Introduction
China is the largest developing country in the world. China’s primary medical technology and medical development level play vital roles worldwide. In China, 50.32% of the population lives in rural areas (Liang and Lv, Reference Liang and Lv2019). Rural doctors constitute an essential part of China’s medical and health team, accounting for 20.71% of health technicians (Chen et al., Reference Chen, Li, Pan, Liu, Ye, Ge, Yang and Han2019). They are significant human resources that directly provide preventive health care and basic medical services for most farmers (Lin et al., Reference Lin, Wei and Zhang2014). In particular, since the beginning of the 21st century, the government has issued a series of policy documents related to rural doctors, who have become important providers of basic medical and public health services. They play a crucial role in the rural medical system and deliver health services to thousands of households (Liu, Reference Liu2004; Zhang et al., Reference Zhang, Chen, Yang, Pan, Li, Yue, Huang, Mao, Zhang and Ma2019), which is a force that cannot be ignored in carrying out rural health work and promoting rural primary health care (Zhang and Yang, Reference Zhang and Yang2019). Given the severe shortage of health resources in rural areas, rural doctors play an important role in providing basic health manpower and basic health services to the rural population (Hu et al., Reference Hu, Zhu, Fu, Zhang, Zhao, Hanson, Martinez-Alvarez and Liu2017). The training and use of rural doctors who can ‘stay and work’ has solved many medical and health problems for rural residents. The health of rural doctors directly affects the quality of primary health care, the relationship between doctors and patients, and even the stability and development of rural society (Wu et al., Reference Wu, Zhao, Wang and Wang2010). Therefore, maintaining the health of rural doctors is an important guarantee for the implementation of various types of health work in rural areas.
In addition to physical health, attention to health conditions should also be given to mental health, as the two factors are closely interconnected (Happell et al., Reference Happell, Wilson, Platania-Phung and Stanton2017). Mental health can be defined as the absence of mental disease or it can be defined as a state that also includes the biological, psychological, or social factors that contribute to an individual’s mental state and ability to function within the environment (Manwell et al., Reference Manwell, Barbic, Roberts, Durisko, Lee, Ware and McKenzie2015). Mental health impacts individuals’ personal and social functioning (Dore and Caron, Reference Dore and Caron2017).
With the development of the social economy, improvements in living standards, the advancement of new medical reform policies, and the enhancement of public awareness of medical care, higher requirements are put forward for medical quality and medical safety. Consequently, the psychological pressure and work intensity of medical staff are greater than those of other occupations. Moreover, tense doctor-patient relationships further increase the pressure on medical staff, making mental health problems increasingly prominent (Gazelle et al., Reference Gazelle, Liebschutz and Riess2015; Lv et al., Reference Lv, Yang and Tian2018). Research shows that doctors report a higher rate of depression and anxiety compared to the general population (Pattani et al., Reference Pattani, Constantinovici and Williams2001; Garelick et al., Reference Garelick, Gross, Richardson, von der Tann, Bland and Hale2007), with a greater incidence of mental illness (Pappas et al., Reference Pappas, Gouva, Gourgoulianis, Hatzoglou and Kotrotsiou2016; Harvey et al., Reference Harvey, Epstein, Glozier, Petrie, Strudwick, Gayed, Dean and Henderson2021).
At present, investigations on doctors’ mental health in China have focused mainly on the top three hospitals, general hospitals and specialized hospitals (Wang et al., Reference Wang, Hua and Wang2013; Lin et al., Reference Lin, Deng, Xie and Pan2013; Lin et al., Reference Lin, Wang, Hu, Zhang, Zhai and Cai2017). They rarely involve primary hospitals or community health service centres. There are few investigations and studies on rural doctors. The sample size is relatively small, and the research period is relatively long (Chen et al., Reference Chen, Wang and Qu2009; Wu, Reference Wu2011; Wang and Wang, Reference Wang and Wang2014), which is insufficient for research on the influence on the mental health of rural doctors and its influencing factors in the new era and environment.
The geographical location of Hebei Province is very important. Surrounding Beijing, the political, economic, and cultural centre of China, it serves as a link between the Northeast Region and various provinces within Shanhaiguan, making its status highly representative. To clarify the mental health status of rural doctors in Hebei Province, this survey randomly selected rural doctors. The Symptom Checklist-90 (SCL-90) was used to evaluate their mental health status, while multifactor analysis identified the factors influencing it. This study provides a scientific basis for health administrations to formulate relevant policies, contributing to the improvement of rural doctors’ psychological condition and their ability to provide primary health care, ultimately fostering the development of the primary health care system.
Methods
Setting
The survey subjects are rural doctors in 11 prefecture-level cities, including Shijiazhuang, Tangshan, Qinhuangdao, Handan, Xingtai, Baoding, Zhangjiakou, Chengde, Cangzhou, Langfang, and Hengshui.
Sample size estimation
The sample size was estimated according to the sample size formula for estimating finite population proportion. Based on the total number of rural doctors in Hebei Province (N = 83,659), with a significance level α set at 0.05, an allowable error δ of 1%, and population standard deviation (S = 0.25), the minimum required sample size was determined to be 2334. Taking into account the response rate and efficiency of the questionnaire, the final sample size was determined to be 2500.
Study design
The multistage stratified cluster sampling method is used to extract research objects. According to the composition of the number of rural doctors in 11 prefecture-level cities, 3–4 counties (county-level cities) were selected from each city, 5–10 towns from each county (county-level cities), and all villages of each selected township (town) were included in the survey. The survey uses one rural doctor from each village clinic to complete a questionnaire, as shown in Figure 1.
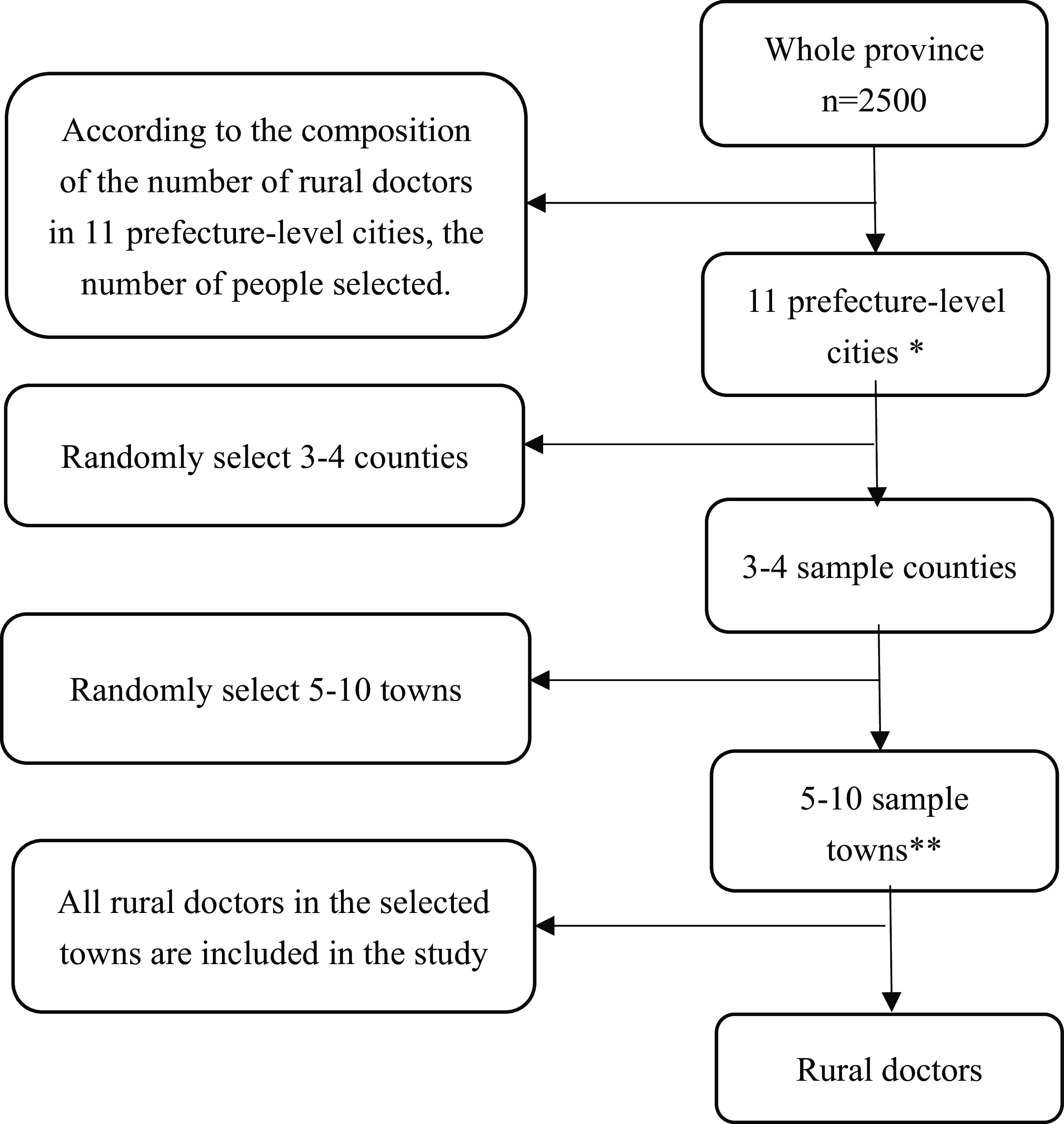
Figure 1. Sampling process flow chart.
* Including two county-level cities, Xinji City (belonging to Shijiazhuang City) and Dingzhou City (belonging to Baoding City).
** According to the estimated number of sampled persons in each city, the number of selected townships varies
Measures
The survey uses a structured questionnaire, which consists of a self-designed basic condition questionnaire and a Symptom Checklist-90 (SCL-90) for rural doctors. Each item uses a 5-level scoring method (none = 0, light degree = 1, moderate = 3, heavy = 4, severe = 5), which takes approximately 10–15 minutes to complete (Derogatis et al., Reference Derogatis, Rickels and Rock1976; Bech et al., Reference Bech, Bille, Moller, Hellström and Ostergaard2014). Primary conditions include gender, age, education, income, work intensity, and physical health. In this study, we used the Chinese version of the SCL-90 to assess rural doctors’ mental disorders and mental health in Hebei Province. The Chinese version of the SCL-90 includes 90 items in 9 dimensions (excluding ‘others’). The main symptom dimensions evaluated are somatization (SOM), obsessive-compulsive disorder (OCS), interpersonal sensitivity (INTS), depression (DEPR), anxiety disorder (ANX), hostility (HOS), phobia (PHOA), paranoia thoughts (PARI), and psychosis (PSY) (Wang, Reference Wang1984).
The Cronbach’s alpha coefficient of the questionnaire is 0.984. The KMO value is 0.988, and Bartlett’s test of sphericity is passed with a significance level of 0.05. These findings indicate that the questionnaire has good reliability and validity.
Variables
According to the scoring standard of the SCL-90 scale, if the total score exceeds 160, or if the number of positive items exceeds 43, or if any factor score exceeds 2 points, the item should be considered positive; if the somatization dimension score is greater than or equal to 24 points, it is considered to indicate somatization symptoms, that is, there are mental health problems; if the obsessive‒compulsive score is greater than or equal to 20 points, it is considered to indicate obsessive‒compulsive symptoms; if the interpersonal relationship score is greater than or equal to 18 points, it is considered sensitive to interpersonal relationships; if the depression dimension score is greater than or equal to 26 points, it is considered to indicate depressive symptoms; if the anxiety dimension score is greater than or equal to 20 points, it is considered to indicate anxiety symptoms; if the hostile dimension score is greater than or equal to 12 points, it is considered to indicate hostile symptoms; and if the terror dimension score is greater than or equal to 14 points, it is considered to indicate horror symptoms; if the paranoid dimension score is greater than or equal to 12 points, it is considered to indicate paranoid symptoms; and if the psychotic dimension score is greater than or equal to 20 points, it is considered to indicate psychotic symptoms.
The participants were classified into four groups according to age: ≤40, 41–50, 51–60, and > 60 years. The education status is divided into four groups, namely no medical education, technical secondary school, junior college, and undergraduate. The working times of the participants were classified into four groups: 1–3, 4–7, 8–11, and ≥12 hours.
Statistical analysis
The data were analysed via the Statistical Package for Social Scientists (IBM SPSS version 25.0). The statistical frequency and proportion were used to describe the sample characteristics. The Chi-square test was also used to compare the proportion of positive screenings among rural doctors with different sociodemographic characteristics. Moreover, t-tests were used to compare the average SCL-90 scores (each of the nine dimensions) between the general Chinese population and rural doctors in this study. The multivariable logistic regression analyses were performed on the factors that may influence mental health via univariate analysis, the SCL-90 total score, and the nine-dimensional indicators used to evaluate mental health. The results are presented as an adjusted odds ratio (ORadj) with a 95% confidence interval (CI). A two-sided P value <0.05 was considered statistically significant.
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of XX (reference number: 2021089). All methods were performed in accordance with ‘Ethical Review Measures for Biomedical Research Involving Human Subjects’ and ‘Regulations of the Ethics Committee of XX’. Before filling out the questionnaire, the interviewees confirmed that they fully understood the precautions. Participation in the research was voluntary, and all participants provided informed consent.
Results
The study distributed a total of 2665 questionnaires to different rural doctors in Hebei, and 2593 questionnaires were returned, resulting in a reasonable recovery rate of 97.30%. Among these 2593 rural doctors, 1872 (72.20%) were male. A total of 30.35% (787) of the participants were less than or equal to 40 years old, 40.99% (1063) were 41–50 years old, 14.69% (381) were 51–60 years old, and 13.96% (362) were over 60 years old. A total of 97.11% (2518) of the participants were married, 74.12% (1922) had lower than junior college degrees, 1.43% (37) had college degrees, and 98.42% of the participants had professional qualifications. Approximately 81.3% of rural doctors are in good health, 15.8% have chronic diseases, and 2.9% have disabilities. The average daily time spent on medical services was 11.82 hours, and 84.77% of rural doctors worked more than 8 hours a day.
A comparison of the total mean scores and factor scores obtained in this survey with the Chinese population norm revealed significant differences, except for SOM (P < 0.05). The total mean scores and factor scores are lower than the Chinese population norm, as shown in Table 1.
Table 1. Respondents’ scores in dimensions of SCL-90 (n = 2593)
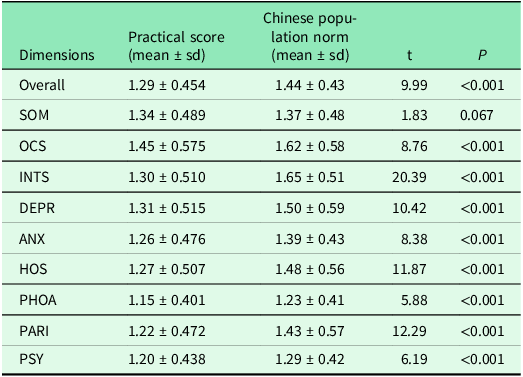
* Chinese population norm: The Chinese population norms were derived from a representative state-wide sample (N = 1890) of Chinese adult residents in 2006 (Dai et al., Reference Dai, Zhang, Sun, Li, Shen and Liu2015; Dong, Reference Dong2010).
According to the screening principle of the SCL-90, the total positive rate of rural doctors was 19.40%. The detection rates of the first three dimensions were OCS (16.40%), INTS (10.80%), and SOM (10.60%). We also found that 10.10% of the responders might have been exposed to depression, 9.00% might have been exposed to hostility, 8.30% might have been exposed to anxiety, 7.90% might have been exposed to paranoid, 6.40% might have been exposed to phobic psychoticism, and 5.40% might have been exposed to phobic anxiety, See Figure 2.
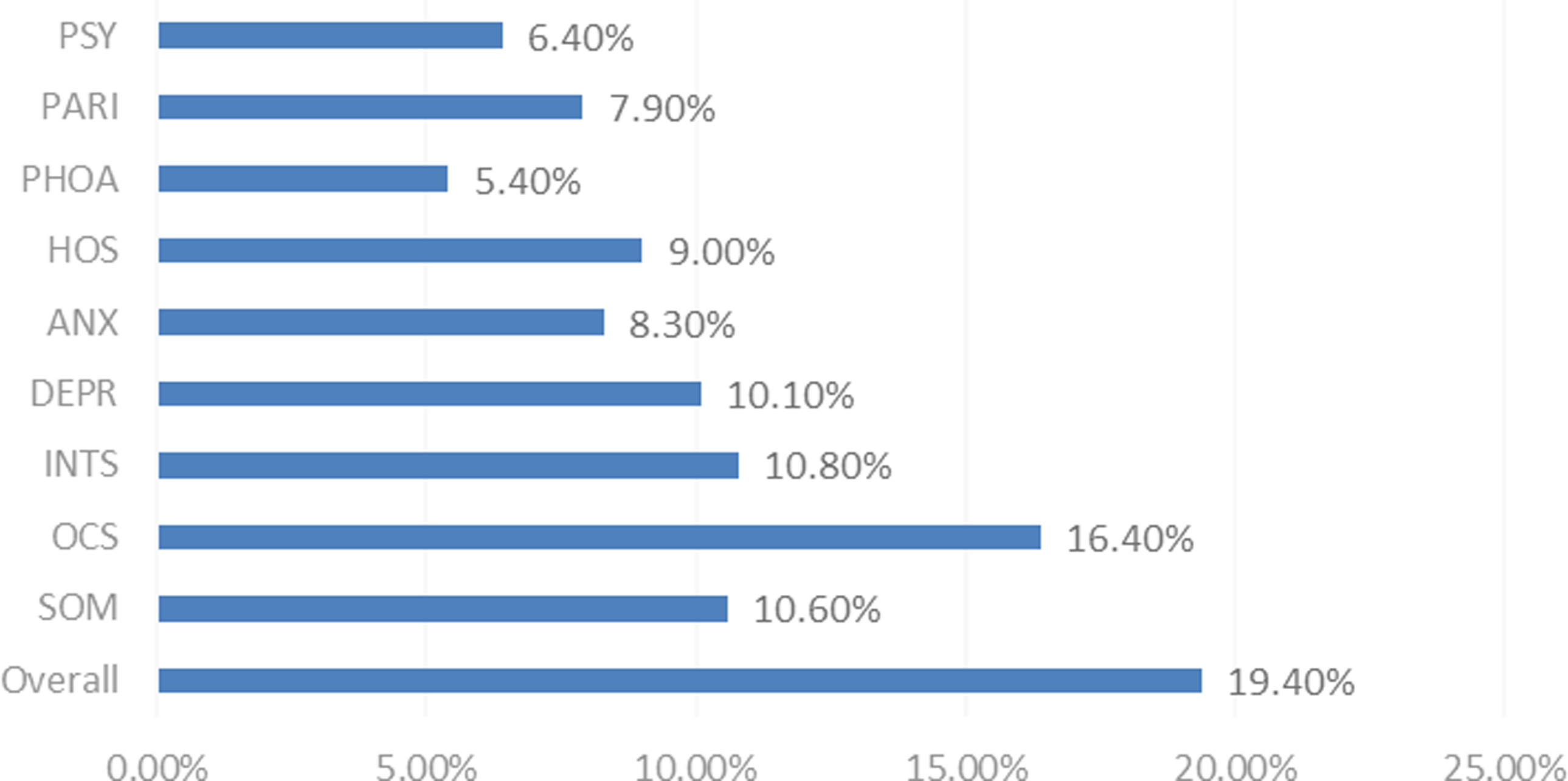
Figure 2. Detection rate in each dimension of SCL-90 among the rural doctors.
The results of the analysis revealed differences in the psychological abnormalities of rural doctors of different ages, genders, health statuses, and working hours. The rates of abnormal total mean scores and the incidence of obsessive-compulsive disorder among rural doctors of different ages were statistically significant (P < 0.05). There were significant differences in the total mean scores of the rural doctors and the psychological abnormalities associated with the nine factors of sex, working hours, and health status. For significance (P < 0.05), see Table 2.
Table 2. Different characteristics of rural doctors SCL-90 abnormal rate [n(%)]
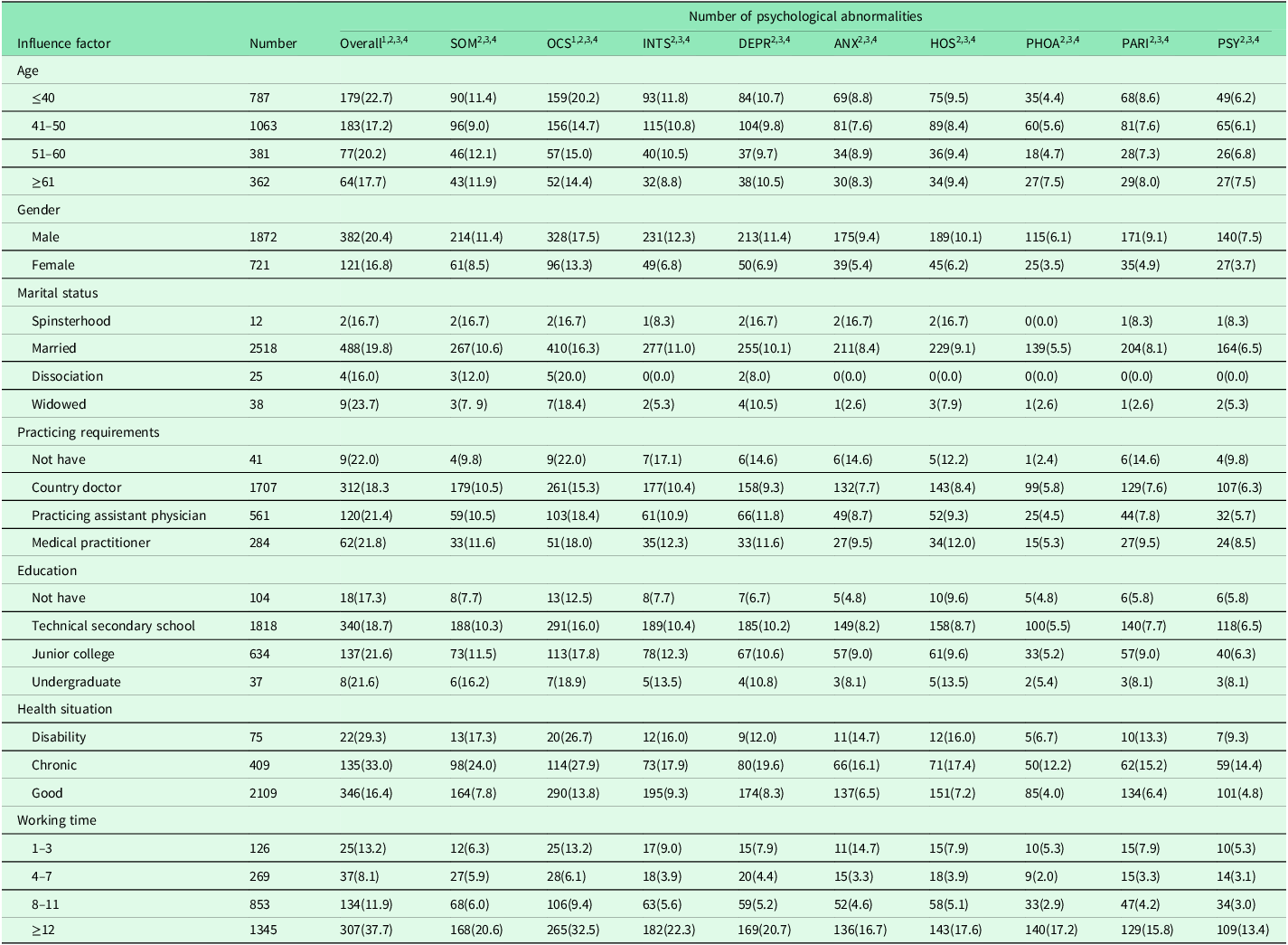
* Chi-square test is used for comparison between groups, P < 0.05.
1 represents the comparison of rural doctors of different ages, P < 0.05
2 means the comparison of rural doctors of different genders, P < 0.05
3 represents the comparison of rural doctors with different health status, P < 0.05
4 represents the comparison of rural doctors with different working hours, P < 0.05.
** In education, ‘No have’ means that there is no medical degree.
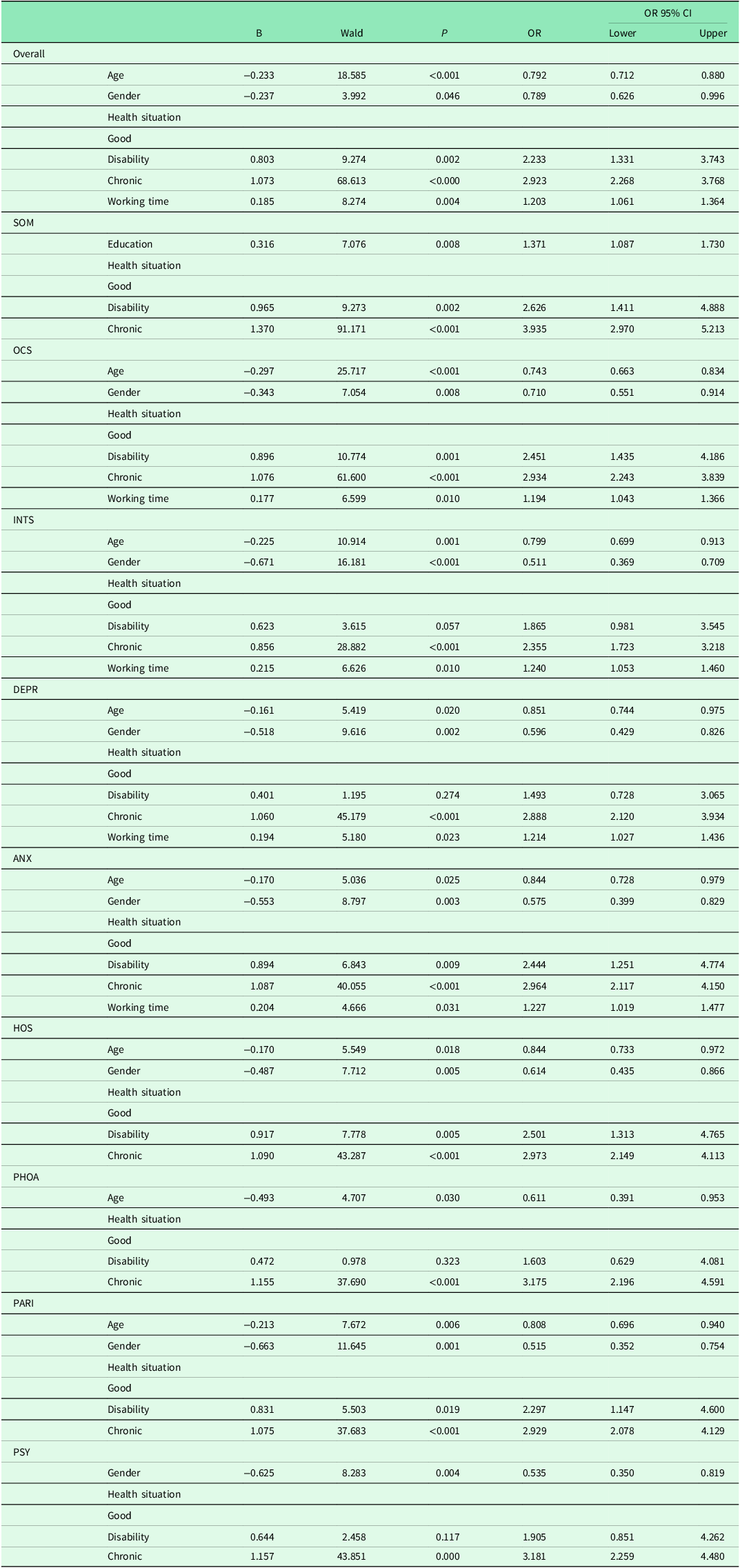
Table 3 shows that age, gender, education, health status, and working time are the main factors influencing the mental health of rural doctors, with gender, age, health status, and working time being particularly significant. The risk of mental health problems among rural female doctors was lower than that among male doctors (OR < 1). Rural doctors with chronic diseases or disabilities were at greater risk of mental health problems. The risks of horror and psychotic symptoms were very high (OR > 3). Younger rural doctors and those with longer working experience were more likely to experience mental health problems. Additionally, rural doctors with higher education levels had a greater risk of somatization (OR = 1.371).
Table 3. Results of multivariate logistic regression analysis
Discussion
Findings and interpretation
-
1. Mental health status of rural doctors in Hebei Province
According to our survey, rural doctors in Hebei Province have better psychological conditions than those in other provinces do (Wu, Reference Wu2011; Lin and Li, Reference Lin and Li2016; Tian et al., Reference Tian, Lu, Yang, Wang, Wang and Zhen2021). First, our investigation was conducted recently, which could be a reason for the results. With the development of medical technology, medical reform policies, and increasing emphasis on primary medical care and rural doctors, the mental health problems of rural doctors have decreased. Second, the findings may be influenced by survey locations. Because different regions have different support policies, Hebei Province is committed to strengthening the benefits of rural doctors, conscientiously implementing and improving policies for elderly individuals, and strengthening subsidies for public health services in township hospitals (Zhu, Reference Zhu2021), which also affects the results. Compared with doctors in some general hospitals in China, rural doctors have better psychological conditions, and their health levels are lower than the Chinese population norm (Gu et al., Reference Gu, Gu, Mei, Lu and Yu2008; Zou et al., Reference Zou, Huang, Wang, Li, He, Min and Zhou2015; Lu, Reference Lu2015). On the one hand, rural doctors are more responsible for treating minor diseases, such as colds, with less difficulty and less pressure than doctors in higher-level hospitals are. On the other hand, currently, patients are more inclined to visit higher-level hospitals, and most of the initial doctors are doctors at the county level and above hospitals. Compared with doctors in higher-level hospitals, rural doctors have fewer consultations and shorter working hours. Therefore, rural doctors have relatively better mental health.
Although the survey results revealed that the mental health of rural doctors in Hebei Province is better than the Chinese population norm, 19.4% still screened positive on the scale. Compared with foreign studies, Chinese rural doctors have more unsatisfactory psychological conditions (Pappas et al., Reference Pappas, Gouva, Gourgoulianis, Hatzoglou and Kotrotsiou2016), so they still need to pay attention. Rural doctors are sequelae of China’s health service development, and they are in a relatively low position. Most of them have no formal professional school education, which leads to a certain degree of professional inferiority complex (Ren, Reference Ren2007), relatively low wages, and social status. They should be called farmers rather than doctors, but they must undertake heavy rural medical and health services. However, doctors or family doctors have higher social status and better incomes abroad, which is the main reason for the difference in mental health.
-
2. Factors influencing the psychological condition of rural doctors
In our study, we found that five factors affected the mental state of rural doctors. The first influencer is age. The younger the rural doctors are, the greater the risk of mental health problems. Young rural doctors, who are just starting to work lack clinical and social experience, are under high pressure for promotion and life and are prone to mental health problems (Sun and Zhang, Reference Sun and Zhang2014; Wu et al., Reference Wu, Wang and Ren2019). In addition, the ‘Suspected Survival and Working Status Report in the Context of the New Medical Reform’ issued by the Chinese Academy of Social Sciences in 2012 stated, ‘After the implementation of the zero markups, the income of clinics dropped by 98.2%. The village clinics were operated by themselves in the past, and the main income was added drugs. After the zero markups, it is difficult for them to maintain operation’ (Han et al., Reference Han, Wang, Liang, Hu, Shao, Wang, Han and Chen2014). Therefore, as the income of village clinics decreases, the income of young village doctors decreases, resulting in dissatisfaction and poor mental health. Moreover, in China, the profession of rural doctors is a family-oriented process that is jointly built by multiple generations (Gao, Reference Gao2018). Young rural doctors must consider their development and professional ambitions and factors such as the reputation of their predecessors and their self-satisfaction with their careers, which will also affect their mental health.
The second influencing factor is gender. The mental health risk of rural male doctors is greater than that of female doctors. First, most rural doctors in China are men. They are the primary source of family income and are under pressure from various aspects of society and family; therefore, they are more likely to experience unhealthy mental conditions such as fatigue and depression, and to a certain extent, these conditions also lead to a decrease in work concentration and motivation. The sleep state of rural doctors is also affected, resulting in a decrease in work efficiency, which is not conducive to the treatment of patients (Wang and Gao, Reference Wang and Gao2015). Men take on more social roles, have a stronger sense of work responsibility, and bear higher societal expectations and requirements, increasing work pressure on male doctors (Dai, Reference Dai2012). Second, men have higher expectations of all aspects of work than women do, and it is difficult for rural doctors to mobilize their enthusiasm for work (Han et al., Reference Han, Wang, Liang, Hu, Shao, Wang, Han and Chen2014). In addition, male doctors tend to have a tougher work attitude, whereas female doctors are relatively better at communication, which makes patients more willing to accept and obey doctors’ orders and results in fewer doctor-patient conflicts.
Third, the longer medical services are provided, the greater the risk of mental health problems for doctors. In China’s basic public health tasks, on average, each rural doctor has to establish files for 1328 people and, at the same time, be responsible for basic medical services (Wang, Reference Wang2012). However, the number of rural doctors is far below the requirements set by the state. It is common for Chinese doctors to work at least 60 hours a week or take long shifts (Dai et al., Reference Dai, Zhang, Sun, Li, Shen and Liu2015). Many doctors are busy and stressed. There is much evidence that there is a positive correlation between long working hours and mental health problems (Richter et al., Reference Richter, Kostova, Baur and Wegner2014; de Cordova et al., Reference de Cordova, Phibbs, Schmitt and Stone2014; Bannai and Tamakoshi, Reference Bannai and Tamakoshi2014). Owing to the shortage of human resources, doctors often have to work overtime or even insist on working with illness. Long working hours and heavy workloads can easily cause psychological problems (Hao, Reference Hao2015). In addition, because rural doctors provide medical services for too long, they will have more physical expenditure and emotional investment, which can easily lead to endocrine hormone disorders, irritability, anxiety, and physical and mental exhaustion, leading to mental health problems.
Physical health is the fourth influencing factor. Rural doctors with chronic diseases or disabilities are at greater risk of psychological problems. We find that mental (physical) health has a significant direct and indirect impact on physical (mental) health. The indirect effect of mental health on physical health is mediated by lifestyle choices and social interactions. The relationship between physical health and mental health is mediated only by past physical activity (Ohrnberger et al., Reference Ohrnberger, Fichera and Sutton2017). Rural doctors have heavy workloads, long working hours, frequent night visits, and irregular lives, making them feel exhausted and seriously affecting their physical and mental health (Lin and Li, Reference Lin and Li2016). The synergy between physical disability or illness and excessive medical service hours also increases mental health problems for rural doctors (Xu et al., Reference Xu, Xu and Xu2013). In addition, drugs used to treat mental illness often cause side effects such as rapid weight gain and sleep disorders, resulting in impaired physical health (Happell et al., Reference Happell, Wilson, Platania-Phung and Stanton2017). Although the work pressure of rural doctors is not as high as that of specialist doctors, they are still under much pressure because of their long working hours and trivial work content, which may further aggravate their psychological problems, thus forming a vicious cycle.
Fifth, rural doctors with a high degree of education are at greater risk of psychological problems. First, doctors with high academic qualifications have a lower sense of accomplishment than doctors with low academic qualifications (Lu et al., Reference Lu, Yan, Zou, Li, Xue and Wang2014), and their professional satisfaction is correspondingly lower. Being in this mood for a long time can induce psychological problems. Second, rural doctors with higher education levels have a more comprehensive range of knowledge and more careful consideration of things, and they are accustomed to suppressing their subconscious desires, which tends to cause psychological problems over time (Tong et al., Reference Tong, Jiang, Zhang, Jia, Lu, Wang, Tang, Zhang, Guo, Li, Jiang, Yu and Lou2018). In addition, rural doctors with higher education levels and more potent professional abilities are highly recognized by villagers (Gao, Reference Gao2018), which results in longer working hours, greater intensity, and greater psychological pressure.
-
3. Suggestions for improving the mental health of rural doctors
As its economy has developed and the level of its health system has improved, China is constantly upgrading the level of rural doctors through medical education, optimizing the structure of rural doctors, broadening the space for their career development, compensating them through multiple channels and increasing their income levels so that they can better serve China’s primary health care (Meng and Yuan, Reference Meng and Yuan2023). However, the quality of life of rural doctors still has to be continuously improved, and their psychological problems must be taken seriously. Rural doctors should be given a certain degree of preference in terms of policy. First, support for rural doctors should continue to increase in the following areas: the first is to train suitable talent following the actual situation; the second is to make reasonable compensation from the economic point of view and improve salaries and wages; and the third is to continuously adjust the planning of talent training by development. Moreover, free regular medical check-up treatment should be provided for physical health-related illnesses so that rural doctors can keep abreast of their health status, prevent chronic diseases and other illnesses from occurring, and form a virtuous cycle of physical-mental health. Additionally, mental health education and psychological counselling lectures should be carried out regularly to assist rural doctors in preventing and solving their psychological problems. In addition, it is necessary to recognize rural doctors at the social level to increase their professional identity and sense of belonging. They support their families and provide good support for rural doctors. To reduce the incidence of their psychological problems, their capacity to provide primary health care services should be improved, and better primary health care services should be provided to the general population.
Strengths and weaknesses
Hebei Province, with 0.2% of China’s area, nurtures 5.28% of the country’s population and is a veritable populous province, of which 56.4% are farmers. This study conducted a survey of rural doctors in several counties in 11 cities of Hebei Province. The scale of the survey was larger and more representative than those used in previous studies. Second, the survey objectively judges the mental health of rural doctors by comparing the results of the SCL-90 with the Chinese population norm and determines the influencing factors of the mental health of rural doctors from different aspects of personal conditions. These findings will contribute to improving the mental health of rural doctors and enable them to provide better primary health care services to the population at large.
The first limitation of this study is that the norm used for comparison dates back to 2006, which may not fully reflect the psychological status of the Chinese population at the time of the survey; however, the lack of recent survey results for comparison affects our comparison results. Additionally, as China lacks established mental health standards for urban doctors, our study omitted comparisons between urban and rural doctors. The second limitation of our study was the reliance on self-reports of SCL-90 sensitive items, such as thoughts of hurting others. Although anonymous self-report questionnaires were used, they might be vulnerable to social expectation bias.
Conclusion
Compared with the Chinese population norm, rural doctors in Hebei Province normally exhibit good mental health; however, 19.4% still experience psychological problems. Young male rural doctors, those with longer medical service durations, chronic illnesses or disabilities, and higher levels of education are at greater risk of developing mental health problems. Attention should be given to the mental health of the rural doctor population to improve primary health care services.
Acknowledgements
The authors are most grateful to Hebei Provincial Health and Family Planning Commission. We also thank all the participants in this study.
Author contributions
LT, YL, and HD contributed to the study concept and design, data interpretation, and strict revision of the manuscript. YL was involved in the research design, manuscript drafting, and data collection and analysis. YZ, YY, NZ, and JL were involved in data analysis. BZ and YW were involved in the study design and manuscript drafting. YX, ZY, and YN were involved in data collection and analysis. All authors read and approved the final manuscript.
Funding sources
This project is a scientific research fund project of the Hebei Provincial Health and Family Planning Commission (the project name is ‘Research on the role positioning and ability improvement of rural doctors in Hebei Province under the background of rural revitalization’; the award number is 20210244). The sponsor is the Hebei Provincial Health Commission, and the grant recipient is Yunqing Xu.
Disclosures
The authors have no conflicts of interest to disclose.
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of Hebei Medical University (reference number: 2021089). All methods were performed in accordance with ‘Ethical Review Measures for Biomedical Research Involving Human Subjects’ and ‘Regulations of the Ethics Committee of Hebei Medical University’. Before filling out the questionnaire, the interviewees confirmed that they fully understood the precautions. Participation in the research was voluntary, and all participants provided informed consent.
Consent for publication
Not applicable.
Availability of data and materials
The datasets used and/or analysed in the present study are available from the corresponding author upon reasonable request.







