Schizophrenia represents a pervasive disturbance of brain function, leading to hallucinations and delusions, social withdrawal and a decline incognitive performance (American Psychiatric Association 1994). Patients with schizophrenia present with a broad clinical spectrum of cognitive, affective, positive and negative and associated behavioural symptoms (Fig. 1). The aetiology of schizophrenia involves both genetic and environmental factors (Reference Tandon, Keshavan and NasrallahTandon 2008). Understanding the biology of schizophrenia is a formidable challenge, owing to the structural and functional complexity of the human brain, the complexity of studying the brain in vivo, difficulties obtaining brain tissue to examine the disease process and/or effects of treatment and, crucially, the lack of objective biomarkers that reflect shared biology and/or brain function across affected individuals (Reference Tandon, Keshavan and NasrallahTandon 2008). The complexity of schizophrenia – both clinically and biologically – suggests that approaches to treatment will similarly be complex rather than simple. It is therefore unlikely that any one drug will address all psychoses and all positive, negative, affective and cognitive symptoms.
Despite recent progress, the underlying genetic and neuronal abnormalities in schizophrenia are largely unknown. Further, more objective assessment of symptoms and their severity and the design and evaluation of treatments remains a formidable challenge. Indeed, most clinicians do not assess their patients using standardised scales, although many such tools are available. However, recent advances in molecular genetics may help develop a better understanding of the pathophysiology of schizophrenia and open up new possibilities for drug discovery and development, and enable a more stratified approach to treating affected individuals.
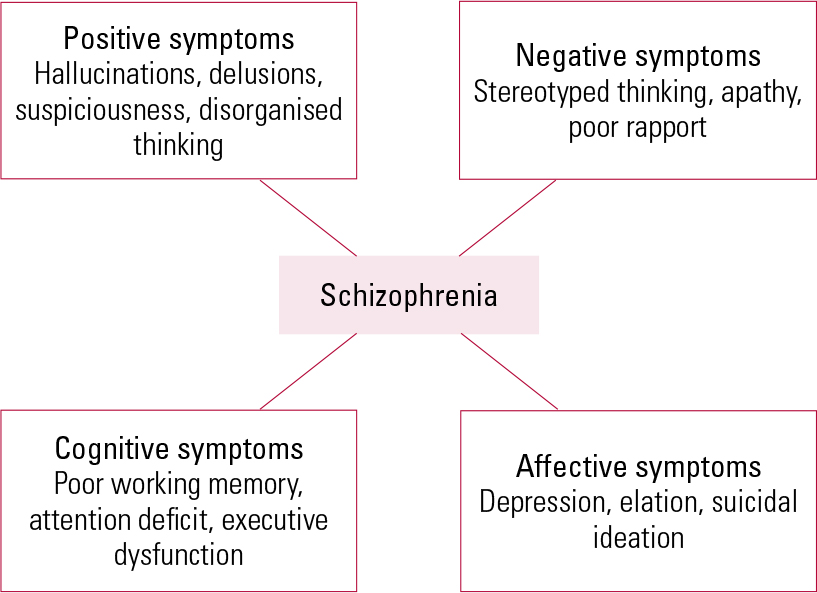
FIG 1 The main symptom domains of schizophrenia.
The discovery of chlorpromazine and the dopamine hypothesis
Chlorpromazine was introduced as an antipsychotic in the early 1950s, after the observation of its pronounced calming effects in individuals with psychotic signs and symptoms (reviewed in Reference Meyer and SimpsonMeyer 1997). Subsequently, Reference Carlsson, Lindqvist and MagnussonCarlsson et al (1958) identified the presence of dopamine in the brain and proposed that abnormal neuronal processes result in an excess of dopamine, causing the symptoms of schizophrenia. They postulated that the antipsychotic action of chlorpromazine is the result of dopamine targeting (Reference Carlsson and LindqvistCarlsson 1963).
Since these early investigations, the hypothesis that dopamine and dopaminergic mechanisms are central to schizophrenia has developed to become useful (Reference Howes and KapurHowes 2009). Indeed, all current antipsychotic drugs are dopamine D2 receptor antagonists (Reference SeemanSeeman 2002). Although antipsychotics have modulated the regulation of dopamine activity in the brain, there is no conclusive evidence that schizophrenia is the result of a primary dopamine abnormality, and it is now widely accepted that the biological basis of schizophrenia encompasses much more than neurochemical abnormalities involving dopamine (Reference CoyleCoyle 2006). The dopamine disturbance observed in some patients with schizophrenia may not even be primary, but a consequence of, or secondary to, the primary biological causes (Reference CoyleCoyle 2006).
Current antipsychotics: stepping-stones to improved treatment options
Chlorpromazine and similar first-generation antipsychotics have a heterogeneous neurotransmitter receptor-binding profile and comparatively low potency, often requiring higher doses to achieve a therapeutic response (Reference SeemanSeeman 2002). The subsequent development of more selective dopamine D2 antagonists led to higher-potency antipsychotics, such as haloperidol and fluphenazine, that could be used in lower doses. In the 1990s, second-generation antipsychotics were introduced and have now become first choice for the treatment of schizophrenia (Reference MortimerMortimer 2003).
Despite the evolution of antipsychotic treatments, it can be argued that there has been little real pharmacological advance since the introduction of chlorpromazine in the 1950s; all current second-generation antipsychotics are still based primarily on dopamine antagonism and have significant side-effects, albeit a different side-effect profile than that of first-generation antipsychotics (Reference Barry, Gaughin and HunterBarry 2012). Furthermore, their limited efficacy with respect to negative symptoms, cognitive and other psychological functions means that second-generation antipsychotics fall short of what is required to meet patients’ needs, and clearly more efficacious compounds are required (Reference Lieberman, Stroup and McEvoyLieberman 2005; Reference Leucht, Arbter and EngelLeucht 2009a, Reference Leucht, Corves and Arbterb). This paucity of new drugs that represent significant innovation is not unique to psychiatry, and it has been estimated that ‘since the mid-1990s about 85–90% of all new drugs provide few or no clinical advantages for patients’ (Reference Light and LexchinLight 2012).
Economic burden of schizophrenia
Social disability remains a pervasive challenge in schizophrenia and as a result many people with the disorder require continuing care and support following treatment for acute episodes of psychosis (Reference Wiersma, Wanderling and DragomireckaWiersma 2000). The functional impairments of schizophrenia result in a significant added economic burden (Reference CoyleCoyle 2006). Indeed, schizophrenia accounts for 16.8 million disability-adjusted life years (the amount of health lost because of a disease or injury) on a global basis, ranging from about 1.6 million to 16 million for high- and low-income countries respectively. The World Health Organization (2008) estimates that schizophrenia, depression, epilepsy, dementia, alcohol dependence and other mental, neurological and substance use disorders constitute 13% of the global burden of disease, surpassing both cardiovascular disease and cancer. Worldwide, schizophrenia is the third highest ranked mental, neurological and substance use disorder after depression (first) and alcohol use disorders (second).
Consequently, disorders of the brain are one of the top economic challenges for healthcare in Europe: their economic burden was estimated at a staggering €798 billion in 2010 (Reference Gustavsson, Svensson and JacobiGustavsson 2011). Direct healthcare costs comprise the largest proportion of the expense (37% direct healthcare costs and 23% direct non-medical costs), although indirect costs associated with patients’ production losses are also relevant (Reference Gustavsson, Svensson and JacobiGustavsson 2011). When treating patients with schizophrenia, most of the direct healthcare costs result from the chronicity of the disease and associated functional impairments, and other physical comorbidities. The economic data emphasises the scale of the challenge and underscores the need for improved drug treatment for schizophrenia as a whole, but in particular the need for treatments for the associated cognitive and negative symptoms (Reference CoyleCoyle 2006).
Given that current drugs do not meet the needs of patients with schizophrenia (Reference Lieberman, Stroup and McEvoyLieberman 2005; Reference Leucht, Arbter and EngelLeucht 2009a, Reference Leucht, Corves and Arbterb), together with the enormous healthcare costs associated with treatment (Reference CoyleCoyle 2006; Reference Gustavsson, Svensson and JacobiGustavsson 2011), there is a compelling case for schizophrenia research to be considered more of a priority in order to improve treatment options (Reference Collins, Patel and JoestlCollins 2011). However, there have been recent signs that a number of the major pharmaceutical companies are reducing their commitment to schizophrenia research. This is unfortunate given the developments taking place across the field of neuroscience. Recent advances in gene technology show that many genetic variants are involved, supporting Bleuler’s early insight (Reference BleulerBleuler 1911) that schizophrenia is a family of conditions and therefore the ideal therapeutic approach is likely to involve a stratified healthcare paradigm, where interventions are tailored to individual needs (i.e. identifying responder subgroups).
Understanding the pathophysiology of schizophrenia: an essential step for drug discovery
Future drug discovery approaches for the treatment of schizophrenia will need to be based on a better understanding of the pathogenesis of the disorder. One of the most important challenges for schizophrenia research at present is to understand better the constituent elements of the disorder, such as negative symptoms, that are resistant to current treatments. With the sequencing of the human genome and development of a range of genome-based and other technologies, there are unprecedented opportunities for gaining insights into complex illnesses such as schizophrenia.
There are at least three key overlapping hypotheses of the underlying pathophysiology of schizophrenia that we should consider: the signal transduction hypothesis, the molecular genetics hypothesis and the neural network hypothesis (Reference Gray and RothGray 2007) (Box 1). It is worth emphasising the overlapping nature of these hypotheses: future hypothetical constructs for schizophrenia are likely to integrate and incorporate features of each and suggest mechanisms for the influence of environmental factors on biological systems.
BOX 1 Overlapping hypotheses underlying the pathophysiology of schizophrenia
-
• Signal transduction hypothesis: altered signalling pathways induce schizophrenia
-
• Molecular genetics hypothesis: susceptibility genes confer risk of schizophrenia
-
• Neural network hypothesis: altered neural networks result in abnormal connectivity in the brain
Signal transduction hypothesis
This hypothesis considers that basic alterations in receptor-mediated signal transduction induce schizophrenia-like symptoms (Reference Gray and RothGray 2007). The aim of drug treatment is to target receptor pathways in order to normalise the altered signalling and treat the symptoms. All currently available antipsychotics and many pipeline drugs are based on this hypothesis and target dopamine signalling (Table 1); however, several lines of evidence suggest that the pathophysiology of schizophrenia is likely to involve neurotransmitters other than dopamine.
The glutamate hypothesis of schizophrenia stems from observations that phencyclidine, an antagonist of the N-methyl-d-aspartate (NMDA) subtype of glutamate receptors, given to otherwise healthy humans induces psychosis that closely resembles schizophrenia, with both positive and negative symptoms of the disease. Phencyclidine exacerbates such symptoms in stable patients with chronic schizophrenia, and pharmacological models have shown that NMDA receptor blockade produces cognitive deficits that resemble those found in schizophrenia. Furthermore, altered levels of components of the glutamate signalling pathway have been observed in cerebrospinal fluid (CSF) and post-mortem brain samples from patients with schizophrenia (Reference Tsai, Passani and SlusherTsai 1995).
Together, these studies suggest that targeting glutamatergic pathways could have antipsychotic benefits and they are receiving attention from drug companies. Indeed, Eli Lilly has developed a selective glutamate agonist LY2140023 (pomaglumetad methionil), which showed improvements in both positive and negative symptoms of schizophrenia in an early study compared with placebo (Reference Patil, Zhang and MartenyiPatil 2007), although a second phase II study produced less conclusive results (Reference Kinon, Zhang and MillenKinon 2011). Unfortunately, the new drug failed to achieve primary end-points for either the overall population or a genetic sub-population in its phase III trials, raising doubts about future development of this drug. This case illustrates well the high costs of developing CNS drugs due to late-stage attrition.
The glycine modulatory site on the NMDA receptor complex is also considered an attractive therapeutic target for schizophrenia. N-methyl-d-aspartate receptor neurotransmission can be enhanced by increasing the availability of the co-agonist glycine at modulatory sites on the NMDA receptors through the inhibition of glycine transporter-1 (GlyT1) on glial cells. Some clinical studies have demonstrated that the GlyT1 inhibitor sarcosine (N-methylglycine) shows antipsychotic activity in patients with schizophrenia. Roche are investing significantly in this area of research and are developing novel and selective GlyT1 inhibitors for the treatment of schizophrenia with a compound known as RG1678 (bitopertin) (Reference HashimotoHashimoto 2011). Bitopertin is currently in phase III trials. Other pipeline drugs targeting other neurotransmitter pathways are now in the early stages of development (Table 2).
TABLE 1 Molecular targets for drugs in development for schizophrenia
Molecular genetic hypothesis
This hypothesis is based on the effects of susceptibility genes underlying the pathophysiology of schizophrenia; targeting such genes or pathways might lead to the development of novel treatments (Reference Gray and RothGray 2007). Complex disorders such as schizophrenia are associated with a spectrum of rare and common genetic variants, with hundreds of contributing loci in the human genome. Advances in molecular genetics have helped to identify putative genes involved in the development of schizophrenia. It is believed that multiple genetic variants, each contributing a modest effect on disease risk, interact with environmental factors to result in the clinical phenotype.
Genome-wide association studies (GWAS) can be used to search for both rare and common susceptibility genes in affected families or in large groups of individuals who do not have a family history of schizophrenia (Reference Owen, Williams and O'DonovanOwen 2009). Such studies have implicated a number of possible candidate genes, enabling investigation of multiple genes in functional biological pathways. Knowledge of genetic factors may offer the potential for prediction, patient stratification and insights into early precursors of schizophrenia when preventive therapies might be applied.
One gene locus, named ‘Disrupted in schizophrenia 1’ (DISC1), is now widely recognised as a genetic risk factor for a spectrum of psychiatric disorders. It is associated with a balanced t(1;11) (q42.1;q14.3) chromosome translocation that was originally identified in a large Scottish family with a heavy burden of major mental illnesses (Reference St Clair, Blackwood and MuirSt Clair 1990). DISC1 has been shown to affect many aspects of central nervous system (CNS) function, including neurodevelopment, neurosignalling and synaptic functioning. It also interacts with numerous proteins involved in neuronal migration, neurite outgrowth, cytoskeletal modulation and signal transduction (Reference Mackie, Millar and PorteousMackie 2007). Additionally, a meta-analysis of five independent data-sets has shown association of single nucleotide polymorphisms (SNPs) in the gene KCNH2 with increased risk of developing schizophrenia (Reference Huffaker, Chen and NicodemusHuffaker 2009). Members of the neuregulin-ErbB receptor (NRG-ErbB) signalling pathway have also been implicated in regulating glutamatergic neurotransmission and are potential genetic risk factors for schizophrenia (Reference BuonannoBuonanno 2010). However, even the most researched candidate genes such as DISC1 and neuregulin-1 (NRG1) are likely to be important in only a small percentage of cases of schizophrenia.
Sample size is an important consideration when conducting genetic linkage and association studies, as underpowered studies can result in false-negative results (Psychiatric GWAS Consortium Coordinating Committee 2009). For example, a study involving nearly 750 patients with schizophrenia and a similar number of controls analysed almost half a million SNPs without identifying a single gene that met the requirements to show it was a risk factor – including DISC1 (Reference Sullivan, Lin and TzengSullivan 2008). It is now accepted that statistically significant genetic variants will only be recognised by using large numbers of patients (more than 10 000) in GWAS, although each potential gene candidate may only contribute a small effect (Psychiatric GWAS Consortium Coordinating Committee 2009). Such genes of small effect size are unlikely to be used as a means of stratifying patient populations. Furthermore, genetic heterogeneity also limits the application of genetic analysis to clinical practice. A complementary approach may be to study smaller, more homogeneous groups, such as the family cohort that led to the identification of DISC1; such refined homogeneous groups may share more of their biological substrate than the heterogeneous groups typically used in clinical trials and may therefore lead to the identification of candidate genes relevant to clinical phenotype in the affected families.
This approach could help identify clinical phenotypes, which may make it possible to stratify treatment options in the future and ‘signpost’ relevant biological pathways that could be targets for novel treatments. This may also be beneficial for investigating the therapeutic potential of novel treatments, as the chance of the beneficial effects of interventional drugs being diluted in a group of heterogeneous individuals should be reduced; the hypothesis being that drugs might be more successful in patients with a specific genotype or phenotype. Reference Ayalew, Le-Niculescu and LeveyAyalew et al (2012) proposed that the top candidate genes identified from GWAS might be used to generate a genetic risk prediction score for particular individuals and suggest that this could lead to a better understanding of schizophrenia, diagnostic issues and therapeutics.
Genetic factors, both known and those yet to be discovered, do not fully explain an individual’s susceptibility to schizophrenia. Indeed, the risk of developing schizophrenia is substantially influenced by environmental factors. Identifying such factors has been difficult owing to the complexity and expense of long-term or cross-sectional studies in at-risk populations and the need to collect and store biosamples for future research to identify biomarkers of disease development. Nonetheless, researchers are exploring multiple diverse factors that might play a role in the development of schizophrenia, perhaps in genetically susceptible individuals, including stressors in adolescence or early adult life (e.g. drug misuse, brain injury, stress/trauma (Reference Howes, McDonald and CannonHowes 2004)) and, more recently, inflammatory processes linked to infection or antigen sensitivity (Reference Severance, Alaedini and YangSeverance 2012).
Neural network hypothesis
This hypothesis supposes that the pathophysiology of schizophrenia results from altered neuronal networks; drugs that are able to somehow reset neural networks will therefore be valuable in the treatment of the disorder (Reference Gray and RothGray 2007). Evidence suggests that schizophrenia is a neurodevelopmental disorder associated with abnormal brain connectivity, resulting from defects in synaptic pruning and migration of neurons. If the alterations in synaptic pruning are a result of primary processes resulting from inherited alterations in genes such as DISC1, then effective treatments must target the underlying deficits. However, if abnormal migration of neurons results in dysregulation of cortical development, this may be more difficult to treat with pharmacological methods.
Brain imaging may help to clarify the functional link between genes, the molecular networks in which they participate, and brain circuitry and function (Reference Potkin, Macciardi and GuffantiPotkin 2010). For example, integrating genetic data from GWAS with brain imaging data identified a number of risk genes for schizophrenia, including several with functions related to progenitor cell proliferation, migration and differentiation, cytoskeleton reorganisation, axonal connectivity and development of forebrain structures (Reference Potkin, Macciardi and GuffantiPotkin 2010).
Future approaches
Refining diagnosis and classification of schizophrenia
Mental disorders are typically defined as either categories of illness or along dimensions of mental or behavioural symptomatology. Categorical approaches are typified by the American Psychiatric Association’s diagnostic criteria, as published in DSM-IV-TR (American Psychiatric Association 1994). However, the recently published DSM-5 (American Psychiatric Association 2013) also introduces a dimensional approach to rating severity for the core symptoms of schizophrenia, to capture the heterogeneity in symptom type and severity presented by different individuals. The definitions of mental disorders in both DSM-IV-TR and DSM-5 are characterised predominantly by symptom criteria for diagnoses and are not related to aetiology or treatment response.
Advances in molecular genetics now suggest that the categorical approach to the diagnosis and classification of major psychiatric illness are inadequate and may hamper research, drug discovery and clinical care. Dimensional approaches emphasise symptoms along a continuum from few, if any, symptoms to clinically significant levels of symptoms (Reference Kaiser, Heekeren and SimonKaiser 2011). Dimensional rather than categorical classification tends to be supported by the results from GWAS, given the substantial genetic overlap between schizophrenia and mental disorders such as bipolar disorder, autism and intellectual disability, with some genetic loci apparently influencing risk for a number of disorders (Reference O'Donovan, Craddock and OwenO’Donovan 2009). These findings challenge the traditional boundaries between psychiatric illnesses, and many researchers are now focusing on the identification of intermediate phenotypes to understand the interplay between the risk genes involved and the psychopathology presented (Reference Rasetti and WeinbergerRasetti 2011). The ultimate aim of this approach is to enable subcategorisation of individuals based on the presence of susceptibility alleles in order to stratify the patient population and thereby improve the treatment of neuropsychiatric illnesses.
Validation of new antipsychotics
Although much of the evidence for the efficacy of antipsychotic therapies has come from short-term clinical trials, most patients discontinue treatment owing to a lack of effectiveness or the development of side-effects, and not all patients respond similarly to this group of drugs (Reference Lieberman, Stroup and McEvoyLieberman 2005). This emphasises the need for stratified care plans with (in future) the routine use of biomarkers to enable clinicians to modify the way they approach, treat and care for patients. However, although there are many potential genetic markers for schizophrenia, there are no validated biomarkers for the disorder that help establish diagnosis or reliably predict response to treatment (Reference Kaddurah-DaoukKaddurah-Daouk 2006). The development of biomarkers capable of assisting differential diagnosis is a key goal in the treatment of schizophrenia, given that diagnosis currently relies entirely on the subjective assessment of clinical symptoms.
Cerebral spinal fluid as a biomarker
One example of this approach is the use of cerebrospinal fluid (CSF) as a potential source for identifying protein-based psychiatric biomarkers (Reference Schwarz and BahnSchwarz 2008; Reference Oertel-Knöchel, Bittner and KnöchelOertel-Knöchel 2011). Indeed, differences in metabolic profiles have been noted between CSF from patients with schizophrenia and healthy individuals, suggesting that analysis of CSF could be used for early diagnosis of schizophrenia (Reference Holmes, Tsang and HuangHolmes 2006). Two potential biomarkers, the nerve growth factor VGF peptide and transthyretin, have been identified (Reference Huang, Leweke and OxleyHuang 2006), although these still require validation before they find their way to clinical application. It is possible that in future, CSF-derived biomarkers could assist in the clinical management of schizophrenia, although whether such an approach is practical or acceptable in clinical practice would be open to debate.
Electroencephalograms as a biomarker
Electroencephalogram (EEG) signals have also been investigated as biomarkers in patients with schizophrenia and offer the promise of predicting the likelihood that novel therapies and compounds will exhibit clinical efficacy early in preclinical development. Electroencephalography may offer much more utility in clinical practice than other neuroimaging methods or CSF sampling. Such EEG analyses might provide a physiological endpoint that could be used to facilitate drug discovery, optimise lead or candidate compound selection, and inform patient stratification (Reference Leiser, Dunlop and BowlbyLeiser 2011).
Brain imaging as a tool for biomarking
Magnetic resonance imaging and other brain imaging methods are also potential tools for investigating drug effects in patients with schizophrenia (Reference McGuire, Howes and StoneMcGuire 2008; Reference Winton-Brown and KapurWinton-Brown 2009). Although such methods may be useful in research settings, they are relatively expensive and may be much more difficult to employ in the context of a clinical trial or clinical practice.
Responsiveness of biomarkers
The responsiveness of biomarkers to drug treatment could be a valuable surrogate end-point in clinical trials, enabling differentiation between responders and non-responders and generally allowing the development of a more stratified/personalised treatment approach. Furthermore, validated targets could help clinicians identify and classify vulnerable patients at an earlier stage of the illness and may therefore facilitate earlier and more effective intervention (Reference Schwarz, Guest and RahmouneSchwarz 2012).
Stratified treatment
Second-generation antipsychotics have become the mainstay of drug treatment for schizophrenia. However, patients who receive antipsychotics differ with respect to treatment response and drug-induced adverse events; this was well demonstrated in the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) programme (Reference Lieberman, Stroup and McEvoyLieberman 2005). Understanding individual differences in response to antipsychotics and susceptibility to metabolic and other side-effects of pharmacotherapy is essential to optimise the treatment of schizophrenia for any given individual.
Recent studies have demonstrated the potential of GWAS to discover novel genes and pathways that may mediate the beneficial effects of antipsychotics (Reference McClay, Adkins and AbergMcClay 2011) as well as their adverse metabolic side-effects (Reference Adkins, Aberg and McClayAdkins 2011). This type of methodology could eventually help to identify the most appropriate drug treatment for individual patients with schizophrenia. Genetic analysis has already successfully identified genetic susceptibility to agranulocytosis induced by clozapine (Reference Athanasiou, Dettling and CascorbiAthanasiou 2011), and evidence from a case study suggests that genotyping can help identify patients suitable for clozapine treatment (Reference McKnight, Guirgis and VotolatoMcKnight 2011). In the foreseeable future, genotyping could aid treatment decisions, ultimately leading to more targeted and individualised treatments.
Translational research in drug development
The global schizophrenia therapeutics market was valued at $6.7 billion in 2010, and is expected to reach $7.3 billion by 2018 (Global Schizophrenia Therapeutics Market 2011). However, innovation within the market is limited, with some pharmaceutical companies pulling out of drug development programmes in psychiatry (Reference SmithSmith 2011). Traditional drug development is not only costly but has high attrition rates, often because efficacy and safety issues are not identified until relatively late in drug development, typically in phase III clinical trials.
It has been recognised that development costs could be reduced through strategies that allow more effective prediction of the success or adverse effects of a candidate drug at an earlier stage in the development pipeline. Translational research might help in this, by enabling prediction of outcomes of treatment with experimental agents earlier in their development. Part of this changed discovery paradigm uses biomarkers to determine pharmacodynamic, efficacy and safety parameters more quickly and earlier than would be the case using traditional clinical end-points (Reference Day, Rutkowski and FeuersteinDay 2009).
What next for pharmacotherapy for psychotic illnesses?
Given the considerations mentioned, what developments are likely in the future? Clearly, the age of highly profitable ‘blockbuster’ drugs may be drawing to a close, and several large pharmaceutical companies have signalled their intention to retreat from the development of psychotropics, and in particular therapeutics for schizophrenia. There is increasing recognition that a more stratified approach to clinical trials could help identify subgroups who respond to particular interventions.
To date, however, there is little to suggest that stratification on the basis of clinical characteristics helps to reliably predict which drugs work best for which patients. In future, the potential to use biomarkers for identifying patients who are more likely to benefit or to experience an adverse reaction in response to a given therapy, and thereby better match specific patient populations with therapies, is likely to represent an important advance in clinical practice (Fig. 2).
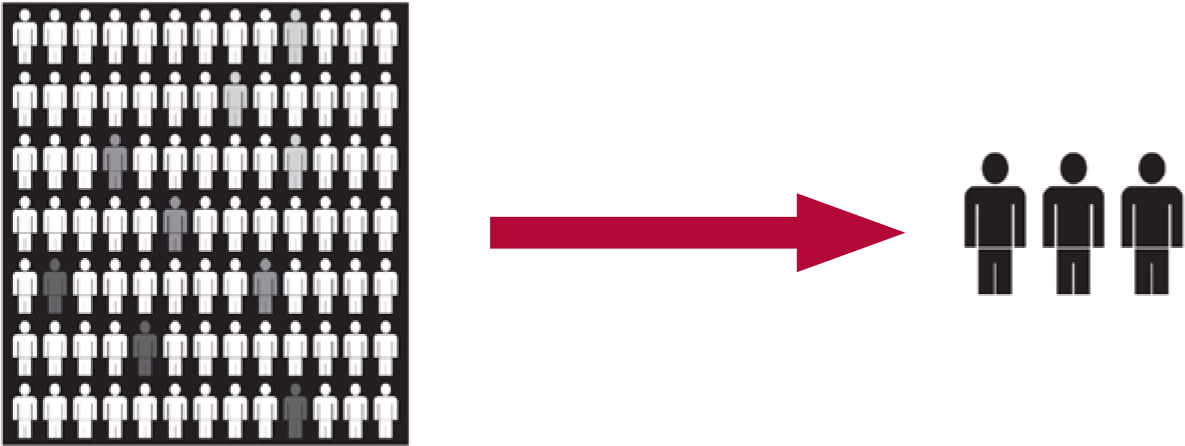
FIG 2 The use of biomarkers to develop a stratified approach to antipsychotic treatment.
Support for DSM-5
Another important consideration is that DSM-IV, which has so dominated interventional research in schizophrenia for many years, may have inadvertently inhibited drug development. As a consequence of using DSM-IV entry criteria and its categorical schemata, participants in trials have constituted a rather heterogeneous clinical group. Clinical trials using DSM-IV entry criteria, a US Food and Drug Administration requirement, may have compromised the identification of therapeutic responses in subgroups and reduced the chances of identifying interventions for negative or cognitive symptom domains. These considerations in part explain support for DSM-5 to include dimensions of psychopathology in addition to diagnostic class (American Psychiatric Association 2010).
Drug combinations and polypharmacy
Many therapeutic areas, such as oncology, require the use of a combination of drugs for their synergistic effects to maximise patient outcomes. Likewise, drug combinations are likely to be required for the treatment of schizophrenia to mitigate the complex interplay of biological, clinical and psychosocial factors, improve efficacy and tolerability of drug treatment and target particular symptom domains (Fig. 3). Thus, rational polypharmacy may be an acceptable strategy in future for the complex symptom profiles presented by patients. As with cancer therapeutics, such an approach may allow incremental improvements in clinical outcomes.
A major problem in schizophrenia treatment is lack of patient insight, and treatment plans must consider this and plan accordingly for its consequences. Poor insight can lead patients to believe that their treatment is not required and/or of no benefit to them and it is therefore often associated with reduced adherence or non-adherence to medication regimes (Reference Buckley, Wirshing and BhushanBuckley 2007). Increased risk of relapse and possible readmission to hospital are likely consequences of poor adherence (Reference Masand and NarasimhanMasand 2006). New methods of drug delivery such as long-acting injectable medication may help treat patients with lack of insight. These types of medication can assure treatment delivery and enable patients to receive maximal benefit from their medication.
Defining recovery
The definition of recovery is also important when considering patient outcomes: clinical neuroscientists might believe that an absence of disease, a lack of symptoms or a ‘cure’ is a prerequisite for clinical recovery, whereas those from a tradition of mental health advocacy often use the term recovery to describe a process of personal recovery, where the emphasis is placed on managing mental health problems, coping better with psychological effects, and pursuing a personally more meaningful life in the community. This latter interpretation involves helping individuals to gain an understanding of their own strengths and weaknesses, but not necessarily aiming for an absence of symptoms (Reference Lieberman, Drake and SedererLieberman 2008).
These contrasting but complementary definitions of recovery should be considered when developing a personalised approach to treatment in patients with schizophrenia. This type of approach is common in other chronic conditions, such as rheumatoid arthritis and diabetes, where the management of symptoms is combined with maximising function over the longer term. Thus, although the emphasis of this review has been on pharmacotherapy, this is of course only one component of an individual treatment or care plan that needs to embrace a range of interventions and strategies within an overall approach underpinned by a recovery ethos that looks to the long term, rather than the management of acute episodes.
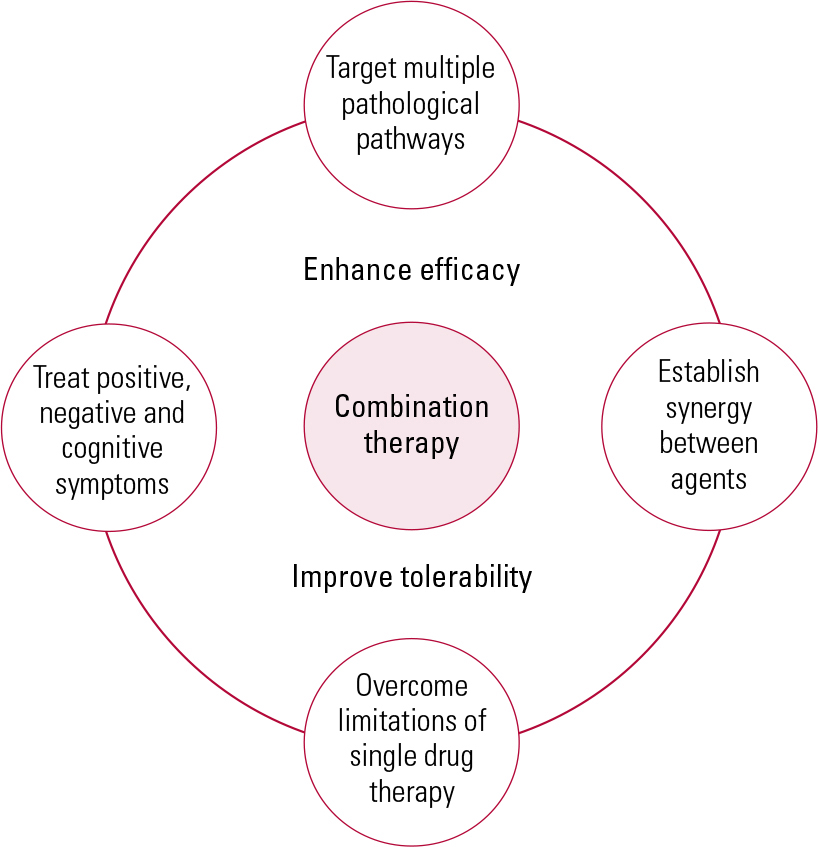
FIG 3 The case for rational polypharmacy. Drug combinations may be necessary to target different symptom types in schizophrenia.
Conclusions
Despite attempts and some progress to improve antipsychotic treatments, there has been little pharmacological advance in the treatment of schizophrenia since the introduction of chlorpromazine in the 1950s. However, recent advances in molecular genetics and neuroscience take us a step closer to a more integrated approach to drug discovery as well as the opportunity to provide stratified healthcare, built on a better understanding of the pathophysiology of the disease and greater knowledge of an individual’s phenotype. The success of such an approach will also depend on having diagnostic tests that can help identify patients who will benefit from targeted therapies. The ultimate aim of these developments is to enable earlier disease identification and intervention to optimise patient care and improve long-term outcomes.
MCQs
Select the single best option for each question stem
-
1 Dopaminergic mechanisms in schizophrenia:
-
a are the primary neurochemical abnormality
-
b were discovered initially through preclinical science
-
c probably account for most psychopathology
-
d will be the basis of the next generation of antipsychotics
-
e represent the best current approach for the treatment of symptoms.
-
-
2 Second-generation antipsychotics:
-
a provide improved efficacy over first-generation antipsychotics for the treatment of positive symptoms
-
b are associated with improved efficacy for negative symptoms
-
c have become the first-choice medication for most patients
-
d have a better safety profile than first-generation antipsychotics
-
e have an atypical mechanism of action for efficacy.
-
-
3 Evidence that glutamatergic neurochemical pathways are implicated in schizophrenia comes from the finding that:
-
a phencyclidine can produce psychotic symptoms in healthy humans
-
b phencyclidine does not exacerbate psychotic symptoms in chronic schizophrenia
-
c phencyclidine is an agonist at glutamatergic (NMDA) receptors
-
d genetic association studies have not revealed glutamatergic-related markers
-
e glutamatergic agonists have been shown to be efficacious in phase III clinical trials.
-
-
4 Regarding molecular genetic studies in schizophrenia:
-
a the DISC1 gene was originally recognised using large GWAS
-
b the NRG-ErbB pathway has a role in dopaminergic neurotransmission
-
c several GWAS have implicated members of the neuregulin pathway
-
d studies have identified multiple genetic variants that contribute significantly to risk of schizophrenia in all cases
-
e these studies cannot be used to identify patients at risk of clozapine-induced agranulocytosis.
-
-
5 The use of translational drug discovery paradigms:
-
a does not involve using biomarkers
-
b precludes clinicians from informing the discovery paradigm
-
c may reduce the attrition rate of drugs under development
-
d should lead to more ‘blockbuster’ drugs
-
e does not require better preclinical disease models.
-
MCQ answers
| 1 | e | 2 | c | 3 | a | 4 | c | 5 | c |
Acknowledgement
With thanks to Dr Marion James of ApotheCom ScopeMedical for editorial assistance in the development of this manuscript.







eLetters
No eLetters have been published for this article.