Introduction
Extracorporeal radiotherapy (ECRT) involves the surgical removal of a bone segment containing a tumour, its irradiation outside the body and subsequent re-implantation. This technique is particularly valuable for limb salvage in bone tumours, offering an alternative to amputation or extensive resections, which can significantly impact the patient’s quality of life. Reference Hong, Millington and Ahern1
Intermediate-grade vascular neoplasms of the bone are rare and challenging to treat. Traditional treatments often involve aggressive surgeries, which can lead to substantial morbidity. ECRT has emerged as a promising technique, combining effective oncologic control with limb preservation. This method leverages the high radiation sensitivity of tumour cells while maintaining the structural integrity of the bone, thus allowing re-implantation and functional recovery. Reference Oshima, Yoshida and Hiruma2
Recent studies and case series have documented the success of ECRT in various bone tumours. The technique has shown favourable outcomes in terms of tumour control, functional recovery and complication rates. Reference Krieg, Davidson and Stalley3 This report presents a case of an intermediate-grade vascular neoplasm treated with ECRT, highlighting its potential as an effective limb-salvage strategy.
Case Presentation
A 28-year-old male patient presented with complaints of mass and claudication. MR imaging revealed a lytic lesion measuring 65 × 40 × 91 mm in the distal diaphysis of the right femur. The lesion was destructive and suspected to be malignant. Surgical excision and intraoperative radiotherapy were planned. After surgical excision, extracorporeal radiotherapy was administered, followed by re-implantation of the treated bone (Figure 1). The patient underwent open reduction, plate/screw fixation, deep soft tissue tumour excision and osteotomy. The excised bone structure was immediately re-implanted as a biological graft after radiotherapy. Postoperative histopathological analysis confirmed intermediate-grade vascular neoplasm without angioinvasion or perineural invasion.
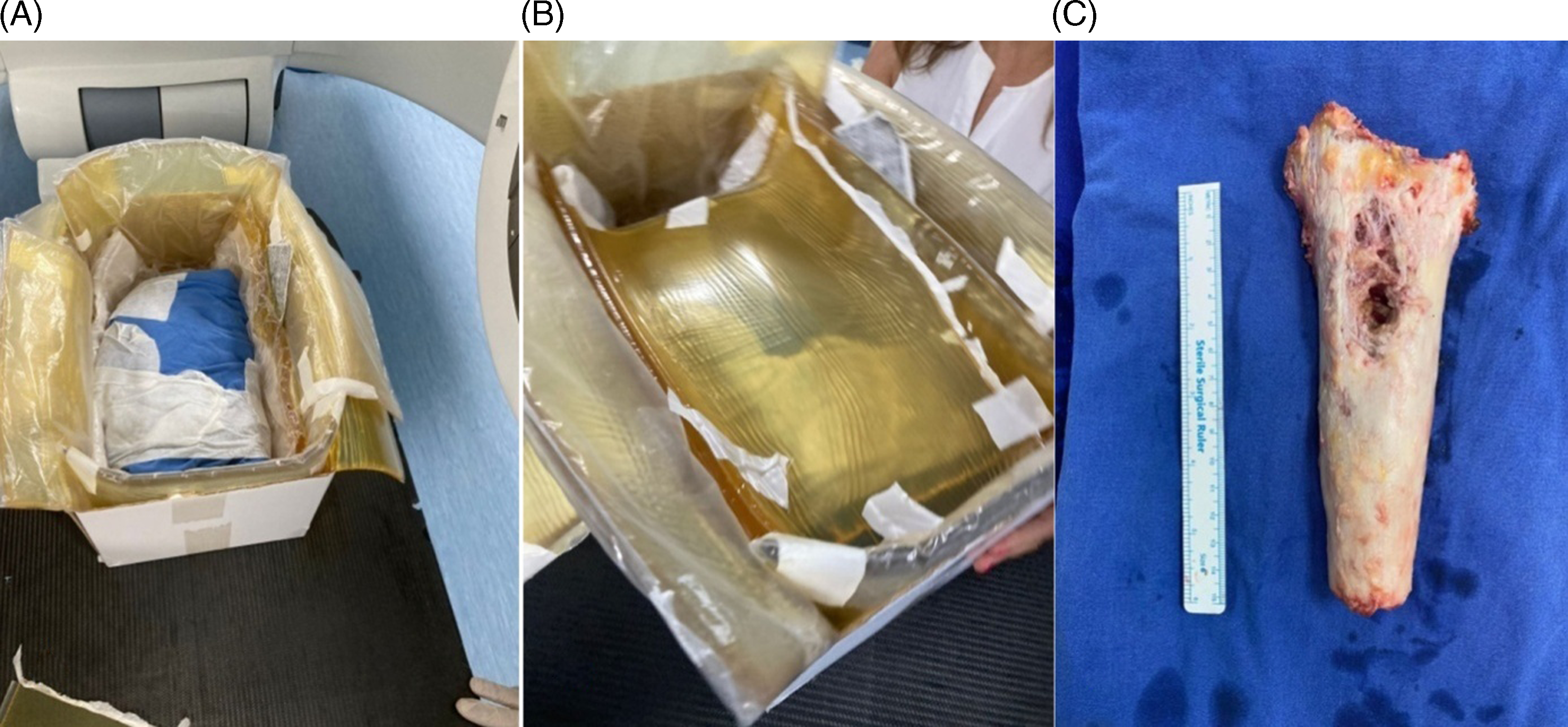
Figure 1. Preoperative and intraoperative images. (A) Preoperative imaging of the right femur for treatment planning system. (B) Setup for extracorporeal irradiation. (C) Intraoperative view of the excised bone segment.
Preoperative Assessment
Preoperative imaging, including computed tomography (CT) and planar X-ray images, confirmed the size and location of the tumour (Figure 2). Patient consent form was obtained. The resected bone segment was planned for extracorporeal radiotherapy to mitigate the risk of local recurrence, regional lymph node involvement and distant metastasis. Reference Nakamura, Abudu and Grimer4
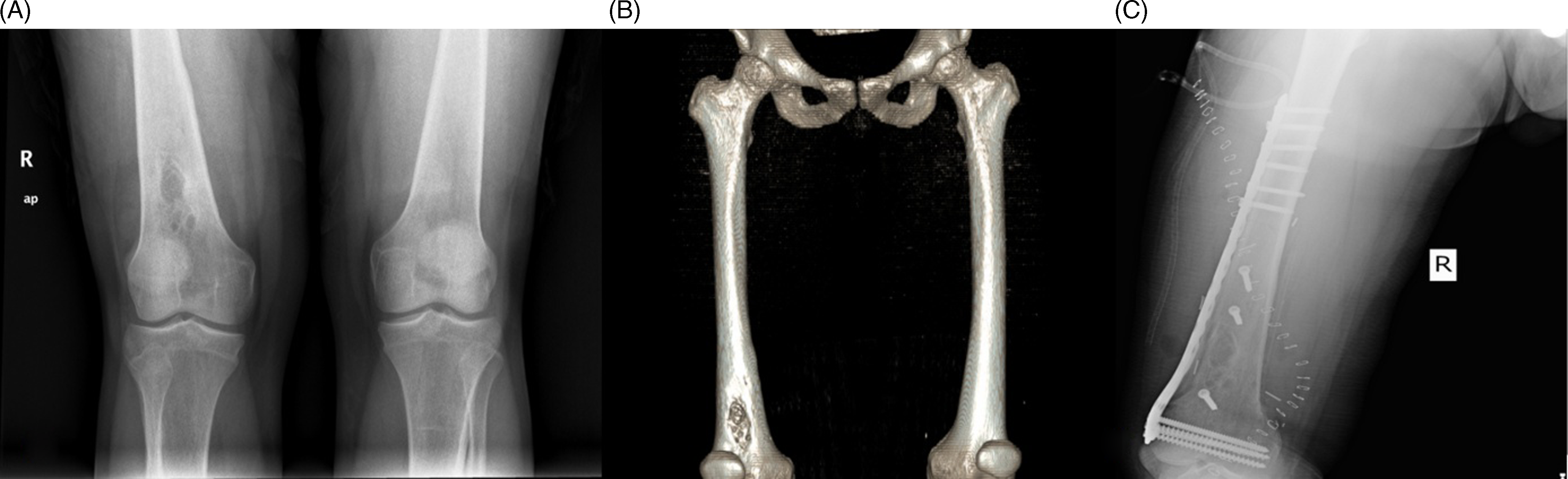
Figure 2. Preoperative CT and X-ray and postoperative images. (A) Preoperative imaging of the right femur showing the extent of the tumour, (B) preoperative CT images of the right femur and (C) postoperative imaging of right femur.
Methods
The bone segment was removed and sterilised. Simulations using Siemens Definition AS CT scanner and Eclipse V13.6 (Varian Medical Systems, Palo Alto USA) treatment planning software were performed to ensure precise radiation delivery. The bone-equivalent material, measuring 25 × 38 cm, was wrapped in a 2 cm bolus and a planning tomography was performed. The bone-equivalent material was contoured as the CTV. A treatment plan was created using a 40 × 40 cm field with 6FFF MV X-ray energy at gantry angles of 270° and 90°. The treatment plan was executed on a Varian Trilogy linear accelerator in a single fraction of 50 Gy (Figure 3).
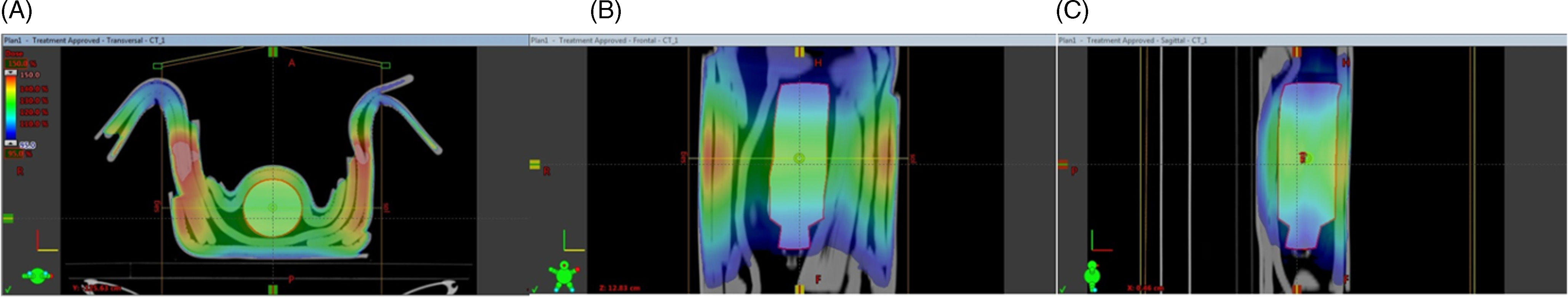
Figure 3. TPS isodose distribution. TPS isodose distribution is observed in (A) transverse, (B) coronal and (C) Sagital planes.
Results
Following irradiation, the bone segment was re-implanted and fixated with metal hardware (Figure 2). Reference Oshima, Yoshida and Hiruma2 Histopathological examination revealed an intermediate-grade vascular neoplasm with no angioinvasion or perineural invasion. Immunohistochemical analysis showed positive reactions for Pansitokeratin, FL1, Vimentin, Cytokeratin-7, D2-40 and CD31, but negative for CD34.
Follow-Up
Follow-up imaging over thirty months showed successful integration of the irradiated bone with no evidence of local recurrence or distant metastasis (Figure 4). The patient experienced a satisfactory recovery with no significant complications. Acute and late side effects were not observed postoperatively or during post-radiotherapy follow-ups. There were no movement restrictions noted upon physical examination.

Figure 4. Follow-up imaging at 4, 12 and 30 months. (A) Follow-up planar X-ray image at 4 months post-operation, (B) follow-up planar X-ray image at 12 months post-operation and (C) follow-up planar X-ray image at 30 months post-operation.
Discussion
ECRT has been successfully used in various bone tumours, demonstrating its effectiveness as a limb-salvage technique. In our case, the procedure provided excellent local control with no recurrence over a thirty-month follow-up period. The irradiation dose of 50 Gy in a single fraction was effective in eradicating the tumour cells while preserving the bone structure. Reference Nakamura, Abudu and Grimer4
Studies have shown that ECRT can achieve similar oncologic outcomes to more radical surgeries, such as amputation, but with significantly better functional results. This technique allows for the preservation of the limb and its function, which is particularly important for young patients with long life expectancies and high functional demands. Reference Tavanaiepour, Broaddus and Chung5
The primary advantage of ECRT is its ability to provide high-dose radiation to the tumour while sparing surrounding healthy tissues. This targeted approach reduces the risk of radiation-induced damage to adjacent structures, which is a significant concern in conventional radiotherapy. Reference Kawaguchi, Ahmed and Matsumoto6
However, the technique is not without challenges. The surgical complexity of removing and re-implanting a bone segment, potential complications such as infection or non-union and the need for specialised equipment and expertise are significant considerations. Reference Gunaseelan, Patro and Lal7 Despite these challenges, the outcomes of our case and others in the literature suggest that ECRT is a viable and effective option for select patients.
Recommendations
Further studies are warranted to standardise protocols, optimise dosimetry and confirm long-term outcomes of ECRT. As more data become available, this technique could become a standard part of the limb-salvage armamentarium for treating bone tumours. Reference Ağaoğlu8
Extracorporeal radiotherapy for intermediate-grade vascular bone neoplasm is a viable limb-salvage technique, providing effective tumour control with acceptable morbidity. Our case demonstrates the potential of ECRT to preserve limb function and ensure oncologic safety. Further research and standardised protocols will enhance the applicability of this technique, potentially making it a preferred option for treating similar bone tumours.
Acknowledgements
We thank the Department of Radiation Oncology at Kocaeli University for their support in this study. This manuscript was presented as a poster presentation at the 15th National Radiation Oncology Congress in Antalya on 06-10/12/2023.
Financial support
None.
Competing interests
None.






