The range of placebo mechanisms can be bewildering, but evolution provides an overarching theoretical framework that permits the integration of the different levels of explanation. Reference TinbergenTinbergen's (1963) classification, for example, divides the causes of behaviours such as placebo responses into proximate mechanisms and ultimate mechanisms (Box 1). This framework allows the integration of physiology, neuroscience, social and developmental psychology, psychodynamics, anthropology and evolutionary biology.
BOX 1 Tinbergen's classification of the causes of behaviour
Proximate mechanisms
Causation (mechanism)
-
• Immediate psychological and physiological stimuli: treatment and the care setting
-
• Mental processes: meaning, expectation, classical conditioning, emotional change,
-
• Social processes, interpersonal relationships
-
• Neurochemical substrate of the brain and body (see Box 2)
Development (ontogenesis)
-
• Culture, ritual, attachment style
Ultimate mechanisms
Evolution (phylogenesis)
How did the behaviour evolve?
-
• ?Selected traits
-
• ?Epiphenomenon of bonding, and the attachment system
Function (adaptation)
What evolutionary advantage does the behaviour confer?
-
• Conservation of resources
-
• Matching healing to environment and risk
We will start by considering the proximate mechanisms, which are subdivided into: causation, which includes immediate psychological and physiological stimuli, meanings, learning and the neurochemical substrate; and development (ontogenesis) – how behaviour is influenced by early experience and how it changes with age (Fig. 1).
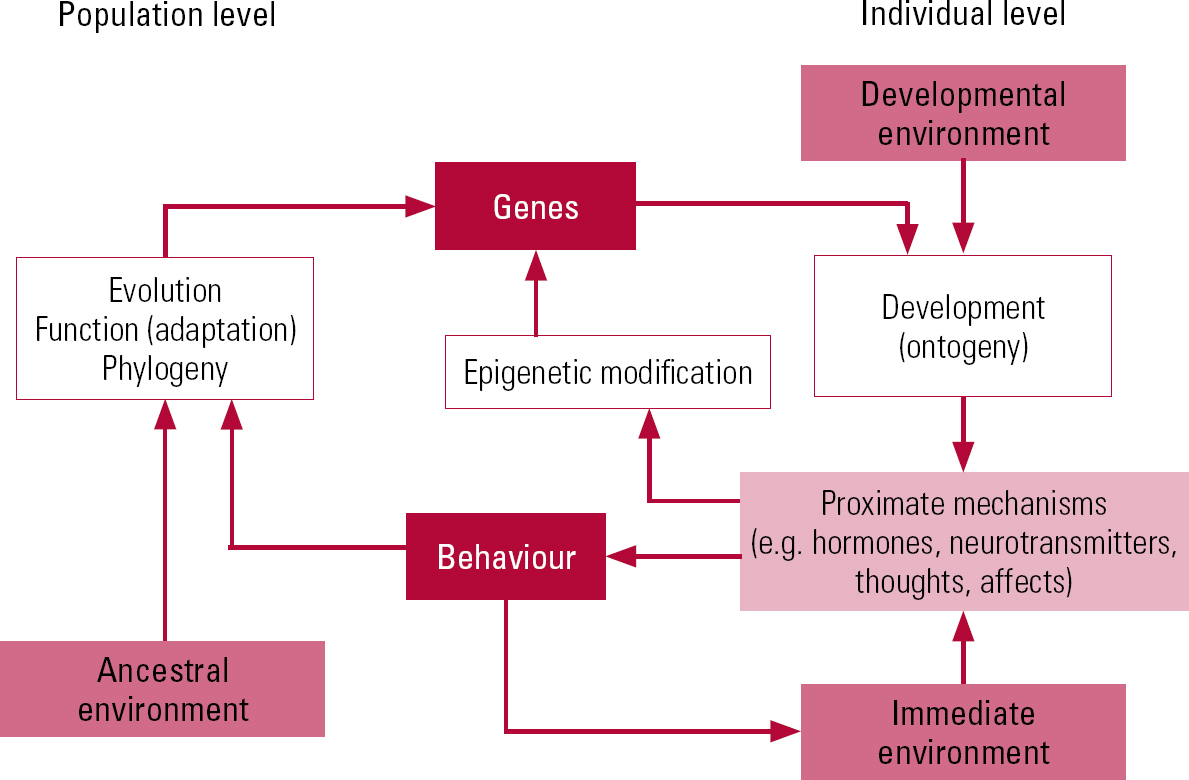
FIG 1 Causal relationships (denoted by arrows) in human behaviour.
Causation
Physiological processes
Placebos lead to changes in physical state, and a growing number of physiological variables that show placebo responses have been identified (Box 2). There are many excellent reviews of this area and the reader is directed to Reference Finniss, Kaptchuk and MillerFinniss (2010) or Reference Benedetti, Mayberg and WagerBenedetti (2005).
BOX 2 Examples of proximate physical mechanisms of placebo
Pain
-
• Activation of endogenous opioids and dopamine (placebo); activation of cholecystokinin and deactivation of dopamine (nocebo)
Parkinson's disease
-
• Release of dopamine in the striatum
-
• Changes in neuronal activity in basal ganglia and thalamus
Depression
-
• Changes in electrical and metabolic activity in different brain regions (e.g. ventral striatum)
Anxiety
-
• Changes in activity of the anterior cingulate and orbitofrontal cortices; genetic variants of serotonin transporter and tryptophan hydroxylase
Addiction
-
• Changes of metabolic activity in different brain regions
Cardiovascular system
-
• Reduction of β-adrenergic activity of heart
Respiratory system
-
• Conditioning of opioid receptors in the respiratory centres
Immune system
-
• Conditioning of some immune mediators (e.g. interleukin 2, γ-interferon, lymphocytes)
Endocrine system
-
• Conditioning of some hormones (e.g. growth hormone, cortisol)
Physical performance
-
• Activation of endogenous opioids and increased muscle work
Alzheimer's disease
-
• Prefrontal executive control and functional connectivity of prefrontal areas
(Reference Finniss, Kaptchuk and MillerFinniss 2010, with permission of Elsevier)
Mental and social processes
There are many proximate psychosocial mechanisms involved in placebo responses. To aid discussion we have classified them using three arbitrary and somewhat overlapping categories:
-
• patient-generated effects
-
• interpersonal healing: clinician-generated effects
-
• interpersonal healing: the patient–clinician relationship.
Patient-generated effects
‘Meaning responses’ and expectations
The meanings that patients attribute to interventions contribute to clinical effects. This effect is idiosyncratic, as it depends on attributions that are influenced by personal history, background and culture (Reference Moerman and JonasMoerman 2002). ‘Meaning responses’ may explain the large differences found between active and inactive placebos. Active placebos are medications used in placebo arms of trials that exert some pharmacological effect that the patient can perceive. The different physiological responses to an active drug and an inert placebo may lead patients and assessors to identify whether or not they are receiving active treatment or placebo. This leads to unmasking (‘unblinding’) and different expectations of treatment and bias in favour of the active drug. Studies have found that drugs, including antidepressants, can be distinguished from placebo more readily than would be predicted by chance (Reference White, Kando and ParkWhite 1992). Unmasking may occur because of the therapeutic effect of the medication or because of side-effects. In both circumstances it could affect the measured outcome.
According to Reference Stewart-Williams and PoddStewart-Williams & Podd (2004a), the expectancy construct has largely replaced related constructs, such as faith and hope, in placebo research. Patients who expect a treatment to help them are more likely to improve, regardless of the treatment. One study, for example, considered post-operative analgesia (Reference Benedetti, Maggi and LopianoBenedetti 2003). Some of the patients receiving analgesia knew that they were receiving it, whereas others did not. The efficacy of the analgesia was greater in the patients who were aware of receiving it. Similarly, being aware that treatment was being withdrawn worsened symptoms more than when treatment was withdrawn without the patient's knowledge. Another study found that dermatology patients given placebo phototherapy reported significant improvements in the condition of their skin, although no changes were detected by masked assessors, suggesting that it was perception only that had altered (Reference Kelley, Boulos and RubinKelley 2009).
An analysis of trials comparing tricyclic antidepressants with inert and active placebos found that active placebos were superior to inactive placebos (Reference ThomsonThomson 1982). Thomson suggested that side-effects may enhance the placebo effect of active medication. A Cochrane review of antidepressant trials using active placebos estimated the effect size of antidepressants to be smaller than estimates produced by comparing antidepressants with inactive placebos (Reference Moncrieff, Wessely and HardyMoncrieff 2004). The authors concluded that their findings were consistent with the hypothesis that effect sizes in antidepressant trials are inflated by the expectations of all participants, including researchers.
Emotional change theory
When people take placebos that they think will lead to the amelioration of unpleasant symptoms or that enhance their sense of mastery and control over a disease, this is likely to promote a reduction in anxiety and stress, which in turn may lead to improvements in psychological and physical health. Reduced levels of depression and demoralisation may provide a further contribution (Reference Stewart-WilliamsStewart-Williams 2004b).
Classical conditioning
Patients who have experienced symptom improvement (unconditioned response) after receiving an active treatment (unconditioned stimulus) may also show improvement (conditioned response) when they receive an inactive treatment or placebo (conditioned stimulus). This has been clearly demonstrated in animal experiments showing that the immune system of rats can be conditioned to respond to placebos (Reference Ader and CohenAder 1975).
Expectation, ‘meaning response’ and conditioning are related and overlapping concepts. Stewart-Williams & Podd argue broadly that expectation is conscious, whereas classical conditioning is unconscious, but that these processes may occur together and have mutual influences (Reference Stewart-Williams and PoddStewart-Williams 2004a). In the debate over whether the placebo effect is due to expectancy or to conditioning, Reference Stewart-WilliamsStewart-Williams (2004b) concluded that expectancy is at the heart of most placebo effects in people, but acknowledged that classical conditioning plays a role in some cases: ‘The effects of expectancies are sometimes unmediated but in other cases are mediated by changes in emotional state, immune system function, perception, or behaviour. Although expectancies are implicated in most placebo effects, a small number of placebo effects may be solely attributable to non-conscious contingency learning’. Reference KirschKirsch (2005) reached similar conclusions in a review of psychotherapy research, reporting that placebo effects are generally mediated by expectancy but that conditioning can have additional or independent effects.
Personality and individual variation
Anxiety predicts larger placebo responses (Reference BeecherBeecher 1956), as do positive expectations about the doctor and treatment, and faith in the doctor and treatment. Beyond this, attempts to find consistent correlations between an individual's personality and placebo-responding in drug trials have not been successful (Reference Doongaji, Vahia and BharuchaDoongaji 1978). Reference LewithLewith (1987) commented on the dramatic differences in placebo response between individual patients and between trials, and concluded that patients respond to placebos in an idiosyncratic manner.
Much effort continues to be invested in identifying ‘placebo responders’ in trials of antidepressants, so that they can be excluded from subsequent analyses, in the hope that this will lead to larger measured drug effects. Some might consider this to be sophisticated manipulation of data to further commercial interests. It does reduce the external validity of the results obtained. However, although situation factors and individual state factors have been demonstrated to produce significant placebo effects, individual traits have not.
Clinician-generated effects
Patients are profoundly affected by, and attach great importance to, the behaviour of their clinicians towards them. A national survey of adult in-patients in National Health Service (NHS) hospitals in England (Reference BoydBoyd 2007) found that, of the top ten aspects of treatment patients rated as most important (out of 82 different aspects of in-patient care), nine concern the clinical relationship and clinicians' behaviour (Box 3). Patients ascribe meaning to what their doctor is wearing and to the manner in which the doctor communicates with them. Their confidence in their clinician is related to how they perceive him or her and will affect their responses to treatment (Reference Moerman and JonasMoerman 2002).
BOX 3 The ten most important aspects of care, as rated by NHS hospital in-patients
-
1 The doctors know enough about my medical history and treatment
-
2 The doctors can answer questions about my condition and treatment in a way that I can understand
-
3 I have confidence and trust in the hospital staff who treat me
-
4 The doctors wash or clean their hands between touching patients
-
5 The nurses know enough about my medical history and treatment
-
6 Before my operation or procedure, I get a clear explanation of what will happen
-
7 The risks and benefits of my operation or procedure are explained to me in a way that I can understand
-
8 The nurses wash or clean their hands between touching patients
-
9 The rooms and ward are clean
-
10 The doctors and nurses are open with me about my treatment or condition
(Reference BoydBoyd 2007: p. 24)
Reference ThomasThomas (1987) examined whether the manner in which general practitioners (GPs) conducted consultations – either ‘positive’ or ‘non-positive’ – affected patients who presented with subjective symptoms but no objective signs. Patients had better recovery and reported greater satisfaction when their GP had a positive manner. The style of the consultation had a greater effect on outcome than receiving or not receiving a treatment.
Patients who received sham acupuncture as treatment for irritable bowel syndrome experienced greater improvement in symptom severity and quality of life if the clinician fostered a positive relationship by showing warmth, attention and confidence (Reference Kaptchuk, Kelley and ConboyKaptchuk 2008). Doctors who were positive and enthusiastic when delivering a placebo increased its effectiveness compared with doctors who were more apathetic about the same treatment (Reference Gryll and KatahnGryll 1978).
What doctors believe about the treatments they are administering can affect clinical outcomes even when they do not vocalise their beliefs to patients. In one arm of a study of analgesia, doctors gave an injection that they believed could contain naloxone, fentanyl or placebo, i.e. it would be expected to increase, decrease or have no effect on pain (Reference Gracely, Dubner and DeeterGracely 1985). These patients had better outcomes than those in the other arm of the study, where doctors believed that the injection contained either naloxone or placebo, i.e. would be expected to increase pain or have no effect. In reality, all patients received a placebo. Here it was the doctors' beliefs about the treatment that were manipulated.
The US National Institute of Mental Health Treatment of Depression Collaborative Research Program reported that imipramine hydrochloride plus clinical management was significantly more beneficial than placebo plus clinical management for individuals undergoing treatment for major depressive disorder (Reference Elkin, Parloff and HadleyElkin 1985). However, when the results were re-analysed to look at the effects of individual psychiatrists on outcome it was found that 9.1% of the variability in self-reported outcome was due to the psychiatrist providing the treatment (Reference McKay, Imel and WampoldMcKay 2006) and that the effect of the psychiatrist was nearly three times larger than that of the medication. This was more pronounced on the self-report outcome measure (the Beck Depression Inventory, where 9.1% of the variance was attributable to the psychiatrist and only 3.4% was attributable to the treatment) than on the observer-rated outcome measure (the Hamilton Rating Scale for Depression, where the results were 6.7% v. 5.9%). The psychiatrists whose patients had superior outcomes had better outcomes for both active treatment and placebo. If treatment outcomes vary between psychiatrists (as is the case in psychotherapy), then observations within psychiatrists are not independent and the probability of detecting differences between treatments and the effect sizes attributed to those differences are artificially inflated. Consequently, the failure to account for individual psychiatrist differences in other antidepressant trials may have inflated the apparent antidepressant treatment effect size. To our knowledge, the 1985 study by Elkin et al has not been replicated using more modern antidepressants.
Patient–clinician relationship
During the treatment of an illness, particularly a chronic illness, the clinician may meet the patient regularly, possibly show an interest in their life, make a formulation of the problem, propose solutions, express concern about the effects of treatment, inquire about the patient's current situation and answer their questions. This implies, whether or not intended or realised, the beginning of a therapeutic process between clinician and patient. Some placebo responses may therefore be considered as due in part to a therapeutic relationship. This is irrespective of whether or not clinicians consider themselves to be providing psychotherapy. If one considers psychotherapy as a patient–clinician relationship, then it is in psychotherapy that this relationship has been studied in most depth. In the next two sections, we consider what psychotherapy process research reveals about the patient–clinician relationship.
Placebo as psychotherapy, psychotherapy as placebo
Early research into the process of psychotherapy explored the relative contributions of specific techniques and non-specific relationship factors. Reference Bowers and ClumBowers & Clum (1988) conducted a meta-analysis of 69 studies comparing forms of behavioural therapy with placebo control conditions to obtain an estimate of the incremental contribution of specific behavioural interventions to the non-specific effects of placebo psychotherapy. They operationalised placebo psychotherapy as having two primary components: discussion of the patient's problem and manipulation of the patient's belief that they were receiving an effective treatment. The meta-analysis included a subset of studies that had a no-treatment condition in addition to a placebo condition, which permitted an analysis of the contributions of non-specific as well as specific treatment effects. The authors concluded that placebo treatment, defined as non-specific psychological intervention that included therapist–patient interactions and discussion of patients' problems, produced a greater effect than no treatment (placebo v. no-treatment effect size = 0.21), but less of an effect than a specific therapy (specific therapy v. placebo effect size = 0.55).
However, claims for the effectiveness of specific techniques in trials have been largely explained by strong investigator allegiance biases, which have been reported to account for 69% of the variance in outcomes (Reference Luborsky, Diguer and SeligmanLuborsky 1999). Different bona fide short-term psychotherapies (psychoanalytic, behavioural, cognitive, humanistic or integrative)have globally comparable outcomes across a range of conditions, with effect sizes in the region of 0.85 (Reference Stiles, Barkham and TwiggStiles 2006; Reference Cuijpers, van Straten and AnderssonCuijpers, 2008). As psychotherapy process research revealed that specific techniques account for little of the variance in outcome, focus shifted to the so-called non-specific effects of being in therapy. Non-specific factors have been conceptualised in various ways, but generally include the therapeutic alliance (consistently accounting for the most variance in outcome), patient factors (such as engagement), therapeutic focus (having a specific focus leads to better outcome), expectation of a good outcome (clinician and patient expectation of success tends to be self-fulfilling), and patient and therapist characteristics. Patient characteristics include belief in the rationale of treatment and degree of disturbance (see below) (Reference Messer and WampoldMesser 2002). However, the averaging effect of randomised controlled trials may obscure important differences at the level of individual patients at different points in psychotherapy.
Change-promoting processes in psychotherapy
In a study of the non-specific hypothesis of therapeutic effectiveness, Jones et al analysed transcripts of therapy sessions using the Psychotherapy Process Q-Sort, a method designed to provide a standard language for the description and classification of the therapy process (Reference Jones, Cumming and HorowitzJones 1988). The sort used a set of 100 items, each representing a clinically relevant variable describing the interaction between the patient and the therapist. Regression analysis demonstrated that 27 of the 100 items were significant predictors of outcome. Almost all significant findings were interaction effects, with the item predictive of outcome interacting with the patient's pre-treatment level of disturbance. Only one item (‘Patient achieves a new understanding or insight’) predicted outcome independent of the level of pathology. ‘Expressive’ therapy processes predicted successful outcome in patients with lesser pre-treatment disturbance, and ‘supportive’ approaches predicted successful outcome in patients with greater pre-treatment disturbance, reflecting the well-known distinction between ‘expressive’ and ‘supportive’ psychotherapy approaches. That is, therapists who successfully treated the most troubled individuals frequently supported the patient's defences through a calm, attentive compliance to avoid upsetting the patient's emotional balance. They also sometimes intervened to help the patient avoid or suppress disturbing ideas or feelings.
Jones et al reasoned that studies have failed to identify consistent correlations between specific aspects of the therapy process and treatment outcomes because they have sought simple, direct associations rather than more complex conceptualisations that reflect the interaction of different variables in clinical treatment. They questioned the distinction between therapeutic technique and general relationship factors, arguing that when psychotherapy process is looked at in sufficient detail, a series of specific factors can be identified, which vary in different situations. They concluded that the non-specific hypothesis is oversimplified and the concept of ‘non-specific factors’ is fairly meaningless. Many of the specific interventions used in the sessions analysed in this study, such as the therapist explaining the rationale behind the treatment, using humour, and giving information, guidance, reassurance and clarification, can, if used appropriately, increase therapeutic alliance and clinical effectiveness in many clinical interactions.
In contrast to earlier psychotherapy process research, this moment-to-moment evaluation of individual patient–therapist interaction appears to be a more fruitful level of analysis. Analysis at this level draws support from research into child development and caregiver–infant interactions which has identified the importance of a number of factors to the development of emotional resilience in the infant: moment-to-moment affective interchanges, synchrony, reciprocity, matching, coherence and attunement (Reference Fonagy, Gyorgy and JuristFonagy 2004; Reference Tronick and NortonTronick 2007). Psychoanalytic writers from different schools have shown how one person (prototypically the mother or other early caregiver, but also the psychotherapist, doctor or nurse) is able to soothe distress in another (infant or patient), transforming distress or anxiety into something more meaningful and manageable. Comparable processes have been described variously as ‘containment’ (Reference BionBion 1962), ‘attunement’ (Reference SternStern 1985) and ‘holding’ (Reference WinnicottWinnicott 1945). These interpersonal processes of emotional attunement or empathy contribute significantly to the building of therapeutic alliances.
Pharmacotherapy and transference
In psychoanalysis, transference refers to the process by which emotions and desires originally associated with one person, such as a parent or sibling, are unconsciously shifted to another person (or even an object, such as medication). Thus, it can be considered a specific subset of meaning responses. Medicines often have special emotional significance for patients that goes way beyond any realistic appreciation of their physical effects:
‘The psychiatrist prescribing medication is no less a transference figure than the psychotherapist. For patients, the decision to comply or not comply with the doctor's recommendations activates unconscious issues of parental expectations. When patients refuse to take medication as prescribed, psychiatrists often react by becoming more authoritarian, insisting that their orders be followed without question. This approach usually backfires because it merely exacerbates the transference disposition to see the doctor as a demanding parental figure’ (Reference GabbardGabbard 2005: p. 144).
Medications may be invested with notions of food, nourishment and care (Reference TutterTutter 2006) or, in more paranoid contexts, poisoning: patients with psychosis can hold paranoid and masochistic beliefs about antipsychotic medication (Reference TitelmanTitelman 1999). Medication may also act as a comforter or security blanket. For example, someone with panic disorder may be unable to leave the house without diazepam in their pocket, even if they have not needed it for years. It is not only medication that can fulfil such an important emotional function: institutions or teams may do so too. The knowledge of being ‘held by’ or ‘being under’ a clinician, out-patient clinic or mental health team may be important in preventing relapse, and the dangers of precipitating relapse by discharging patients with chronic disorders is familiar. The psychiatrist and psychoanalyst Henri Rey used the expression ‘brick mother’ to describe how a psychiatric hospital itself can represent a place of safety and containment for patients who are afraid of breaking down (Reference Steiner and JacksonSteiner 2001).
Thus, psychotherapeutic skills and understanding are not distinct from other aspects of healthcare provision; rather, they represent a highly developed form of expert consultation which has relevance for the rest of psychiatry and the whole of medicine when dealing with illness.
Development (ontogenesis)
Individual development of the capacity to respond to placebo
Without prior experiences of healing situations, it would not be possible for expectancies to develop. Thus, culturally specific healing practices might be less effective if used with individuals alien to them. Consequently, some degree of acculturation or familiarity with the healing practices may be required to activate placebo responses.
A clear forerunner of the placebo response can be seen when a child who has fallen and scraped a knee goes to a parent in tears, and is cured by a kiss. Even earlier in development, rocking, singing, soothing and other empathetic responses of caregivers to distressed infants can all be seen to have elements in common with placebo effects. A kiss will not have the same soothing effect irrespective of who gives it. This highlights the importance of trust and emotional attachment in relationships.
Attachment to caregivers is a primary instinctual behavioural system (Reference BowlbyBowlby 1969). Attachment style can be secure, insecure or disorganised, depending on early infant–carer interactions. Attachment style influences vulnerability to psychiatric disorders and patterns of engagement with professional caregivers (Reference MaMa 2006, Reference Ma2007). Studies in diabetes have shown that attachment style influences how individuals adhere to treatment to such an extent that it is predictive of the degree of diabetic control that they achieve (Reference Ciechanowski, Katon and RussoCiechanowski 2001, Reference Ciechanowski, Russo and Katon2004). Patients who adhere to medication regimens (even if the medication is placebo) have better outcomes than those who do not (Reference Horwitz and HorwitzHorwitz 1993), the so-called ‘healthy adherer’ effect. We are not aware of any research exploring direct links between attachment and placebo responses.
Reference Miller, Colloca and KaptchukMiller et al (2009) have asked why it should take the intervention of a healer to release placebo effects. The solution they propose is that:
‘in the face of illness-related distress, it is difficult to generate hope for relief by personal strategies. The illness itself impedes hoped-for relief. Typically, in the throes of suffering from illness, especially if worried about mortality or serious morbidity, we can't think, wish, or will the expectation that relief is in store. It takes the intervention of an authoritative or protective figure to promote hope and expectation for relief, leading to the placebo effect’ (Reference Miller, Colloca and KaptchukMiller 2009: p. 532).
The decision to believe, it would appear, is not in our hands.
Now we will turn to ultimate mechanisms of the placebo effect: phylogenesis (evolution) and function (adaptation).
Evolution (phylogenesis)
As already noted, placebo effects occur in various mammals. The immune system of rats responds to placebos after conditioning with immunosuppressive drugs (Reference Ader and CohenAder 1975). Horses with airway heaves (equine asthma) have objective responses to acupuncture, but no more so than to sympathetic human handling (Reference Wilson, Berney and PeroniWilson 2004). Indeed, sympathetic handling reduces a range of physiological markers of arousal in domesticated mammals.
Anthropologists have described healing rituals in all cultures. Physical examination, medical paraphernalia, jargon, clinic routines can all be seen from an anthropological perspective as elaborate cultural rituals to manage illness, distress and death (Reference FoxFox 1992; Reference Thompson, Ritenbaugh and NichterThompson 2010). Placebo effects may be considered as technical explanations of how healing and caring works. The universality of placebo responses suggests a likely evolutionary basis to the underlying mechanisms.
Function (adaptation)
Placebo responses permit the organism to modify its internal processes and behaviour through the somatic and autonomic nervous systems, endocrine system and immune system. The stimuli for placebo responses are our perceptions of the internal and the external, material and psychosocial environments, now or in the near future, particularly the state of our social interactions, i.e. feeling valued, cared for, understood, respected and so on, which lead us to feel more positive and hopeful, and reduce fear. Adaptive advantages might result from evolution of abilities to modify our internal environment in the light of positive evaluations of our external environments, social interactions and appraisals of the future.
Defence regulation
Reference NesseNesse (2008) stresses that placebo responses primarily entail modification of the body's defences rather than of disease processes. Evolution has selected for mechanisms that defend against injury, infection or poisoning, which threaten survival and reproductive fitness. The central nervous system regulation of these defences, examples of which are listed in Box 4, is influenced by appraisals of the environment. This evolved capacity for regulation functions as a health management system.
BOX 4 Examples of the body's defences
-
• Somatosensory: pain, lethargy, nausea, anxiety, depression, fever, itching
-
• Skeletal: flight, freezing
-
• Visceral: sneezing, coughing, vomiting, diarrhoea
-
• Motor responses
-
• Humoral responses: immune modulation, regulation of the hypothalamic–pituitary–adrenal axis
Defences should be expressed at an optimal level to protect against a given threat, but many defences appear to be over-expressed. A signal-detection analysis can explain this apparent paradox. When the cost of expressing an all-or-nothing defence is low compared with the potential harm it protects against, the optimal system will express many false alarms. For example, vomiting may cost only a few hundred calories and a few minutes, whereas not vomiting may result in a chance, however small, of death from poisoning. This has been dubbed ‘the smoke detector principle’ (Reference NesseNesse 2001).
The over-expression of many defences allows that they can often be dampened without compromising fitness. The regulation of defences allows that otherwise ‘protective’ defences can be turned off both in situations of extreme danger, to facilitate escape, and in situations propitious for recovery, where they may no longer be necessary for protection. This may explain why pain is reduced both when facing immediate threat and when being cared for.
Costs and benefits of defence and tissue repair
Reference HumphreyHumphrey (2000) provides a further reason for the evolution of placebo adaptations. He identifies the biological costs and short-term risks to the organism of repairing itself. Mounting an immune response consumes energy, protein and micronutrients (hence the weight loss associated with immune responses), and there are risks to the self from autoimmune disease. Fever has a huge calorific cost. Prolonged vomiting and diarrhoea lead to loss of energy, electrolytes and water. Rebuilding damaged tissues requires rest, energy and nutrients. Humphrey argues that it is adaptive to the organism, and confers a fitness advantage, to be able to control when to activate these costly self-repair mechanisms, turning them on only when circumstances are propitious for recovery, rather than risking these expenditures at times when the extra costs may further threaten immediate survival.
Attachment and social triggers for self-healing
In John Bowlby's concept of an environment of evolutionary adaptedness (Box 5) the presence of, and receiving care from, members of the clan would indicate a propitious moment. In contemporary life, the availability of solicitous healthcare professionals, with the promise of care, treatment and cure, indicates to the organism that now is a propitious time to invest resources in self-repair, thus triggering the instinctual placebo processes. So when caring, treatment and cure seem distant (i.e. uncaring, rejecting, unconvincing doctors and treatments), the organism may perceive that circumstances are not favourable for recovery and therefore not invest biological resources in self-repair. In addition, unpleasant body defences such as nausea, vomiting, cough, fever, pain and muscular spasm may remain active.
BOX 5 The environment of evolutionary adaptedness
‘In the case of biological systems, structure takes a form that is determined by the kind of environment in which the system has been in fact operating during its evolution […] This environment I propose to term the system's “environment of adaptedness.” Only within its environment of adaptedness can it be expected that a system will work efficiently.’
(Reference BowlbyBowlby 1969: p. 47)
Some support for the importance of perceptions of the favourability of the social environment and of its relationship to immune system function, growth, health and survival comes from the observations of extreme emotional neglect in orphanages at the beginning of the 20th century. In a study of children in orphanages in the USA, Reference SpitzSpitz (1945) reported death rates among infants in the first year of life of 32% to 75%. Reference BakwinBakwin (1942) described increased susceptibility to infection among infants in orphanages despite high hygienic and nutritional standards, which reversed when infants received more handling and ‘mothering’. He argued that loneliness was an important factor in failure to thrive, susceptibility to infection and ultimately death.
Not all aspects of the human capacity for responding to placebos are necessarily adaptive in their own right. The traits of placebo-responding may be emergent properties, or epiphenomena, of something that is adaptive. For example, Reference Miller, Colloca and KaptchukMiller et al (2009) have suggested that social living, with a prolonged period of dependency on parents, is what gives rise to the power of authority/parental figures to influence our perceptions of security and our feelings of well-being. The goal of the attachment system is to maintain proximity to caregivers who would provide safety from danger. Thus, at times of threat, the attachment system becomes activated. Manifestations of attachment behaviour change with the stage of the life cycle and attachment style, but at times of subjectively perceived threat, which includes illness, proximity and caring are sought from attachment figures, who may come to include trusted professional carers (Reference BowlbyBowlby 1957, Reference Bowlby1969). Attachment to caregivers is therefore adaptive and selected for, and placebo-responding may be an emergent property of the attachment system.
Evolutionary models of depression emphasise adaptive functions of depressed mood and associated behaviours, including communicating a need for help, signalling yielding in a hierarchy conflict, and fostering disengagement from commitments to futile or dangerous goals such as challenges to dominant figures or actions without necessary resources (Reference NesseNesse 2000). Seen from a functional perspective, it is to be expected that depression would respond to interpersonal caring. Thus, to consider the response to caring as a ‘placebo’ response is to fail to understand that one of the adaptive functions of depressed behaviour and mood is precisely to elicit caring.
Refining the placebo effect
Any given placebo response is likely to be multifactorial and idiosyncratic, and thus the contribution to individual clinical improvement is difficult to predict. Placebo effects vary widely, as does the conscious influence that clinicians can have over them, but they are definitely not irrelevant. Reference Ernst and ReschErnst & Resch (1995) have suggested that:
where direct physical effects (true treatment effects) are the mechanical or chemical effects of medication, surgery or other intervention.
Independent effects are spontaneous remission, natural variation, regression to the mean, time effects and unidentified parallel interventions, including the Hawthorne effectFootnote a and artefacts of trial design.
Placebo effects include:
-
1 patient effects (conditioning, expectation, meaning response, emotional change, personality, attitude towards change, etc.);
-
2 clinician effects (communication style, authority, warmth, compassion, guidance, etc.);
-
3 the patient–clinician relationship (fit, rapport, containment, empathy, being alongside, accurate understanding and clarification of problems, compassion, dialogue, attachment, etc.).
However, the role of interpersonal healing is subtle, complex and profound. There is no evidence that its effects are additive, and they may have complex non-linear interactions. Arguably, the very idea that ‘true’ drug effects can be isolated in a simple way from the clinical encounter between patient and doctor is misleading.
Conclusions
The placebo has been an elusive concept. It is not a unitary thing and has no unique properties of its own. However, placebo effects are real psycho-biological events. The magnitude of placebo effects is determined by the meanings and expectations that individuals bring, the context, which includes the interpersonal relationship between patient and doctor, and the wider social and institutional setting. Patients' expectations, conscious or unconscious, are influenced by past experiences and relationships, present relationships with clinicians and expectations about the future.
In illness, the doctor–patient relationship can have greater effects on clinical outcomes than the specific evidence-based therapy being administered. This has been named the efficacy paradox (Reference WalachWalach 2001) and it is as true for pharmacotherapy as for psychotherapy.
Maximising therapeutic placebo effects is an effective and valid clinical goal. Skilful consulting and attention to the doctor–patient relationship increase therapeutic alliance and clinical effectiveness. This is one of the most effective, safest and cost-effective interventions available to doctors.
It cannot be overstated that a medical system that feels and appears unfriendly, rejecting or overstretched will be less effective and patients will abandon it in favour of one that does not, irrespective of the quality of the evidence for technical aspects of the treatments offered. As long as medical care is experienced as impersonal, unconcerned and uncaring, patients will seek out those human healing attributes elsewhere, as they provide the emotional setting in which the patient can experience being looked after and start to recover.
MCQs
Select the single best option for each question stem
-
1 Placebo effects do not include:
-
a psychotherapeutic effects of the encounter with the physician
-
b direct physical or mechanical effects of the procedure
-
c patient effects intrinsic to the individual patient's beliefs
-
d clinician effects due to the appearance of the physician
-
e patient–clinician relationship effects.
-
-
2 The following do not contribute to true placebo responses:
-
a patients' expectations
-
b patients' meaning responses
-
c spontaneous recovery in patients
-
d patients' health beliefs
-
e patients' attitudes towards change.
-
-
3 True placebo effects include:
-
a natural course of the disease
-
b classical conditioning
-
c natural variation of the disease
-
d trial baseline effects
-
e other unidentified, parallel interventions.
-
-
4 The size of placebo effect in a given trial is:
-
a fixed and equal in all arms of the study
-
b the same in all trial patients and all trial situations
-
c irrespective of trial design
-
d a linear property that can be subtracted from the overall effect size
-
e influenced by the relationship with treating clinicians.
-
-
5 Placebo mechanisms that reduce pain are mediated by:
-
a activation of cholecystokinin
-
b deactivation of dopamine
-
c activation acetylcholine
-
d activation of endogenous opioids
-
e activation of serotonin.
-
MCQ answers
| 1 | b | 2 | c | 3 | b | 4 | e | 5 | d |
Acknowledgement
The authors would like to express their gratitude to Professor George Ikkos for his helpful suggestions on this article.




eLetters
No eLetters have been published for this article.