Introduction
Advancements in radiotherapy have revolutionized cancer treatment, allowing for greater precision and effectiveness in targeting tumours while minimizing damage to surrounding healthy tissue. Reference Chen and Kuo1 Central to these advancements is the use of multileaf collimators (MLCs), which are devices within linear accelerators (LINACs) that shape the radiation beam to conform to the three-dimensional shape of the tumour. Accurate MLC modelling within treatment planning systems (TPS) is crucial for ensuring that the dose delivered to the patient matches the treatment plan, thereby optimizing therapeutic outcomes and reducing side effects. Reference Chui2
Historically, MLC modelling in the Eclipse TPS (Varian Medical Systems Inc., Palo Alto, CA) has relied on relatively simplified models. Up to version 17.0 (V17.0), these models primarily utilized the dosimetric leaf gap (DLG) and leaf transmission factor (LTF) parameters. Reference Hsu3,Reference Rostami, Barzegar, Usman, Paloor, Mkanna, Al-Sabahi and Hammoud4 The DLG accounts for the effective width of the radiation beam passing through nominally closed MLC leaves with rounded tips, while the LTF represents the amount of radiation transmitted through the MLC leaves. These parameters were designed to improve dose calculation accuracy, especially for dynamic treatments such as intensity-modulated radiotherapy and volumetric modulated arc therapy (VMAT). However, these original models had notable limitations in accurately predicting dose distributions, particularly in scenarios involving complex leaf movements, small field sizes and off-axis regions. Reference Vieillevigne, Khamphan, Saez and Hernandez5
The DLG parameter in Eclipse V17.0 and earlier versions is applied during the treatment planning process to adjust the fluence map, representing the beam intensity. The dose calculation algorithm of the Eclipse TPS, which models the leaf ends as rectangular instead of round, incorporates the DLG parameter to account for leaf transmission by adjusting the positions of the leaf tips during fluence calculation. 6 Each leaf tip of the MLC leaf pair is shifted back by half the DLG value, ensuring that the separation between a fully closed leaf pair matches the DLG value. However, during treatment delivery, discrepancies can arise due to the simplifications inherent in the DLG model, particularly for complex and off-axis MLC movements. Reference Stanslaw, Fred and Kirpal7 Many studies showed the determination of the DLG value in Eclipse V17.0 and earlier versions often proved insufficiently accurate for clinical needs, necessitating tuning of DLG to achieve the best dosimetric agreement between measurement and calculation. Reference Vieillevigne, Khamphan, Saez and Hernandez5,Reference DiCostanzo and Ayan8,Reference Middlebrook9
With the introduction of Eclipse version 18.0 (V18.0) and subsequent versions, a new modelling approach, known as the enhanced leaf model (ELM), was implemented. This model incorporates a more detailed geometric representation of the MLC, capturing the intricacies of the leaf tip shape and the thickness of the leaf body through advanced ray tracing techniques. The leaf gap (LG) parameter in the ELM more accurately represents the physical characteristics of the MLC leaves. This includes the modelling of rounded leaf tips, drive screw cutouts and leaf body thickness, all incorporated through divergent ray tracing across the leaf structure. Reference Van Esch, Kulmala, Rochford, Kauppinen and Harju10 Compared to DLG values used for non-ELM MLCs and those used with older algorithm versions, DLG is defined differently for ELM MLCs and can have negative values. The DLG in V18.0 and later corresponds more strongly to the mechanical gap between ‘closed’ leaf ends on the device, which can result in a negative DLG value. 11
During treatment planning in Eclipse V18.0, the DLG parameter is used to adjust the fluence map more precisely by taking into account the true shape and position of the MLC leaves. This results in a more accurate representation of the beam’s transmission through the MLC, considering the varying path lengths and the actual physical structure of the leaves. During dose calculation, this detailed modelling allows for better prediction of the dose distribution, particularly for small field sizes and complex geometries. In treatment delivery, the ELM model aims to reduce discrepancies observed with the traditional DLG model, providing a more accurate dose delivery to the patient. Reference DiCostanzo and Ayan8
Accurate MLC modelling is particularly important for VMAT and stereotactic body radiotherapy (SBRT) techniques, where dose delivery depends on rapid and complex leaf movements that generate many small, irregular apertures. Errors in representing leaf-tip geometry, interleaf transmission and dosimetric LG can propagate to discrepancies in fluence maps and dose distributions, especially in off-axis and small-field regions. Reference Rostami, Barzegar, Usman, Paloor, Mkanna, Al-Sabahi and Hammoud4,Reference Vieillevigne, Khamphan, Saez and Hernandez5 These issues are amplified in SBRT, which involves small target volumes, sharp dose gradients and hypofractionated regimens. ICRU Report 91 12 highlights the unique challenges of small-field dosimetry in stereotactic radiotherapy, emphasizing the need for accurate beam modelling and verification to ensure treatment quality. In this context, evaluating the ELM compared with the traditional model is clinically important, as it directly addresses these challenges and provides insight into whether the newer modelling approach improves dose calculation accuracy and deliverability in small and large field VMAT applications.
The objective of this study is to compare and evaluate the effectiveness of MLC modelling in Eclipse V18.0 (using the ELM method) against the traditional MLC modelling in Eclipse V16.1 (using DLG and LTF). This evaluation focuses on the dosimetric accuracy and deliverability in VMAT and lung SBRT treatments by assessing the gamma index pass rates post-treatment delivery for both Eclipse V16.1 and V18.0 plans. The gamma index is a widely used metric in radiotherapy that compares the calculated dose distribution to the measured dose distribution, providing a quantitative measure of the agreement between the two.
By conducting this comprehensive evaluation, this study aims to determine whether the ELM in Eclipse V18.0 and later versions provides superior dose accuracy compared to the traditional model. The findings have the potential to inform clinical practice by supporting the adoption of the ELM in newer Eclipse versions and highlighting the importance of accurate MLC modelling techniques to achieve optimal patient outcomes in radiotherapy.
Materials and methods
LINAC, MLC and TPS
All measurements were performed on Varian TrueBeam machines (Varian Medical Systems, Palo Alto, CA) equipped with a 120-leaf Millennium MLC. The beams used in this study had energies of 6MV, 10MV, 6FFF and 10FFF. Prior to collecting any data, the LINAC underwent and successfully passed dosimetric and mechanical testing through the machine performance check.
Treatment plans were developed using the Eclipse TPS (Varian Medical Systems, Palo Alto, CA), utilizing two distinct versions. Eclipse V16.1 employed the original MLC modelling approach, based on the DLG and leaf transmission factor (LTF) parameters. In contrast, Eclipse V18.0 incorporated the ELM, which features advanced ray tracing and an improved geometric representation of the MLC leaves.
MLC modelling parameters:
For Eclipse V16.1, DLG and LTF parameters were calculated and for Eclipse V18.0, the ELM parameters, including the DLG and LTF in respect of advanced ray tracing features and details of MLC design, optimized by TPS per Vendor guidelines. 6,Reference Stanslaw, Fred and Kirpal7
MLC modelling verification
For the verification of MLC modelling in both versions of the TPS, measurements were taken under the following conditions: a 10 × 10 cm2 open field, a fully blocked field by MLC Bank A, a fully blocked field by MLC Bank B and sweeping gap fields with gap sizes of 4, 6, and 20 mm, moving from left to right. The measurements were performed using the source-to-axis distance technique, with a source-to-surface distance of 90 cm, at a depth of 10 cm in a solid water phantom, with the gantry set to 0 degrees. A Farmer chamber (TN30013) with a length of 2.3 cm was used for dose measurements. The percentage dose differences between the measured values and the calculated values by the TPS were compared for both MLC models, Eclipse V16.1 and Eclipse V18.0.
Patient selection and data collection
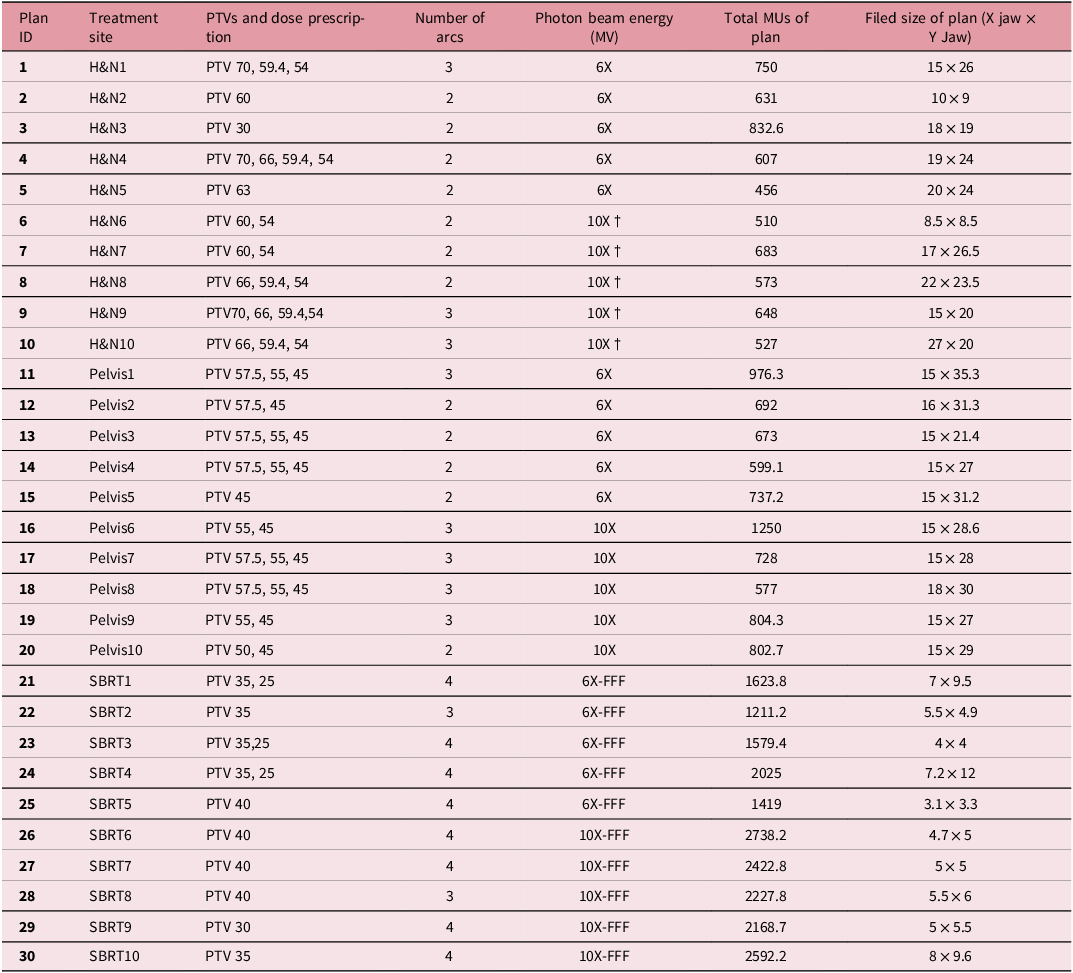
The study includes a retrospective analysis of 30 patients treated with VMAT. The cohort is divided into three groups, including Head-and-Neck (H&N) Cases (10 patients), Pelvic Cases: (10 patients) and lung SBRT Cases (10 patients). Although all plans were delivered using the VMAT technique, lung SBRT cases were analysed separately to reflect their stereotactic nature and small-field characteristics. Detailed demographic and treatment information for each case is provided in Table 1. For ethical considerations, patient data were anonymized. To ensure a comprehensive energy-specific comparison by site and modulation level (6MV, 10MV, and FFF beams), a subset of 5 cases of H&N cases was re-optimized at 10MV for research-only analysis; these plans were not used for patient treatment.
Table 1. Details of clinical VMAT plans (H&N, pelvic and lung SBRT) used for evaluation of enhanced leaf model (V18) vs. original MLC model (V16.1) in Eclipse TPS

†Indicates research-only re-optimization at 10MV for comparative analysis; not clinically delivered.
Treatment planning methodology
For each case, including VMAT and lung SBRT treatment, plans were generated using photon optimizer (PO) algorithms in Eclipse TPS, ensuring consistency in the planning approach. The PO algorithm was used for optimizing treatment plans, applying identical clinical goals and constraints for all cases. The Acuros XB (AXB) algorithm was used for the final dose calculation in both versions of Eclipse (V16.1 and V18.0), with a grid size of 2.5 mm for VMAT and 1.25 mm for SBRT plans.
All VMAT and Lung SBRT plans used a coplanar arc geometry, with between 2 and 4 arcs depending on the treatment site, as detailed in Table 1. Collimator angles were alternated between arcs (typically 15°–30° offsets) to reduce tongue-and-groove effects. Gantry rotation spanned nearly 360° for pelvic and head-and-neck cases, while SBRT arcs were tailored to lesion location to optimize OAR sparing. Jaw tracking was enabled for all plans. These parameters and more details, summarized in Table 1, ensure that potential confounding effects from geometry and planning methodology are minimized, allowing for a direct comparison of MLC modelling between V16.1 and V18.0.
Evaluation of dosimetric impact of the MLC modelling in V16.1 and V18.0 in Eclipse TPS
In the initial phase of evaluating the dosimetric impact of MLC modelling between Eclipse TPS versions V16.1 and V18.0, we performed a recalculated VMAT Picket Fence (PF) test. This involved dynamically controlling the central 40 pairs of leaves (leaf numbers 11 to 50) from both the left (X1) and right (X2) leaf banks, moving them from left to right. The leaves paused at 1.5 cm intervals to create ten 0.2 × 20 cm gaps. The beam was delivered while the gantry rotated between 179 and 187 degrees, with a constant dose rate, leaf speed and gantry rotation maintained throughout the arc. This setup allowed us to directly observe the effect of MLC modelling in Eclipse TPS V16.1 and V18.0 on the agreement between measured and planned MLC tests. Images were captured using an aSi-1200 Electronic Portal Imaging Device (EPID), mounted on the gantry via a robotic arm. The EPID had an active dosimetry area of 40 × 40 cm², with a 1,190 × 1,190 pixel array and a pixel pitch of 0.336 mm. We compared the delivered PF test results with the plans generated by the TPS for both MLC modelling configurations using global gamma index evaluation.
In the next phase of the study, for patient-specific quality assurance, verification plans were generated using the AXB algorithm within the Eclipse Portal Dosimetry system. Among the three available algorithms—Analytical Anisotropic Algorithm, AXB and Portal Dose Image Prediction— to maintain consistency between the original plans and the recalculated verification plans, AXB was selected to calculate predicted portal dose distributions, which were then compared with EPID measurements for gamma index analysis. Gamma index was calculated for each treatment plan using three criteria: 1%/1 mm, 2%/2 mm and 3%/3 mm in 10% threshold dose distribution. Pass rates were compared between the traditional MLC model (Eclipse V16.1) and the ELM (Eclipse V18.0) to assess the agreement between the calculated and measured dose distributions. Differences in gamma index pass rates between the two TPS versions were analysed using paired t-tests for each treatment group (H&N, pelvic, Lung SBRT).
Results
DLG and LTF values for Eclipse version 16.1 and Eclipse version 18.0
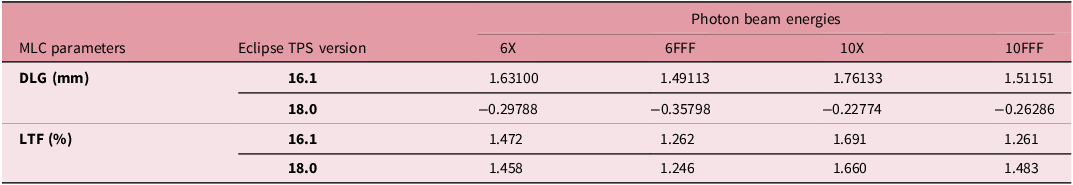
DLG and LTF values for both versions of Eclipse TPS (V16.1 and V18.0) for four different energies, including 6X, 6FFF, 10X and 10FFF, are summarized in Table 2.
In Eclipse Version 18.0, as shown in Table 2, the DLG is defined differently for the ELM-based MLC modelling and often exhibits negative values, better reflecting the concept of MLC tip retraction during plan delivery. There is no correlation or similarity between the DLG values in Versions 18.0 and 16.1. However, the LTF values are very similar across both versions, with the differences being negligible.
Table 2. DLG and LTF values of Eclipse version 16.1 and Eclipse version 18.0 for 6MV, 6FFF, 10MV, and 10FFF photon beams

MLC modelling verification for Eclipse version 16.1 and Eclipse version 18.0
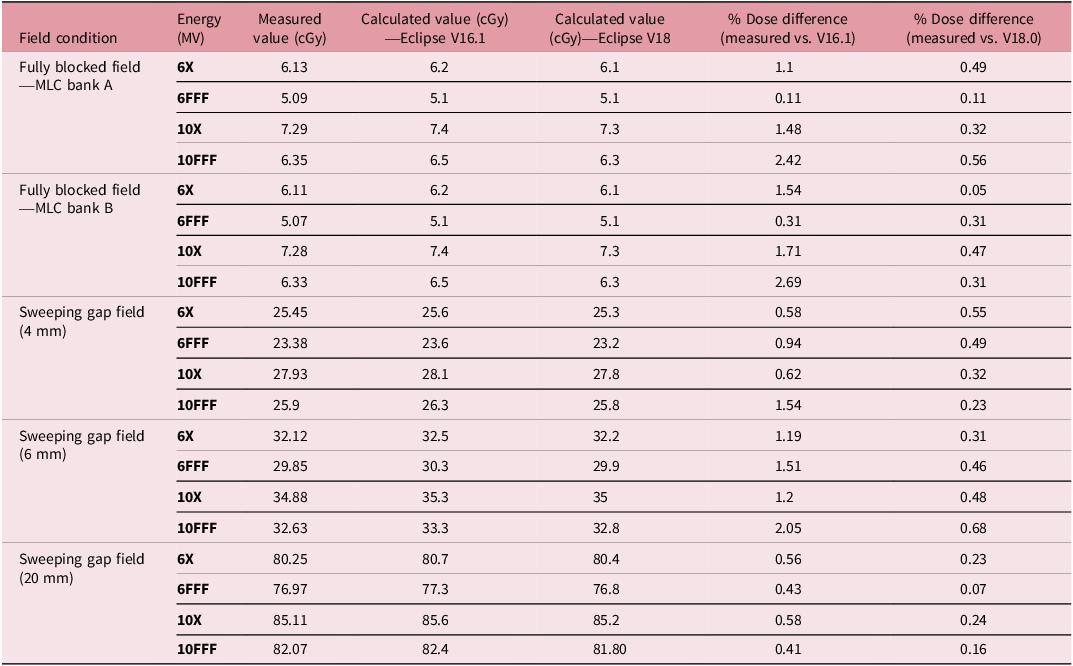
Table 3 presents the measured values, calculated values for both Eclipse TPS versions V16.1 and V18.0 and the percentage differences for a 10 × 10 cm² open field, a fully blocked field by MLC Bank A, a fully blocked field by MLC Bank B and sweeping gap fields with gap sizes of 4, 6 and 20 mm (moving from left to right).
Table 3. Comparison of measured and calculated dose values for various field configurations and eclipse TPS versions (V16.1 vs. V18.0)

As shown in Table 3, for all energies and verification fields, Eclipse V18.0, utilizing the ELM, exhibited smaller dose differences compared to measurements than Eclipse Version 16.1.
Dosimetric impact of the MLC modelling in Eclipse version 16.1 and Eclipse version 18.0
In this study, the AXB dose calculation algorithm in Eclipse TPS versions V16.1 and V18.0 was utilized for dose calculation. This algorithm requires the DLG and LTF values for any plan that utilizes MLC. To assess the dosimetric impact of MLC modelling at Eclipse TPS version, for each photon beam energy, including 6MV, 10MV, 6FFF, and 10FFF, the intensity profiles of the PF plans calculated by Eclipse TPS V16.1 and V18.0 on the central axis are compared with the intensity profile of the measured PF test by EPID (Figure 1).

Figure 1. Cross-line intensity profile of PF test measured by EPID in comparison with PF plans calculated by Eclipse treatment planning system for AXB V16.1 and AXB V18.0 for 6MV, 6FFF, 10MV and 10FFF photon beams.
Figure 2 displays the global gamma index pass rates (3%/3 mm), (2%/2 mm) and (1%/1 mm) between the measured PF test and the PF plans created in the TPS for Eclipse TPS versions V16.1 and V18.0. Eclipse V18.0 demonstrated the best agreement between the measurement and the planned PF pattern.

Figure 2. Global gamma index pass rates (3%/3 mm), (2%/2 mm) and (1%/1 mm) between the measured Picket Fence test and the Picket Fence plans created in the Eclipse TPS for AXB version 16.1 and AXB version 18.0.
Figure 3 shows the average gamma index pass rates (3%/3 mm, 2%/2 mm and 1%/1 mm) for patient-specific verification using portal dosimetry for 60 clinical VMAT plans, including 30 different cases, each one recalculated twice with AXB V16.1 and V18.0. The AXB algorithm in Eclipse V18.0, which utilizes the ELM for MLC modelling, showed higher gamma index pass rates across all energies. Significant differences in gamma index pass rates (1%/1 mm) have been observed between the AXB algorithm in Eclipse V18.0 and Eclipse V16.1 for all energies. As seen in Figure 3, for 6X beam, the gamma index pass rates (1%/1 mm) increased from 70% to 85%, and for 10X beams, it rose from 87.8% to 92.1%. Similarly, for flattening filter-free (FFF) beams, 6FFF showed an improvement from 82.4% to 84.96%, and 10FFF increased from 82.4% to 88.1%.

Figure 3. Percentage of average dose gamma index pass rate (3%/3 mm), (2%/2 mm) and (1%/1 mm) of patient-specific verification using portal dosimetry for photon beam energy, including 6MV, 10MV, 6FFF and 10FF, for both TPS versions (V16.1 and V18.0).
Discussion
This study aimed to compare the dosimetric accuracy between the traditional MLC modelling in Eclipse V16.1 and the ELM in Eclipse V18.0. The results demonstrated significant improvements (p < 0.05) in dose calculation accuracy, treatment deliverability and gamma index pass rates with the ELM, particularly for VMAT plans (H&N, pelvic and lung SBRT) treatments.
The ELM in Eclipse V18.0 provides a more sophisticated geometric representation of the MLC, accounting for the physical structure of the leaf tips and gaps between leaves. The DLG and LTF parameters used in V16.1, while effective for standard treatments, often failed to capture the complexity of MLC leaf movements in MLC leaf pattern tests like PF and highly dynamic treatments, especially for small field sizes and off-axis regions. Reference Van Esch, Kulmala, Rochford, Kauppinen and Harju10 The results of this study demonstrate that the ELM significantly reduces these dose discrepancies (p < 0.05). This improvement aligns with earlier studies that have shown the benefits of enhanced MLC modelling in improving dose calculation accuracy for complex cases. Reference Van Esch, Kulmala, Rochford, Kauppinen and Harju10
Validation of MLC modelling was performed using closed leaf and sweeping gap field tests, which are sensitive to both static and dynamic MLC movements. The results of this validation (see Table 3) showed that Eclipse V18.0 exhibited consistently smaller dose differences when compared to V16.1 across all photon energies and field configurations. For example, in the fully blocked field by MLC Bank A for 6MV, the percentage dose difference was reduced from 1.1% in V16.1 to 0.49% in V18.0, while for 10FFF, the difference dropped from 2.42% to 0.56%. These findings underscore the improved accuracy of the ELM in Eclipse V18.0, which provides a more accurate representation of the physical behaviour of MLC leaves. Similarly, the sweeping gap field test, which simulates dynamic leaf movement across the treatment field, demonstrated lower percentage dose differences with Eclipse V18.0. For the 6 mm sweeping gap field at 6MV, the dose difference decreased from 1.19% in V16.1 to just 0.31% in V18.0, while for 10FFF, the difference dropped from 2.05% to 0.68%. This reduction in dose discrepancy highlights the ELM’s superior ability to model complex MLC movements, which is particularly crucial for the accurate delivery of treatments like VMAT and SBRT.
In next step of study, the PF test was used to evaluate the performance of the MLC model in both versions of Eclipse. This test is particularly useful for assessing the dynamic accuracy of MLC movements during arc-based treatments like VMAT. The gamma index pass rates for the PF test under the 1%/1mm criterion showed a marked improvement with Eclipse V18.0 for all photon beam energies. For 6MV, the gamma pass rate (1%/1 mm) increased from 75% in V16.1 to 91% in V18.0, and for 10FFF, it improved from 71% in V16.1 to 90% in V18.0. These improvements confirm that the ELM provides a more accurate geometric and dosimetric representation of MLC leaf positioning, which is crucial for high-precision treatments such as SRS and SBRT. Our findings align with earlier reports that highlighted the limitations of traditional MLC modelling. Vieillevigne et al. and Middlebrook et al. demonstrated that tuning of the dosimetric LG was often required to achieve acceptable accuracy in small-field stereotactic plans, underscoring the need for improved modelling. Reference Vieillevigne, Khamphan, Saez and Hernandez5,Reference Middlebrook, Sykes, McCavana, Moore and Thwaites13
Furthermore, the analysis of clinical cases revealed a significant improvement in gamma index pass rates across all energies and treatment sites (p < 0.05). For example, in the head-and-neck cases, the average gamma pass rate (1%/1 mm) increased from 70% in V16.1 to 91.8% in V18.0. Similarly, for the lung SBRT cases, the pass rate for 1%/1 mm increased from 82.4% in V16.1 to 87.3% in V18.0 (Figure 3). These results are particularly important for SRS and SBRT treatments, where even small dosimetric errors can have a significant impact on clinical outcomes. The clinical importance of accurate MLC modelling is further emphasized by ICRU Report 91, which highlights the challenges of small-field dosimetry in stereotactic treatments and the potential clinical consequences of dose inaccuracies. 12
The improvements observed with the ELM in Eclipse V18.0 are clinically significant, particularly in complex treatments like VMAT and lung SBRT. The reduction in dose discrepancies, as evidenced by PF tests and clinical VMAT cases, suggests that the ELM provides a more reliable and accurate representation of MLC behaviour. This improved accuracy is essential for reducing the risk of treatment errors and ensuring that the prescribed dose is delivered precisely to the target volume. Reference Rostami, Castero Neto, Prasad, Khalid and Hammoud14
The findings of this study align with previous research that has demonstrated the dosimetric advantages of the ELM. Ann Van Esch et al. Reference Van Esch, Kulmala, Rochford, Kauppinen and Harju10 found excellent agreement between measurements and dose calculations with the new ELM model. They confirm that the ELM is more accurate than the original MLC modelling, particularly for dynamic treatments like VMAT and SBRT.
This study has certain limitations. First, intracranial SRS plans were not included because of their limited availability in our dataset. Instead, we analysed lung SBRT cases, which also involve small-field, highly modulated VMAT deliveries. While SBRT is not identical to SRS, these cases provide a reasonable surrogate for evaluating the performance of the ELM in small-field conditions. Thus, our findings still offer meaningful insight into the potential benefits of ELM for stereotactic treatments, in line with previously published SRS-focused studies. Reference Vieillevigne, Khamphan, Saez and Hernandez5,Reference Van Esch, Kulmala, Rochford, Kauppinen and Harju10
An additional limitation of this work is the relatively small sample size (30 patients), divided across three treatment groups. While sufficient to demonstrate consistent trends, the limited number of cases may restrict the statistical power and the ability to fully capture inter-patient variability.
Conclusion
In conclusion, the ELM in Eclipse V18.0 provides improved accuracy in treatment plan deliverability compared to the traditional MLC model in Eclipse V16.1. The improvements in gamma index pass rates, particularly under the most stringent criteria (1%/1 mm), highlight the clinical significance of the ELM for high-precision treatments like VMAT, SBRT and SRS. These findings support the adoption of Eclipse V18.0 in clinical practice, where the enhanced accuracy of the ELM can improve patient outcomes and optimize the delivery of complex radiotherapy treatments.
Acknowledgment
Open Access funding provided by the Qatar National Library.
Competing interests
The authors declare that there are no conflicts of interest.