Highlights
-
• Among patients seen at a Canadian memory clinic, 9.7% reported using cannabis for medicinal, recreational or both medicinal and recreational reasons.
-
• Cannabis users were younger, more likely to have a mood disorder and to be smokers.
-
• More research is needed on how cannabis affects the progression of cognitive disorders.
Introduction
The prevalence of cannabis use has been increasing in the general Canadian population since the legalization of recreational cannabis in October 2018.Reference Hall, Stjepanović, Dawson and Leung1 Among Canadian adults aged 45 years and older, the prevalence of cannabis use steadily increased from 2018 to 2020.Reference Rotermann2 A cross-sectional survey in 2020 found that 8% of Canadians aged 65 and older had used cannabis products in the previous 12 months.3 Concurrently, the absolute and relative number of individuals aged 65 and older has also been increasing.4 With an aging population, dementia and other forms of cognitive impairment are becoming increasingly important public health concerns. In 2016, an estimated 564,000 Canadians were living with dementia, and this number is predicted to rise to 937,000 by 2031.Reference Chambers, Bancej and McDowell5
In October 2018, the commercial sale of cannabis for recreational purposes became legal in Canada. The production and sale of cannabis products is regulated by Health Canada, which licenses producers and sellers. Health Canada mandates a maximum tetrahydrocannabinol (THC) content and requires manufacturers to label their products with the amount of THC and cannabidiol.
However, even before legalization, societal perspectives were shifting toward increased acceptance of cannabis use.Reference Black and Joseph6 Individuals who had previously used cannabis as young adults were more accepting of it as they aged, compared to previous generations.Reference Lloyd and Striley7 Among Canadian older adults, legalization further shifted beliefs about cannabis and played a major role in de-stigmatizing its medicinal use, although recreational use still carried more stigma.Reference Baumbusch and Sloan Yip8 A qualitative study found that older Canadian adults who began using cannabis were likely motivated by its perceived medicinal benefits.Reference Baumbusch and Sloan Yip9 Most older adults see the use of cannabis for medical purposes as acceptable, while viewing recreational use as risky.Reference Arora, Qualls and Bobitt10 Favorability toward recreational cannabis use appeared to decrease with older age.Reference Arora, Qualls and Bobitt10 Cannabis use among older populations has been linked to specific demographic and health factors, including being male, not married, having multiple chronic diseases, experiencing psychological stress and using other substances such as alcohol, tobacco, recreational drugs and prescription drugs.Reference Lloyd and Striley7 The increasing rate of cannabis use among older adults can be attributed to greater exposure and acceptance of cannabis, as well as the rise in its availability and accessibility following legalization.Reference Black and Joseph6
Cannabis has some medicinal properties that may make it attractive to patients with cognitive disorders and their caregivers. Cannabis and derivative cannabinoids have shown some promise in treating the behavioral and neuropsychiatric symptoms of dementia such as agitation and aggression.Reference Walther, Schüpbach, Seifritz, Homan and Strik11–Reference Herrmann, Ruthirakuhan and Gallagher14 Older adults without dementia who began using cannabis after the age of 60 often used it for medicinal purposes, including managing pain, sleep, anxiety and depression. Medical cannabis has been associated with self-reported positive effects on sleep, pain and mood symptoms among older dementia-free users in Canada.Reference Tumati, Lanctôt, Wang, Li, Davis and Herrmann15 Additionally, cannabis may have neuroprotective anti-inflammatory effectsReference Watt and Karl16,Reference Ehrhart, Obregon and Mori17 and has been associated with a reduction in beta-amyloid production and tau phosphorylation in in vitro and animal studies.Reference Aso, Juvés, Maldonado and Ferrer18,Reference Ferrer19 Consequently, some caregivers are turning to cannabis as a means to address emotional and sleep-related challenges in patients with dementia.Reference Kaskie, Bobitt and Herrera20
However, cannabis use among older adults with cognitive impairment carries risks and uncertainties. Regardless of frequency and amount, cannabis use is a risk factor for injury and has been associated with an increased rate of emergency department visits among older adults aged 50 and older, even when accounting for other potential risk factors.Reference Choi, Marti, DiNitto and Choi21 There is also the risk of negative acute and chronic health consequences and adverse effects from interactions with prescribed medications.Reference Han and Moore22 The data on efficacy are also inconsistent; for example, a crossover randomized controlled trial found that low-dose oral THC did not significantly reduce neuropsychiatric symptoms compared to placebo.Reference van den Elsen, Ahmed, Verkes, Feuth, van der Marck and Olde Rikkert13 Moreover, there is limited high-quality evidence, with the overall quality of studies often rated as low.Reference Bahji, Meyyappan and Hawken23 There is still a need for more robust, large-scale randomized controlled trials to establish definitive efficacy and optimal dosing. The literature underscores the evolving landscape of cannabis use in older demographics and the need for further understanding of cannabis use among patients with cognitive disorders.
Because there are few data on the prevalence and characteristics of cannabis use among older adults with cognitive complaints, we conducted an exploratory study to investigate the prevalence and correlates of cannabis use in patients attending a Canadian specialty cognitive assessment clinic. With the legalization of cannabis and changing patterns of use, understanding the prevalence and correlates of cannabis use is important to ensuring clinicians are prepared to detect and provide informed advice to both patients with cognitive concerns and their caregivers about the use of cannabis products.
Methods
Participants
This study was based on analysis of data collected from participants enrolled in the PROspective Registry of Persons with Memory SyMPToms (PROMPT). PROMPT was established in July 2010 and compiles data on patients who have been evaluated at the Cognitive Neurosciences Clinic, which is located at two urban tertiary care centers in Calgary, Alberta, Canada. Patients are referred to this clinic by a primary care provider or specialist physician and assessed for cognitive concerns (e.g., possible dementia) by a psychiatrist or cognitive neurologist. Participants included in this study attended the Cognitive Neurosciences Clinics from February 11, 2019, to May 3, 2023.
Ethics
Informed consent was obtained from all participants. This study was approved by the Conjoint Human Research Ethics Board at the University of Calgary (REB15-0992).
Data collection
Participants’ information on age and sex was collected as part of the general medical history. Other data were captured by their healthcare provider on a standardized initial visit form (see Appendix). These data included race, highest level of education, smoking status, frequency of alcohol use, cognitive diagnosis (SCD, MCI, dementia, other) determined at the clinic, cannabis use characteristics (no use, recreational use, medicinal use), history of stroke, obstructive sleep apnea (OSA), insomnia, psychiatric diseases (i.e., mood disorder, anxiety disorder, psychotic disorders), Montreal Cognitive Assessment (MoCA) scores, Mini-Mental State Examination (MMSE) scores and agitation (based on a positive response to this question from the Mild Behavioral Impairment Checklist: “has the person become agitated, aggressive, irritable or temperamental?”).Reference Creese, Griffiths and Brooker24 Cannabis use was defined as the ingestion or smoking of any part of the cannabis plant or its derivatives and was subtyped according to the participant’s understanding of whether the product included CBD only or included THC, with or without CBD. Medicinal use of cannabis was classified as use to treat medical symptoms, as reported by the patient. Clinic physicians did not direct patients to take cannabis for medicinal reasons or prescribe synthetic cannabinoids and provided advice regarding the use of cannabis according to their clinical judgment. SCD refers to a self-perceived decline in cognition that does not require confirmation by an informant and in which there is no objective evidence of impairment by cognitive testing.Reference Jessen, Amariglio and van Boxtel25 MCI is an at-risk state for dementia where a person shows cognitive decline based on both cognitive tests and concerns from the individual, an informant or clinician, but these deficits do not interfere with independence in activities of daily living.Reference Lopez-Anton, Santabárbara and De-la-Cámara26 Dementia refers to a level of cognitive decline where independent daily function is impaired.Reference Foster, Herring and Doron27 “Other” cognitive diagnoses include psychiatric disorders, neurodevelopmental disorders and normal cognition, which were determined by the healthcare provider. Information on dose, frequency and method of cannabis consumption was not captured.
Statistical analysis
Patients were categorized as recreational cannabis use, medicinal cannabis use or both based on whether “yes” was marked as a response for “recreational marijuana” or “medicinal cannabis” use or whether cannabis use was written in the “other abused substances” section of the intake form. Among medicinal users, information was collected on the type of cannabis, being CBD or THC. Characteristics were compared between current cannabis users and non-users using the two-sample t-test or chi-squared test as appropriate. Due to relatively low numbers, recreational and medicinal users were combined for analyses where users and non-users were compared. Because of insufficient numbers of cannabis users, multivariable analysis was not performed. Participants with missing data were excluded from analyses. Statistical analyses were performed with the software R. A p-value of < 0.05 was considered significant. This exploratory pilot study did not correct for multiple comparisons.
Results
Among 438 participants enrolled in the PROMPT registry during the study period, 200 were excluded because of missing cannabis use information (n = 199) or missing sex information (n = 1). Reasons for missing cannabis use information were not recorded but were likely due to patients not being asked, refusing to answer the question, or being unsure of their cannabis use status. Characteristics of excluded and included patients are shown in Table 1. Participants included in the study were more likely to be older and have a history of current or former smoking, alcohol use, insomnia, OSA, mood disorders, anxiety disorders, stroke and agitation. There was a significant difference in the distribution of cognitive diagnoses between the two groups, with a higher prevalence of dementia, MCI and SCD among included participants and a higher prevalence of other cognitive diagnoses (including psychiatric disorders, neurodevelopmental disorders and normal cognition) among those excluded. There were no significant differences in sex, race, education, psychotic disorders, MoCA or MMSE.
Table 1. Characteristics comparing excluded participants to included participants
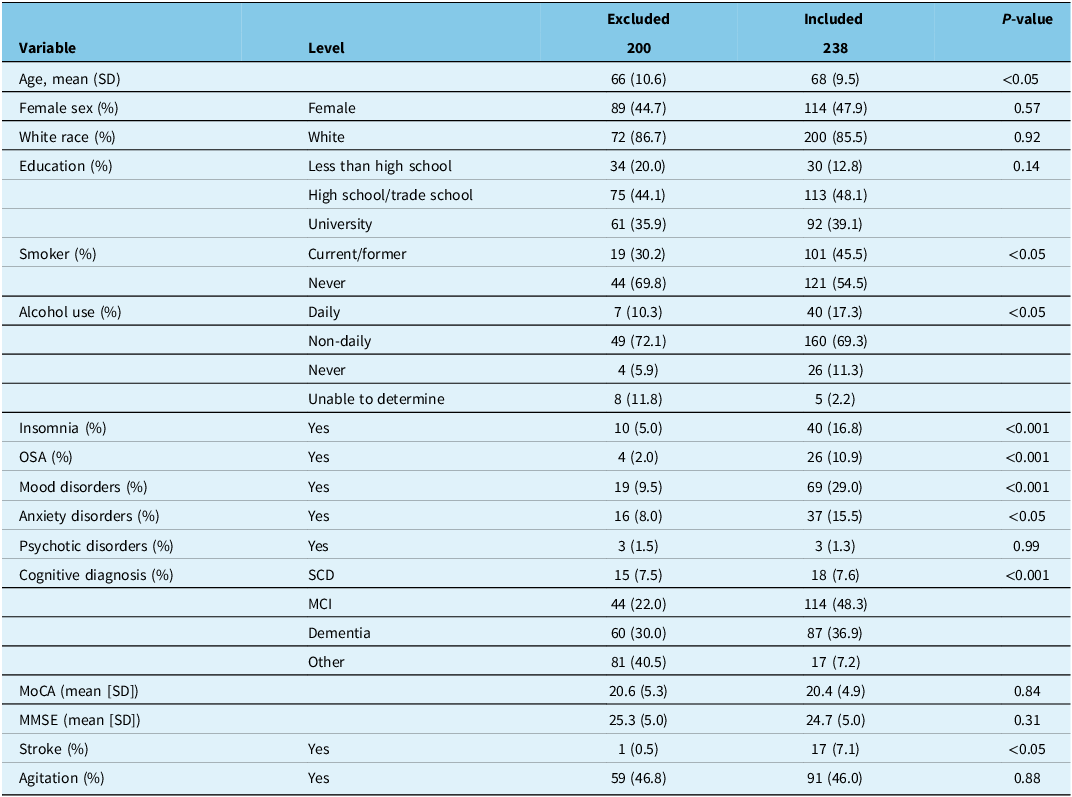
Note: Data were missing on sex for 1 patient, race for 121 patients, education level for 33, smoking status for 153, alcohol use for 139, cognitive diagnoses for 2 and agitation for 114. “Other” cognitive diagnoses include psychiatric disorders, neurodevelopmental disorders and normal cognition. OSA = obstructive sleep apnea; MCI = mild cognitive impairment; SCD = subjective cognitive decline; MoCA = Montreal Cognitive Assessment; MMSE = Mini-Mental State Examination.
Among patients with recorded cannabis information, 23 out of 238 (9.7%; 95% CI 6–14%) reported using cannabis (Table 2). No patients were taking prescription or illegal synthetic cannabinoids. Cannabis was more commonly used for recreational than medicinal purposes: 12 took cannabis for recreation, 8 for medicinal purposes and 3 for both recreational and medicinal purposes. Among those using for medicinal purposes, half used CBD, and half used THC products. Those who reported cannabis use were younger (mean age of non-users 68.87 [SD = 9.49] vs 62.00 [SD = 7.51] for users; p = 0.001), more likely to have reported a diagnosis of a mood disorder (56.5% vs 26%, p < 0.05) and more likely to be former or current cigarette smokers (73.7% vs 42.9%, p < 0.05). Comparing those that do and do not use cannabis, there were no significant differences in sex, race, education, alcohol use, insomnia, OSA, anxiety disorders, psychotic disorders, cognitive diagnosis, MoCA, MMSE, stroke or agitation.
Table 2. Characteristics of all participants categorized as cannabis users (n = 23) and non-users (n = 215)
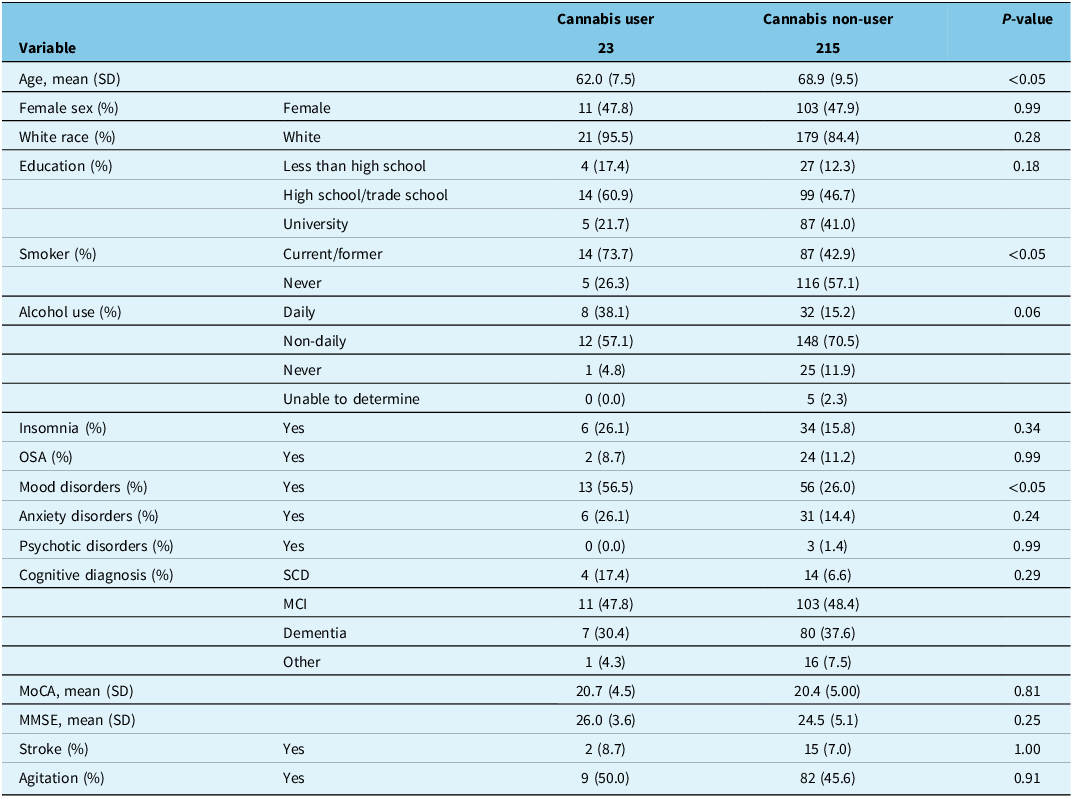
Note: Data were missing on race for 4 patients, education for 3 patients, smoking status for 16, alcohol use for 7, cognitive diagnosis for 2 and agitation for 40. “Other” cognitive diagnoses include psychiatric disorders, neurodevelopmental disorders and normal cognition. OSA = obstructive sleep apnea; MCI = mild cognitive impairment; SCD = subjective cognitive decline; MoCA = Montreal Cognitive Assessment; MMSE = Mini-Mental State Examination.
Discussion
In this exploratory study of older adults attending a Canadian cognitive assessment clinic, approximately 1 in 10 patients with information collected on cannabis use status reported using cannabis. This is similar to general population data showing 8% of Canadians aged 65 and older used cannabis products in 20203, which is higher than the 2.9% prevalence observed in older Americans.Reference Maxwell, Jesdale and Lapane28
There are few data on the use of legal, recreational or medicinal use of cannabis among community-dwelling persons living with cognitive disorders or dementia. In a focus group study conducted in Los Angeles, USA, in 2019, at which time cannabis use was legal in California for medicinal and recreational use, 3 out of 26 caregivers indicated that they provided cannabis to a person with dementia.Reference Kaskie, Bobitt and Herrera20 However, systematic surveys of clinic patients or persons with cognitive disorders in the general population are lacking.
Two-thirds of those who used cannabis in our study reported recreational use, contrasting with previous studies where older adults typically framed their cannabis use as medicinal.Reference Baumbusch and Sloan Yip8 Factors contributing to cannabis use in this demographic may include the positive effects of cannabis on reducing agitation and aggression in those with dementia as well as its broader benefits for sleep, pain and mood symptoms.Reference Walther, Schüpbach, Seifritz, Homan and Strik11,Reference Herrmann, Ruthirakuhan and Gallagher14,Reference Kaskie, Bobitt and Herrera20,Reference Outen, Burhanullah and Vandrey29,Reference Liu, Chau, Ruthirakuhan, Lanctôt and Herrmann30 This may also reflect societal trends toward greater acceptance of recreational cannabis use.Reference Lau, Sales, Averill, Murphy, Sato and Murphy31 This underscores the relevance of investigating the factors contributing to the sustained use of cannabis in this age group, particularly within the context of cognitive concerns.
We found that certain characteristics distinguished cannabis users from non-users. Cannabis users were younger, which reflects a generational shift in the acceptance of cannabis use.Reference Lloyd and Striley7 Cannabis users were also more likely to be former or current cigarette smokers, which corresponds with smoking being a risk factor for cannabis use and vice versa.Reference Weinberger, Wyka and Goodwin32 Cannabis use is associated with increased initiation of cigarette smoking, less smoking cessation and higher risk of smoking relapse.Reference Weinberger, Delnevo and Wyka33 The mechanisms underlying this association involve nicotine and cannabis both acting on the brain’s reward system, potentially making individuals who smoke cigarettes more susceptible to using cannabis.Reference Martin-Soelch, Kobel and Stoecklin34
The higher prevalence of mood disorders (56.5% vs 26%, p < 0.05) among those who reported cannabis use in our study raises questions about the potential bidirectional relationship between cannabis use and mood disorders in older adults. Although our cross-sectional study does not allow for causal inferences, this finding suggests that cannabis could either be used as a form of self-medication for mood symptoms or be a contributing factor to the development or exacerbation of mood disorders through various biological and psychosocial pathways.Reference Khantzian35,Reference Karila, Roux and Rolland36 A systematic review by Sourkhou et al. found that cannabis use is associated with increased depressive and manic symptoms, as well as a higher likelihood of developing major depressive disorder and bipolar disorder.Reference Sorkhou, Dent and George37 Cannabis use was linked to an unfavorable prognosis in both mood disorders, suggesting a negative influence on the course and outcomes of these disorders.Reference Sorkhou, Dent and George37 Kuhns et al. report a bidirectional relationship between cannabis use and the onset of depression, with worse prognoses for both depression and bipolar disorder, including a higher risk of suicidality.Reference Kuhns, Kroon, Colyer-Patel and Cousijn38 Evidence suggests an association between mood disorders and cannabis use across different age groups.Reference Mann, Cheung and Stoduto39 This prompts the need for longitudinal research to elucidate the temporal dynamics of this relationship, specifically within the demographic of older adults with cognitive impairments, as this could have implications for mental health interventions and screening strategies.
Multiple small clinical trials have explored the use of medical cannabisReference Peprah and McCormack40 or synthetic cannabinoids (drugs that stimulate cannabis receptors)Reference Bahji, Meyyappan and Hawken23 for the treatment of neuropsychiatric symptoms of dementia, including agitation. However, when interpreting results of cannabinoid research, it is important to recognize that there are chemical differences between phytocannabinoids (derived from the cannabis plant), endocannabinoids (endogenously produced metabolites that have activity on cannabinoid CB1 and CB2 receptors)Reference Lu and Mackie41 and synthetic cannabinoids (chemically synthesized derivatives of cannabinoids for prescription or illegal use) that may affect their medicinal properties. Canadian guidelines for medical management of dementia do not address cannabis use,Reference Ismail, Black and Camicioli42 while Canadian guidelines for managing behavioral and psychiatric symptoms of dementia recommend the use of nabilone (a synthetic cannabinoid) for the treatment of refractory agitation with low-quality evidence, without addressing the use of phytocannabinoids.Reference Hatch, Seitz and Bruneau43
The impact of cannabis on cognition is controversial. A systematic review of cannabis use in older adults found that, while conclusions were limited by variability in the products used and quality of the research methods, modest reductions in cognitive performance were seen in users taking higher doses and among those with heavier lifetime use.Reference Scott, Brennan and Benitez44 On the other hand, cannabis has been reported to reduce neuroinflammation and prevent aggregation of amyloid and tau in preclinical studiesReference Watt and Karl16–Reference Ferrer19 and therefore might reduce the rate of cognitive decline in Alzheimer’s disease. However, this hypothesis has not been tested in adequately powered clinical trials. Instead, most trials have tested the effects of cannabis on neuropsychiatric symptoms, and surprisingly, most of them did not report the effects on cognitive test scores. A systematic reviewReference Scott, Brennan and Benitez44 found evidence from only two small (50 or fewer subjects each) randomized controlled trials: one trial found no effect of THC on episodic memory,Reference van den Elsen, Ahmed and Verkes12 but another found that the synthetic cannabinoid nabilone improved MMSE over 6 weeks of treatment.Reference Herrmann, Ruthirakuhan and Gallagher14
A limitation of this study is that many patients did not have their cannabis use status collected. Participants with cannabis information were more likely to be older and have a history of current or former smoking, alcohol use, insomnia, OSA, mood disorders, anxiety disorders, stroke and agitation (Table 1). Participants included also had a higher prevalence of dementia, MCI and SCD, whereas those excluded had a higher prevalence of other cognitive diagnoses, including psychiatric disorders, neurodevelopmental disorders and normal cognition. The higher prevalence of these conditions among included participants may indicate an underlying bias in data collection, where clinicians might have been more diligent in questioning patients on cannabis use if they presented with more complex health profiles and more pronounced health issues. Patients and family members may have also underreported cannabis use due to stigma or concerns about provider perceptions, leading to an underestimation of cannabis use. The limited sample size results in an underpowered study, and these findings need confirmation through future larger studies. However, even if all patients with missing cannabis information were non-users, the prevalence of use (∼5%) would still be appreciable, indicating that clinicians should systematically ascertain cannabis use in all patients attending a cognitive assessment clinic.
Additional limitations of our study that impact the interpretation and generalizability of the findings should be considered. First, our data collection form only accounts for participants who currently use cannabis and does not account for those who may have used cannabis in the past. Additionally, among current users, we did not collect information on dosing and method of cannabis consumption. Due to the limited sample size, we could not perform multivariable logistic regression to identify characteristics independently associated with cannabis use. Additionally, the duration of cognitive symptoms and cannabis use is unclear, leaving open the question of whether cannabis contributes to cognitive decline and presentation to the memory clinic or whether it is used to manage symptoms associated with cognitive decline.
These limitations underscore the need for larger longitudinal studies with prospectively collected data on cannabis use. These studies should collect information on lifetime as well as current use, the reasons for use including symptoms that prompted use, whether the decision to use cannabis was made by the person affected by the cognitive disorder or by their care partner and symptoms of dependence or abuse. Determining the exposure to THC and CBD is very complex due to the variety of products available in Canada, which may include solid concentrates, hash, dried flower, edibles, vape oils, tinctures, topicals, oral oils in capsules, oral oils in drops and drinks.Reference Wadsworth, Rynard and Driezen45 While Health Canada requires product labels that report the quantity of THC and CBD, the accuracy of these labels has been called into question, as the products are not manufactured to drug grade. For example, one study found that 40% of cannabis products in Ontario had assayed levels of THC that were outside variability limitsReference Doggett, Fein, Campbell, Henriquez, Busse and MacKillop46; most commonly, the product was labeled as being more potent than it actually was.
Overall, this exploratory study provides preliminary insights into cannabis use among older adults in Canada with concerns or diagnoses of cognitive impairment, revealing that a notable 10% use cannabis, primarily for recreational purposes. This underscores the importance of regularly screening for cannabis use to minimize potential adverse effects from interactions with other medications or other side effects, such as dizziness or falling.Reference Bertram, Porath and Seitz47 As societal attitudes toward cannabis evolve and its accessibility increases, understanding its effects on older adults with cognitive disorders becomes increasingly critical. Future research should aim to include larger sample sizes and longitudinal designs to confirm these preliminary findings and should investigate patients’ motivations for use, the relationship of cannabis use with mood disorders and the role of cannabis in cognitive decline. Understanding these dynamics is important for healthcare providers to offer informed guidance and support to older adults with cognitive concerns who use or are considering using cannabis.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cjn.2025.64.
Acknowledgments
The PROMPT registry is supported by funding from the Katthy Taylor Chair of the University of Calgary.
Author contributions
Individual author contributions are listed below:
YYY: Designed the study, performed statistical analyses, interpreted the data and wrote the first draft of the manuscript.
CM: Critically reviewed and revised the manuscript.
DPS: Critically reviewed and revised the manuscript.
ZI: Critically reviewed and revised the manuscript.
DBH: Critically reviewed and revised the manuscript.
EES: Supervised the study design and analysis, obtained funding, critically reviewed and revised the manuscript.
Funding statement
None.
Competing interests
Yvette Ysabel Yao reports no disclosures. Colleen Maxwell reports no disclosures. Zahinoor Ismail reports serving as a consultant for CADTH, Eisai, Eli Lilly, Lundbeck/Otsuka, Novo Nordisk and Roche. Kimberly G. Williams reports funding from the Calgary Parkinson’s Research Initiative, honoraria from Scotia Bank and leadership roles in the Federation of Medical Women of Canada and Canadian Medial Forum. Karyn Fischer reports no disclosures. David B. Hogan reports no disclosures. Dallas P. Seitz has received funding through the University Health Foundation – Alberta Roche Collaboration in Health research grant competition and a leadership role as the Scientific Director of Recovery Alberta. Eric E. Smith reports no disclosures.




Target article
Cannabis Use Prevalence and Correlates in Patients Attending a Canadian Cognitive Clinic
Related commentaries (2)
Reviewer Comment on Yao et al. “Cannabis Use Prevalence and Correlates in Patients Attending a Canadian Cognitive Clinic”
Reviewer Comment on Yao et al. “Cannabis Use Prevalence and Correlates in Patients Attending a Canadian Cognitive Clinic”