lot of them were not prepared for delivery due to financial constraints. I often noticed that some women were defaulters, coming to collect their cards but never returning for follow-up care. When asked why, they reported they couldn’t afford transportation to the facility. ‘ - Participant M3
Notably, the association between HDP and PPD was recognized by healthcare providers, who observed that women with HDP were predisposed to PPD due to factors such as preterm delivery and stress.
‘Most of these women deliver babies prematurely, or even lose their babies, so most of them do go into some form of depression postpartum.’- Participant D1
‘Yes, because women who are hypertensive are predisposed to issues like preterm delivery or surgical delivery.’- Participant D4
‘Hypertensive disorders generally put patients at risk of more extensive investigations and care procedures during the antenatal period which tends to put a lot of stress on them that can trigger depression post-delivery’- Participant D3
‘ Most of the women that suffer postpartum depression with hypertension are mostly those who already have a pre-existing emotional imbalance in terms of maybe they are having issues at home.’ - Participant M4
‘The intrapartum period is also critical. If a midwife providing care during labour is not compassionate or mishandles a woman, it affects her mental health. Certain procedures can be traumatic. I have had an experience where a woman suffered a tear during delivery and later shared that she could never forget the event. She remembered the midwife telling her that she had made the delivery difficult, so she would be sutured without anaesthesia.
If we make the intrapartum period stressful or punitive, it can have lasting consequences. Imagine a woman newly diagnosed with hypertension going through labour, then receiving sutures without anaesthesia. The postpartum period becomes mentally torturous—she keeps thinking about these events, and it can lead to depression.
So, I would say that events throughout pregnancy can significantly impact the development of depression following hypertensive disorders in pregnancy ‘ – Participant M3
The interviews revealed that most healthcare professionals relied on clinical judgment rather than standardized screening tools for diagnosing and managing PPD in HDP patients. However, some participants mentioned using the Patient Health Questionnaire 9 (PHQ-9) and the Mental Health Assessment Scale.
‘I think we use the Mental Health Assessment Scale.’- Participant M4
‘Mainly based on clinical judgment for now.’- Participant D5
‘I use the PHQ 9 questionnaire for screening.’- Participant D3
‘Based on the clinical judgement.’- Participant M5
When participants were asked about their familiarity with the EPDS, most healthcare providers reported limited or no familiarity with the tool. Several participants explicitly stated they were not familiar with it: ‘I am not, please’ (Participant M1), ‘No, I am not’ (Participant M3), ‘No please’ (Participant M5), and ‘I am sorry. No, I am not very familiar with it’ (Participant D1). One participant mentioned having seen the tool but noted limited engagement: ‘No. I think I have seen it once, but I have not really paid attention… we are now really trying to incorporate maternal mental health into our whole system’ (Participant D5). These responses indicate that the EPDS is not commonly recognized or utilized in clinical practice among the healthcare providers in this study, with most participants reporting a lack of familiarity with the tool.
The association between HDP and PPD was acknowledged by healthcare providers, who attributed it to factors such as stress, socio-economic status, and medication compliance. Intrapartum events, lack of family support, and extensive medical care during pregnancy were also cited as contributing factors. Participants emphasized the need for holistic care and support to mitigate the risk of PPD among women with HDP.
‘Cost of care, the fact that some of them do lose their babies, the fact that some of them need caesarean section for their delivery.’- Participant D1
‘Hypertensive disorders generally put patients at risk of more extensive investigations and care procedures during the antenatal period which tends to put a lot of stress on them that can trigger depression post-delivery.’- Participant D3
‘The intrapartum events a woman experiences can really affect how the preeclampsia or hypertensive disorder could deteriorate into depression. Women who go through very difficult births or experience complications during pregnancy and antenatal care can easily become depressive during the postpartum period. Sometimes, it also depends on the quality of care they receive. If a pregnant woman faces tedious procedures before accessing care, it worsens her condition. For example, if she is newly diagnosed with hypertension, pregnancy itself is already stressful. Adding a new diagnosis and the challenge of navigating long queues and extended wait times for lab tests and consultations can be overwhelming. These experiences mentally affect the women we care for.’ - Participant M3
‘The medication is very painful. Also, anxiety because when we tell them that they are blood pressure is high, mostly they think about the baby, whether the baby is going to survive, and what is happening in their system.’ - Participant M2
Overall, stress, medication compliance, lack of social support, and the management challenges associated with HDP were identified as significant risk factors for PPD among women with HDP. Healthcare providers emphasized the difficulty some women face in maintaining medication compliance, particularly due to the pain associated with treatment and anxiety about the health of both the mother and baby. Addressing these factors was seen as essential for improving maternal mental health outcomes.
Discussion of results
The systematic review revealed higher rates of depressive symptoms, state anxiety, and trait anxiety in the postpartum period among women with HDP compared to controls. The meta-analysis indicated a strong, positive association between HDP and PPD, with pooled odds ratios ranging from 2.24 to 2.61. Notably, the risk of PPD escalated with the severity of HDP, particularly in cases of severe preeclampsia and eclampsia, suggesting a dose-response relationship that supports a causal link.
In the qualitative study, healthcare professionals provided insights that bolstered the generalizability of the findings. Interviews revealed a substantial number of hypertensive pregnancies, with frequency estimates ranging from 5 to 100 cases per month. PPD prevalence among HDP patients was estimated between 2% and 50%, with the highest likelihood of PPD observed in severe preeclampsia and eclampsia cases. Healthcare providers observed varied trends in HDP and PPD prevalence, citing factors such as increased awareness of maternal mental health and socio-economic influences. They noted that stress, preterm delivery, and socio-economic factors predispose women with HDP to PPD.
The perspectives of healthcare professionals highlighted the mental health consequences of HDP post-delivery. Lack of social support and medication compliance were identified as significant risk factors for PPD among women with HDP. The variability in observations and estimates among participants indicated challenges in generalizing prevalence rates even within a single facility, emphasizing the necessity for more extensive research. The findings suggest that addressing both physical and mental health in a comprehensive manner is crucial for improving maternal outcomes.
Comparisons between women with and without hypertensive disorders revealed significant disparities in vulnerability, with lower PPD rates in the absence of hypertensive conditions. The stress of managing HDP itself, compounded by traumatic deliveries, significantly impacts the postpartum mental state. Strengthening social support systems, improving antenatal and intrapartum care, and providing counselling and support for those with HDP can mitigate the risk of PPD.
These findings align with previous research. Blom et al., Reference Blom, Jansen, Verhulst, Hofman, Raat and Jaddoe2010 reported a significant association between preeclampsia and PPD (OR 2.4; 95% CI: 1.28–4.50; p = 0.007). A meta-analysis by Caropreso et al, Reference Caropreso, De Azevedo Cardoso, Eltayebani and Frey2020 revealed an increased risk of PPD among women with preeclampsia (OR 1.54) and gestational hypertension (OR 1.42). They also found a significant association between preeclampsia and the severity of depressive symptoms both during and outside the perinatal period. Youn et al, Reference Youn, Lee, Han, Kim, Lee, Oh, Jeong and Cho2017 found that preeclampsia was associated with PPD (OR 1.12; 95% CI: 1.03–1.22) even after adjusting for various factors. Additionally, Meltzer-Brody et al., Reference Meltzer-Brody, Maegbaek, Medland, Miller, Sullivan and Munk-Olsen2017 reported that preeclampsia increased the risk of depression in the first year postpartum by 1.45 times (IRR 1.45; 95% CI: 1.14–1.84).
The multi-pronged findings provide credible evidence that HDP and PPD frequently co-occur and likely share an underlying connection in Ghana. The systematic review and the Meta-analysis included studies from other LMICs, and interviews focused specifically on the Ghanaian context. The implications of the systematic review and Meta-analysis extend beyond statistical associations, providing a foundation for understanding the multifaceted dimensions of HDP-PPD co-occurrence. The dosage-response gradient not only substantiates the statistical linkage but also underscores the clinical relevance of hypertensive severity in predicting postpartum mental health outcomes. Amalgamation of findings from the systematic review and qualitative study paints a comprehensive picture of the intricate association of HDP and PPD in the Ghanaian context. Together, this emphasizes the importance of screening and supportive mental health interventions for those experiencing HDP.
The high estimated prevalence of PPD among HDP patients suggests that providers need to have a high index of suspicion. The prevalence estimates provided by healthcare professionals underscore HDP as a major health priority in pregnancy, with varying caseloads reaching up to 100 hypertensive patients per month in some instances. The co-occurrence rates of PPD among HDP patients, reaching 50%, illuminate the vulnerability of this population, particularly when compounded by stressors related to labour and adverse outcomes. On the other hand, discrepancies in prevalence estimates and observations among healthcare professionals highlight the challenges in generalizing prevalence rates even within a singular facility.
The diverse factors identified, including economic influences, lack of awareness, and stress, underscore the need for a holistic approach to maternal care that addresses both physical and mental well-being. It is crucial to note that the experiences women undergo during labour play a significant role in the onset of postpartum depression, a finding consistent with the observations reported by study participants. The observed increase in co-occurring conditions aligns with global concerns about the intersection of physical and mental health during the perinatal period.
The lack of familiarity with tools like the EPDS is concerning and likely contributes to the variability in estimates. Sole reliance on clinical judgment for identifying PPD among women with prior hypertensive disorders signifies a critical gap in current healthcare practices. Standardizing screening practices is imperative. Implementing systematic use of validated screening tools, such as the EPDS, in routine maternal care could enhance the detection of PPD in this at-risk population. Combining clinical judgment with standardized instruments holds promise for improving identification and subsequent support. Trends are unclear, so monitoring rates over time is also key.
Comparisons between women with and without hypertensive disorders reinforce disparities in vulnerability. The substantially lower rates of postpartum depression in the absence of hypertensive conditions highlight the amplified risk faced by those battling hypertension alongside stressful deliveries.
Strengthening social support systems and enhancing experiences in antenatal and intrapartum care emerged as ways to potentially mitigate this risk of association. The stress of managing HDP itself also appears pivotal. Making care patient-centred and raising awareness may lessen the blow of diagnosis. Counselling couples on preparing for the potential outcomes can set appropriate expectations. Addressing unresolved trauma from negative labour experiences, such as the absence or inadequate use of anaesthesia during perineal tear repair, should be a priority. Healthcare providers should receive training on trauma-informed care, pain management, and empathetic communication to ensure respectful and patient-centred maternity care. Additionally, institutional guidelines should be reinforced to standardize pain relief practices and promote accountability in obstetric care. The high prevalence of PPD among HDP patients highlights the need for a high index of suspicion and a holistic approach to maternal care that integrates mental health support.
The systematic review included studies with varying designs and methodologies, introducing heterogeneity that impacted estimated precision. The studies were from other LMICs, as no Ghanaian literature was available, limiting generalizability to the Ghanaian population. Variations in healthcare systems and practices across countries affected external validity. Also, the qualitative data relied on professionals’ recollections rather than direct patient data, introducing recall bias and subjectivity. Lastly, excluding women patients’ perspectives was a significant limitation, undermining representativeness and qualitative insights. However, the comprehensive approach of combining quantitative and qualitative data provided a robust understanding of the link between HDP and PPD. Despite the limitations, the strong analytical data and contextual insights from healthcare professionals offer a compelling argument for the increased risk of PPD in women with hypertensive disorders. These findings highlight the need for integrated perinatal care strategies, tailored interventions, and enhanced mental health policies to address this vulnerable population’s needs effectively.
Conclusion
The comprehensive approach combines quantitative and qualitative methods to highlight the connection between HDP and PPD. The results from both methods confirm this link. Quantitative data indicate a higher occurrence of PPD in women with HDP, suggesting a significant relationship between hypertensive disorders and increased likelihood of PPD. Qualitative data, derived from healthcare professionals in Ghana, provided real-life insights into the prevalence, patterns, perceptions, and risk factors associated with HDP and PPD. This approach reinforces the conclusion that women with HDP are at a higher risk for experiencing postpartum depressive symptoms.
The results advocate for integrating mental health screening and treatment into standard perinatal care for women with hypertensive disorders of pregnancy (HDP). This includes enhancing awareness, training, and the use of validated screening tools by healthcare providers to promptly identify mental health issues in this vulnerable population. The findings emphasize the need for tailored counselling, peer support networks, and postpartum monitoring for women who have experienced hypertension. Structured interventions can offer emotional and practical support to prevent postpartum depression. Recent research highlights the importance of incorporating mental health screening, awareness, and support programs into prenatal and postnatal care. The study urges policymakers to consider the link between pregnancy disorders and the risk of postpartum depression when designing maternal health policies and care models. It advocates for mental health policies that prioritize psychological well-being as a core element, addressing psychosocial risks alongside physical ones throughout women’s health journeys.
The World Health Organization’s manual on integrating health into maternal and child health services, released in September 2022, provides a detailed framework for improving maternal healthcare services in Ghana. This evidence-based manual offers guidance for program managers, healthcare administrators, and policymakers on organizing and overseeing child health services, aiming to maintain quality integrated mental health services for women during the perinatal period. The Royal College of Obstetricians and Gynaecologists (RCOG) and the National Institute for Health and Care Excellence (NICE) have also developed guidelines to support women with mental health issues during pregnancy and postnatal periods. These guidelines include recommendations for managing mental health concerns, assessments, treatments, and support, and can be integrated into maternal health services policies to enhance the quality of care.
Cultural aspects include beliefs about care practices, family dynamics, societal views on motherhood and mental health—all influencing how women perceive pregnancy, access support services and adapt to postpartum health challenges. Influences such as policies, resource allocation, institutional norms, socioeconomic disparities in healthcare access based on ethnicity as well as biases in healthcare settings all have a role to play. These factors affect women’s ability to access quality prenatal care services, available support during pregnancy and postpartum assistance, for mothers. The cultural and systemic aspects, when combined shape the environment in which women navigate pregnancy, childbirth and the postpartum period.
By incorporating these guidelines into Ghana’s mental health policies, the country can improve its ability to provide effective mental healthcare to pregnant and postpartum women. Fully understanding these components is vital for providing care to individuals throughout their pregnancy and postpartum journey. This does not only improve well-being but also contributes to better pregnancy outcomes and childbirth experiences for all women.
Funding statement
This research received no specific grant from any funding agency, commercial entity or not-for-profit organization.
Competing interests
The authors have no conflicts of interest to declare.
Ethical standard
Ethical approval was obtained from the Research Ethics Committee at the College of Nursing, Midwifery, and Healthcare, University of West London (approval number 01690), and from the institutional review board of UGMC under reference UGMC/IRB/089/23. Prior to participation in the study, written informed consent was obtained from all participants. The consent process ensured that participants were fully informed about the study’s purpose, procedures, potential risks, and benefits, as well as their right to withdraw from the study at any time without any consequences. The confidentiality and anonymity of all participants were strictly maintained throughout the study.
















