Introduction
Support for family caregivers is an integral aspect of palliative care as a life-threatening disease also impacts people close to the patient (World Health Organization 2020). Family caregivers commonly experience physical symptoms such as sleep disturbance and fatigue, as well as depression, anxiety, and distress (Alam et al. Reference Alam, Hannon and Zimmermann2020). In a longitudinal survey study among advanced cancer patients and family caregivers in the Netherlands, family caregivers’ emotional functioning was lower than that of patients (van Roij et al. Reference van Roij, Raijmakers and Ham2022). As such, family caregivers should be considered as care recipients alongside the patient (Hudson et al. Reference Hudson, Morrison and Schulz2020). Family caregivers also play an important role in the care for the patient. With increasing shortages in healthcare and the ageing population, their role in palliative care provision is becoming even more important (Etkind et al. Reference Etkind, Bone and Gomes2017; Michaeli et al. Reference Michaeli, Michaeli and Albers2024; PZNL, AHzN, KWF and VPTZ 2020). Therefore, family caregivers being well-supported by healthcare professionals is a prerequisite to ensure high-quality care for the patient as well.
A recent scoping review found that existing clinical guidelines for the support for family caregivers state that healthcare professionals should assess and meet their emotional, practical, physical, social and existential support needs, provide information, involve them in the patient’s care and decision-making, help them in preparing for the patient’s death, and offer bereavement support (Coelho et al. Reference Coelho, Albuquerque and Neto2025). However, several studies have demonstrated that such support is not structurally embedded in practice, for example, in the Netherlands and the USA (Becqué et al. Reference Becqué, Rietjens and van der Heide2021; Hoffstädt et al. Reference Hoffstädt, Boogaard and Tam2023; Sabo et al. Reference Sabo, Chin and Sethares2022). Therefore, a change of practice is warranted. Such a change may be evoked by the implementation of an organizational intervention aimed at structurally modifying the everyday practices of healthcare professionals, with the goal of embedding consistent support for family caregivers within the organization. However, implementation of such organizational interventions is associated with numerous challenges such as lacking resources, high workload, and resistance to change (Geerligs et al. Reference Geerligs, Rankin and Shepherd2018; Williams et al. Reference Williams, Perillo and Brown2015). Strategies for successful implementation of organizational interventions include flexibility in implementation and adaptation of the intervention to the organization’s existing structures (Collingridge Moore et al. Reference Collingridge Moore, Payne and van den Block2020; Powell et al. Reference Powell, Fernandez and Williams2019). To this end, we developed an organizational intervention that could be tailored to the organization’s context to improve support for family caregivers. During the intervention, healthcare professionals engaged in a structured practice improvement trajectory in which they worked toward achieving organization-specific goals to enhance their current practice of supporting family caregivers. Healthcare professionals took the lead in defining these goals to foster ownership and reduce resistance to change. The aim of this study was to evaluate the impact of this tailored organizational intervention on the support for family caregivers.
Methods
Study design
To evaluate the impact of the tailored organizational intervention on the support for family caregivers, a convergent mixed-methods study design was adopted (Creswell and Clark Reference Creswell and Clark2017). Qualitative and quantitative data were collected and analyzed independently, followed by their integration to facilitate a holistic understanding of the intervention’s effect. The study was conducted in various healthcare settings between December 2021 and August 2023. Before and after the intervention, surveys were distributed among healthcare professionals (same group pre and post) and recently bereaved family caregivers (different groups pre and post). Additionally, after the intervention, focus groups with participants were conducted, and final evaluation reports were written.
This study was part of a larger Dutch study called “Support for family caregivers” (2017–2024; Hoffstädt et al. Reference Hoffstädt, Boogaard and Tam2023, Reference Hoffstädt, Tam and Stoppelenburg2024). This substudy was preregistered on the Open Science Framework (OSF) in November 2021 (Stoppelenburg et al. Reference Stoppelenburg, van der Steen and van der Linden2021). Some deviations from the preregistration occurred: qualitative data and a survey study among family caregivers were added, and some adjustments were made in the outcome measures based on how the healthcare organizations shaped their improvement trajectory. These deviations from the preregistration are described in the “measures” section. The Medical Ethics Committee Leiden Den Haag Delft approved the study (N21.072).
The intervention and its procedure
An open call was issued with national coverage through the funder (Netherlands Organization for Health Research and Development; ZonMw), inviting Dutch healthcare organizations to participate in this implementation study. In total, 24 organizations initially applied. Seven organizations dropped out due to insufficient workforce and unfortunate timing because of large organizational changes or other ongoing projects. Consequently, a total of 17 organizations (6 hospices, 5 home care organizations, 3 nursing homes, 2 hospitals, 1 transmural organization) implemented the intervention, the vast majority of which were in urban areas. The intervention comprised a structured practice improvement trajectory consisting of 5 steps. First, in each participating organization, a project team was assembled consisting of a project ambassador and 3–6 other team members of various professions to support them, including at least 1 member of the organization’s management team. The project ambassador was appointed internally based on their motivation, expertise, and availability. At the frequent contact moments during the whole study period, the research team regularly assessed the motivation of the project ambassador and their project team and tried to accommodate their needs to maintain their engagement. Second, the project team and some additional healthcare professionals (the group ranging from 6 to 11 people) conducted the “Family caregiver journey” workshop, which was developed as part of the study (Boere Reference Boere2021). The structured workshop facilitated a discussion on the organization’s current support for family caregivers, its strengths and weaknesses, and a brainstorm on strategies to address shortcomings. Third, based on the workshop’s outcomes, the project teams developed an action plan with organization-specific goals to improve the support for family caregivers, including actions required to achieve those goals. Goals that were set and corresponding actions either related to the support for family caregivers directly (e.g., improving information provision or the support provided after the patient’s death) or aimed to create preconditions for healthcare professionals to support family caregivers (e.g., organizing helpful tools or increasing healthcare professionals’ required skills and knowledge). A more detailed account of the content of the action plans is provided in a separate study (Stoppelenburg et al. Reference Stoppelenburg, Hoffstädt and van Bodegom-vos2025). Project teams were provided with a template for the action plan, which is provided in Supplement 1. Fourth, the project teams kicked off with an educational session for all healthcare professionals of the involved departments or teams to notify them of the action plan and what is needed from them to achieve the goals. Last, project teams worked toward achieving their goals over the following year. Quarterly evaluation meetings were held to monitor progress. A toolkit was available to facilitate achieving the goals, including brochures with information for healthcare professionals and family caregivers. In each organization, 1 researcher (MT or HH) was involved and available for project ambassadors to give instructions and advise on the action plan’s content and feasibility and general implementation, and to receive updates regarding progress.
Measures
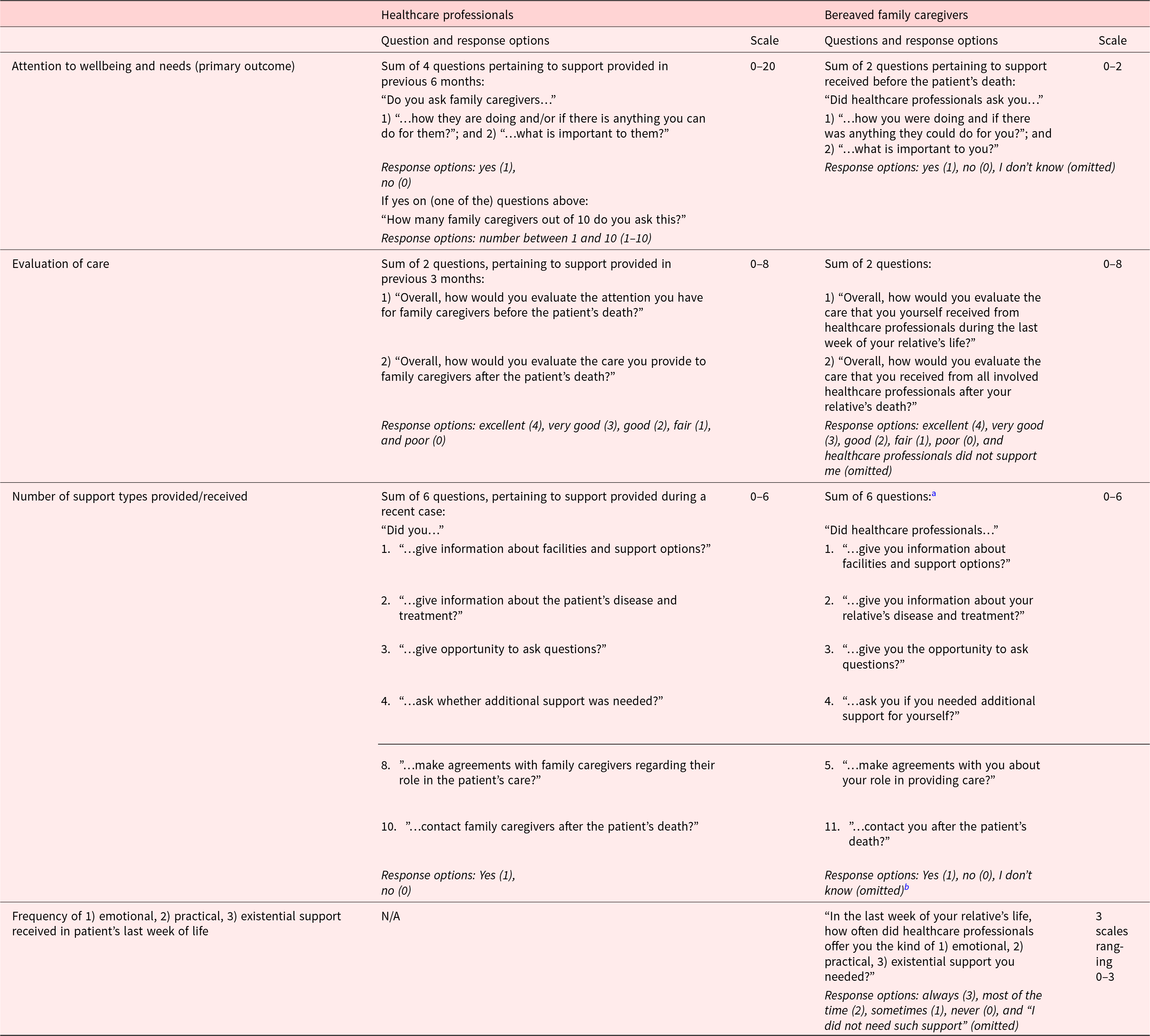
The surveys were self-developed as no existing instrument covered our purpose. Both surveys addressed demographic characteristics, healthcare professionals’ attention to family caregivers’ wellbeing and needs, more specific support types (e.g., information provision, inquiring after additional support needs), and evaluation of care that was provided or received. Some questions were sourced from existing Dutch family caregiver surveys and adapted to be applicable to healthcare professionals (Hoffstädt et al. Reference Hoffstädt, Klapwijk and Hartog2025; van der Steen et al. Reference van der Steen, Ribbe and Deliens2014). A detailed description of all quantitative outcome measures is provided in Table 1.
Table 1. Outcome measures regarding the effect of the ON2 intervention

a Questions 1–5 pertained to support received before the patient’s death.
b Question 5 had the response options “yes,” “no, but I would have liked this,” and “no, but I did not need this.” The latter were treated as a negative response.
Primary outcome measure
The primary outcome measure was “attention to wellbeing and needs,” which encompassed whether healthcare professionals asked family caregivers how they were doing, if they could do anything for them, and what was important to them. For healthcare professionals, a 0–20 scale was computed based on 4 questions. For family caregivers, a 0–2 scale was computed based on 2 questions (Table 1). This slightly deviates from the primary outcome measure preregistered with the OSF, which reads “the number of healthcare professionals who ask at least 80% of family caregivers how they are doing and/or whether they can do something for them.” The adjustment was made to gain a broader understanding of this aspect of care.
Secondary outcome measures
The 5 secondary outcome measures were: 1) evaluation of care; 2) number of support types provided/received; and family caregivers’ reports on the frequency of 3) emotional, 4) practical, and 5) existential support received during the patient’s last week of life (Table 1). The latter 4 secondary outcome measures were not preregistered with OSF. Furthermore, 1 secondary outcome measure preregistered with OSF was dropped from analysis: “the needs of healthcare professionals for support in providing pre and post-death care to family caregivers assessed with selected items from the End-of-Life Professional Caregiver Survey.” This outcome measure was dropped as the educational needs included in the survey were rarely targeted by the action plans.
Evaluation of care
For both healthcare professionals and family caregivers, a 0–8 scale was computed by summing 2 questions assessing evaluation of care provided or received before and after the patient’s death.
Number of support types provided/received
For both healthcare professionals and family caregivers, a 0–6 scale was computed by summing 6 items assessing whether a specific support type was provided or received, such as information provision or whether there had been contact after the patient’s death.
Frequency of 1) emotional, 2) practical, and 3) existential support received in the patient’s last week of life: These outcome measures were assessed only among family caregivers. Each outcome comprised 1 question assessed with a 0–3 scale.
Data collection
Quantitative data
Before the intervention, the research team digitally distributed the survey to the healthcare professionals involved in the project who had regular contact with family caregivers. The family caregiver survey was distributed by postal mail to the family caregiver who had been most involved during the disease trajectory of each patient who had died in the previous 6 months while under the care of a participating healthcare team or department. The most involved family caregiver was mostly, but not exclusively, the person who was noted as the primary contact person. All family caregivers of the age of 18 or older were eligible to participate. After the intervention, surveys were distributed in the same manner among the engaged healthcare professionals and a new group of recently bereaved family caregivers. Respondents agreed with the use of their data as they completed and returned the survey. Data entry and management were facilitated by Castor EDC (2019).
Qualitative data
Project ambassadors completed an evaluation form prior to the final evaluation meeting, which regarded the progress of the set goals, specific changes in work processes, encountered barriers and facilitators, and sustainability of the changes that were made. Furthermore, the involved researcher wrote a report on what was discussed during the final evaluation meeting. Last, online focus groups were conducted after the intervention with project team members of each healthcare setting. The focus groups were guided by a topic list similar to the topics addressed in the final evaluation form. All focus groups were recorded and transcribed clean verbatim.
Data analyses
Quantitative data analysis
First, descriptive statistics were used to present demographic characteristics and the support that was provided or received. Second, for each outcome measure of healthcare professionals, mixed model analyses were performed to assess differences between pre and post-intervention. Participant ID was included as a random factor to account for variability between individuals. Type of healthcare setting and an interaction term between pre-post intervention and healthcare setting were added as fixed factors. If the interaction term was significant, the model was run separately for each healthcare setting. When non-significant, the model was rerun without the interaction effect. As the family caregiver data was unpaired, rather than the participant ID, the different healthcare organizations were added as a random factor. Because this accounted only for minor variation, we opted for linear regression analyses. Interaction effects were examined as in the healthcare professionals’ analyses. For scale computation of all outcome measures only complete cases were used.
Both mixed model and regression analyses were initially conducted with robust standard errors using bootstrapping due to heteroscedasticity in the data. However, when analyses were performed separately for each healthcare setting, results were presented with non-robust standard errors as bootstrapping was impossible due to the smaller sample sizes.
All analyses were performed in IBM SPSS (version 29; Reference Corp2022). The 95% confidence intervals were inspected to determine significance.
Qualitative data analysis
Focus group transcripts and final evaluation reports were analyzed with conventional qualitative content analysis (Hsieh and Shannon Reference Hsieh and Shannon2005). HH coded the data inductively while being guided by the research aim of exploring the intervention’s impact on the support for family caregivers. Categories were created and discussed with the research group. Analyses were performed in ATLAS.ti (version 24; 2023).
Integration of quantitative and qualitative data
After both the quantitative and qualitative data were analyzed, the findings were compared to identify overlapping findings and findings unique to 1 data type. Conclusions informed a narrative in which the data types complemented each other.
Results
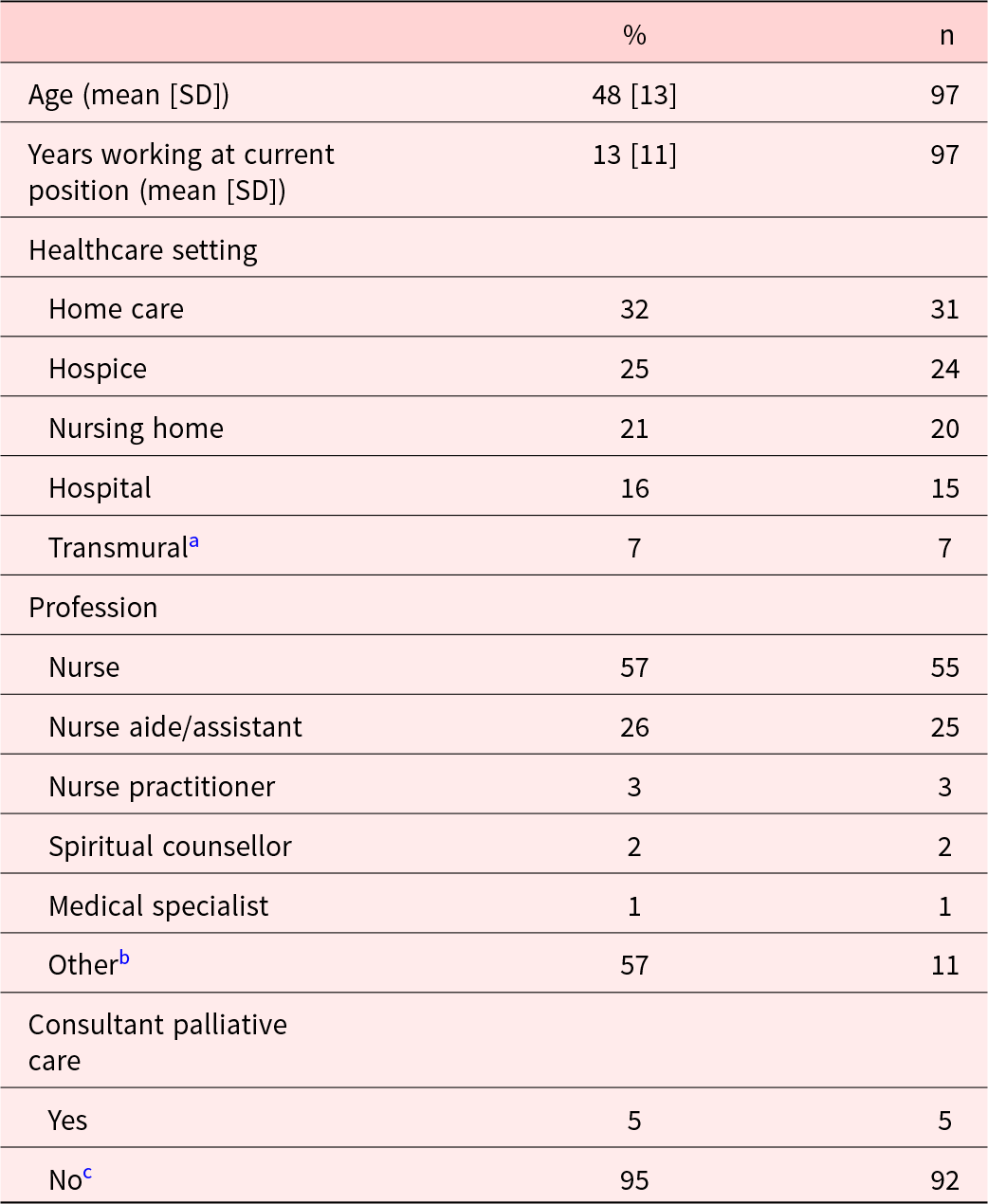
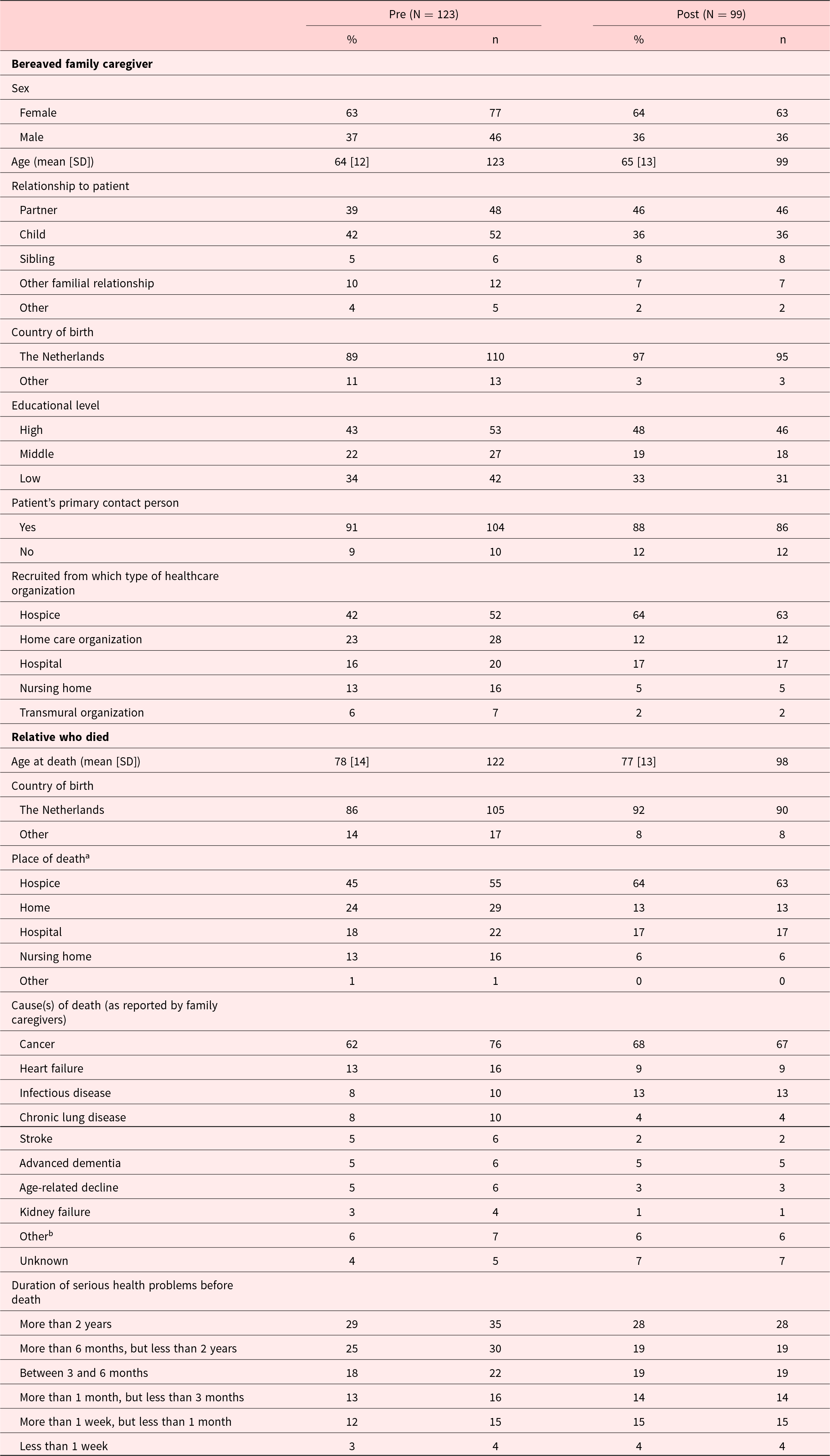
In total, 97 professionals completed the pre- and post-survey. The survey was initially distributed to volunteers working at hospices as well, which was later deemed unsuitable as the survey primarily focused on healthcare professionals’ responsibilities. Therefore, we are unable to report a response rate exclusively for healthcare professionals. Most healthcare professionals were nursing staff (83%) and most worked in home care (32%), followed by hospices (25%) and nursing homes (21%; Table 2). All participating healthcare organizations were represented in the sample of healthcare professionals, with the number of responses per organization ranging from 1 to 14 (median = 6). Of the family caregivers (Table 3), 129 out of 350 responded to the pre-survey (37% response rate) and 100 out of 216 to the post-survey (46% response rate). Seven responses (pre: n = 6; post: n = 1) were excluded as open-ended responses reported on experiences with non-participating healthcare organizations. Two participating healthcare organizations were not represented in the pre- and post-survey samples of family caregivers, as no response was received to either survey (1 home care organization and 1 hospice). The number of included responses from family caregivers per organization to the pre-survey ranged from 0 to 17 (median = 7; no response from 3 healthcare organizations), and to the post survey, this ranged from 0 to 24 (median = 3; no response from 4 healthcare organizations). Most family caregivers were recruited through participating hospices (pre: 42%; post: 64%). Both before and after the intervention, most family caregivers were the patient’s partner (pre: 39%; post: 46%) or child (pre: 42%; post: 36%). Demographic characteristics of the 2 groups of family caregivers and their deceased relatives (pre and post) were similar (Table 3).
Table 2. Characteristics of healthcare professionals at baseline (paired pre-post data of 97 healthcare professionals)

a A healthcare organization that provides nursing care in various healthcare settings.
b Living room supervisor/welfare assistant/activities coordinator (n = 6), hospice coordinator (n = 3), hospice manager (n = 1), case manager (n = 1).
c Three healthcare professionals answered “no” at baseline and “yes” at the post-measurement.
Table 3. Characteristics of the bereaved family caregivers and their relatives who died (non-paired pre-post data)

a In some cases, the patient died in a different setting from where the respondent was recruited (e.g., recruited from home care.
b E.g. ALS, internal bleeding, liver failure, hip fracture. organization, but the patient died in a hospital).
In total, 22 project team members of 14 of the 17 organizations participated in the focus groups. Most were project ambassadors (n = 10), followed by managers (n = 8) and other project team members (n = 4). An individual interview was conducted with a nursing home manager involved in two of the nursing homes of a single organization who could not attend the focus group.
The qualitative data analysis led to findings regarding the intervention’s impact at 3 levels that informed the narrative below: the direct impact on the support for family caregivers as provided by healthcare professionals and received by family caregivers, the impact on the healthcare team, and the impact on the healthcare organization. Quantitative findings pertained to the first level. An overview of the descriptive statistics for all survey items is provided in Supplement 2.
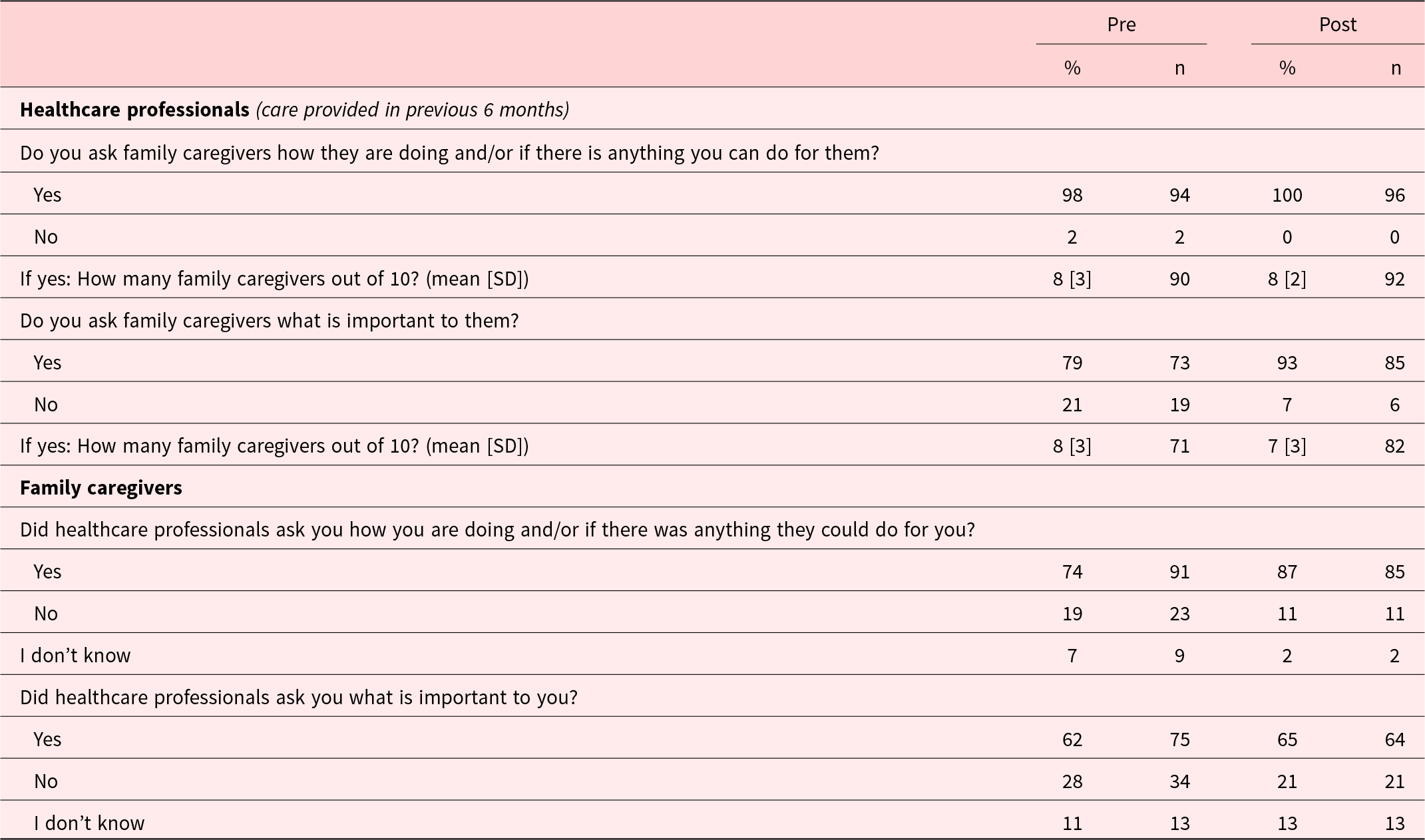
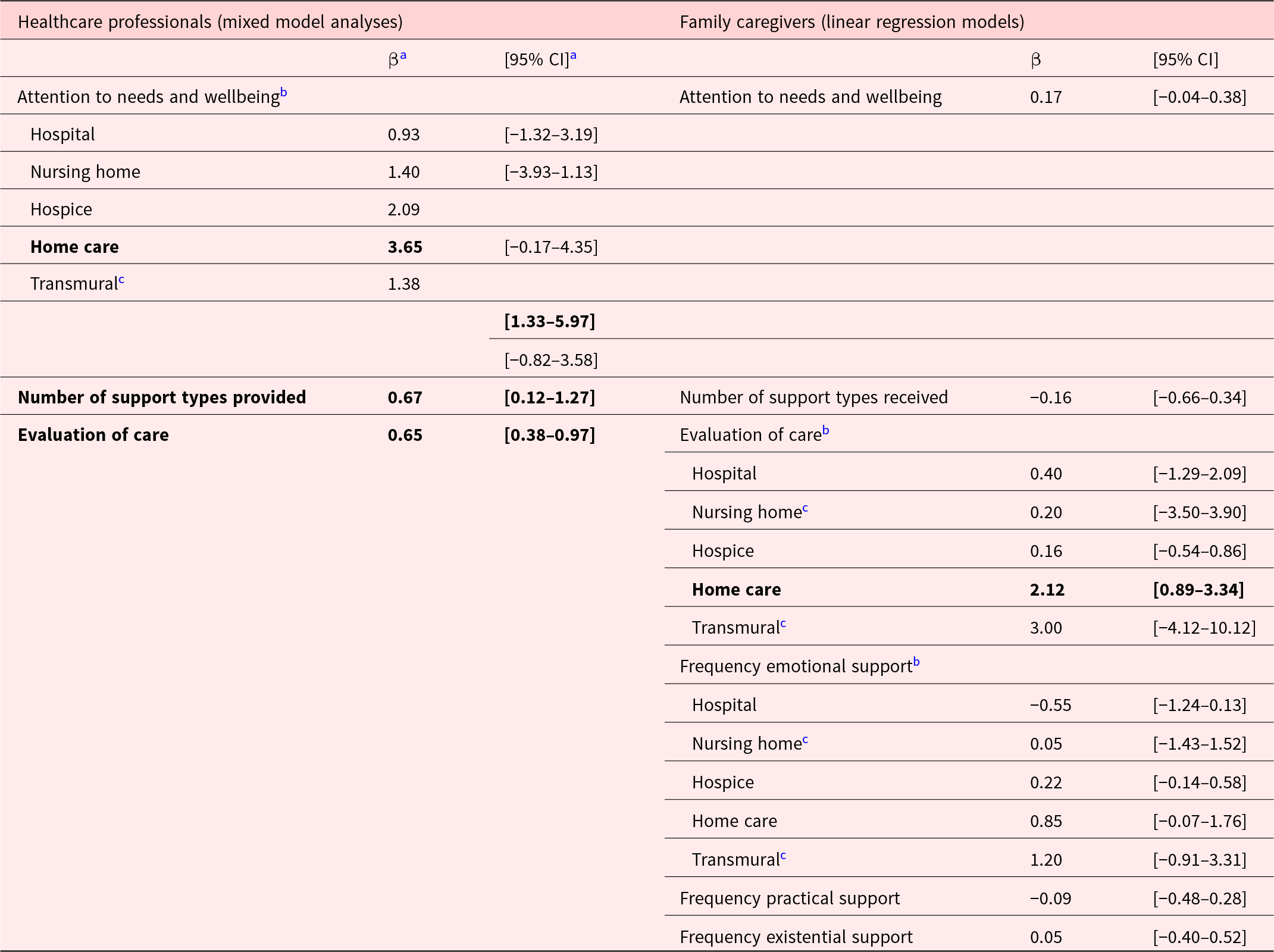
The intervention’s direct impact on the support for family caregivers
Both before and after the intervention, (almost) all healthcare professionals reported to have asked family caregivers how they were doing and/or if they could do anything for them (pre: 98%; post: 100%), and the majority asked at least 80% of family caregivers (pre: 71%; post: 72%). An increase was observed in the number of healthcare professionals reporting to have asked family caregivers what was important to them (pre: 79%; post: 93%; Table 4). The mixed model analysis on “attention to wellbeing and needs” demonstrated a significant increase among healthcare professionals working in home care (β = 3.65; 95% CI: 1.33–5.97; Table 5). With regard to family caregivers, more reported to have been asked how they were doing and if anything could be done for them in the post-intervention group (87%) than in the pre-intervention group (74%; Table 4). A smaller increase was observed in family caregivers reporting to have been asked what is important to them (pre: 62%; post: 65%). The linear regression analysis on “attention to wellbeing and needs” received by family caregivers did not demonstrate a significant increase (Table 5). No large increase was observed in reports of having received sufficient support and guidance (pre: 64%; post: 68%). However, after the intervention family, caregivers reported more often that sufficient attention was paid to them (pre: 61%; post: 74%).
Table 4. Healthcare professionals’ attention to family caregivers’ wellbeing and needs before and after the intervention

Table 5. Intervention effects on care provided and care received – outcomes of mixed model and linear regression analyses

a β = beta coefficient, 95% CI = 95% confidence interval.
b In these models, a significant interaction term implied a difference between pre- and post-intervention assessments and differences by type of healthcare setting. Therefore, these models were run separately for healthcare settings.
c Sample sizes of healthcare professionals or family caregivers recruited from these settings were very small (n < 10). Due to the resulting limited statistical power, the outcomes from these settings should be interpreted with caution.
Qualitative data also implied improvement on healthcare professionals’ attention to family caregivers wellbeing and needs as, across all organizations, an increased awareness of healthcare professionals of the importance of doing so was reported. Project team members mentioned that healthcare professionals more frequently engaged in informal conversations with family caregivers. In some cases, the intervention also brought about “that there is now more focus on family caregivers from the intake, instead of that being something that has to grow over time.” (researcher’s evaluation report; home care organization).
New and improved actions of healthcare professionals to support family caregivers
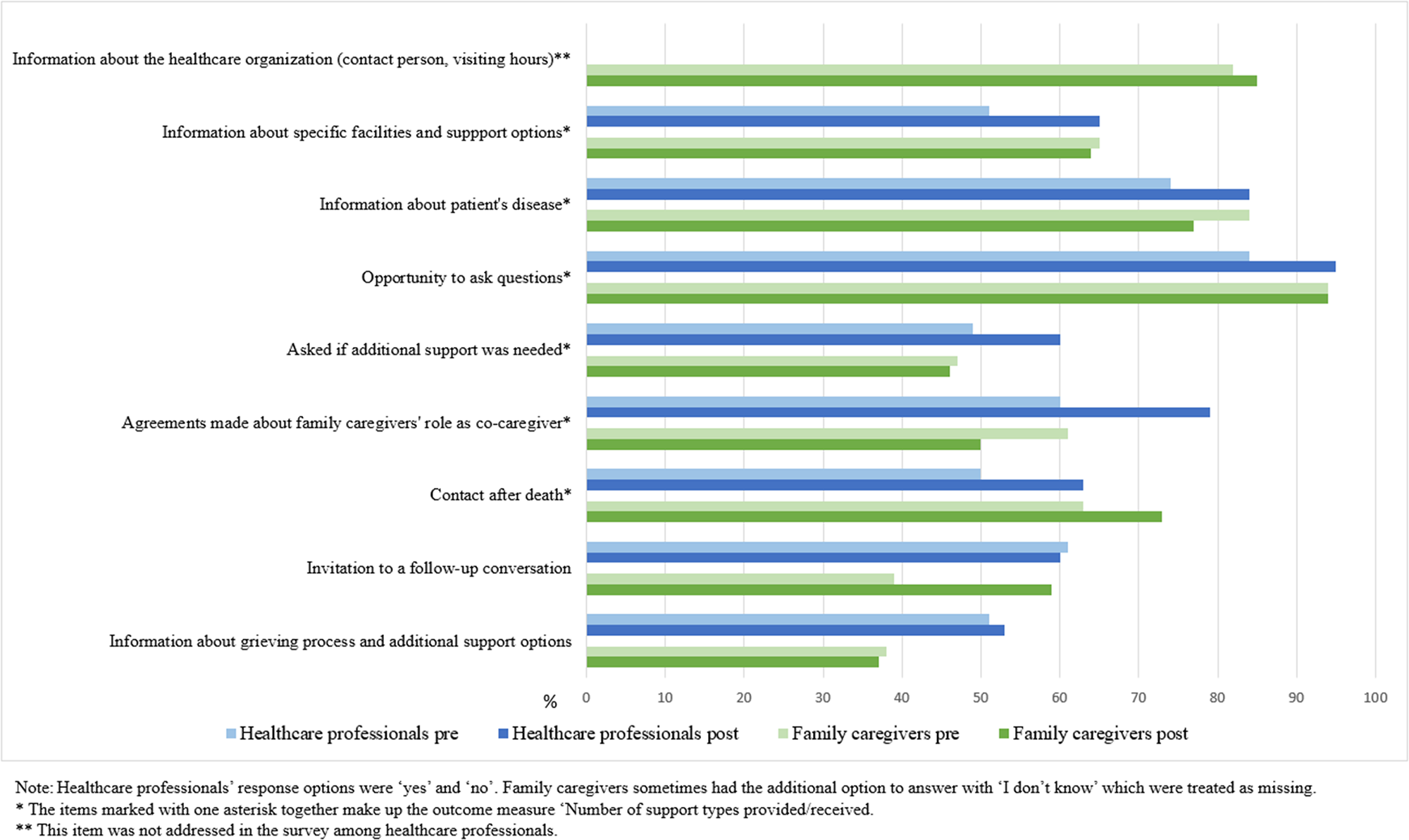
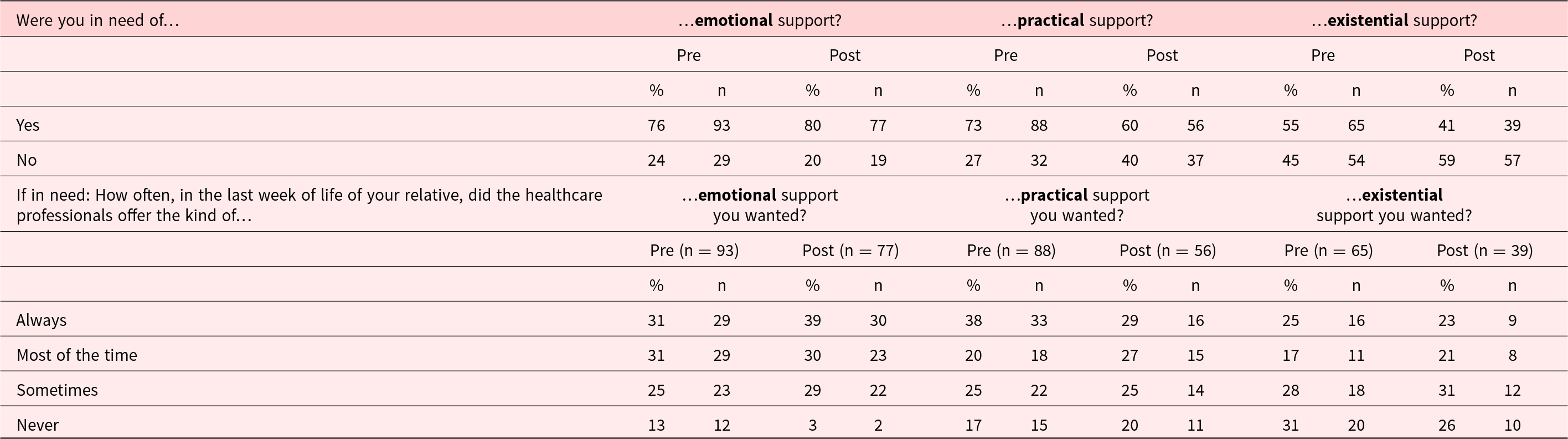
The quantitative data showed increases in healthcare professionals’ reports on whether they provided specific types of support during a recent case (Figure 1). The largest increase was found in making agreements with family caregivers about their role as co-caregiver (pre: 60%; post: 79%) and information provision about specific facilities and support options (pre: 51%; post: 65%). The mixed model analysis on “number of support types provided” demonstrated a significant increase (β = 0.67, 95% CI: 0.12–1.27; Table 5). Among the family caregivers, no appreciable increases were observed in specific support types that were received before the patient’s death. Increases were observed in having had contact with healthcare professionals after the patient’s death (pre: 63%; post: 73%) and a follow-up conversation (pre: 33%; post: 46%; Figure 1). The linear regression analysis on “number of support types received” did not demonstrate a significant increase. Nor did the linear regression analyses on the frequency in which family caregivers reported having received the kind of emotional, existential and practical support they wanted (Tables 5 and 6).

Figure 1. Specific care provided by healthcare professionals and received by family caregivers.
Table 6. Frequency of emotional, practical, and existential support that was received by family caregivers before and after the intervention

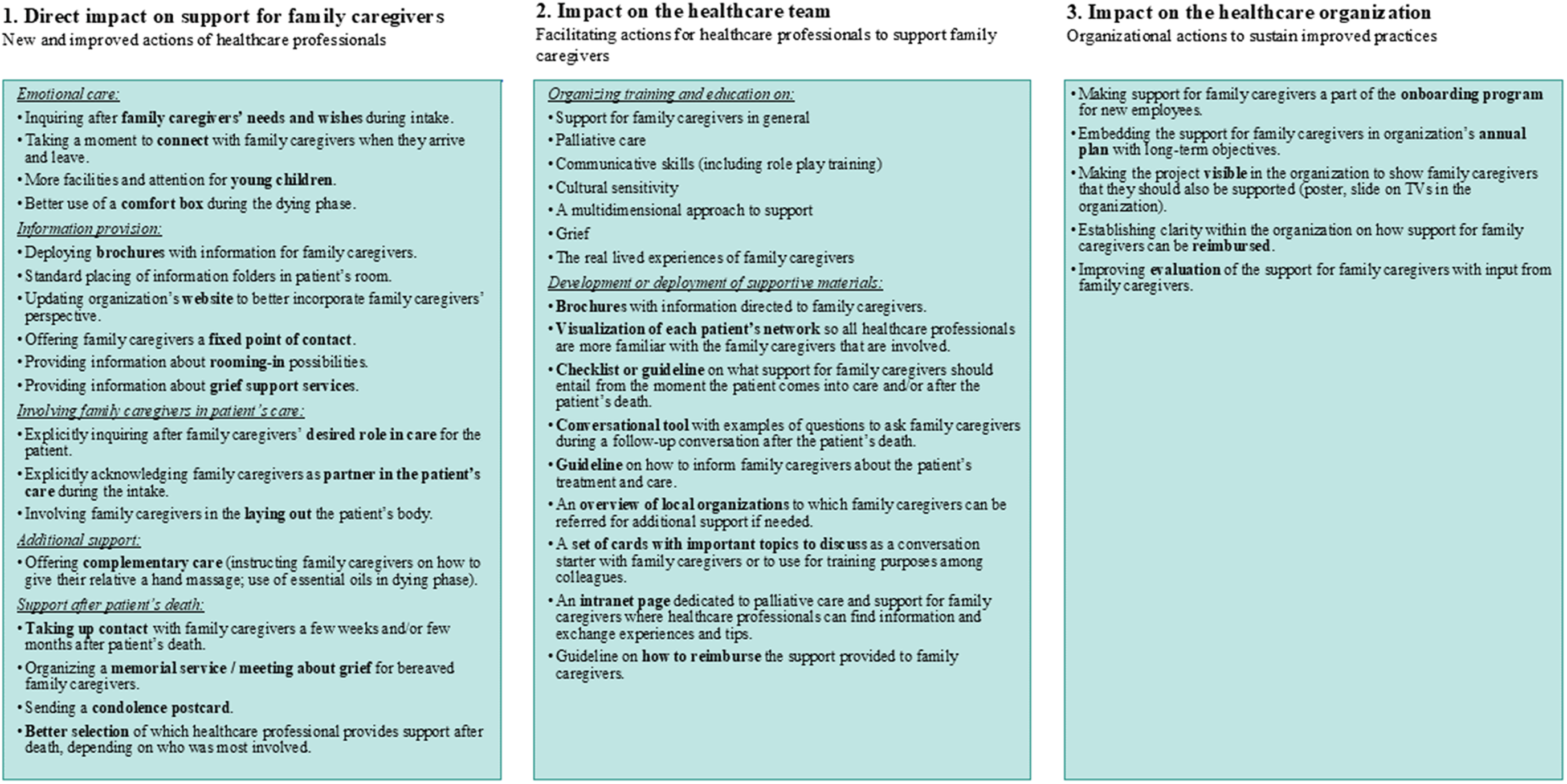
The qualitative data illustrated several and diverse changes in work processes of healthcare professionals. In some cases, this entailed improving existing practices, while in other cases, new practices were introduced. An overview of new and improved actions is presented in the first box of Figure 2. The adjusted work processes related to providing emotional support and information, family caregivers’ involvement in the patient’s care, additional support, and support after the patient’s death. The intervention also contributed to the support for family caregivers becoming more structured: “On the one hand, we did a lot of things that were good, but not in a very structured way. Everyone did it in their own way. And we have been able to really improve this.” (project ambassador during focus group; nursing home).
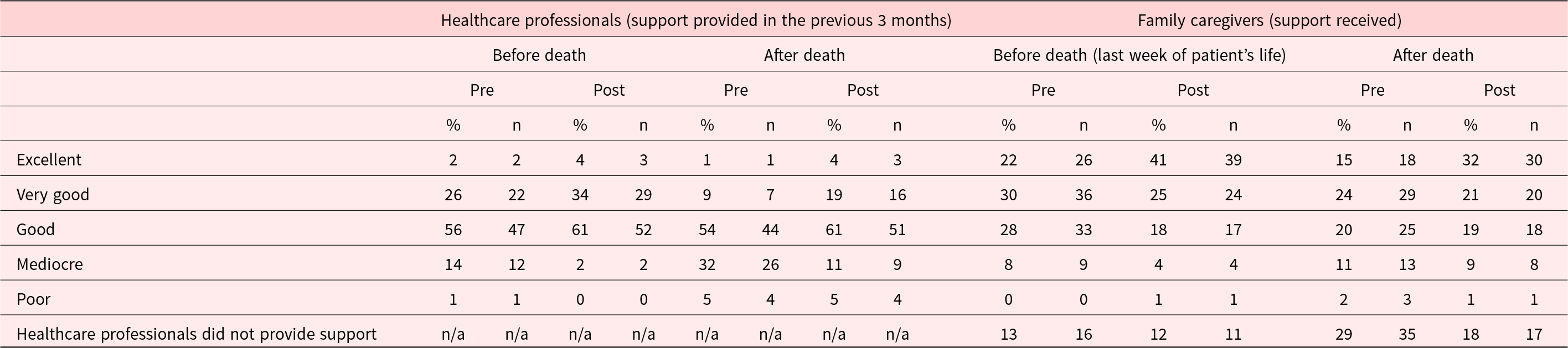
Evaluation of care for family caregivers
After the intervention, more healthcare professionals evaluated the attention they had for family caregivers before the patient’s death in the previous 3 months as “excellent” or “very good” than before (pre: 28%; post: 38%). This was also the case for their evaluation of the care they provided after the patient’s death (pre: 10%; post: 23%; Table 7). The mixed model analysis demonstrated a significant increase in their overall evaluation of the care they provided (β = 0.65; 95% CI: 0.38–0.97; Table 5). With regard to the family caregivers, those in the post-intervention group evaluated the care they received in their relative’s last week of life more commonly as “excellent” or “very good” than those in the pre-intervention group (pre: 52%; post: 66%). This was also the case for their evaluation of care after the patient’s death (pre: 39%; post: 53%; Table 7). The linear regression analysis on their overall evaluation demonstrated a significant increase only among those who received care from home care organizations (β = 2.12; 95% CI: 0.89–3.34; Table 5).
Table 7. Evaluation of care provided by healthcare professionals and received by family caregivers before and after the intervention

In an evaluation report was mentioned that “family caregivers were more satisfied and felt seen” (project ambassador’s evaluation report, transmural organization). Elsewhere was mentioned that, since the intervention, “more positive reactions and expressions of gratitude were expressed [by family caregivers] at the participating hospital department compared to other departments” (researcher’s evaluation report, hospital).
The intervention’s impact on the healthcare team
Support for family caregivers as a part of the workplace culture
Multiple project team members noted that due to the intervention and the increased awareness it brought about, the support for family caregivers became more commonplace and embedded in the workplace culture. In some cases, family caregivers were more often mentioned in electronic health records, and they became more often a topic of discussion during team meetings: “Every healthcare professional is much more aware of the importance of providing good care for the family caregivers. This is increasingly considered as a given.” (manager’s evaluation report; hospice).
Facilitating actions for healthcare professionals
The intervention also helped to better equip healthcare professionals and increase their confidence in supporting family caregivers. In all organizations, one or more educational sessions were organized. Some project teams also worked on creating guidelines or checklists on what support for family caregivers should entail in general or on more specific elements. In some cases, it was explicitly mentioned that such educational sessions and the availability of tools contributed to “confidence among employees in terms of knowledge and skills” (project ambassador’s evaluation report; home care organization). An overview of those facilitating actions is provided in the second box of Figure 2.
Positive spillover effects
In a few instances, the intervention brought about positive spillover effects for healthcare teams. For example, the intervention contributed to better collaboration with other disciplines or among colleagues. Personal experiences came up in the discussions during the journey workshop or during the educational sessions, which contributed to the team becoming more close-knit. This also resulted in more insight into personal experiences of colleagues and strengths and weaknesses with regard to support for family caregivers, which helped to see how team members might complement each other: “You have your specializations within your team. And you can also kind of look at, what kind of family caregiver is in front of you and who would be compatible. And then to start with ‘How would you prefer to die yourself?’ During the training they had to tell each other about that, so then you know: oh those two [healthcare professional and family caregiver] are a match for such-and-such reason. (…) Then you can say, gosh, you know, that’s really your thing, or you’re good at that, would you please take the time to do that, because you are just better suited for it.” (project ambassador during focus group; nursing home).
Furthermore, the intervention and the related discussions made healthcare professionals more aware of the potential impact of a patient’s death on their own wellbeing, leading them to pay more attention to each other when a patient died.
The intervention’s impact on the healthcare organization
The intervention also brought about changes at the organizational level. A researcher’s final evaluation mentioned that the project contributed to “a new culture” in a hospice in which the new working procedures were thoroughly embedded. Furthermore, during a focus group, it was mentioned that the project “set a process of transformation in motion” in the healthcare organization that would continue beyond the 1-year implementation period (project team member; nursing home). In some organizations, actions were executed on the organizational level with the specific aim to sustain the new practices and to further improve the support for family caregivers. An overview of all actions undertaken at the organizational level is provided in the third box of Figure 2. Examples are incorporating the support for family caregivers in the annual plan of the healthcare organization and making the support for family caregivers a part of the onboarding program of new employees. Also, more clarity on reimbursement of support for (bereaved) family caregivers was established in some organizations. Overall, by focusing on the support for family caregivers for a year, support for family caregivers became a part of the organization’s culture.

Figure 2. Changes in practices related to support for family caregivers as demonstrated by qualitative data.
Unachieved goals and barriers
Not all goals that were set were fully achieved in all healthcare organizations during the year of implementation. In some cases, despite the action plans generally being considered feasible by project team members, some intended actions to achieve the goals turned out to be difficult to implement in routine practice in a 1-year period. Examples of actions that were not, or to a limited extent, executed, are: standard use by healthcare professionals of a newly developed checklist on support for family caregivers (goal: create more clarity for healthcare professionals on what support for family caregivers should entail), standard distribution of brochures to family caregivers (goal: improve information provision), involving family caregivers in multidisciplinary team meetings (goal: improve family caregivers’ involvement in the patient’s care), and keeping track of positive experiences with the patient while they were in care to give this to family caregivers after the patient’s death (goal: improve the support provided after the patient’s death). Frequently mentioned reasons for (partly) unachieved goals were staff shortages and high workload, which made it difficult to find the time to execute the action plan and to keep the project at the forefront of healthcare professionals’ minds. Other reasons were limited confidence of healthcare professionals in their own skills and knowledge to support family caregivers, a lack of managerial support, the absence of a strong project leader who had sufficient time for the project, and large ongoing organizational changes, such as mergers or expansions.
Discussion
In this study, a mixed-methods effect evaluation was conducted of a tailored organizational intervention on the support for family caregivers of patients with life-threatening diseases. Quantitative findings were mixed with statistical analyses indicating improved support for family caregivers, especially in healthcare professionals’ reports, but this pattern not being consistent across all types of support and all outcome measures. Qualitative findings showed an increased awareness of healthcare professionals of the importance of supporting family caregivers and numerous improvements in healthcare professionals’ work processes related to emotional care, information provision, family caregivers’ involvement in the patient’s care, and support after the patient’s death.
Family caregivers’ reports of support that was received after the patient’s death showed more improvement compared to the support before the patient’s death. This may be due to recollections of support after death being more distinct as it consists of fewer interactions with fewer healthcare professionals (Boven et al. Reference Boven, Dillen and van den Block2022; Coelho et al. Reference Coelho, Albuquerque and Neto2025). Furthermore, in some organizations, support after death was (re)introduced as part of the intervention, whereas support before death was already present to a certain extent prior to the intervention. Therefore, it can be understood that the contrast between the pre- and post-measurement reports of support received after the patient’s death was more pronounced.
The mixed quantitative findings in this study may in part be attributed to the challenges of quantitatively assessing the effectiveness of a complex intervention that allows a great degree of flexibility in implementation. It has been emphasized in multiple studies that capturing the effect of tailored, context-specific interventions with quantitative measures generally falls short (Datta and Petticrew Reference Datta and Petticrew2013; Jansen et al. Reference Jansen, Bal and Bruijnzeels2006; Skivington et al. Reference Skivington, Matthews and Simpson2021). Although the core components of the present intervention were standardized, considerable variation existed in the specific support types that were targeted by each participating healthcare organization. Therefore, standardized quantitative outcome measures across all organizations may not fully capture the impact of the intervention (Skivington et al. Reference Skivington, Matthews and Simpson2021).
Taking all data into consideration, it can be concluded that the intervention had a positive impact on the support for family caregivers. However, not all goals were (fully) achieved. This is not surprising as literature has reported an average of 10% of improvement on main targets after implementation of interventions aiming to change clinical practice (Grol and Grimshaw Reference Grol and Grimshaw2003). Various challenges to implementation are known, such as low resources and high workload of healthcare professionals (Geerligs et al. Reference Geerligs, Rankin and Shepherd2018; Parmar et al. Reference Parmar, Sacrey and Anderson2022). Taking this into consideration, a year of implementation may be insufficient to sustainably improve various elements of support for family caregivers. The intervention may need to be better integrated into the organization’s culture, which can be achieved by reevaluating the support for family caregivers after a year of implementation and establishing a new action plan with refined (partly) unmet goals and/or deciding on new areas for improvement. As such, support for family caregivers can be improved in phases, depending on what is feasible within the organization at that moment in time.
The intervention has appealing advantages for clinical practice. First, the intervention’s flexibility makes it suitable for any healthcare organization that provides care for patients with life-threatening diseases. Depending on what is feasible within their organization, project teams can decide on the extensiveness of their goals and the scale of implementation. Second, as the healthcare professionals themselves are in charge of the action plan’s content, a sense of ownership is facilitated, which increases chances of success and sustainability of the intervention’s effects (Cowie et al. Reference Cowie, Nicoll and Dimova2020). Last, as the intervention aims to modify the everyday practices of healthcare professionals, it is complementary to existing interventions that directly target family caregivers through, for instance, structured needs assessment, psychoeducation, skills training, facilitating their self-care or organizing family meetings (Aoun et al. Reference Aoun, Toye and Slatyer2018; Becqué et al. Reference Becqué, Rietjens and van Driel2019, Reference Becqué, van der Wel and Aktan-Arslan2023; Gonella et al. Reference Gonella, Mitchell and Bavelaar2022; Theißen et al. Reference Theißen, Ullrich and Oechsle2024). The current intervention offers a framework within which such interventions can be integrated if they align with the action plan. When implementation of the intervention is considered, certain preconditions should always be met, the most important of which are managerial support, allocated time for project team members to manage the trajectory, and the absence of large reorganizations or other ongoing projects (Cowie et al. Reference Cowie, Nicoll and Dimova2020; Geerligs et al. Reference Geerligs, Rankin and Shepherd2018; Mathieson et al. Reference Mathieson, Grande and Luker2019).
Strengths and limitations
A strength of this study is its mixing of quantitative and qualitative methods, enabling a deep understanding of the intervention’s effect on support for family caregivers. However, the study also has limitations. First, uncertainty exists as to whether family caregivers’ survey responses were based solely on their experiences with the participating healthcare organization, as they may also have received care from other, non-participating healthcare organizations (Wolf et al. Reference Wolf, Niederhauser and Marshburn2021). Therefore, their responses may partially reflect experiences with those other healthcare organizations (e.g., their GP), which limits the extent to which they can be interpreted as reflecting the impact of the intervention. Second, the vast majority of participating healthcare professionals were nursing staff, limiting the generalizability of the findings to other professions. Third, as a suitable survey did not exist, the survey that was used was not validated. Consequently, the reliability and validity of the survey items and outcome measures are unknown. Fourth, the pre- and post-surveys were distributed to family caregivers of patients who had died in the previous 6 months. As a result, the time between the patient’s death and survey completion varied across the respondents. Furthermore, the post-survey responses partly reflect experiences of support midway through implementation. At that time, not all actions of the action plans had been fully executed. Consequently, the family caregiver survey results may not fully capture the intervention’s impact. Fifth, the small sample sizes within each healthcare setting (especially the nursing home and transmural setting) limited the statistical power of the mixed model and linear regression analyses, warranting thoughtful interpretation of the outcomes of these analyses. Last, differences likely existed in the effect of the intervention on the support for family caregivers across healthcare settings and the different healthcare organizations. However, as each organization worked on its own goals, meaningful comparisons could not be made.
Future research
Future research is necessary to further explore the intervention’s impact on the support for family caregivers. First, uncertainty exists regarding the sustainability of the improvements that have been implemented. The long-term effect of the intervention on the support for family caregivers should be investigated, including the barriers and facilitators to its sustainment. Second, research on a larger scale is needed to explore whether the intervention’s effectiveness differs for different healthcare settings or professions. Third, future research may target volunteers as they also have an important role in palliative care provision (Bloomer and Walshe Reference Bloomer and Walshe2020).
Conclusion
In conclusion, a tailored intervention in healthcare organizations improves the support provided to family caregivers. Due to its flexibility, the intervention can be adopted across all kinds of healthcare organizations. However, preconditions such as managerial support and sufficient time for project teams should be met. Future research should investigate the long-term effect of the intervention and the barriers and facilitators to sustaining it.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1478951525101582.
Acknowledgments
We would like to thank the healthcare organizations who participated in our study, especially the project team members who carried out the intervention, and the family caregivers who participated in the survey study. We are indebted to Willemijn Boere, MSc, and Dr.ir. Marieke Sonneveld of the Delft University of Technology for the development of the “Family caregiver journey” workshop.
Funding statement
Funding was provided by the Netherlands Organisation for Health Research and Development (ZonMw; 844001706).
Competing interests
The authors declare none.