Introduction
Children with life-limiting conditions (LLC) are exposed to frequent hospitalizations. Parents become indispensable supporters of their care, even in a hospital setting. Regardless of their own workload, parents feel that they must be present at all times as the experts and advocates for their child (Brown and Ritchie Reference Brown and Ritchie1990; De Geeter et al. Reference De Geeter, Poppes and Vlaskamp2002). Previous studies on parental experiences show that a hospital stay, especially in an intensive care setting, can be exhausting and burdensome, and that there are several support needs and wishes (Aldridge Reference Aldridge2005; Farrell and Frost Reference Farrell and Frost1992; Hallström et al. Reference Hallström, Runesson and Elander2002). Thus, special structures for children with LLC are recommended (Bösch et al. Reference Bösch, Wager and Zernikow2018). This study aims to identify the burdens and needs of parents of children with LLC in an inpatient setting. Investigating the experiences of parents of terminally ill and hospitalized children can help to better understand their support needs and promote family-centered care. However, so far, little is known about the experiences of inpatient stays from the perspective of parents.
To this end, we interviewed mothers and fathers of children who had been cared for in a dedicated acute pediatric palliative care (PPC) unit about their burdens and needs during hospitalizations, both in the PPC unit and in other pediatric inpatient wards.
Methods
We conducted a descriptive qualitative interview study with parents who have had inpatient experiences with their child with an LLC on our PPC unit, as well as other hospital wards. Our 8-bed PPC unit offers specialized inpatient care and support for children with LLC and their family caregivers. Most families experienced frequent hospital admissions to both the PPC unit and other pediatric wards (e.g., general inpatient unit, pediatric intensive care unit).
Eligible parents were identified through gatekeepers from the Munich PPC Center according to the above-mentioned criteria.
The method and its reporting follow the Consolidated Criteria for Reporting Qualitative Research (COREQ) (Tong et al. Reference Tong, Sainsbury and Craig2007).
Sampling and recruitment
Parents were contacted by the first author. Of the 13 parents approached, 11 agreed to participate in the study (7 mothers, 4 fathers). Two parents refused to participate, one after their child’s death and the other due to a lack of time. Participants were selected through purposeful sampling if their child had at least one inpatient stay on the PPC unit. To learn about parents’ experiences, we aimed for particularly diverse and information-rich cases. The following factors were varied to reach maximum variation: the child’s age, the child’s illness, the parent’s gender, the admission of the child with or without their parents, and the involvement of a specialized pediatric palliative home care team (SPPHC) prior to admission.
Data collection
All participants provided written informed consent. The interview was semi-structured according to Helfferich (Reference Helfferich2005). Four main questions were asked: (1) Can you tell me how your child came to be admitted to the PPC unit? (2) How do you experience everyday life on the PPC unit? (3) What do you feel is good about the PPC unit, and what would you wish for in addition or differently? (4) Do you have experiences with other wards or hospitals? If so, how did you experience the stays there compared to the stay at the PPC unit? Optional supplementary questions were included to obtain more details. At the end of the interview, parents could add further important aspects.
The interview guide was reviewed by a research group with methodological and clinical expertise. Personal interviews were conducted by the first author, S.S., a medical student, from April 2021 to May 2021, partially online via RedConnect, a data-secure and certified provider for video consultations, due to pandemic-related contact restrictions. All interviews were audiotaped and transcribed verbatim. All personal data were irretrievably anonymized, and audio recordings were deleted after study completion. This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The ethics committee of the Munich University Hospital reviewed and approved the study protocol and materials (no. 19–2519).
Data analysis
The interview transcripts were analyzed mainly by S.S. using qualitative content analysis following (Kuckartz Reference Kuckartz2016) and the software MAXQDA2020. Around 20% of the material was double-coded by J.G. to strengthen reliability. First, deductive main codes were developed starting from the research question. After coding all interviews, the codes were reviewed and discussed by the research group (S.S., J.G., K.H., G.D.B., M.F.). Subcodes were then developed inductively for each main code from the data. For each category, content, coding rules, and prototype examples were defined to increase transparency and reliability. The coding scheme and all codings were reviewed by J.G. and discussed in joint analysis sessions. Then, all relevant text passages were coded with the differentiated coding scheme. Finally, a summary-grid-table was developed. Codings and code summaries were evaluated in thematic order. The interview guideline, the coding list, and the summary-grid-tables are available from the first author (S.S.). In order to maintain anonymity, the participants’ informed consent does not allow us to share the complete interviews with third parties.
Results
Of the 13 parents contacted, 11 gave their informed consent and were interviewed. One interviewee was excluded from the analysis because he could not remember enough details of his child’s inpatient stay. The characteristics of the remaining 10 participants are shown in Table 1; all patients received palliative care, and no curative treatments were performed in light of the underlying diseases. Admission to the PPC unit occurred mostly due to refractory symptoms in order to achieve symptom control, and in two cases, for postoperative care in a palliative situation. The interviews took between 21 and 86 minutes.
Table 1. Parent and child characteristics (10 parents of 10 children)
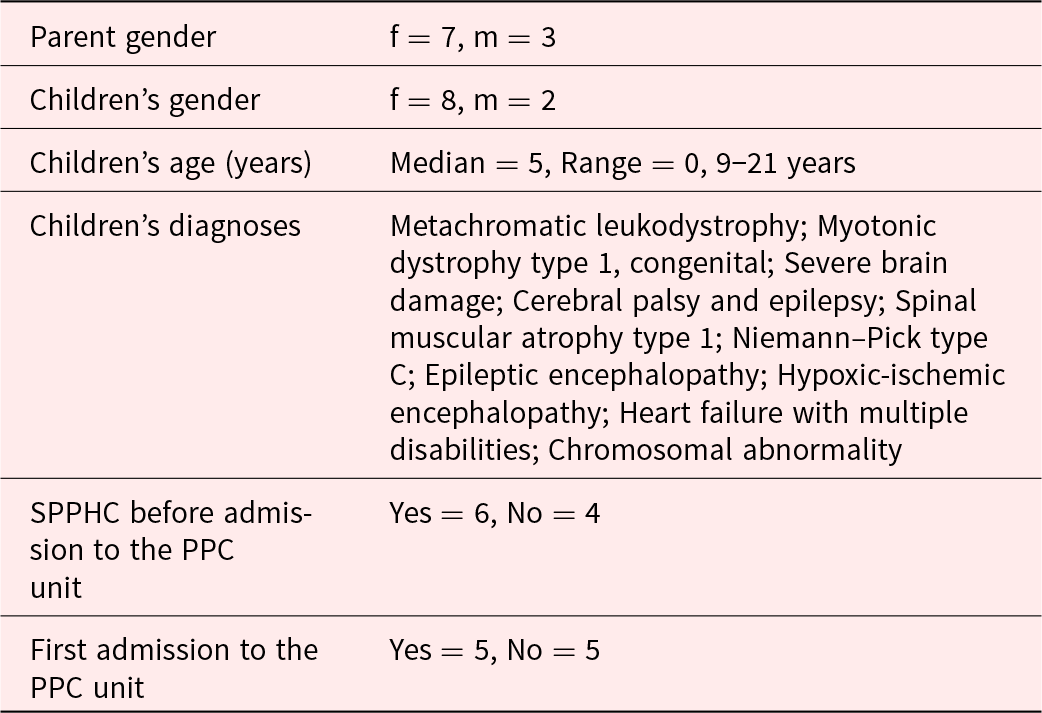
Note: f = female, m = male, Md = median, R = range, PPC = pediatric palliative care, SPPHC = specialized pediatric palliative home care.
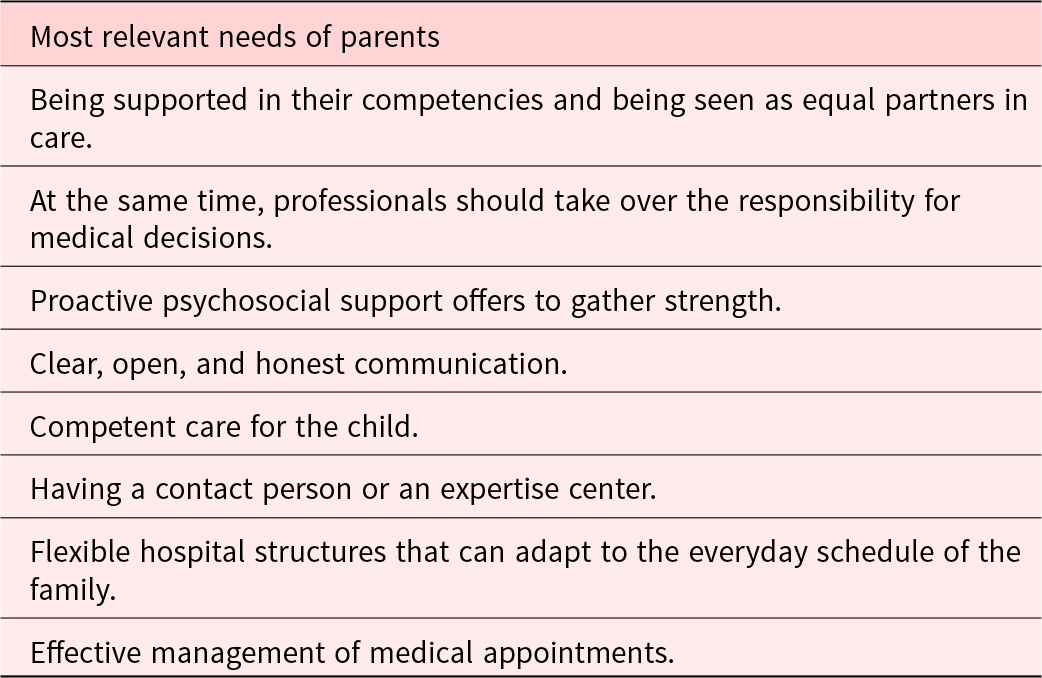
Three major topics were reported by the parents: (1) structural conditions, (2) commitment and competence of professionals, and (3) cooperation between parents and professionals. All parents in our study had experiences on a PPC unit as well as on other hospital wards. They reported a strong contrast between their experiences on the PPC unit compared to other hospital wards. At the end of each quote, we mention whether it refers to a general pediatric ward (GPW), an intensive care unit (ICU), or the PPC unit. Parents’ most relevant needs are shown in Table 2.
Table 2. Parents’ most relevant needs
Structural and organizational conditions
For parents, structural conditions have a great influence on the first impression and the comfort character of a hospital ward.
Constructional characteristics
Noisy and usually illuminated rooms, poor sleeping facilities for parents, and the lack of recreation rooms or parent rooms were strongly criticized. Staying in shared patient rooms was described as very stressful. Parents highly appreciated a more welcoming and familiar environment with single rooms for patients, a parent’s kitchen, a living and playroom, and balconies to get a breath of fresh air. They preferred spacious, family-friendly rooms that did not reflect the hospital atmosphere and therefore made them feel more comfortable.
When special apartments were available for the parents, they really appreciated this possibility to withdraw, to gain distance, to sleep restfully, and to experience longer time-outs while being available if necessary. Parents embraced the possibility to focus on themselves as parents with their own needs.
She [Daughter] was actually quite relaxed, that’s why [we enjoyed] the parents’ kitchen with the play area, where she spent a lot of time in the end. I think she noticed that she was in a hospital, but she still had her own space where she could move around, and it was not quite so hectic, because the palliative care unit is a bit more to the side, so there is not quite such a hospital feeling. (10_V, referring to the PPC unit)
Structural obstacles
Poor scheduling management, short-term rescheduling, as well as long waiting times and inflexible processes, were described as stressful. In addition, the family’s daily routine, which is usually determined by the child’s illness, often could not be maintained due to strict hospital routines. Having to adapt to the hospital structure and still take on many of the tasks of care at the same time was described as stressful. Furthermore, admissions without an accompanying adult were hardly possible in most of the pediatric inpatient wards.
Parents were grateful when they were offered specialist consultations directly on the unit. Thus, many concerns could be met in a structured way and the daily routine was more flexible to meet the needs of the child, which was perceived as a great relief.
It was simply great that all the specialists came to the unit for consultations. That was a huge advantage, and it also gave our child a lot of peace and quiet, so that everything could be clarified on the unit. I actually found that to be the decisive advantage of the whole unit. (04_M, referring to the PPC unit)
Shortage of nursing staff
Parents observed a shortage of nursing staff and, hence, a lack of time for the care of each individual child and even more so for the care of the family. They felt that their child received only medical and nursing care, which was not perceived as sufficient, especially in the context of an LLC. Parents wished for their child to be seen and cared for with age-appropriate needs and developmental tasks despite the illness. Since some parents were used to one-to-one care of their child at home by an outpatient nursing service, they expected the same level of care in the hospital because of their child’s complex care needs. As this was not guaranteed in the hospital, they felt less supported and more stressed than in their domestic care setting.
Non-medical offers
Although parents appreciated the existing possibilities, such as pedagogical offers and additional therapists for the sick child, some still wished for more non-medical support. When the affected child, together with the whole family, was the focus of care, it was perceived as beneficial.
Well, there is the whole multidisciplinary team. It starts with the nurses, even the ward assistant, if I had any need, […], there are also therapeutic possibilities for me, for example, where I can go […], if the nursing care is good enough at that moment, that I can also accept a therapeutic offer. (5_M, referring to the PPC unit)
Commitment and competence of care professionals
From the parents’ reports, the attitude and behavior of the professionals and their commitment in taking care of children and families is a central issue.
Professionals’ commitment
A high commitment to the child’s wellbeing, personal motivation, and empathy, especially among the nurses, were described as key factors affecting parents’ experiences in the hospital. Parents felt relieved and reassured when there was always someone available with time and an open ear, and their concerns were well understood and taken seriously. A caring and supportive attitude of the staff made it easier for parents to deal with and accept existing shortcomings and difficulties. Parents acknowledged that some professionals wanted to support them even more than the existing structures (staffing ratio, available time, etc.) allowed.
I was mostly touched by the commitment, that people are willing to go to such a ward, to work with such a high emotional burden, and still give their best, […] to do something good for the child, to motivate us and to say, hey, this is a difficult phase you are going through, but we will still try to have a nice day with you. (4_M, referring to the PPC unit)
Many professionals, particularly on general wards, were experienced as overburdened – both professionally due to the medical complexity and emotionally in dealing with the severity of the illness and the fate of the family.
Competence
Above all, the high competence of the professionals strengthened parents’ trust in the care team. Parents emphasized that competence in dealing with difficult and burdensome situations was crucial. This was particularly important because most inpatient stays took place during a crisis, possibly in a life-threatening or end-of-life situation, and was always related to the question: Will my child survive this crisis?
When you are admitted to the ward in an acute situation, you are of course very worried as a parent, you never know whether I will now be in a final situation, whether it is now the time, because when I have a child in palliative care, it is always the first thing I think of... (4_M, referring to the PPC unit)
Parents appreciated the availability of a broad spectrum of specialists, both in the inpatient team itself and in the extended team of consultants. The sense of safety and trust in the team enabled parents to hand over parts of their child’s care, including medical responsibility, to the staff. This generated time for “normal parenting.”
Cooperation between parents and professionals
A cooperative partnership as well as respectful and honest communication between parents and professionals were described as being particularly important.
Cooperative partnership
Parents perceive themselves as medical experts for their child and her disease. They therefore appreciate respectful interaction and partnership. They want clinicians to consider their experience and knowledge as important for their child. At the same time, parents wish for guidance as medical lay persons in need of caring for a severely ill child. They want their voice to be heard as part of the decision-making process, but they do not want to be the only decision-makers. They wish to hand over the medical responsibility for their child and the medical decisions to the professionals. When they felt left alone in coming to a decision, they felt insufficiently supported.
Parents know best, you get so tired of that at some point. Of course, it’s nice when you are awarded so much, so much competence, and of course you develop that over the years. But somehow you wish that someone says: and that is what we’re doing now, and that’s it, somehow you just don’t get that at all in the course of the disease, when you have a child with such a rare condition. (01_M, referring to a GPW)
Communication
Parents complain when open and honest communication is missing.
Well, at least [missing communication] worries you immediately, in terms of the situation, how safe you feel and how safe you feel about your child. […] So above all with [the mother] then it had the effect that at some point, […] that you then also doubt the competence of the professionals. And that’s not good, it should really not be like that, because you trust them and in a certain way you depend on them to make you feel safe. (11_V, referring to an ICU)
During inpatient stays, parents often experienced themselves as advocates for their own child against the professionals. They often had to tell the child’s medical story repeatedly, which was perceived as very stressful. Parents criticized the lack of communication and information transfer within hospital teams as well as with specialists from other departments, between hospitals, or with outpatient health care partners. Therefore, parents emphasized the importance and helpfulness of having a multidisciplinary SPPHC team to assist with the transition from an inpatient stay to the home setting.
Discussion
This study explores parents’ needs and experiences when their child with an LLC is admitted to a hospital setting. Some of the parents’ responses are in line with published reports (Aoun et al. Reference Aoun, Gill and Phillips2020; Callery Reference Callery1997; Cramer and Klaus Reference Cramer and Klaus2014; Gill et al. Reference Gill, Hashem and Stegmann2021; Inglin et al. Reference Inglin, Hornung and Bergstraesser2011; Kirk et al. Reference Kirk, Glendinning and Callery2005; Mattsson et al. Reference Mattsson, Arman and Castren2014; Romaniuk et al. Reference Romaniuk, O’Mara and Akhtar-Danesh2014; Seliner et al. Reference Seliner, Latal and Spirig2016; Vasli and Salsali Reference Vasli and Salsali2014). For instance, in our study, as well as in previous studies, parents criticized the architectural structures of hospitals. Severely ill patients and their families prefer single rooms for privacy and a suitable environment for families. Common spaces for exchange with fellow patients and their families and to avoid loneliness are also mentioned as important (Bertuzzi et al. Reference Bertuzzi, Martin and Clarke2023; Curtis and Northcott Reference Curtis and Northcott2017; Engler et al. Reference Engler, Gruber and Engler2020).
Other criticisms of hospital structures and organization, such as the standardized and less individualized care and strict schedules on the wards might be more difficult to meet, as standard procedures and structured processes are a necessary feature of inpatient settings. Graham et al. have shown that parents of chronically ill children describe that their needs “do not fit in the acute care model” (Graham et al. Reference Graham, Pemstein and Curley2009).
Our results show that the care needs of children with complex chronic and life-limiting conditions and their families requires a multiprofessional approach (Verberne et al. Reference Verberne, Schouten-van Meeteren and Bosman2017). Sundal et al. highlighted the need for so-called “home-like care” in the hospital (Sundal Reference Sundal2024; Sundal and Vatne Reference Sundal and Vatne2020). This is particularly true for severe and multiply disabled children, who comprise the majority of children with LLC. Pedagogical and psychosocial support should be made available to these families during inpatient stays (Brenner et al. Reference Brenner, Kidston and Hilliard2018; Cassidy et al. Reference Cassidy, Quirke and Alexander2023).
Taking care of a child with a LLC is a significant challenge for parents. Parents need to become competent healthcare providers and medical experts to care for their child at home (Lazzarin et al. Reference Lazzarin, Schiavon and Brugnaro2018). However, in a hospital setting, they are often still treated as “lay persons” without medical expertise and need to fit into the predefined hospital structures and adapt to hospital rules, while providing a substantial part of the care because of the lack of staff (Rennick et al. Reference Rennick, St-Sauveur and Knox2019). As mentioned in other studies, parents need support in providing and participating in the care of their children and want to be seen as equal partners with exclusive expert knowledge and be respectfully involved in daily care and decision-making processes (Engler et al. Reference Engler, Gruber and Engler2020; Lam et al. Reference Lam, Chang and Morrissey2006; Melo et al. Reference Melo, Ferreira and Lima2014; Seliner et al. Reference Seliner, Latal and Spirig2016). Parents see themselves as advocates for their child and perceive this task as exhausting (Fields et al. Reference Fields, Fraser and Taylor2023). At the same time, parents want to hand over the medical responsibility to the professionals (Hagvall et al. Reference Hagvall, Ehnfors and Anderzén-Carlsson2014). Sharing responsibility for a decision can make the further course of the disease more bearable for parents, as the perceived blame does not rest solely on their own shoulders. This ambivalence in the behavior of parents represents a key result of our study.
Having a child with LLC places an immense burden on the parents – not only in terms of medical care but even more so on an emotional and psychological level, often impacting their own health and well-being (Sevin et al. Reference Sevin, Barth and Wilds2022). Thus, it is crucial to provide support and therapeutic offers not only for the children but for their parents, helping them cope with the emotional challenges and process their child’s illness.
Professionals need to develop an understanding of these partially antagonistic needs of parents to address them in a supportive way. In our study, parents highlighted that their satisfaction with an inpatient stay mainly depended on the attitude of the professionals, which is in agreement with recent reports (Fields et al. Reference Fields, Fraser and Taylor2023; Rico-Mena et al. Reference Rico-Mena, Güeita-Rodríguez and Martino-Alba2023). Especially on general wards, professionals were perceived as overburdened with the complexity of patients with LLC (Seliner et al., Reference Seliner, Wattinger and Spirig2015). Engler et al. have shown that parents sometimes even felt that their chronically ill child was deprioritized against acute cases (Engler et al. Reference Engler, Gruber and Engler2020).
A respectful relationship between professionals and the patients and their families can make challenges in caring for children with LLC more bearable and acceptable (Avis and Reardon Reference Avis and Reardon2008; McIntosh and Runciman Reference McIntosh and Runciman2008). Professionals should try to support burdened parents’ competence through active care and supportive offers. Concepts for general and intensive inpatient care need to include how to support parents with their coping and involve them in the patient’s care according to their needs and wishes (Doupnik et al. Reference Doupnik, Hill and Palakshappa2017; Smith et al. Reference Smith, Swallow and Coyne2015; Ygge and Arnetz Reference Ygge and Arnetz2004). Therefore, an extension of this study is planned involving inpatient nurses and other health care professionals to learn about their views and needs and how new care concepts can be successfully implemented.
This study has several limitations. One is the sample selection through gatekeepers, which could have biased our results. In addition, some of the responses may reflect social desirability. Since all parents in our study had experiences with PPC, our results may not be generalizable to parents of children with LLC without the experience of PPC. As patients with oncological diseases make up only a small part of patients in PPC (Bender et al. Reference Bender, Riester and Borasio2017), no parent of a child suffering from cancer participated in our study. Finally, the monocentric study design limits the generalizability of the results to other health care settings.
To conclude, our data show the complex emotional situation of parents of children with LLC in an inpatient setting. On one side, they justly demand support and respect for their acquired competencies as caregivers and “experts for their child.” On the other hand, they wish for the team to take over responsibility for especially medical decisions and thus ease their emotional burden. Thus, our findings underscore the need for specialized pediatric palliative care teams and structures, especially in tertiary pediatric centers, where most of these patients are cared for. The PPC teams should be available to support the ward teams in meeting the complex care needs and the challenging emotional situations and decision-making processes that arise in the care of children with LLCs and their families (Stoesslein et al. Reference Stoesslein, Gramm and Bender2023).
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S147895152510028X.
Competing interests
This research received no specific grant from any funding agency, commercial or not-for-profit sectors. The authors have no relevant financial or non-financial interests to disclose.




