Introduction
Tonsillectomy is a common ENT procedure for children and adults. Performing tonsillectomies as same-day surgeries has the potential to save significant hospital resources incurred with overnight hospital admissions. Surveying patients and carers has shown that they prefer day-surgery tonsillectomy,Reference Bain, Kelly, Snadden and Staines1 as it allows them to recuperate in a comfortable and familiar home environment.
It is ideal to identify the appropriate patient groups to receive day-surgery tonsillectomy pre-operatively.Reference Abdullah and Chung2 The University Hospital Geelong, Australia, found that patients over the age of two years old, with American Society of Anaesthesia score of 2 or less, undergoing tonsillectomy for breathing obstruction experienced fewer post-operative complications than other tonsillectomy patients and were appropriate candidates for day surgery.Reference Morris, Hassin and Borschmann3 Other centres include factors such as severity of obstructive sleep apnoea,Reference Cooper, Ford and Bajaj4 body mass index (BMI), end tidal CO2 levelReference Hamilton, Thung, Tobias, Jatana and Raman5 and distance from hospitalReference Hanss, Nowak, Decaux, Penon and Bobin6 in their patient selection criteria for day-surgery tonsillectomy.
A survey of ENT surgeons in 2008 demonstrated that fewer than one-quarter of Australian ENT surgeons performed day-surgery tonsillectomies.Reference Macfarlane, Nasser, Coman, Kiss, Harris and Carney7 The main reasons for the reluctance of ENT surgeons to perform day-surgery tonsillectomies are (1) concerns about the risk of primary post-tonsillectomy haemorrhage and being able to promptly treat patients when this occurs, (2) treating post-operative pain and (3) treating post-operative nausea and vomiting.Reference Stocker8
Readmission post tonsillectomy is costly for hospitals and inconvenient for patients and carers. Common reasons for readmission include post-tonsillectomy haemorrhage, reduced oral intake, pain and nausea and vomiting.Reference Hession-Laband, Melvin, Shermont, Murphy, Bukoye and Amin9
A serious complication of tonsillectomy is haemorrhage, which can be life threatening.Reference Windfuhr, Schloendorff, Baburi and Kremer10 A 2022 review of post-tonsillectomy haemorrhage morbidity in Australian hospitals found an overall return-to-theatre rate (repeat operation to control post-tonsillectomy haemorrhage) of 1.6 per cent. Internationally, reported return-to-theatre rates ranged between 0.3 per cent in Taiwan and 6.0 per cent in Germany.Reference Li, Forer and Veivers11
Study aims
Given the low uptake of day-surgery tonsillectomy in Australia,Reference Macfarlane, Nasser, Coman, Kiss, Harris and Carney7 the aim of this study is to assess the safety and feasibility of same-day discharge for elective tonsillectomy patients. The primary outcome is readmission rate within 24 hours, and the secondary outcome is post-tonsillectomy haemorrhage rate.
Materials and methods
Study methods were informed by the Standards for Quality Improvement Reporting Excellence (SQuIRE) guidelines.Reference Kelz, Schwartz and Haut12
Ethical considerations
The Southern Adelaide Local Health Network Human Research Ethics Committee granted exemption (4808) on the basis that de-identified data were used as this was assessed as a quality-improvement project.
Context
The retrospective surgery series included all patients who underwent tonsillectomy at the Southern Adelaide Local Health Network in Australia from January 2018 to May 2023. Tonsillectomies are performed at two sites in the network: Flinders Medical Centre and Noarlunga Hospital.
The current Southern Adelaide Local Health Network day-surgery tonsillectomy protocol was instituted in 2017. Eligible patients for day-case tonsillectomy are over the age of 4 years, live within 15 km of a tertiary hospital, and the patients or carers have access to a telephone and car. The indications for a tonsillectomy are generally infective, sleep-disordered breathing, for asymmetrical tonsils. Patients under the age of two years of age or under 12 kg are not suitable for Southern Adelaide Local Health Network and referred to the state’s quaternary children’s hospital for their surgery. Other criteria in the protocol that precludes patients from day-surgery tonsillectomy are documented obstructive sleep apnoea (OSA), failure to thrive (weight < 5th centile for age), severe cerebral palsy, neuromuscular or craniofacial anomalies, mucopolysaccharidosis, American Society of Anaesthesia score of 3 or above, congenital heart disease or BMI > 99th centile for their age. Hence, day-surgery patients were generally healthy and had American Society of Anaesthesia scores of 1 or 2 for the Southern Adelaide Local Health Network tonsillectomy protocol. Patients who were not suitable for day-surgery tonsillectomy were monitored in hospital with oximetry (continuous monitoring for paediatric patients) and routine post-operative ward observations, as per the protocol.
Study design
The list of patients who underwent tonsillectomy during the study period was retrieved from the hospital’s communication auditing reporting tool database. Trainee medical officers identified complications contemporaneously by searching hospital records for post-tonsillectomy haemorrhage-related presentations or admissions to South Australian hospitals. The Stammberger post-tonsillectomy haemorrhage grade was recorded as part of the patient’s assessment. The investigators sourced supplementary information about surgical treatment by a search of the patients’ electronic records. Routine follow up was a phone call six weeks post-operatively to the patient or parent of a paediatric patient.
Participants
Inclusion and exclusion criteria
Inclusion criteria were (1) elective tonsillectomy via any method and by any level of surgeon (resident, registrar, fellow or consultant), with the surgery performed at Southern Adelaide Local Health Network, and (2) combined tonsillectomy with other ENT procedures (for example adenoidectomy or turbinate reduction). Concurrent tympanostomy tube insertion was not considered an additional procedure due to the unlikelihood of tube insertion complicating the two-week post-operative recovery from tonsillectomy.Reference Yaman, Yilmaz, Alkan, Subasi, Guclu and Ozturk13
Patients identified by the communication auditing reporting tool complication database who underwent tonsillectomy by a surgeon in a non-Southern Adelaide Local Health Network hospital, or an emergency tonsillectomy for uncontrolled infection were excluded.
Measures
The primary outcome was readmission within 24 hours of discharge. The secondary outcome was primary and secondary post-tonsillectomy haemorrhage rates. The comparison groups were “Day surgery”, being discharged the same day of surgery, and “Hospital stay”, discharging after one or more nights spent in hospital post-operatively.
Analysis
Data are presented as count (n) and percentage. A chi-square test was used for statistical analysis of heterogeneity between the day-surgery and hospital-stay groups.
Results
During the study period, 1658 patients underwent tonsillectomy at Southern Adelaide Local Health Network (Table 1), of which 584 (35 per cent) patients were under 6 years old, 428 (26 per cent) were between ages 6 and 17 years old inclusive and 646 (39 per cent) were <18 years old. Overall, there were 664 patients in the day-surgery group, and 994 patients in the hospital-stay group. 30 per cent (199) of day-surgery patients were paediatric (under 18 years old), compared to 82 per cent (813) of the hospital-stay patients. Of the hospital-stay patients, 936 patients (94 per cent) were discharged on day 1 post-operatively, and the remaining 58 patients (6 per cent) stayed 2–18 nights in hospital. The one patient who remained in hospital for 18 nights suffered an asthma exacerbation that required prolonged treatment.
Table 1. Demographics of patients undergoing day-surgery or hospital-stay tonsillectomies
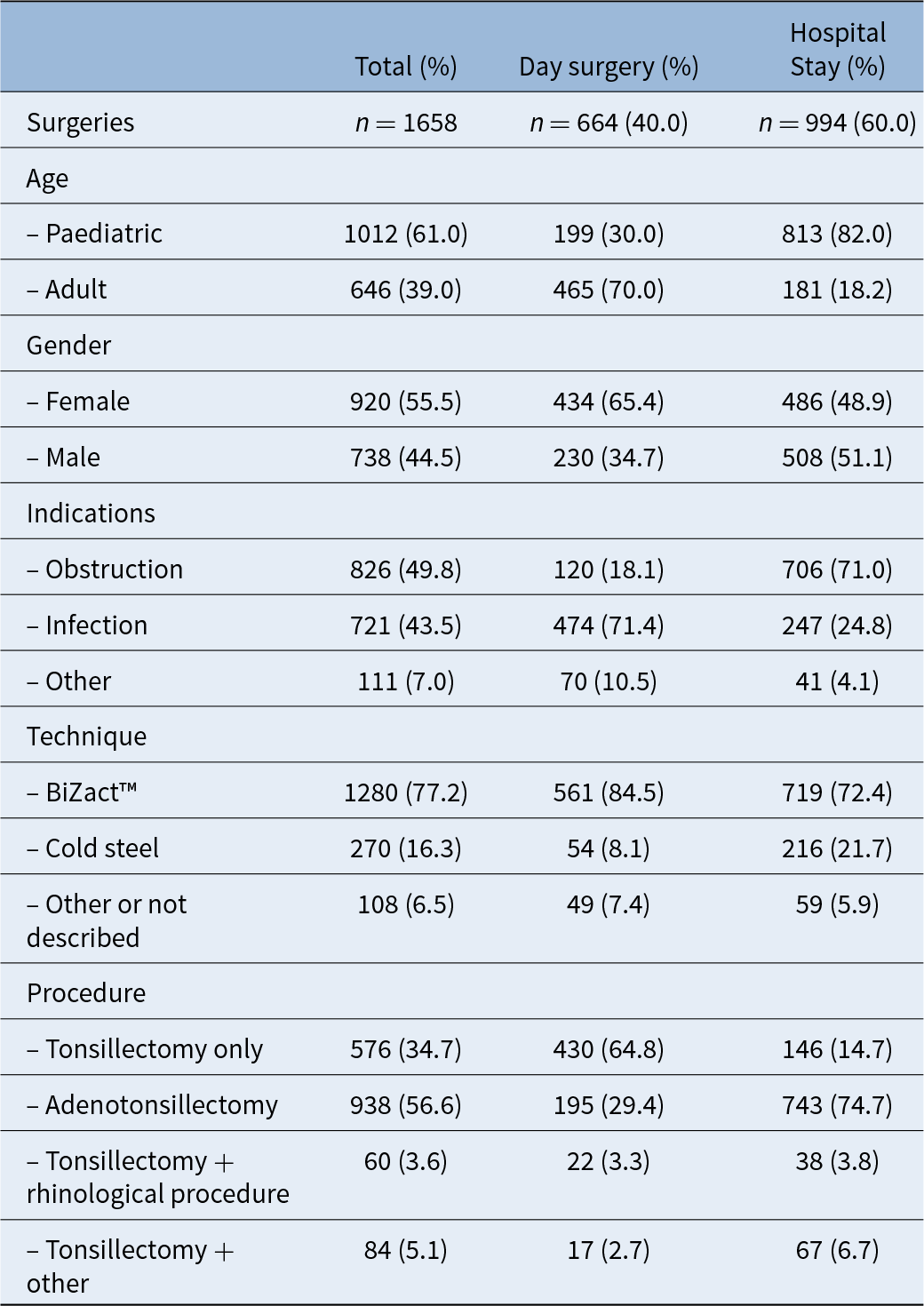
Patients underwent a variety of additional procedures along with their tonsillectomy. Thirty-four per cent (567 patients) received tonsillectomy only. Fifty-seven per cent (938 patients) underwent tonsillectomy with adenoidectomy. Four per cent (60 patients) underwent tonsillectomy and concurrent nasal or sinus surgery, and five per cent (84 patients) underwent tonsillectomy and a different ENT procedure (e.g. laryngotracheobronchoscopy or tongue-base channelling).
The main tonsillectomy technique used was BiZact™ (77 per cent), followed by cold steel dissection (16 per cent). The main indications for tonsillectomy in children (under 18 years old) were sleep-disordered breathing (74 per cent) and recurrent infections (22 per cent). The main indications for tonsillectomy in adults (18 years or older) was recurrent tonsillitis (77 per cent) and tonsil lesions (7 per cent), with the remainder of indications being obstructive sleep apnoea (OSA) or unspecified in the database (Table 1).
The number of day-surgery tonsillectomies more than doubled from 2018 (17 per cent of all tonsillectomies) to 2019 (41 per cent of all tonsillectomies). Across all five years of the study the range of day-surgery proportions was 17 per cent (72) in 2018 to 52 per cent (128) in 2022 (Figure 1).
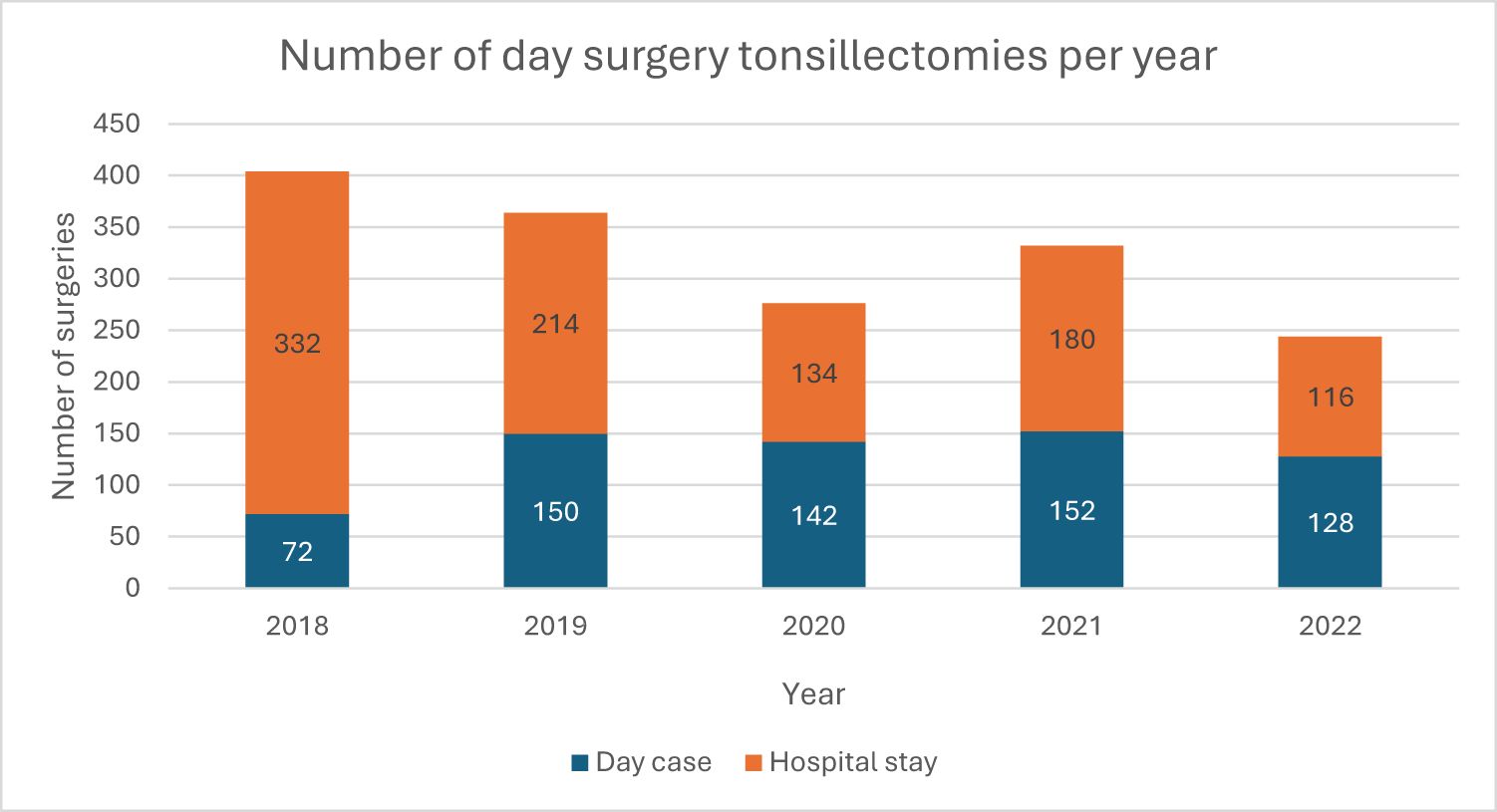
Figure 1. Number of tonsillectomies completed at Southern Adelaide Local Health Network as same-day surgery and hospital stays for any number of nights over a 5-year period (2018–2022). Total tonsillectomies n = 1658. Total day surgeries n = 664. Total hospital-stay surgeries n = 994.
The readmission rate within 24 hours of discharge was 0.60 per cent (4 patients) for the same-day surgery group and 0.64 per cent (6 patients) for the overnight-stay group (Figure 2). No patients who stayed more than one night in hospital were readmitted within 24 hours of discharge. The relative risk of readmission within 24 hours of discharge for the day-surgery group was 0.940, with the readmission rate being statistically similar between the two groups Χ 2(1, N = 1600) = 0.009, p = 0.9244). In the day-surgery group, the most common reason for representation was haemorrhage (0.5 per cent) followed by poor oral intake (0.2 per cent). None of the day-surgery patients returned to hospital within 24 hours of discharge for pain. In the hospital-stay group, the most common reason for representation was haemorrhage (0.3 per cent), followed by pain (0.2 per cent) and poor oral intake (0.1 per cent). The most common day for readmission for both day-surgery and hospital-stay patients was day 5 post-operatively.
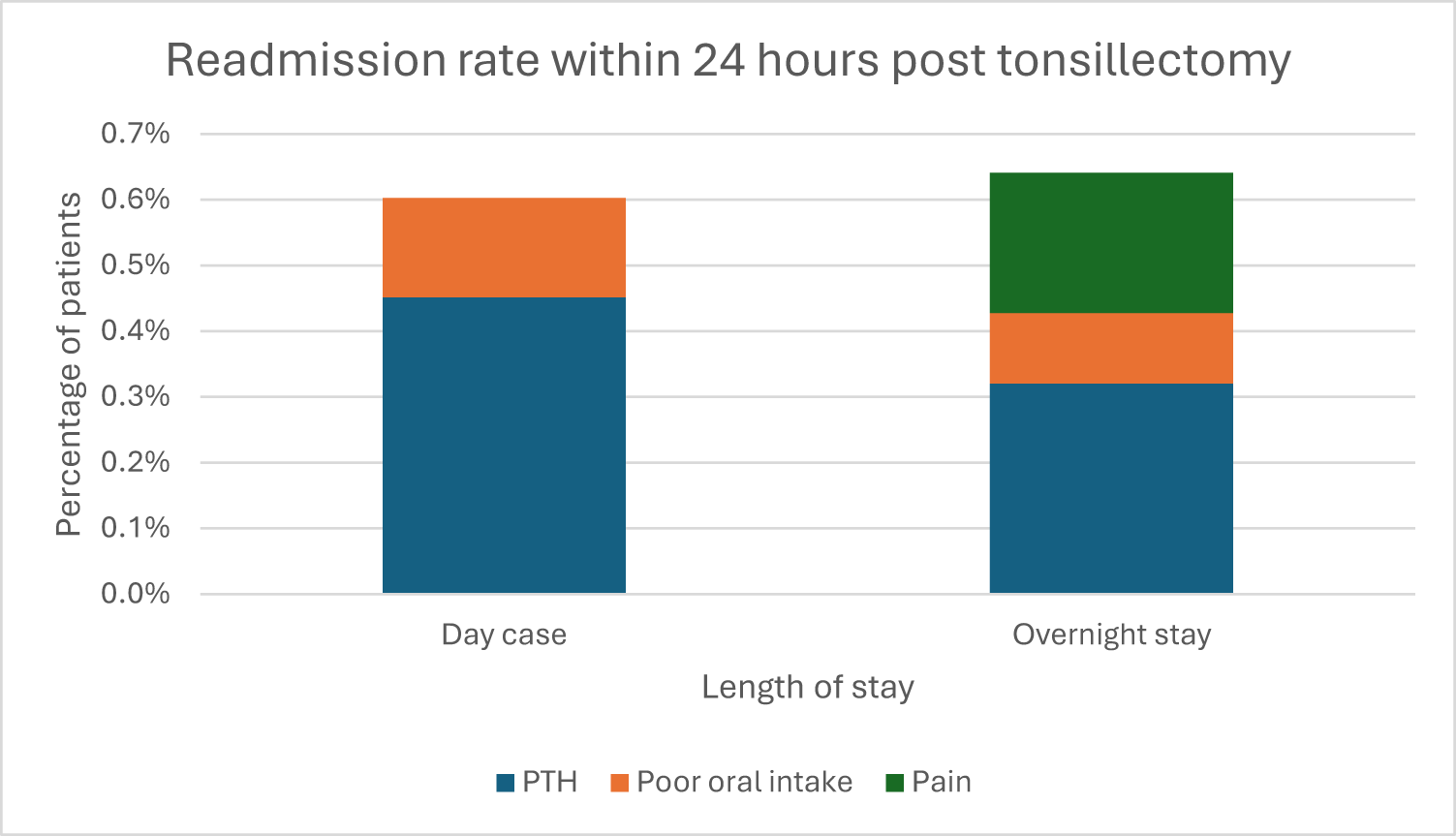
Figure 2. Comparison of readmission rate within 24 hours of discharge for day surgery and overnight stay patients, grouped by reason for readmission. PTH is post-tonsill-ectomy haemorrhage. Four day-surgery and six overnight-stay patients represented within 24 hours.
Three of the day-surgery patients (0.5 per cent) required ward-based treatment for post-tonsillectomy haemorrhage and one patient (0.2 per cent) required a return to theatre for management of their post-tonsillectomy haemorrhage. One hospital-stay patient (0.1 per cent) was readmitted for observation, five hospital-stay patients (0.5 per cent) were readmitted for ward-based treatment and none required a return to theatre within 24 hours of discharge.
The primary post-tonsillectomy haemorrhage rate was higher for hospital-stay patients (0.6 per cent) than for day-surgery patients (0.3 per cent), with a relative risk of 0.5 for primary post-tonsillectomy haemorrhage in the day-surgery group (Χ 2(1, N = 1658) = 0.751, p = 0.3862). All six hospital-stay patients with primary post-tonsillectomy haemorrhage were confirmed to have been planned for overnight stay at the time of operation, by reviewing the operation record.
Secondary post-tonsillectomy haemorrhage occurred in 89 (13 per cent) of the day-surgery patients compared with 63 (6 per cent) of the hospital-stay patients (13 per cent), with a relative risk of 1.97 for secondary post-tonsillectomy haemorrhage in the day-surgery group (Χ 2(1, N = 1658) = 19.624, p < 0.0001). The peak incidence of post-tonsillectomy haemorrhage was day 5 post-operatively for both groups (Figures 3 and 4).
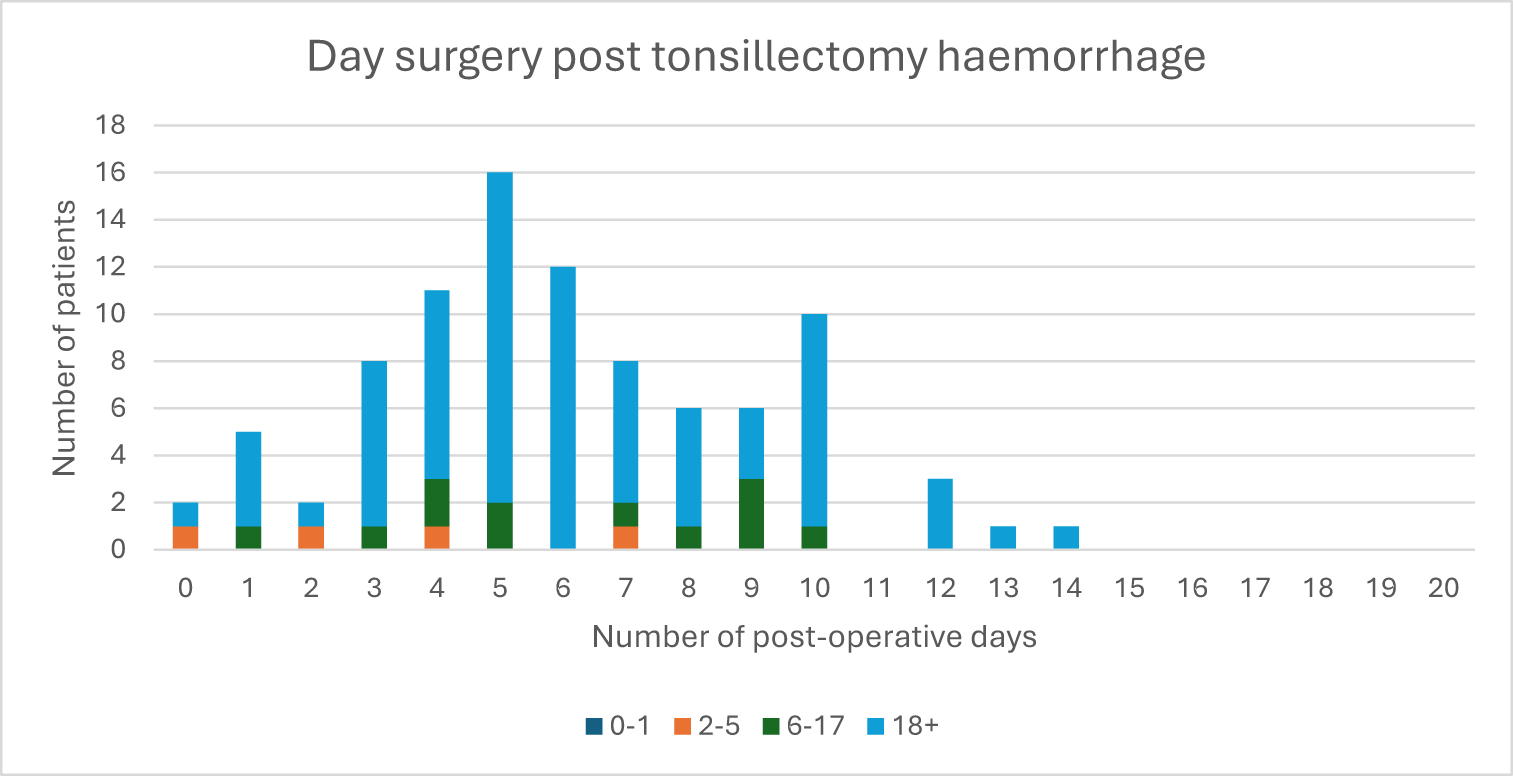
Figure 3. Number of patients with post-tonsillectomy haemorrhage (PTH) for each post-operative day for day-surgery tonsillectomy patients (n = 664), grouped by patient age in years. Total number of day-surgery patients with PTH n = 91.
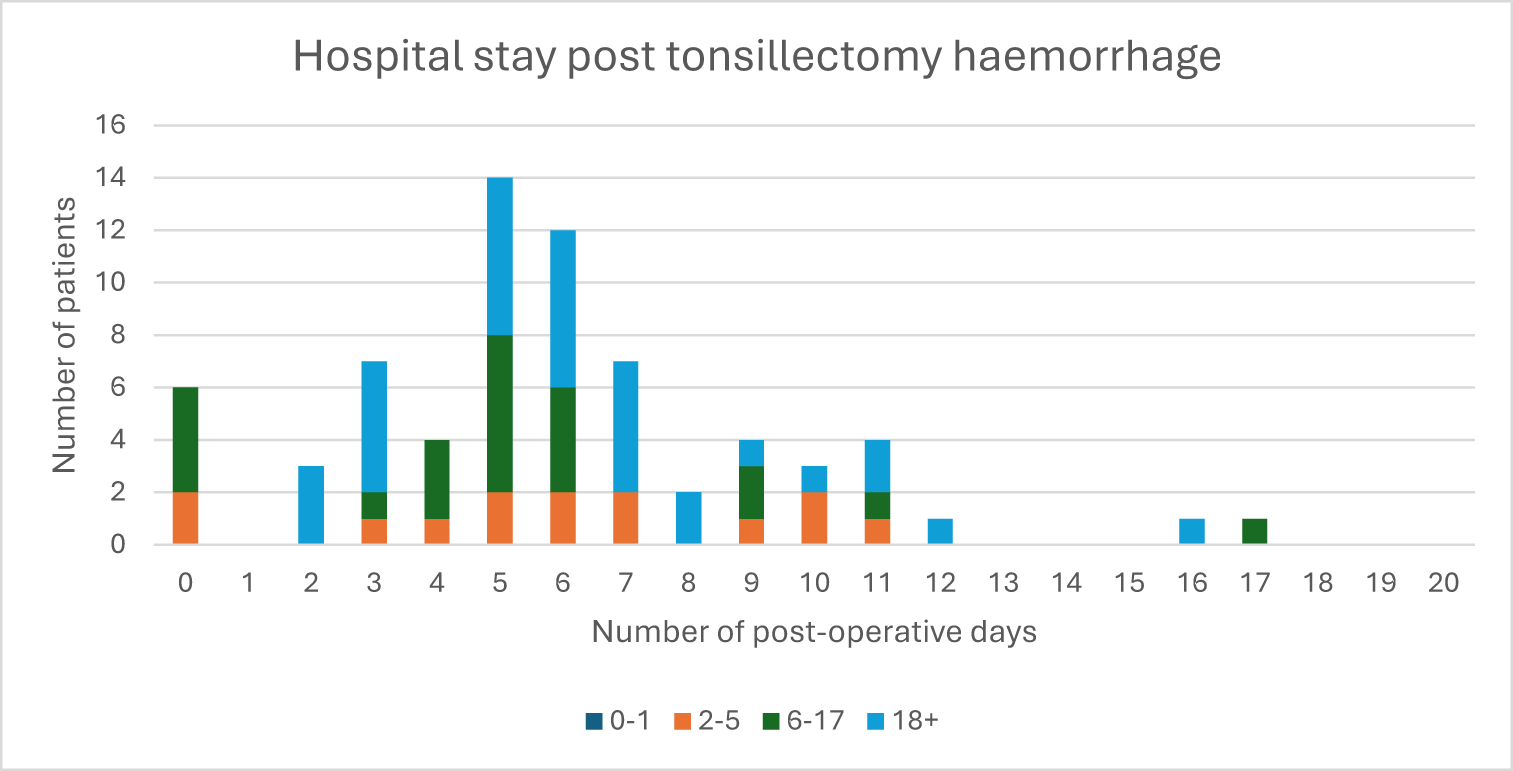
Figure 4. Number of patients with post-tonsillectomy haemorrhage (PTH) for each post-operative day for hospital-stay tonsillectomy patients (n = 994), grouped by patient age in years. Total number of day-surgery patients with PTH n = 69.
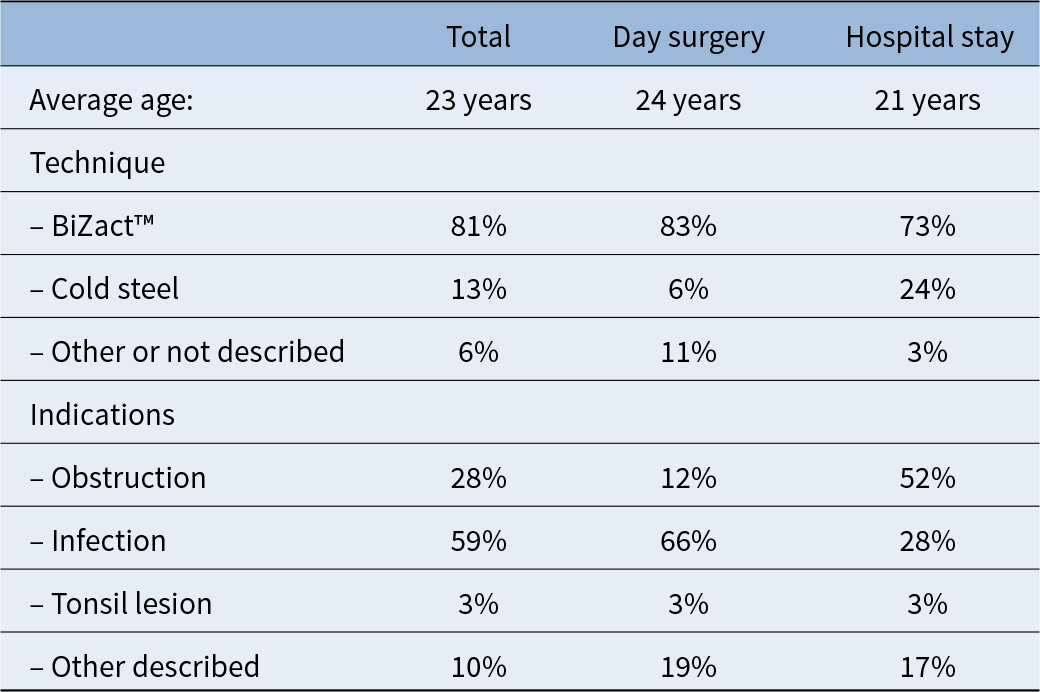
Out of 91 patients experiencing post-tonsillectomy haemorrhage for the day-surgery group, 72 (79 per cent) were Stammberger grade A (history of bleeding with no active bleeding on examination). Eight patients (9 per cent) were classified grade B (minor bleeding requiring treatment with local anaesthetic). Nine patients (10 per cent) were classified grade C (returned to the operating theatre for arrest of post-tonsillectomy haemorrhage but no transfusion required). Two patients (2 per cent) were classified grade D (required blood transfusion) (Table 2). Of the day-surgery patients with secondary post-tonsillectomy haemorrhage, 93 per cent underwent BiZact™ tonsillectomy, and 74 per cent were performed for recurrent tonsillitis. The average age of patients with secondary post-tonsillectomy haemorrhage was 24 years for day-stay patients (median age 23) and 21 years for hospital-stay patients (median age 16) (Table 3).
Table 2. Stammberger grade of all post tonsillectomy haemorrhage for day-surgery and hospital-stay tonsillectomy patients
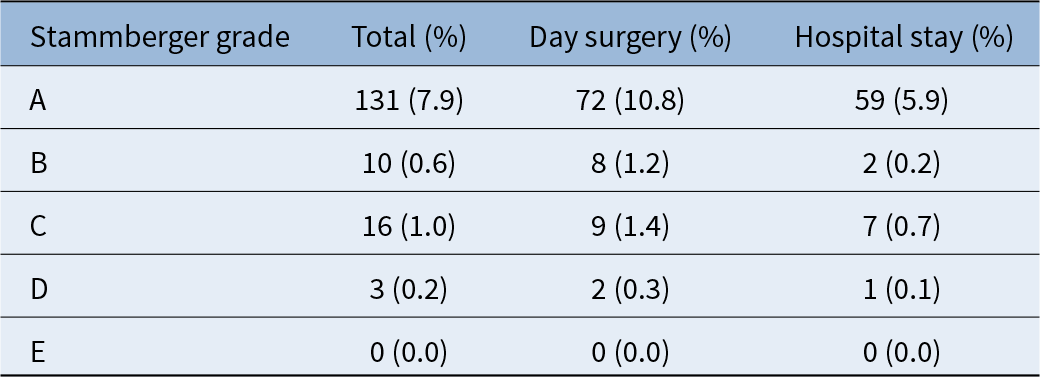
Table 3. Characteristics of patients with secondary post-tonsillectomy haemorrhage for day-surgery and hospital-stay patients
Similarly, most (86 per cent, n = 59) of the 69 patients in the hospital-stay group who experienced post-tonsillectomy haemorrhage were classified Stammberger grade A. Two patients (3 per cent) were classified grade B, seven patients (10 per cent) were classified grade C and one patient (1 per cent) was classified grade D. No patients in either group died (grade E).
The return-to-theatre rate for day-surgery patients was 1.7 per cent, and the return-to-theatre rate for hospital-stay patients was 0.8 per cent.
Analysis
Summary
Our study demonstrated that approximately half of the tonsillectomies undertaken at Southern Adelaide Local Health Network were same-day surgeries in 2022. The readmission rate within 24 hours of discharge was comparable for the day-surgery tonsillectomy group and the hospital-stay group. The primary post-tonsillectomy haemorrhage rate was lower in the day-surgery group than the hospital-stay group.
Interpretation
The number of day-case tonsillectomies increased from 18 per cent to 52 per cent across the period of the study, which may be attributable to increasing familiarity with implementing the protocol over the 5 years. Day-surgery tonsillectomy is well established in the USA. A 2019 review estimated 99 per cent of US paediatric tonsillectomies were performed as day surgeries.Reference Johnson, Zhang, Chorney, Kou, Lenes-Voit and Ulualp14 The US national tonsillectomy guidelines recommend children <3 years old and with severe sleep apnoea do not receive day-surgery tonsillectomies.Reference Mitchell, Archer, Ishman, Rosenfeld, Coles and Finestone15 Specialist Trust hospitals in the United Kingdom found no increase in adverse outcomes for hospitals that discharged fewer than 50 per cent of children on the same day of surgery compared with hospitals that discharged more than 70 per cent of children the same day. This study suggested that specialist centres could aim for a 70 per cent paediatric day-surgery tonsillectomy rate.Reference Gray, Takhar, Navaratnam, Day, Swart and Snowden16 This is much higher than Southern Adelaide Local Health Network’s paediatric day-surgery tonsillectomy rate of 20 per cent, and indicates there may be capacity for clinicians to increase implementation of the patient selection protocol or broaden the inclusion criteria (e.g. reducing the minimum age to 2 years old).Reference Morris, Hassin and Borschmann3 Our day-surgery tonsillectomy protocol also depends on patient scheduling, where afternoon procedures for children are not eligible for day-surgery tonsillectomy. Increasing the proportion of day-surgery procedures would rely on multidisciplinary changes in our centre, including extended support in the post-anaesthetic care unit.
The low readmission rate within 24 hours of discharge indicates that surgeons identified appropriate patients to undergo day-surgery tonsillectomy, and they were unlikely to require hospital care within 24 hours of discharge compared to patients in the hospital-stay group. The readmission rate within 24 hours of discharge for the day-surgery group (0.6 per cent) is similar to the readmission rate at a Scottish children’s hospital in 2014 which had no readmissions within 24 hours after day-surgery tonsillectomy.Reference Elsobky, Ahmad, Qureshi, Izzath and Sadiq17 A paediatric day-surgery unit in the United Kingdom reported a higher day-surgery tonsillectomy readmission rate of 4 per cent in the 1990s.Reference Hellier, Knight and Waddell18
A prospective audit in the United Kingdom in 2013 found that the severity of pain within 24 hours of tonsillectomy was no different between children receiving day surgery and children who stayed in hospital overnight.Reference Norrington, Flood, Meek and Tremlett19 This indicates that pain is unlikely to be a reason for readmission within 24 hours post-operatively if patients are discharged with appropriate analgesia and post-operative instructions.
The primary post-tonsillectomy haemorrhage rate of 0.3 per cent for the day-surgery group is comparable to the primary post-tonsillectomy haemorrhage rate reported by Pringle et al. in their 1996 review of day-surgery tonsillectomies,Reference Pringle, Cosford, Beasley and Brightwell20 which quoted a range of post-tonsillectomy haemorrhage rates in the included studies of 0.14–4.4 per cent. More recently, a 2018 study in Europe found a post-tonsillectomy haemorrhage rate of 2–8 per cent in their day-surgery tonsillectomies.Reference Atfeh and Richardson-May21 This suggests that primary post-tonsillectomy haemorrhage is a low risk, and it may not be necessary to require all patients to stay in hospital overnight after tonsillectomy due to concerns of post-tonsillectomy haemorrhage. Other reasons that surgeons routinely admit patients post tonsillectomy are anticipating the need for management of pain and nausea.Reference Stocker8 However, only one patient from each of the day-surgery and overnight-stay groups was readmitted within 24 hours of discharge for reduced oral intake. This suggests that pain and oral intake were able to be adequately managed at home in the same-day surgery cohort.
The secondary post-tonsillectomy haemorrhage rate was significantly higher in the day-surgery tonsillectomy group than the hospital-stay group, which is a concern to the authors of this study. We hypothesise that the higher secondary post-tonsillectomy haemorrhage rate was due to the age distribution of patients in this groups as most of our patients with secondary post-tonsillectomy haemorrhage were adults. There was also a higher proportion of adult patients in the day-surgery group, and it has been demonstrated in other studies that adults have a higher risk of post-tonsillectomy haemorrhage than children, possibly due to slower mucosal healing and higher rates of infections.Reference Li, Forer and Veivers11 The other possibility was the higher rate of BiZact™ tonsillectomy in the day-surgery group compared to the use of cold steel in the hospital-stay group (Table 1). BiZact™ tonsillectomy as a ‘hot tonsillectomy technique’ has been shown to have a higher secondary post-tonsillectomy haemorrhage rate compared to the cold steel technique.Reference Mao, Woods, Athanasiadis, MacFarlane, Boase and Joshi22 The most common grade severity of haemorrhage for both groups was grade A (haemorrhage prior to presentation that has self-resolved), and the return-to-theatre rate for both groups was comparable with the national benchmark of 1.6 per cent.Reference Li, Forer and Veivers11
In appropriate circumstances, performing day surgeries can result in a substantial financial saving for hospitals.Reference Faramarzi, Fardid, Kaboodkhani, Emadi, Shahmohammadi and Keshavarz23 A 1990 NHS report identified tonsillectomy as a suitable day-surgery procedure to reduce the costs of service provision.24 In 2023 the cost of an overnight hospital stay at Southern Adelaide Local Health Network was $2409 per patient. The 664 day-surgery tonsillectomies are estimated to have saved the institution approximately $1.2 million over the five years of the study, compared with keeping those same patients in hospital overnight after surgery.
Limitations
The major limitations of this study are inherent to a retrospective review, with lack of data regarding the surgeons’ level of training and estimated volume of blood loss for post-tonsillectomy haemorrhage. Our protocol also selected for low-risk patients in the day-surgery group, thus creating a selection bias. Complications may be under-reported if patients presented to other hospitals for post-operative care, although we attempted to capture these by asking patients at their post-operative review for any admissions to other hospitals. Additionally, the number of patients who were eligible for day surgery per the patient selection protocol but not offered at the surgeon’s discretion was not recorded. This makes it difficult to estimate the effect of surgeon discretion compared to the patient selection criteria during the implementation of same-day tonsillectomy. Our patient selection protocol is also unlikely to be generalisable to low-resource healthcare settings, due to regional variation in access to emergency treatment.
• Day-surgery tonsillectomy is not widely implemented in Australia, and the safety of day-surgery tonsillectomy in an Australian setting has not yet been established
• Day-surgery tonsillectomy is safe and feasible for low-risk patients over four years of age, with a low readmission rate and similar risk of primary post-tonsillectomy haemorrhage for day-surgery and hospital-stay patients
• Day surgery tonsillectomy is indicated for patients over four years of age who are American Society of Anaesthesia scores 1 or 2 and do not have obstructive sleep apnoea (OSA), or significant craniofacial or neuromuscular anomalies, and the patient lives within 15 km of access for hospital care
• Day-surgery tonsillectomy has a potentially valuable cost savings for institutions in carefully selected patients
Conclusions
Further considerations beyond the Southern Adelaide Local Health Network protocol can be made when assessing suitability for day-surgery tonsillectomy. Patients from linguistically diverse backgrounds may benefit from additional in-hospital support with post-operative counselling and support with translators.Reference Jones, Austad, Silver, Cordova-Ramos, Fantasia and Perez25 Suspicion of severe OSA without a pre-operative polysomnogram can be a reason that clinicians choose to keep patients in hospital after surgery.Reference Stocker8
Beyond patient selection protocols, there are other means for clinicians to optimise day-surgery tonsillectomies. Guidelines from Oxford in the United Kingdom suggest robust antiemetic and analgesia administration, perioperative warming and hydration as key factors to increase the success of same-day discharge for tonsillectomy.Reference Chaidas and Winterborn26
Our results demonstrate that a protocol-led, same-day surgery tonsillectomy is safe and feasible in carefully selected patients. Day-surgery patients have comparable readmission rates within 24 hours of surgery with patients who stay one or more nights in hospital; they also do not experience a higher rate of primary post-tonsillectomy haemorrhage. Further research is required to investigate the higher rate of secondary post-tonsillectomy haemorrhage in day-surgery patients. The low readmission rate and primary post-tonsillectomy haemorrhage rate indicate that same-day tonsillectomy is safe and feasible to implement in an Australian healthcare setting.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0022215125000441
Data availability statement
The de-identified data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Authorship statement
SD and EHO designed the work; SD acquired and analysed data; SD and EHO drafted, revised and approved the manuscript; SD and EHO agree to be accountable for all aspects of the work.
Conflict of interest
Professor Eng Hooi Ooi was a consultant for Medtronic in providing educational meeting presentations on BiZact™ tonsillectomy.
Acknowledgements
Dr Ashlee Kimball contributed to the literature review.
Funding
No external funding was provided for this study.
Ethical considerations
Southern Adelaide Local Health Network Human Research Ethics Committee granted exemption (4808) on the basis that de-identified data was used as this was assessed as a quality improvement project.









