Introduction
A recent poll undertaken by a major health insurance provider indicates many New Zealanders underestimate the impact of non-communicable diseases (NCDs), with half believing these diseases cause only 10–50% of deaths when, in fact, they account for 90% of total mortality 1,2 . More significantly, premature death remains high, with those over 30 having a 10% probability of dying from one of the four major NCDs (cardiovascular disease, cancer, chronic respiratory disease and diabetes) before age 70 3 . NCDs significantly burden NZ’s economy, with type 2 diabetes alone costing NZ$2.1 billion annually, or 0.67% of Gross Domestic Product 4 . This cost, including treatment and lost productivity, is expected to increase by 70–90% over the next 20 years, as recent projections estimate half a million cases by 2040 5 .
Indigenous Māori populations and Pacific Island peoples face chronic health inequities due to poor healthcare access and systemic racism, leading to high comorbidity and high premature mortality rates Reference Walsh and Grey6–8 . These inequities cost NZ$863.3 million annually in avoidable illnesses, injuries, and deaths – costs which are largely borne by Māori families and communities Reference Reid, Paine and Te Ao9 . Increased morbidity also leads to social costs like early labour force withdrawal, absenteeism, reduced productivity, informal caregiving, and decreased social participation and quality of life Reference Nikolic, Stanciole and Zaydman10 .
The perception that NCDs, particularly those linked with obesity and poor metabolic health, are caused by individual behaviours and are solely the concern of the individuals affected is a common one Reference Lundell, Niederdeppe and Clarke11–Reference Kolata15 . However, this view is increasingly challenged by those who recognise that social, structural, and environmental factors significantly limit individuals’ ability to make personal health choices Reference Marmot and Bell16–Reference Thirlaway and Davies19 . Nowhere is this more apparent than in the evidence for Developmental Origins of Health and Disease (DOHaD), which proposes that the trajectory of an individual’s lifelong health is heavily influenced by early-life environmental factors, starting before conception and even across generations Reference Gluckman, Hanson and Mitchell20–Reference Mengelkoch and Hill22 .
Investing in public awareness of DOHaD principles is therefore crucial for addressing social determinants of health and guiding health policies towards actions that will ultimately relieve future generations of burdens both physiological and fiscal. This study aims to evaluate baseline awareness and knowledge of NCD and DOHaD concepts in the wider NZ population and to identify potential avenues for knowledge translation interventions. Specifically, we aim to measure public familiarity with the characteristics of NCDs as chronic, non-transmissable diseases that develop slowly over the life course. Using a range of indirect and direct questioning approaches to determine participants’ awareness of NCD risk factors, our objective is to determine the extent to which NZers understand the association between early-life environmental exposures and later-life health, and which demographics may predict DOHaD awareness. The survey is not specifically targeted towards any particular age group or life stage, as DOHaD knowledge translation increasingly recognises that addressing structural factors contributing to detrimental early-life environmental influences is likely to have a greater (and less stigmatising) effect than interventions targeting individual behaviour change Reference Low, Gluckman and Hanson17,Reference Penkler, Hanson, Biesma and Muller23 .
Methods
Ethical approval
This study was approved by the University of Auckland Human Participants Ethics Committee (UAHPEC; refs 013093/16008, 23,178).
Survey tool
A short questionnaire, suitable for both face-to-face and digital formats Reference Hildreth, Oyamada and Bay24 , was used to measure awareness of NCD risk factors and DOHaD concepts. Developed by the research team, the Public Understanding of DOHaD survey has previously been used with tertiary students in NZ and Japan, and with NZ primary and secondary school teachers Reference Hildreth, Oyamada and Bay24,Reference Oyamada, Lim, Dixon, Wall and Bay25 . It includes a mix of open-ended questions to capture respondents’ perspectives ‘in their own words’ and Likert scales to assess knowledge around the impacts of health behaviours of parents and offspring at various life stages Reference Hildreth, Oyamada and Bay24 . Responses are subsequently coded for quantitative analysis, enabling the findings from this study to act as a baseline for future comparison with repeated surveys in the same and other populations.
Subject sampling and data collection
During the initial data collection period, trained research assistants approached adults outside five major Auckland retailers, selected for their broad appeal. Permission was granted by retail management. Data collection occurred over five months in 2015 and was carried out on a variety of days and times. In 2016, following a preliminary analysis of the data Reference Bay, Dixon, Morgan, Wall and Oyamada26 , a local cultural festival was added to obtain a more representative sample based on contemporary census data Reference Stats27 . A total of 702 interviews were conducted, with about 2,300 people declining to participate.
Participants gave verbal consent after a brief explanation of the study. Demographic information, including age, gender, education, occupation, and ethnicity, was collected. Interviewers used checklists of common responses, recording any unique answers verbatim Reference Singer and Couper28 . At the end of the interview, participants received a leaflet directing them to further information about NCDs and DOHaD, as well as study results once available.
A repeat survey planned for 2020–21 was delayed due to COVID-19 and, due to ongoing restrictions in NZ, shifted to online data collection in mid-2022 following updated ethical approval. Using the online survey platform Qualtrics, 1121 anonymous responses were gathered from social media users via paid ads on Facebook and Instagram. Advertising initially targeted all NZ users aged 16+; this was refined to focus on underrepresented demographics as the campaign progressed Reference Ali, Foreman, Capasso, Jones, Tozan and DiClemente29 . Based on our own and others’ experience, we were aware that recruiting Māori and Pacific respondents, particularly young males, via social media may be challenging Reference Ni Mhurchu, Blakely and Funaki-Tahifote30,Reference Kearns, Baggott and Harwood31 . However, engaging these groups in research is important not only due to racially based health inequities, but also obligations under the Treaty of Waitangi to work towards reducing disparities for Māori Reference Reid, Paine and Curtis32,Reference Came and Tudor33 . In consultation with Kaiarahi (Māori advisors), advertising creative was designed to appeal to Māori through positive depiction of Māori whānau (families), use of reo Māori (Māori language) and whakataukī (proverbs). To minimise self-selection bias, the accompanying text simply invited viewers to ‘help researchers understand New Zealanders’ thoughts and opinions about lifelong health’ Reference Arigo, Pagoto, Carter-Harris, Lillie and Nebeker34,Reference Choi, Milne, Glozier, Peters, Harvey and Calvo35 . Participants could enter a draw for a $250 gift card, with contact details recorded separately to maintain anonymity. An additional 108 responses were obtained through snowball sampling. After removing duplicates, 814 valid responses were available for analysis.
In early 2023, with COVID-19 restrictions lifted, 96 face-to-face interviews were conducted at two Auckland retail locations. This enabled a comparison of methods and supported purposive recruitment of additional subjects from demographics that had proven difficult to reach via online advertising Reference Bethlehem36 .
Data analysis
Although the questionnaire included open-ended and multiple-choice questions, data analysis was mainly quantitative, with open-text responses coded into categories. IBM SPSS Statistics v.29 was used to analyse statistical data, with significance at p = 0.05.
For each survey question, chi-square tests compared responses by demographics and cohorts, as shown in Fig. 1. Wherever a significant difference was identified, pairwise comparisons were made to determine the source and rule out confounding factors. Overall, these comparisons showed only one significant difference between 2015–16 responses and 2022-23 responses that could not be explained by participant age, ethnicity or data collection method (Fig. 1(d)). Although there were insufficient responses collected in 2023 to test for significance, no obvious differences were apparent in a comparison of face-to-face interview responses between 2015–16 and 2023 (Fig. 1(e)). A final comparison between cohorts (Fig. 1(f)) identified significant differences between the 2022 cohort (online questionnaire) and the 2015, 2016 and 2023 cohorts (face-to-face interview).
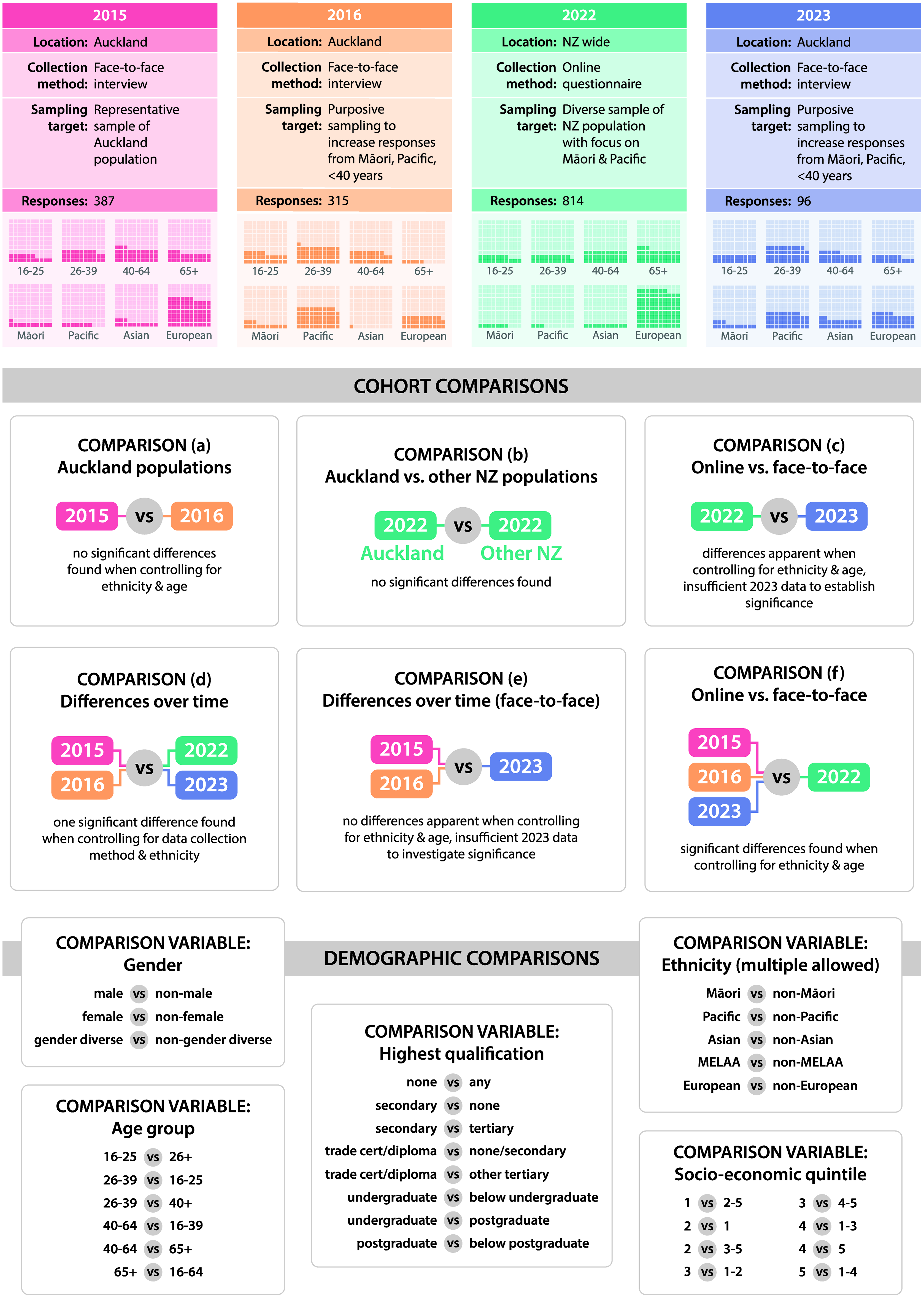
Figure 1. Overview of study progression and analysis between cohorts and demographics.
Despite the original intention to treat the 2015–16 data as a baseline from which to explore changes over time, these comparisons suggested that public knowledge of DOHaD concepts had not changed in any measurable way between 2015–2023. Therefore, subsequent analysis focused on determining which participant demographics are most likely to predict DOHaD awareness. Responses were combined into one dataset for analysis, the characteristics of which are described in the Total responses column of Table 1. All significant differences found are detailed in the Results below.
Table 1. Demographics of survey respondents in each cohort (percentages). As the cohorts have been combined for analysis, totals for each characteristic are shown in the total responses column. The final column (NZ total population) illustrates how this dataset compares to percentages in the NZ population
* Gender diverse was not included as a coding category for the 2015-16 data, however 5 of the 702 subjects were recorded as neither Male or Female. There was no Gender diverse category in the 2018 NZ Census.
** MELAA is a category used in the NZ census inclusive of people from the Middle East, Latin America, Africa.
Odds ratios were calculated where relevant to measure the strength of associations identified, for the purpose of better understanding how DOHaD awareness differs between demographic groups. Trends resulting from the grouping of multiple Likert scale statements were evaluated using linear regression to establish directionality and marginal homogeneity tests to confirm the statistical significance of differences observed. Mann-Whitney U tests were used to compare scores for the maternal nutrition questions based on demographics.
Demographic data included age, gender, occupation, and education. Socioeconomic status (SES) was derived from education and occupation, using the New Zealand Socioeconomic Index contemporary to each dataset (NZSEI-13, NZSEI-18), and categorised into SES quintiles Reference Fahy, Lee and Milne37,Reference Boven, Shackleton, Bolton, Sporle and Milne38 . Participants identified their ethnicities, coded into six categories: Māori, Pacific Island, Asian, Middle Eastern/Latin American/African (MELAA), European/Pākeha and Other Ethnicity. Multiple ethnicities were allowed, resulting in combined representation of over 100%.
A full description and rationale of methods used is outlined in a separate manuscript, pending publication Reference Hildreth, Oyamada and Bay24 .
Results
In total, 1612 New Zealanders took part in a public survey between 2015 and 2023. The respondent demographics are described in Table 1. Figure 1 provides an overview of the different cohorts and comparisons made between them.
Differences between cohorts
The composition of each cohort differed significantly, highlighting some of the challenges faced by researchers in attempting to recruit a representative sample. In 2016, data collection at a local cultural festival was needed to increase Pacific and Māori participation as these populations had proven difficult to engage in a retail context the previous year. Forced online due to COVID-19 restrictions, 2022 survey responses skewed older, more educated, and predominantly of European descent despite efforts to target a younger, diverse audience, using Māori language advertising and imagery specifically designed to attract Māori and Pacific social media users. This suggests that Facebook and Instagram alone were insufficient to engage a representative NZ sample, and the comparatively small face-to-face sampling in the 2023 cohort did not correct this imbalance.
However, combined responses from 2015 to 2023 approximate the demographics represented in the 2018 census (as shown in Table 1) 39 . As the combined dataset is more representative of the NZ population than any of the individual datasets, treating the data as a whole increases the statistical power to predict NZers DOHaD knowledge based on associated characteristics. Therefore, our analysis is not centred on comparing the earlier and later cohorts but rather on exploring factors contributing to DOHaD awareness in the community.
Non-communicable disease awareness
The first section of the questionnaire assesses participant knowledge of NCDs, their characteristics and risk factors. Overall, 59.2% of respondents were familiar with the term ‘non-communicable disease’, with older participants much more likely to recognise it: 30.1% of 16–25 year-olds versus 78.9% of those 65+ (p < 0.001). A higher level of educational attainment was also associated with familiarity, while only 25.5% of Pacific respondents said they had heard it before (p < 0.001), shown in Fig. 2(a).
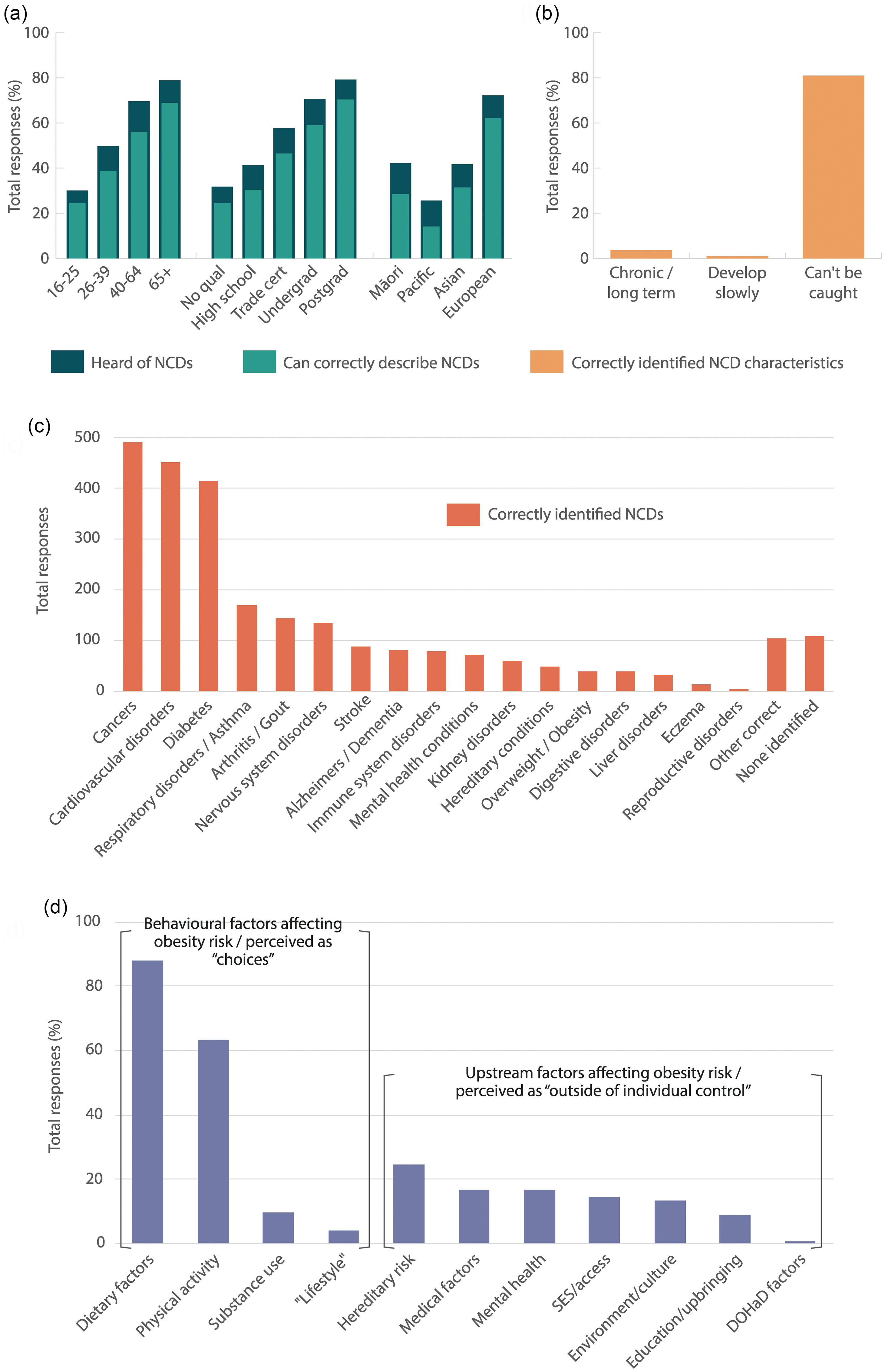
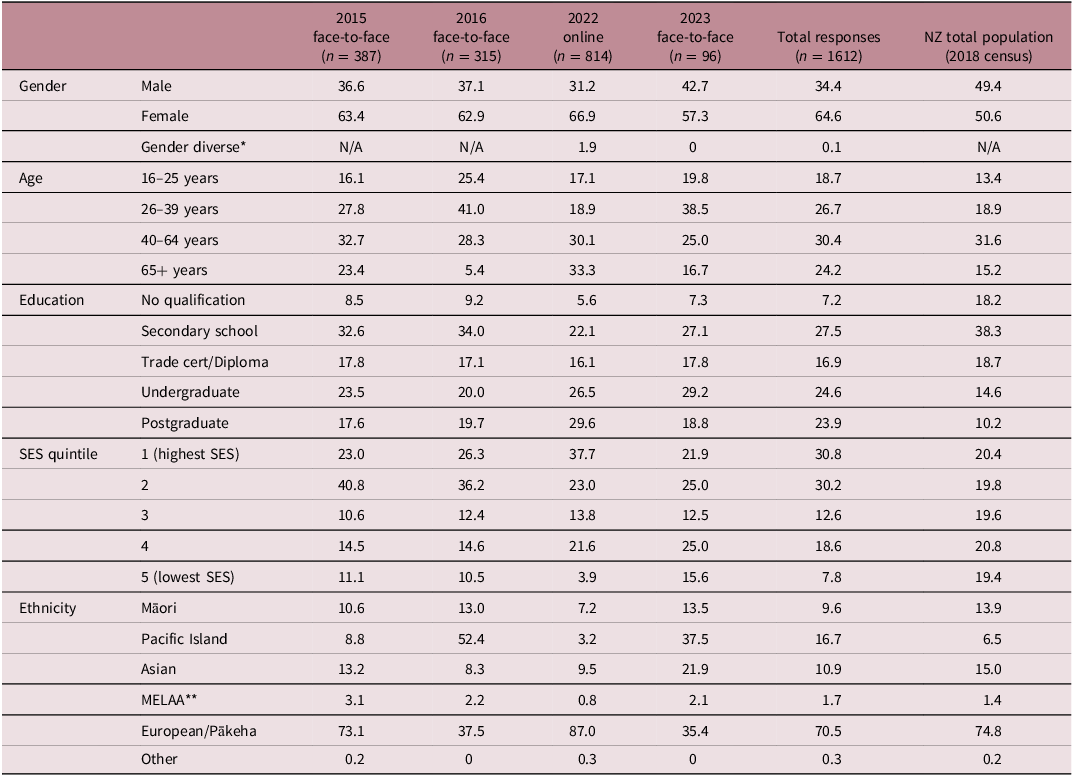
Figure 2. (a) Respondent familiarity with the term “non-communicable disease”, grouped by age, education and ethnicity; (b) Overall proportion of respondents identifying each of 3 key characteristics of NCDs when asked to describe the term’s meaning; (c) Count of NCDs identified by respondents when asked to list examples of NCDs; (d) Factors identified as contributors to obesity risk.
Those familiar with the term ‘non-communicable disease’ were asked about its meaning, with 89.2% providing a correct definition, and no significant differences were observed among the remainder who did not. Participants’ definitions were coded based on their identification of three pre-defined characteristics of NCDs: a) Slow to develop, b) Chronic or long-lasting, and c) Can’t be caught from another person. Can’t be caught featured in 81% of responses, while Slow to develop and Chronic were less frequently mentioned, by 1.0 and 3.7% of subjects respectively (Fig. 2(b)).
To illustrate their understanding of the concept, the same participants were then invited to list examples of NCDs, with 82.7% providing at least one correct answer and some online respondents listing ten or more diseases. Cancer, heart/cardiovascular disease and diabetes were the most common examples offered (Fig. 2(c)). Viral and bacterial infections were the most frequent incorrect examples. In total, 14.8% gave entirely or partially inaccurate answers, and 11.8% were unable to name any conditions. Of those familiar with the term ‘non-communicable disease’, online data collection was the strongest predictor of the ability to provide accurate examples, as face-to-face interview subjects were around six times less likely to attempt to list any examples at all (OR 6.63, 95% CI 4.15–10.59).
Identification of NCD risk factors
To conclude the NCD section of the questionnaire, participants were asked to ‘list some things that might increase your chance of developing overweight or obesity’. Responses were coded into 11 core categories, with Dietary factors (87.8%) and Physical activity (63.4%) most frequently identified (Fig. 2(d)). Online respondents often listed multiple risk factors and thus were more likely to mention Physical activity, Socioeconomic factors, Pre-existing medical conditions (including medication side effects), and Genetic or hereditary factors (p < 0.001). Dietary factors was the only risk category more likely to be identified by face-to-face subjects (92.8% vs 85.7% online; p < 0.001), and this also increased with age (85.3% aged 16-25 to 93.1% aged 65+; p = 0.004). An increase in responses relating to Mental health factors between 2015-16 and 2022-23 represents the only significant change over time for any of the survey questions (8.7% to 23.1%; p < 0.001, Fig. 1(d)). This difference was most noticeable amongst Asian participants (15.6% to 38.0%; p < 0.001) and those aged <40 years (8.4% to 20.2%; p = 0.006).
Higher educational attainment was associated with responses of Genetic or hereditary factors (p < 0.001), Education or upbringing (p = 0.001), and Environmental or cultural factors, a broad category encompassing references to the physical or social environment such as food marketing, employment or time pressures and recreational opportunities as well as racism and colonialism (p = 0.007). Female and gender diverse participants listed more Pre-existing medical conditions, Genetic or hereditary factors, and Mental health factors (all p < 0.001), with the small number of gender diverse participants being more than three times as likely as both males and females to identify risk factors in these categories (OR 5.62, 95% CI 2.02–15.64; OR 4.54, 95% CI 1.60–12.83; OR 3.28, 95% CI 1.16–9.29 respectively). Overall, online, educated, European ethnicity and non-male respondents showed greater awareness of upstream, environmental factors contributing to obesity risk, in addition to individual behavioural factors such as diet and exercise (p < 0.001).
Impact of early-life environmental factors on health throughout the life course
The second section of the questionnaire focuses on awareness of the impact of parental health and nutrition on lifelong health, using Likert scales with options Agree, Strongly agree, Disagree and Don’t know. Slightly agree was also offered in the 2015/16 interviews and, for the purposes of comparison, this option was randomly allocated to 50% of the face-to-face interview scripts in 2023. However, few participants selected it, and a decision was made to omit the option from the online questionnaire, and treat Slightly agree responses as Agree.
The first statement, The food we eat affects our health and wellbeing, received 99% agreement. Those who disagreed were mostly of Māori or Pacific ethnicity and had no formal educational qualification (p < 0.001).
Importance of parental health prior to conception
More subjects viewed maternal preconception health as influential for fetal health than paternal health, as shown in Fig. 3(a). Agreement with both statements showed a linear increase in relation to educational attainment, and in the case of maternal health, was also linked with increasing age and socioeconomic status (all p < 0.001). Younger respondents (16-25) were less aware of the contribution of paternal preconception health (p = 0.001). Of those who didn’t agree with these and several other statements, online respondents were significantly more likely to choose Don’t know than their face-to-face counterparts, who favoured Disagree (p < 0.001). Males were more likely to select Disagree than Don’t know (p = 0.034) regarding paternal health, as were people of Pacific ethnicity, regardless of gender or data collection method (p < 0.001).
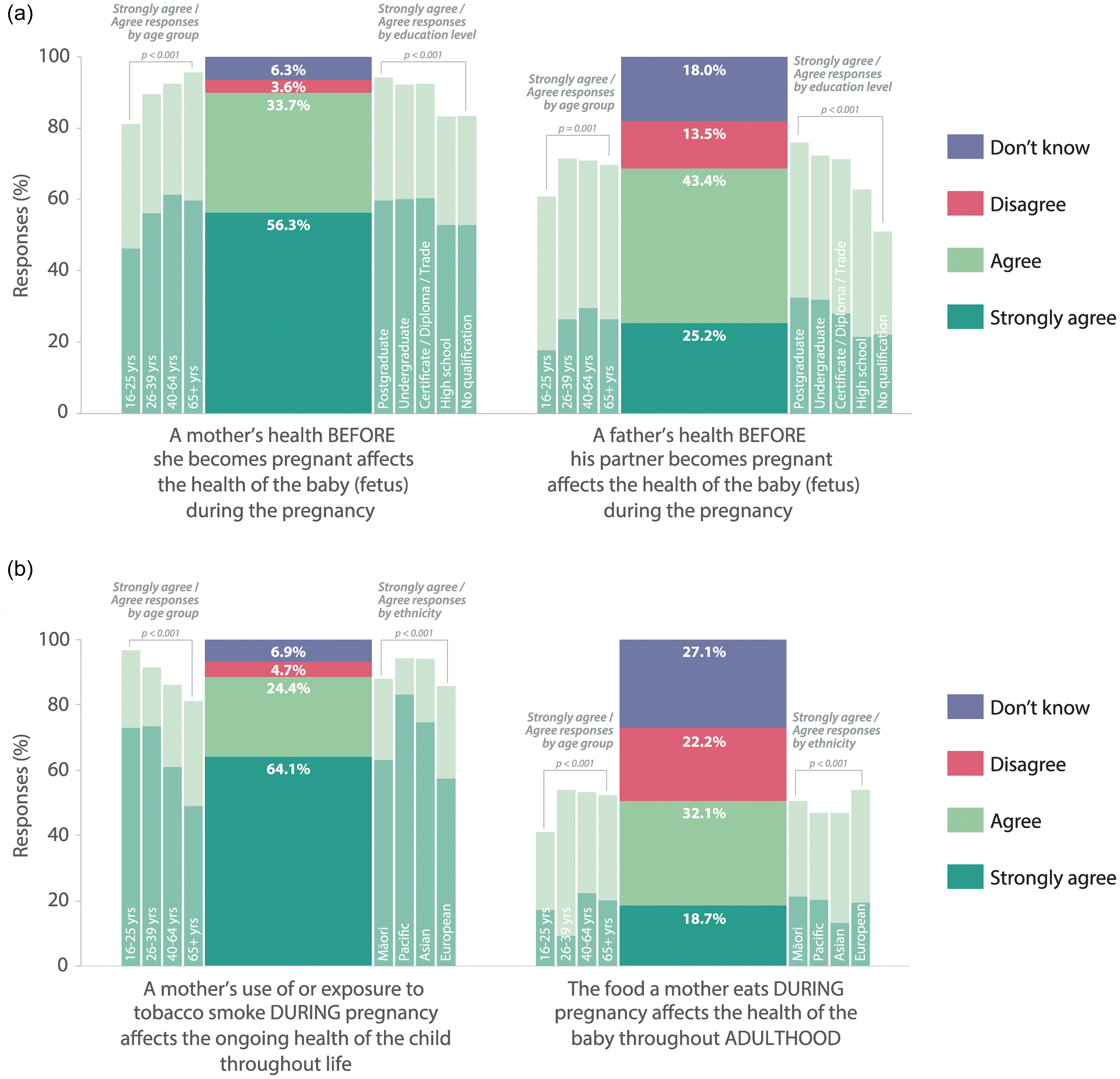
Figure 3. (a) Perceived importance of maternal vs. paternal preconception health for the health of the fetus. Side bars show proportion of agreement in each bracket for age and educational attainment; (b) Perceived long-term effects of maternal diet vs. prenatal tobacco exposure. Side bars show proportion of agreement in each bracket for age and ethnicity.
An additional statement regarding paternal health was added to the online survey: A father’s health BEFORE his partner becomes pregnant may affect the health of the baby THROUGHOUT adulthood. Agreement was highest among those with postgraduate qualifications (71.4% vs 57.5%, p < 0.001), whereas males were most likely of all demographics to disagree that a father’s health could have an ongoing impact for the child (17.1% vs 9.6%, p = 0.003).
Effect of maternal and infant nutrition on lifelong health
While 96.6% agreed that The food a mother eats DURING pregnancy affects the health of the baby (fetus) DURING the pregnancy, fewer recognised its long-term impact: 77.7% agreed the effects persisted through infancy, 69.8% through childhood, and 50.8% agreed prenatal nutrition could affect adult health.
Figure 4(a) illustrates the decrease in agreement and corresponding increase in both Disagree and Don’t know responses concerning the potential impact of maternal diet at different life stages. Tests of marginal homogeneity confirm significant differences across the four statements. As the vast majority of answers reflected this trend, scores can be allocated based on the point at which each participant stopped agreeing with the statements (if at all). Comparison of scores indicates European ethnicity, university education, and familiarity with DOHaD terminology were linked to higher agreement, while 16–25 year-olds were least likely to agree beyond the first statement (all p < 0.001). This is reflected in the linear regression trends in Fig. 4(b–d).
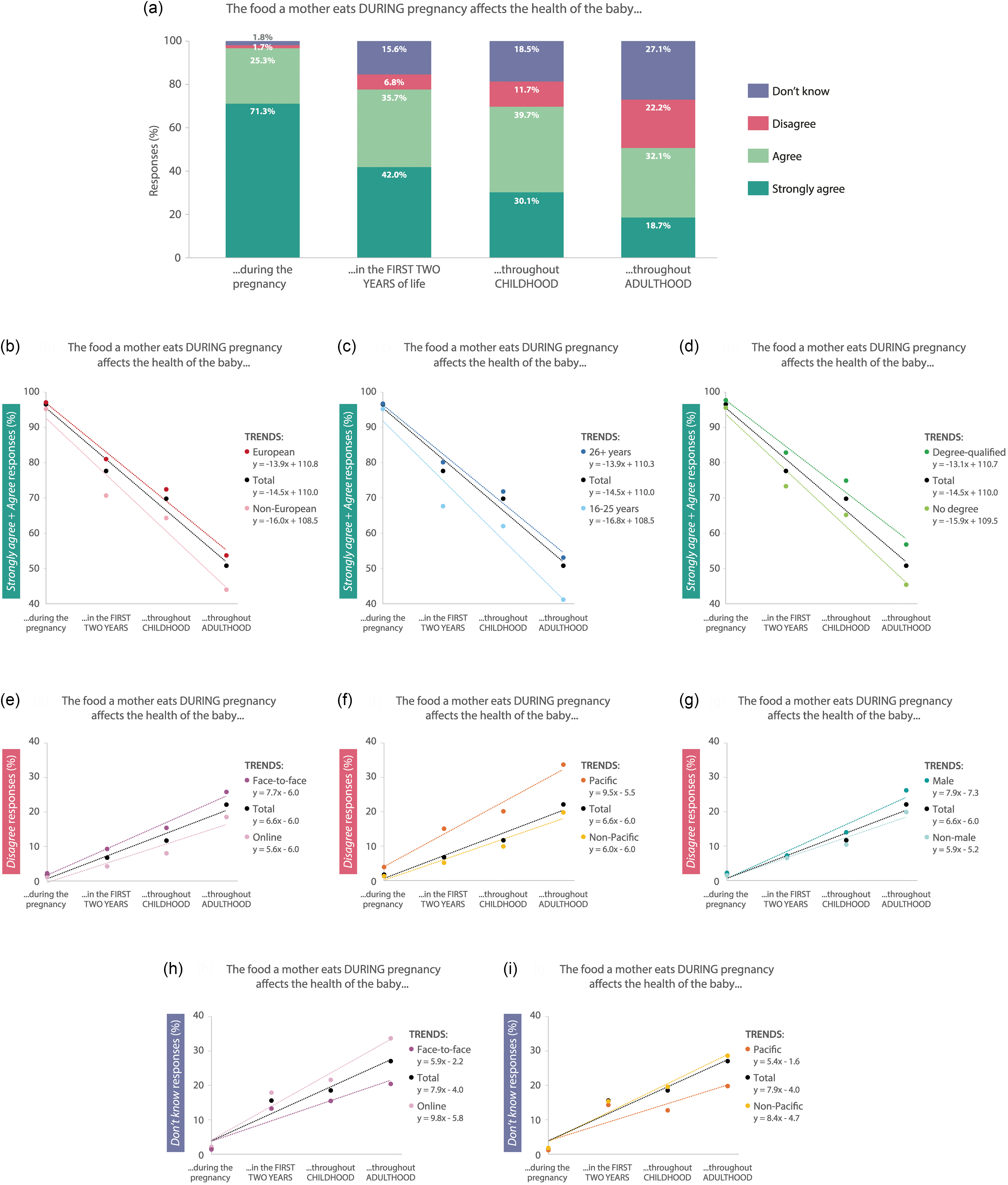
Figure 4. (a) Perceived impact of maternal diet on lifelong health of the child. Responses for each of the four statements are significantly different (p<0.001); (b-d) Differences in combined “Strongly agree” and “Agree” responses based on ethnicity, age and education, shown with linear regression trend lines; (e-g) Differences in “Disagree” responses based on data collection method, ethnicity and gender, shown with linear regression trend lines; (h,i) Differences in “Don’t know” responses based on data collection method and ethnicity, shown with linear regression trend lines.
As with most of the Likert statements, disagreement was highest amongst face-to-face interview respondents and those of Pacific ethnicity, whereas online respondents favoured the Don’t know option (Fig. 4(e,f,h,i); all p < 0.001). Males were more likely to choose Disagree than Don’t know for statements about childhood and adulthood impacts, regardless of data collection method or ethnicity (Fig. 4(g); p = 0.04; p = 0.004, respectively).
A similar trend was seen with infant nutrition: 93.2% agreed it affects health throughout childhood, dropping to 75.6% for adulthood. More female respondents agreed with both (94.5%, p = 0.006; 77.8%, p = 0.004) while Asian respondents were less likely to agree with the latter (68.0%, p = 0.016). The strongest predictors of agreement remained educational attainment, age and European ethnicity.
Maternal nutrition vs. tobacco exposure
The final Likert scale statement was A mother’s use of or exposure to tobacco smoke DURING pregnancy affects the health of the child. In the online survey, this was clarified as the ongoing health of the child throughout life, which resulted in proportionally fewer Strongly agree responses, however total agreement remained similar (Fig. 2(b)). In contrast to ratings for the previous statements, agreement was higher amongst younger, non-European respondents (both p < 0.001), with age <26 being the biggest predictor of agreement (96.3% vs. 80.6% for age 65+). Pacific and Asian subjects were more likely to recognise the risks of maternal tobacco exposure (p = 0.001; p = 0.004, respectively), as were those with a University qualification (p = 0.015).
Knowledge of DOHaD terminology
31.7% of participants had heard of ‘Developmental Origins of Health and Disease’ or ‘First 1000 Days’, a term highlighting the importance of the period from conception to age two Reference Bellieni40 (Fig. 5(a)). Recognition of this terminology was strongly associated with European ethnicity, higher socioeconomic status and online data collection (all p < 0.001), with 49.0% of online participants claiming familiarity with the phrases.

Figure 5. (a) Proportion of subjects familiar with DOHaD terminology; (b) Source of participant familiarity with terminology; (c) Number of key elements mentioned in participants’ definitions of DOHaD terms; (d) Overall proportion of respondents identifying each of 3 key elements of DOHaD when asked to describe the term’s meaning.
Only 5.5% of online respondents could fully define the terms, encompassing three pre-defined criteria: a) the early-life period begins prior to conception, b) the terms refer to early-life environmental factors, and c) adult health can be impacted (Fig. 5(c)). Environmental factors was the most commonly recognised element (55.6%), followed by adult health impact (43.0%) and prior to conception (12.2%), as shown in Fig. 5(d).
Other sub-group analyses
While face-to-face interviews were conducted in Auckland, the 2022 online survey targeted participants across New Zealand, with regional response rates proportional to population size. No significant geographical differences were found that could not be explained by other participant characteristics.
Categorisation by occupation enabled comparisons between health professionals, educators and others with university qualifications. Health professionals were more familiar with NCDs and DOHaD terminology (77.1% vs. 50.8%, p < 0.001). They also more frequently cited Education or upbringing (18.0% vs 6.9%, p < 0.001), Environmental or cultural factors (23.8% vs 13.2%, p = 0.003) and Socioeconomic factors (27.0% vs 15.4%, p = 0.002) as contributors to obesity risk. Both health professionals and educators were more likely than other degree-qualified participants to agree that the preconception health of mothers (98.8% and 98.6% vs 90.5%, p = 0.001) and fathers (86.7% and 83.6% vs 69.4%, p < 0.001) may affect fetal health, however there were no differences for any of the other Likert statements.
Discussion
These findings show low awareness of DOHaD concepts in New Zealand, highlighting the need for initiatives to promote understanding of the long-term impacts of environmental exposures in early life.
Awareness of NCD risk
Verbatim responses to open-ended questions provided insights beyond the face value of the questions, particularly in the online setting Reference Singer and Couper28 . While most subjects exhibited a basic understanding of NCDs, the obesity risk factors identified reflect a belief that metabolic disease susceptibility is largely determined by an individual’s behaviour (diet and physical activity) or completely outside of their control (heredity). This aligns with findings from a recent Swiss survey, where participants overestimated the extent to which NCDs can be prevented or delayed by lifestyle changes Reference Irani, Coquoz, von Wolff, Bitterlich and Stute41 . An exception may be younger subjects, who were least likely to link dietary factors with obesity risk, an outcome supported by other studies in which adolescents discount the likelihood of developing metabolic disorders during their lifetime, and the potential health impacts of their behaviour Reference Dickerson, Smith, Sosa, McKyer and Ory42–Reference Schwartz, Forthun and Ravert44 . This contrast may be a reflection of participant characteristics (youthful optimism) or susceptibility to fundamental attribution error (failure to consider environmental effects on others but not oneself) Reference Lundell, Niederdeppe and Clarke11,Reference Granot and Balcetis45 .
Those who did identify environmental and sociocultural contributors to obesity risk predominantly did so as part of a longer, more detailed response. While indicating an appreciation for complexity, this also highlights the extra cognitive work necessary to progress beyond simple heuristics of individual responsibility Reference Lundell, Niederdeppe and Clarke11 . By contrast, framing of the question in a similar survey produced almost 90% agreement that …the environment influences the development of obesity either ‘a lot’ or ‘a fair amount’, suggesting that incorporation of a prompt can lead to deeper consideration of health determinants Reference Lynch, Lewis, Macciocca and Craig46 .
Increased recognition of links between mental health and obesity was the only notable difference between the 2015/16 and 2022/23 cohorts. While the COVID-19 pandemic was an obvious contributor towards both poor mental health and elevated obesity risk during this period, further exploration would be needed to determine the origin of increased awareness Reference Melamed, Selby and Taylor47,Reference Santomauro, Herrera and Shadid48 . Factors such as social media use, economic instability, widening inequality and increased academic pressure on young people could also play a role Reference Foulkes and Andrews49 . Regardless, this finding represents a small step closer to public acceptance of the social determinants of health.
Awareness of DOHaD concepts
McKerracher et al. used different Likert scale statements to calculate a ‘DOHaD knowledge’ score for 330 pregnant participants in Canada, but likewise found greater awareness among older subjects and higher socioeconomic groups Reference McKerracher, Moffat and Barker50 . A Norwegian study of prospective parents using the same scale found that it was male respondents who agreed most strongly with the statements Before pregnancy, both what the mother and the father eat affects the growth and health of their baby and What a woman eats before pregnancy affects the child’s risk of becoming obese as an adult Reference Salvesen, Valen and Wills51 . It is unclear from the phrasing whether responses to the former statement primarily focused on the maternal component. By addressing each parent’s preconception health separately, it was apparent that NZers, particularly those of reproductive age, considered maternal health to be more influential than paternal – a belief shared by Lynch et al.’s Australian subjects Reference Lynch, Lewis, Macciocca and Craig46 .
Lynch et al. also found similar recognition of DOHaD terminology, with approximately a third of the 31–32% who recognised each of the phrases we tested being unable to describe any elements of the definition. Respondents recalled encountering the terms online or from health professionals, unlike the present study, where traditional media (print or mass media) and formal education or professional development were common sources. This suggests DOHaD concepts may be more extensively taught in NZ universities, as fewer than 8% of the Australian participants lacked tertiary qualifications Reference Lynch, Lewis, Macciocca and Craig46 .
Cultural differences
Pacific Island respondents showed a significant preference for the Disagree Likert option over Don’t know, regardless of data collection method. Further investigation may reveal whether this tendency has cultural roots or if there is another underlying reason why Pasifika people believe the statements to be untrue. They were also least likely to recognise ‘non-communicable disease’. This contrasts with evidence from the Cook Islands, where colleagues have recently undertaken the same survey (n = 397). This survey identified awareness of NCDs in 73% of respondents, of whom 49% could accurately describe NCDs Reference John, Samuel-Ioane, Vickers, Tu’akoi and Bay52 , highlighting the importance of reflecting on context as well as factors such as ethnicity when considering awareness of health-related terminologies. It should also be noted that – as illustrated by the DOHaD phrases – familiarity with terminology does not necessarily equate to understanding Reference Trevethan53,Reference Ladwig, Dalrymple, Brossard, Scheufele and Corley54 . For this reason, we emphasise that the survey tool measures awareness and, to an extent, knowledge rather than understanding.
Māori ethnicity was not associated with any findings of practical significance, and Māori were underrepresented in both 2015-16 and 2022-23 despite purposive interview sampling and targeted online advertising. International evidence suggests social media may increase engagement with harder-to-reach communities Reference Thornton, Batterham, Fassnacht, Kay-Lambkin, Calear and Hunt55,Reference Topolovec-Vranic and Natarajan56 . However, traditional Māori communication preferences strongly emphasise whakawhanaungatanga (mutually respectful relationship-building) and kānohi ki te kānohi (face-to-face) interaction, highlighting a fundamental mismatch between Māori cultural values and the transient, transactional nature of survey research Reference Berryman, Berryman, SooHoo and Nevin57 . The resulting underrepresentation suggests our tests may lack the statistical power to detect significant associations with Māori ethnicity Reference LeCroy, Potter and Bandeen-Roche58 and that engagement with this population might be enhanced via more collaborative research methods and explicit identification of how the research may benefit Māori.
Notably, males were among those most likely to disagree with several Likert statements, particularly in relation to fathers’ health prior to conception Reference McGowan, Lennon-Caughey, Chun, McKinley and Woodside59–Reference Shawe, Patel, Joy, Howden, Barrett and Stephenson61 . This represents a challenge for knowledge translation as achieving a shift to Agree is presumably more difficult from an initial Disagree response than a Don’t know. The Don’t know response reflects a lack of awareness, suggesting that people using this response will not have preconceived notions or biases to overcome once exposed to new information or ideas. In contrast, a person who disagrees with a concept may experience cognitive dissonance and will need to go through the more complex process of challenging, unpacking and changing perceptions to move to a point of incorporating new thinking Reference McKimmie, (eds. Zeigler-Hill and Shackelford62 . By offering the Don’t know option, the survey tool allows an honest response without forcing the respondent to predict or guess the correct response. This provides vital evidence for the development of health promotion tools, which, if there are high levels of disagreement, must offer opportunities to critically evaluate current perceptions to explore and apply different ideas – representing the process of cognitive change that is strong enough to stimulate behaviour change Reference Sun, Li, Cheng, Pan, Shen and Hua63 . A qualitative investigation of NZ men’s perceptions would help to clarify the reasons for disagreement and guide future interventions.
Recruitment and data collection
In addition to providing insight into public awareness of NCD and DOHaD concepts, this study demonstrated how different methods of recruitment and data collection could potentially achieve a representative sample of the NZ population. Future surveys could combine online methods to capture a majority of the responses at minimal expense, supported by face-to-face purposive sampling at carefully chosen locations and public events to reach younger males, Māori and Pacific peoples, and those with lower educational attainment Reference Bethlehem36,Reference Thornton, Batterham, Fassnacht, Kay-Lambkin, Calear and Hunt55,Reference Atkeson, Adams and Alvarez64 .
Such a dataset would need to be analysed carefully, as these findings show online data collection impacts participant responses in two notable respects. Firstly, online participants were more likely to choose Don’t know Likert options than the face-to-face subjects who preferred Disagree. While the proportion of Agree responses is unaffected, it is worth investigating whether the interviewer or interview setting inhibits participants from admitting their lack of expertise Reference Atkeson, Adams and Alvarez64–Reference Couper, Singer, Conrad and Groves67 . Secondly, online respondents appeared more familiar with NCD and DOHaD terminology. This, too, could be attributed to feeling uncomfortable or rushed in a face-to-face situation; alternatively, seeing the phrases in writing may aid recognition, particularly if the surrounding environment makes hearing difficult. Interviewers should therefore ensure they enunciate these terms clearly, encouraging participants to take their time before responding Reference Suchman, Jordan and Tanur65 .
Implications for future interventions
The key question arising from these findings is ‘how can future DOHaD knowledge translation interventions support equitable health outcomes?’ Our results show that those most aware of DOHaD concepts are highly educated, older, more health literate and less likely to experience ethnicity-based discrimination Reference Nutbeam68–Reference Sørensen, Van den Broucke and Fullam70 . This indicates that existing or prior efforts at DOHaD knowledge translation have been less successful at reaching those who would benefit most, thereby risking a widening of the gap between those with different levels of awareness, and reinforcement of generational health disparities Reference Nutbeam and Lloyd71 .
Two findings suggest ways to address this: health workers and educators are more knowledgeable about preconception health, so exploring ways to leverage their expertise could promote DOHaD awareness. Additionally, public awareness campaigns and policy changes have successfully reduced smoking rates and increased understanding of associated risks Reference Gendall, Hoek, Maubach and Edwards72,Reference Trappitt, Li and Tu73 , and we found this awareness to be highest amongst populations that are typically less likely to engage with life-course research or health promotion messaging Reference LeCroy, Potter and Bandeen-Roche58 . While recognising the difference in complexity between nutritional and non-nutritional environmental exposures associated with DOHaD concepts compared to smoking, reviewing the strategies employed to translate evidence about the long-term consequences of tobacco use may provide insights for effective engagement with hard-to-reach populations.
Strengths and limitations
The questionnaire used in this study combines easily coded open-ended questions with ranking options to produce robust quantitative data with minimal prompting or framing of participant responses. This enables us to distinguish between basic awareness or genuine understanding of concepts presented. Having established that the vast majority of differences observed were not due to changes over time, treating the data collected over an 8-year period as a single entity provides a strong basis for comparisons based on participant characteristics. However, the method of data collection (online vs. face-to-face) impacted both the sample demographics and the responses. Recruitment of important minority groups, particularly Māori, was challenging, affecting the statistical power of observations relating to these groups.
Despite efforts to recruit a representative sample, respondents were more educated than the general NZ public, which is unfortunately not unusual for studies of this nature Reference Ni Mhurchu, Blakely and Funaki-Tahifote30,Reference Bonevski, Randell and Paul74 . Socio-economic status (SES) of participants was inferred based on education and occupation in preference to requesting personal or household income information, both to reduce the length of the survey and to prevent participant discomfort. Due to the higher proportion of subjects with university qualifications, responses were unevenly distributed across SES quintile groups, which limited our ability to identify trends based purely on SES. However, for the purposes of comparison with other studies, educational attainment provides a reasonable proxy. The survey results consistently reveal formal education to be one of the strongest predictors of both NCD and DOHaD awareness, a finding echoed by several others in a variety of settings, at least in relation to NCDs Reference Irani, Coquoz, von Wolff, Bitterlich and Stute41,Reference Rios Duarte, Mendivil and Pena-Silva75–Reference Sheshachalam and Chakravarthy77 . Therefore, due to the higher education level of our subjects, it is reasonable to assume that the general population has less knowledge than the findings presented here indicate.
Conclusion
Substantial time and resources are devoted to measuring NCD prevalence, making it clear that rates are increasing and that NCDs disproportionately impact particular groups in society. However, a notable gap exists in understanding public awareness of early-life factors contributing to NCD development. This lack of knowledge hinders our ability to identify potential intervention targets and track shifts in understanding over time, which is crucial as we tackle the NCD crisis in Aotearoa New Zealand.
Our research demonstrates how a simple tool can illuminate gaps in public awareness of DOHaD concepts. This insight can inform strategies for knowledge translation, fostering a broader societal dialogue about early-life environmental exposures. Our findings suggest that a transdisciplinary approach, engaging key stakeholder groups, could amplify DOHaD messaging and strengthen relationships with demographics currently underrepresented in the data.
Finally, our comparison of data collection strategies indicates that carefully implemented mixed approaches could be used to assess the impact of knowledge translation over time, providing a basis for evidence-informed action at the personal, community and societal levels.
Data availability statement
Access to datasets presented in this article will be considered upon written request to the corresponding author.
Acknowledgements
The authors acknowledge the following people who contributed to the development and evolution of the Public Understanding of DOHaD survey tool: Masahito Oyamada, Robyn Dixon, Sarah Morgan, Clare Wall, and Lily Yang. We are also indebted to Deborah Kakis and Amy Renelle for their support with the statistical data analysis.
Author contribution
JLB led development of the Public Understanding of DOHaD Survey and collection of the 2015-16 data; JRH led collection of the 2021-22 data and collated the combined data set used in this study; JRH and JLB analysed the combined dataset; JRH prepared the original draft, both authors contributed to review and editing; both authors have read and agreed to the published version of the manuscript.
Financial support
This work was supported by the Liggins Institute’s Faculty Research Development Fund (3706937) at the University of Auckland. Jillian Hildreth is supported by a University of Auckland Doctoral Scholarship.
Competing interests
None.
Ethical standard
The University of Auckland Human Participants Ethics Committee (UAHPEC; refs. 013093/16008, 23,178) granted ethical approval for the survey tool. All participants grant informed consent (written or oral, depending on the setting) before engaging with the survey. All researchers or assistants working with the data are either named as collaborators in accordance with the ethics process or are required to sign a confidentiality agreement.









