Introduction
Adults aged over 50 years make up more than 36 per cent of the population of the United Kingdom (UK) and the Office for National Statistics (2019) estimates that by 2050, one in four people will be over the age of 65 years and the fastest growing age group are the over 85 years. Rao and Roche (Reference Rao and Roche2017) reported that increasing risky drinking, in terms of health risks resulting from excessive consumption, are rising among older people in the UK (see also Office for National Statistics, 2018). Further, the literature shows that numbers of older adults presenting for alcohol treatment has risen dramatically (Wadd et al., Reference Wadd, Forrester, Galvani and Lapworth2011; Knott et al., Reference Knott, Scholes and Shelton2013; Wadd and Galvani, Reference Wadd and Galvani2014; Frisher et al., Reference Frisher, Mendonça, Shelton, Pikhart, De Oliveira and Holdsworth2015). Yet there is little in the literature to explain the reason for this.
Amongst the general population, factors associated with increased and higher-risk drinking at older ages are being male, not having an ongoing health problem, having a ‘white’ ethnic identity and having a minority sexual orientation (Borok et al., Reference Borok, Galier, Dinolfo, Welgreen, Hoffing, Davis, Ramirez, Liao, Tan, Karno, Sacco, Lin and Moore2013; Wilson et al., Reference Wilson, Kaner, Crosland, Ling, McCabe and Haighton2013; Rao et al., Reference Rao, Schofield and Ashworth2015; Bryan et al., Reference Bryan, Kim and Fredriksen-Goldsen2017). However, Drabble et al. (Reference Drabble, Midanik and Trocki2005), from analysis of the 2000 US National Alcohol Survey, found no significant effect for men who have sex with men drinking more, but they did find some evidence for lesbian and bisexual women. Kuerbis (Reference Kuerbis2020) discussed how the baby-boom generation are vulnerable to increased hazards from alcohol due to biological factors which reduce tolerance to alcohol with age, comorbidity with other health conditions, and psychosocial factors arising from bereavement, loneliness, caring responsibilities and retirement. The retirement effect is especially so for those who reside in communities where high levels of socialisation is encouraged and those who had derived high job satisfaction from work or had encountered high levels of workplace stress (Kuerbis and Sacco, Reference Kuerbis and Sacco2012; Kuerbis, Reference Kuerbis2020). These studies suggest that loneliness, isolation and lack of emotional support can foster higher-risk drinking and that having a close friend can prevent high-risk drinking, but it depends on the nature of the relationships and networks. Platt et al. (Reference Platt, Sloan and Costanzo2010) and Brennan et al. (Reference Brennan, SooHoo, Lemke and Schutte2016) drew attention to having a history of problematic drinking in earlier life being associated with increased drinking later in life. The increased likelihood of problem alcohol use in later years is also associated with having a history of drinking, having friends who approved of drinking and having financial resources to do so (Hajat et al., Reference Hajat, Haines, Bulpitt and Fletcher2004; Moos et al., Reference Moos, Schutte, Brennan and Moos2010b; Wilson et al., Reference Wilson, Kaner, Crosland, Ling, McCabe and Haighton2013; Kelly et al., Reference Kelly, Olanrewaju, Cowan, Brayne and Lafortune2018; Kim et al., Reference Kim, Spilman, Liao, Sacco and Moore2018).
Social influences may also protect against problematic drinking. For example, religion has been reported as particularly important for creating strong bonds and linked to lower-risk drinking (Moos et al., Reference Moos, Schutte, Brennan and Moos2010b). Tamres et al. (Reference Tamres, Janicki and Helgeson2002) found from a meta-analysis of studies that women were more likely to adopt coping strategies which involve discussing problems with others and seek more emotional support than men, and this increased social engagement might inhibit problematic drinking. Nolen-Hoeksema (Reference Nolen-Hoeksema2004) discusses social sanctions among older drinkers (notably the disapproval of others and negative imagery of drunk women) as a positive influence and that women were more influenced than men, especially in avoiding stigma associated with heavy drinking.
From the literature mentioned above, it is clear that the consumption of alcohol is affected by social interactions with others and the community. However, these more socially oriented studies tend to focus on single indicators to characterise multifaceted social constructs. Consequently, there is need to investigate alcohol use (and risks) among older adults using more comprehensive and meaningful social variables. These variables can include variables reflective of the nature of relationships; including family composition; caring responsibilities and close friends; social status as measured by employment, education levels and economic standing; and beliefs, attitudes and understanding of public health issues. These variables can be placed under the umbrella of social capital which is characterised by the attributes and relationship with actors and entities in a person's social network, and the value they derive from being network members.
Social capital – a multi-faceted social construct
The widely cited scholars Bourdieu (Reference Bourdieu and Richardson1986), Coleman (Reference Coleman1990) and Putman (Reference Putman1993) are often credited for popularising the debate on what constitutes social capital and its diverse range of consequences. Bourdieu (Reference Bourdieu and Richardson1986) was interested in the power dynamics between different groups in society, proposing that connections with social networks create opportunities for members to access resources, thus generating social capital. Coleman (Reference Coleman1990) highlighted the role of social structure in generating social capital, arguing that social capital exists in a range of networks that enable or restrict the actions of members, such as families, communities, school and various other institutions. Coleman (Reference Coleman1990) also highlighted the importance of norms, rules and trust in sustaining relationships in networks. Putman (Reference Putman1993) extended analysis to include levels of civic engagement, such as volunteering and political participation, as extended forms of social capital.
Social capital can be measured at both individual and community levels. Individual-level social capital can be broken down into two components, cognitive and relational social capital (Nahapiet and Ghoshal, Reference Nahapiet and Ghoshal1998). Relational social capital is the relationship with others, the sharing of knowledge and empathy and support within social networks. The cognitive component refers to subjective feelings such as trust in others, acceptability of norms and rules. At the community level, the focus, according to Nahapiet and Ghoshal (Reference Nahapiet and Ghoshal1998), tends to be on ties to structural organisations, and access to resources made available through these ties.
Several studies have used the framework of Nahapiet and Ghoshal (Reference Nahapiet and Ghoshal1998) to measure social capital among alcohol users (e.g. Åslund and Nilsson, Reference Åslund and Nilsson2013; Larm et al., Reference Larm, Åslund, Starrin and Nilsson2016). However, social capital is difficult to measure as there is no set agreement on the validity of constructs, though most scholars agree that a range of indicators should be used to reflect the multi-dimensional nature of social capital (Claridge, Reference Claridge2017). There is no set tool found in the social capital literature base and, as pointed out by Claridge (Reference Claridge2017), researchers tend to develop their own instrument specific to their research context.
Various researchers have investigated the influence of social capital by constructing social capital from attributes of those who a person can access or attributes of the community from data collected by questionnaire, or interviews or administrative data, or by a combination of these methods. Examples include Rose (Reference Rose2000) and Shields (Reference Shields2008), who used survey data to link social capital to health indicators, and Gayen and Raeside (Reference Gayen and Raeside2010), who used interview completed questionnaires to show the importance of social connectedness to disseminate knowledge regarding health care. Burchfield and Mingus (Reference Burchfield and Mingus2008) used interviews in a study of sex offending and its relation to social capital and Fraser (Reference Fraser2021) used administrative data to link social capital to community resilience to climate change. The study of Gayen et al. (Reference Gayen, Raeside and McQuaid2019) of older people's ability to access new employment collected data by a questionnaire survey and face-to-face interviews.
Social capital and alcohol use among older adults
Ties to structural organisations, e.g. workplaces, tend to diminish as people age, while individual-level social capital becomes more important (Zhang and Lu, Reference Zhang and Lu2019). Moreover, individual-level social capital has been found to be a key predictor of health outcomes among older adults (Nyqvist et al., Reference Nyqvist, Forsman, Giuntoli and Cattan2013; Imamura et al., Reference Imamura, Hamano, Michikawa, Takeda-Imai, Nakamura, Takebayashi and Nishiwaki2016; Liotta et al., Reference Liotta, Inzerilli, Palombi, Madaro, Orlando, Scarcella, Betti and Marazzi2018). For example, relational social capital, including family networks, has been reported as having a strong positive effect on health outcomes amongst the over fifties (Alvarez et al., Reference Alvarez, Kawachi and Romani2017; Lu et al., Reference Lu, Jiang, Lou, Zeng and Liu2018). On the other hand, Boneham and Sixsmith (Reference Boneham and Sixsmith2006), Cramm et al. (Reference Cramm, Møller and Nieboer2012) and Holdsworth et al. (Reference Holdsworth, Mendonça, Pikhart, Frisher, De Oliveira and Shelton2016) point out that relational capital tends to decline with age as social networks fragment. Network fragmentation arises through members leaving the network, because of network members dying, moving location, or breaking of connections resulting from leaving organisations such as the workplace, illness or friendship rifts, travel difficulties and economic isolation.
Relational and cognitive capital have been highlighted as important factors for understanding alcohol use among older adults. Older adults who engage in less-resourceful networks are thought to be ‘at greater risk of alcohol abuse’ (Shiovitz-Ezra and Litwin, Reference Shiovitz-Ezra and Litwin2012). High alcohol consumption among adults has previously been associated with low social trust among older men, resulting in lone drinking or heavier drinking with those they trust and minimal moderating influences of those who are not close friends (Lindström, Reference Lindström2005). For adults over 50, poor quality of spousal relationship and friends' approval of drinking are given as causal factors leading to increased drinking by Moos et al. (Reference Moos, Brennan, Schutte and Moos2010a). Network types, in the sense of the preference of engaging with homophilic networks in which members share similar attitudes and values and endorse each other's behaviour (Shiovitz-Ezra and Litwin, Reference Shiovitz-Ezra and Litwin2012), have also been associated with high-risk alcohol consumption.
Evidence from studies conducted among the general adult population (not focused on older people) on the relationship between social capital and alcohol use indicate this may be influenced by gender. For example, Larm et al. (Reference Larm, Åslund, Starrin and Nilsson2016) reported that greater cognitive capital is associated with lower levels of drinking, however, this effect was only observed among those identifying as women. In contrast, there is some evidence that those identifying as men drink more heavily when engaged in networks which give more drinking opportunities (Murphy et al., Reference Murphy, Roberts, Kenward, De Stavola, Stickley and McKee2014).
Chuang and Chuang (Reference Chuang and Chuang2008) found that close neighbourhood ties and social participation are beneficial for both men and women. Additionally, Seid (Reference Seid2016) found socialising with male friends, engagement with organisations and general trust among network members were significantly associated with heavy drinking. Alcohol was argued to play an important role in the socialisation processes. However, these studies did not focus on older adults.
Sexual minority older women have been found to have comparatively higher association with higher-risk drinking than heterosexual women. Bryan et al. (Reference Bryan, Kim and Fredriksen-Goldsen2017) speculated that this might be because heterosexual women when feeling under stress might receive support from discussion with their social networks in a low-alcohol environment, whereas lesbian and bisexual women's social support tends to involve social activities which encourage higher alcohol intake.
Rationale and aim
We know from studies conducted with older adults, in which social capital is defined, that a lower level of social capital is associated with increased risk drinking and even harmful drinking at higher-risk levels. However, these studies are restricted to examining one form of social capital, i.e. cognitive or relational capital, and the relative importance of each are unknown. In addition, these studies do not account for the influence of gender on the relationship between social capital and alcohol risks among older adults. Consequently, the aim of the present study is to examine whether relational and cognitive social capital are associated with higher or lower risk of alcohol use among a sample of adults aged 50 or older, and to assess the extent to which this relationship differs between those identifying as men and those identifying as women.
Materials and methods
The data were collected by a cross-sectional survey of people aged 50 and over recruited from National Health Service (NHS) general medical practitioners (GPs) throughout the UK in 2016. This was done under the auspices of the Drink Wise Age Well project, which was a community multi-level intervention aimed at reducing alcohol use and related harms among people aged over 50 (Seddon et al., Reference Seddon, Wadd, Wells, Elliott, Madoc-Jones and Breslin2019). The survey collected self-reported data on alcohol risk (as measured by the Alcohol Use Disorders Identification Test (AUDIT-10)) (Bohn et al., Reference Bohn, Babor and Kranzler1995) and the social functioning aspects of a person's quality of life, as measured by the short-form 12-item questionnaire (SF-12), which was developed from the 36-item Medical Outcomes Survey (Ware et al., Reference Ware, Kosinsk and Keller1996). The survey was posted to 76,000 people aged over 50 and registered with a GP (Seddon et al., Reference Seddon, Wadd, Wells, Elliott, Madoc-Jones and Breslin2019). GP practices in demonstration areas (intervention-delivery areas) and control areas (no intervention) sent out the survey (with a prepaid postage envelope for return) to all people aged over 50 listed at their practice (Seddon et al., Reference Seddon, Wadd, Wells, Elliott, Madoc-Jones and Breslin2019). A total of 30 NHS general practices were recruited to administer the survey from the following locations: Scotland (Glasgow and Dundee), England (Devon, Sheffield, Lincolnshire and Derby), Wales (Cwm Taf Morgannwg University Health Board and Betsi Cadwaladr University Health Board) and Northern Ireland (Western Health and Social Care Trust and Southern Health and Social Care Trust). NHS GP practices were selected from low, medium and high socially deprived areas within each location.
Everyone registered with designated GP practices and aged over 50 was invited to complete the paper-based questionnaire. These patients were subsequently sent an invitation letter to request participation in the study, and a multi-language information sheet and consent from, as well as a stamped addressed return envelope to send the completed survey. All participants were given the option of completing the questionnaire online or by returning a completed paper questionnaire by mail. All responses were anonymous. It is noted that the value of gaining sensitive information by online means is debatable, as illustrated by De Bernardo and Curtis (Reference De Bernardo and Curtis2013) who report advantages but others, such as Olsson et al. (Reference Olsson, Samuelsson and Viscovi2019), question the representativeness of online surveys directed to older people. Kelfve et al. (Reference Kelfve, Kivi, Johanson and Lindwall2020) argue that both paper-based and online questionnaires should be simultaneously offered when surveying older people. The link to the online questionnaire was in the invitation letter and on the front of the questionnaire. The Snap Surveys (2016) platform was used to facilitate anonymous online data collection using a secure website.
The overall response rate was 22 per cent with 16,678 surveys returned (of which 415, i.e. 2.5%, were returned online). The collected data were then inputted into Microsoft Excel and then to the statistics package Stata 14.0 (StataCorp, College Station, TX) to aid with the analysis.
UK Government statistics show around 24 per cent of over 65-year-olds do not drink at all (NHS, 2017) and as these people are not at risk from alcohol-related harm, we excluded non-drinkers from our analysis (20%, N = 3,313). A further 3,381 cases were excluded because of 5 per cent or more missing values in key variables, leaving 9,984 cases. Examples of key variables with missing values are the AUDIT-10 score with 13.9 per cent missing cases (N = 1,714 cases), ‘I would not tell someone if I had an alcohol problem’ containing 7.5 per cent missing cases (N = 931), ‘I am proud of the community I live in’ having 7 per cent missing cases (N = 868) and ‘people with alcohol problems only have themselves to blame’ with 6.1 per cent missing cases (N = 749).
Ethical approval for this study was granted by the National Health Service Research Ethics Committee UK.
Variables and analyses
The survey was designed to allow investigation of many aspects of older people's quality of life and their alcohol intake and patterns of consumption. The questions of interest for the study reported here covered demographic aspects, measures of the quantity of alcohol consumption and questions to allow the derivation of measures of social capital. The demographic questions included age, sex, sexual orientation, ethnicity, health, marital status, education and religion. For questions on alcohol consumption, the AUDIT-10 score (Bohn et al., Reference Bohn, Babor and Kranzler1995) was used to assess alcohol-related risks, with scores less than 8 defined as low health risk, scores in the range 8–15 defined as increasing health risk and scores above 15 classified as high risk or dependent drinkers. The direct measurement of social capital is difficult, as pointed out by Stone (Reference Stone2001), and often relies on respondents reporting intensity of contact with friends and associations, and asking respondents to report on the human capital (education and economic status) and social status (reflected by nature of employment and positions of influence in society). Lin (Reference Lin2001) and Putman (Reference Putman1993) give details of how to assess social capital using this approach. This approach was not available in the questionnaire used as including these would have added greatly to the complexity of the questionnaire and could compromise ethics, especially in asking respondents to report on their friends and associates. To overcome this problem. social capital was assessed from their close relationship status (has a current partner: yes/no) and questions which can give proxies for social capital. In this study, respondents were asked their agreement with statements related to the respondent's perception of alcohol intake and wellbeing. The wellbeing questions were taken from the SF-12 questions. For example, a statement relating to alcohol is ‘People with alcohol problems should feel ashamed’ and a wellbeing statement was ‘I am proud of the community I live in and feel part of it’. The sociological theory and social network theory behind this is that attitudes and beliefs can be formed and reinforced by interaction or lack of interactions with others (Putman, Reference Putman1993; Scheufele and Shan, Reference Scheufele and Shan2000; Lin, Reference Lin2001). A list of the variables selected from the general survey for this study is presented in Table 1.
Table 1. Variables used

Since allocation of questions to the elements of social capital is open to question and we could not find a generally agreed measure, we applied exploratory factor analysis to form scores by correlating the responses to questions considered to be indicators of social capital and then assigned them to a social capital component. As the variables associated with social capital were nominal (yes/no answers) or ordinal (agree, don't know or disagree), exploratory factor analysis was undertaken by first computing a polychoric correlation matrix and then applying varimax rotation to derive orthogonal factors; this procedure is exemplified by Aletras et al. (Reference Aletras, Kostarelis, Tsitourido, Niakas and Nicolaou2010). This matrix construction and factor analysis were conducted in Stata 14.0 (De Bruin, Reference De Bruin2006). This generated two variables standardised to range from −3 to +3, with a mean of zero. In Table 1, ‘I have a partner’ is listed as a control variable in the studies, but as it is relational in nature, it was moved to a social capital measure and included in the factor analysis for the present study.
After obtaining these variables, independent t-tests were used on the factor scores to compare the social capital components between those categorised low alcohol risk and those high alcohol risk. Finally, we applied logistic regression to understand the significance of the social capital components on the likelihood of a respondent being low or high risk while controlling for age, sex, ongoing health problem, religion and level of formal education. To understand the relative effect of the variables, the model was developed sequentially by initially only including the social capital variables and then control variables were added one by one. Finally, interactions between the social capital variables and the control variables were examined. To assess significance of the coefficients in the model, a value of p of less than 5 per cent was taken as an indicator of statistical significance.
Results
Initially a three-level categorisation of the AUDIT-10 score, as advanced by Bohn et al. (Reference Bohn, Babor and Kranzler1995), was taken as the dependent variable, however, the distribution of this variable in our survey gave 79.5 per cent of respondents classified as low-risk drinkers (AUDIT-10 score <8), 17.85 per cent increasing risk drinkers (AUDIT-10 score 8–15) and 2.65 per cent high-risk drinkers (AUDIT-10 score >15). This would imply the need for multinominal logistic regression. However, although the high-risk and dependent drinkers are important as they require more support interventions and are likely to experience negative health-related consequences from alcohol, the relatively low numbers of this group are likely to result in unreliable estimates of regression coefficients for this group. Consequently, the increasing and high-risk and dependent risk drinkers were combined to form a group labelled ‘higher-risk drinkers’ for comparison with ‘low-risk drinkers’. A summary of the distribution of the variables selected are presented in Table 2.
Table 2. Summary of variables

Note: AUDIT-10: Alcohol Use Disorders Identification Test.
Control variables used were age which had a mean of 63.87 years (45.95% were older than 65 years), sex (50.42% were female), ethnicity (7.45% stated they were not white), health (38.58% stated that they had a long-term illness, disability or infirmity), degree or equivalent (38.21% stated they had a degree or equivalent) and religion (73.85% reported they identified with a religion). Due to the lack of diversity in the responses to the questions on sexual orientation and ethnicity, we excluded these variables.
To form the social capital variables, the responses to the statements chosen to reflect social capital shown in Table 2 were entered into polychoric exploratory factor analysis to derive scores to represent the social capital variables. The factor scores derived are displayed in Table 3. The factor scores accounted for 94.2 per cent of the original variation in the data and the Kaiser–Mayer–Olkin measure of sample adequacy was 0.729 suggesting, according to Hair et al. (Reference Hair, Anderson, Tatham and Black1998), that the factor analysis is acceptable in terms of reliability.
Table 3. Factor scores representing social capital components

Note: Factor scores less than 0.2 have been suppressed to facilitate interpretation.
We labelled the two factors generated as relational and cognitive capital, with relational capital associating with most of the variance in the data.
We assessed the significance of the differences in the means of the capital scores for the two groups of drinkers as identified by their AUDIT-10 scores. The results are exhibited in Table 4. Higher values of relational and cognitive capital are significantly associated with membership of the lower-risk group (p < 0.001).
Table 4. Independent t-test results

Notes: AUDIT-10: Alcohol Use Disorders Identification Test. SD: standard deviation.
We applied binary logistic regression modelling to understand the significance of the social capital components of predicting if someone was at higher risk from alcohol consumption, while controlling for age, sex, ongoing health problem and religion. The coefficients and odds ratios of the variables derived from the sequential development of the model are presented in Table 5. First, we present the social capital elements. In the next column we add the following control variables: sex (0 = male, 1 = female), age in years, and health status (0 = no long-term illness, disability or infirmity, 1 = have a long-term illness, disability or infirmity). In the next column religion is added, coded as 0 if the respondent stated they did not identify with a religion and 1 if they stated they identified with a religion. Finally, we add the variable called degree (coded 1 if they had a degree or equivalent or 0 otherwise). In the remaining column we present the interactions between sex and the social capital variables. Other interactions with the control variables and the social capital variables were explored but none were found significant nor to change the signs and significance of values. These are not reported in the table.
Table 5. Logistic regression models predicting the likelihood of being at higher risk of alcohol consumption
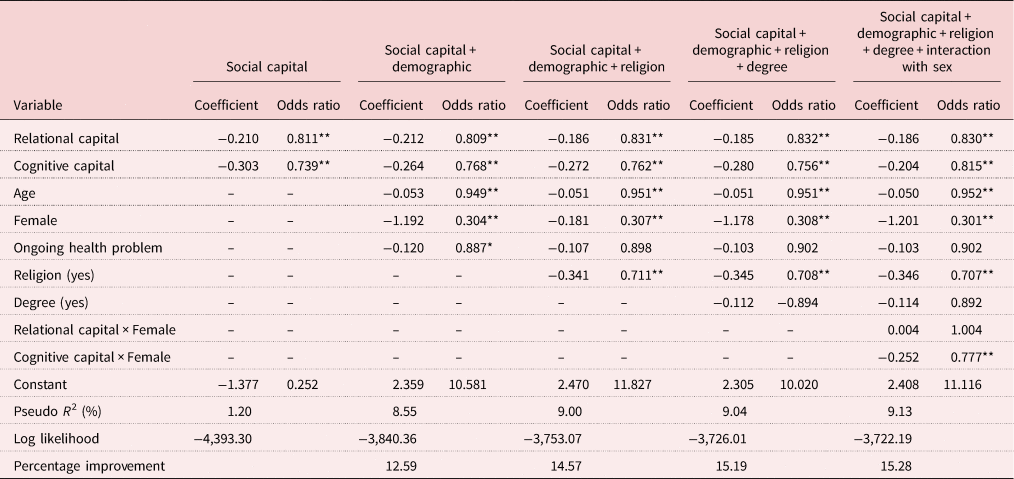
Significance levels: * Significant at the 5 per cent level, ** significant at the 1 per cent level.
Considering social capital components separately, an increase in relational or cognitive capital was associated with lower-risk drinking. When sex, age and health status are added, all appear as having a significant effect on the AUDIT-10 score, with being female, being older and having an ongoing health problem all being positively associated with a low risk of alcohol consumption. Again, relational and cognitive capital remain significantly associated with reducing the risk or higher risk. When religion is added, identifying with a religion is found to have a strong and significant association with lower risk. The other control variables (sex, age and health) for both the social capital components (relational and cognitive capital) remain significant in lowering the likelihood of being in the risk of being in the higher-risk group. Having a degree or equivalent was then added but was found only to have a small effect and was only significant at the 10 per cent level.
Interactions between the social capital variables and the control variables were considered but the only improvement to the model was when the interaction between social capital and sex of the respondent was considered. Being female had no significant effect when combined with relational capital but did have a significant effect at the 1 per cent level when combined with cognitive capital.
Discussion
Empirical evidence on associations between social capital components and alcohol risk among older adults is limited. To the best of our knowledge, this is the first study to examine associations between two types of social capital (relational and cognitive) and alcohol risk among adults aged over 50 which also considered the sex of the respondent. The results showed that higher levels of relational and cognitive capital have a statistically significant effect on alcohol risk, with higher levels of both being associated with lower-risk drinking. Of the two forms of social capital, cognitive capital has a marginally stronger association than relational capital, except when the interaction with sex (being female) is considered. Although not shown here, we ran the factor analysis based on the polychoric correlation matrix with those who never drank included and found that this group had higher levels of relational and cognitive social capital than the other groups.
Our findings provide new knowledge to the existing evidence base on social capital by demonstrating the significant effect of relational and cognitive capital on older adult drinkers. Being female had no significant effect when combined with relational capital but did have a significant effect when combined with cognitive capital.
Research conducted on the general population found that being female was associated with lower levels of drinking (Larm et al., Reference Larm, Åslund, Starrin and Nilsson2016). Other general population-based studies point to a negative effect of relational capital on women's drinking, including raised CAGE scores and binge drinking (Chuang and Chuang, Reference Chuang and Chuang2008; Murphy et al., Reference Murphy, Roberts, Kenward, De Stavola, Stickley and McKee2014; Seid, Reference Seid2016). Research has highlighted how women are more likely to be engaged in kin-based networks (Parks-Yancy et al., Reference Parks-Yancy, Di Tomaso and Post2006; O'Neill and Gidengil, Reference O'Neill and Gidengil2013), which, depending on their attitudes and behaviours around alcohol, can act as a barrier or an enabler to higher-risk drinking. Relational capital, such as close friends and family, can provide informal control to group members, promoting healthier lifestyles and attitudes around alcohol use. Alternatively, being socially connected through networks also has the potential to expose people to environments conducive to alcohol use. Indeed, social interactions have been reported as more strongly associated with risky alcohol use than structural factors such as education and employment, particularly when social groups approve of drinking (Shiovitz-Ezra and Litwin, Reference Shiovitz-Ezra and Litwin2012), with the effect even stronger for women (Seid, Reference Seid2016). It is to be noted that these studies reporting the negative impact of relational capital did not focus on older people. It is possible, as Villalonga-Olives and Kawachi (Reference Villalonga-Olives and Kawachi2017) suggest, that alcohol-related behaviours spread or are discouraged within social networks via the process of social contagion, with exposure to relational capital impacting people differently. This may explain why we observed a weaker association between relational capital, lower-risk drinking and being female. Overall, for older drinkers we found that the higher one's relational capital is, the lower the likelihood of higher-risk drinking.
The notion that cognitive and relational capital have a harm-reducing effect on alcohol risk is consistent with similar general population studies (Shiovitz-Ezra and Litwin, Reference Shiovitz-Ezra and Litwin2012; Larm et al., Reference Larm, Åslund, Starrin and Nilsson2016). However, a novel finding from our study is the interaction between sex and cognitive capital, indicating that older females have a significantly higher benefit from increased cognitive capital than do males.
Other harm-reducing factors which have been used as control variables in our study are consistent with existing research: being older, having an ongoing health problem, identifying with a religion and, although marginal, receiving higher education (Hajat et al., Reference Hajat, Haines, Bulpitt and Fletcher2004; Kim et al., Reference Kim, Spilman, Liao, Sacco and Moore2008; Murphy et al., Reference Murphy, Roberts, Kenward, De Stavola, Stickley and McKee2014).
Social networks developed through the lifecourse reduce as people reach retirement while the extent of social capital also deteriorates as a result of retiring from work and networks relating to work, and perceptions of reduced health. Previous research has reported that changes in life circumstances limit alcohol intake among people over 55 (Ward et al., Reference Ward, Barnes and Gahagan2011; Borok et al., Reference Borok, Galier, Dinolfo, Welgreen, Hoffing, Davis, Ramirez, Liao, Tan, Karno, Sacco, Lin and Moore2013). Our study also supports the evidence elsewhere of an age-related decline in alcohol consumption among both men and women (Burton et al., Reference Burton, Henn, Lavoie, O'Connor, Perkins, Sweeney, Greaves, Ferguson, Beynon, Belloni, Musto, Marsden, Sheron and Wolff2016; National Health Service, 2017; Office for National Statistics, 2019). It can be argued that decreased mobility as people age, combined with increased medication intake, reduces the opportunities for social participation, which in turn limits alcohol intake among this age group.
Implications for policy and practice
A key question is how policy makers and practitioners might utilise our findings? Information about how social capital can impact on older adults' drinking may guide interventions aimed at reducing drinking in later life. Policy directives such as ‘successful ageing’ have been commissioned by the European Union on the assumption that social capital is good for health (Leone and Hessel, Reference Leone and Hessel2016). Social network-based interventions have been reported as effective in changing health behaviours and experimental research has shown that by influencing social networks, lifestyles can be promoted (Po'e et al., Reference Po'e, Heerman, Mistry and Barkin2013; Young and Jaganath, Reference Young and Jaganath2013; Gesell et al., Reference Gesell, Barkin, Sommer, Thompson and Valente2016). Promoting positive social networks and positive mindsets may be a promising approach to reducing alcohol risk, but care needs to be taken on connecting people to networks which promote refraining from alcohol consumption. Such interventions have been found to be effective in other areas of public health. One example is Harnessing Online Prevention Education, which was aimed at preventing HIV among men who have sex with men (MSM), by engaging the MSM community in online debates and conversations around HIV prevention (Young and Jaganath, Reference Young and Jaganath2013). The Growing Right Onto Wellness (GROW) trial is another example (Po'e et al., Reference Po'e, Heerman, Mistry and Barkin2013; Gesell et al., Reference Gesell, Barkin, Sommer, Thompson and Valente2016). This involves the promotion of healthier lifestyles through the formation of new social groups and social norms to encourage beneficial behavioural change. The authors concluded from preliminary results that network ties and a sense of cohesion are important mediators for change, recommending the inclusion of network building in health-related interventions (Gesell et al., Reference Gesell, Barkin, Sommer, Thompson and Valente2016). This could also be applied in the context of older drinkers, and particularly those where networks are associated with risky health behaviours. A relevant example from the UK is the Drink Wise Age Well initiative in which the use of existing networks such as arts, sports or interest groups are used to promote activities that do not focus on drinking and, where these do not exist, provide the resources to develop these network groups (Holley-Moore and Beach, Reference Holley-Moore and Beach2016). A key aim of Drink Wise Age Well is to develop resilience thus preventing harmful drinking among older people.
Alternatively, recovery-focused initiatives may be more suited to those who already engage in harmful drinking and have lower levels of capital. The aim is to develop more-extensive support networks that may help people form positive social identities (Mercer et al., Reference Mercer, Crocetti, Branje, Van Lier and Meeus2017). Here, the emphasis is also on peer rather than professional support, whereby recovery is co-produced through social interaction, social norms and social influences. Self-help groups seek to do this by allowing a transition into new recovery-oriented networks. Referrals into these groups could be from self, alcohol services or through social prescribing from primary care (Drug and Alcohol Findings, 2017). An example of how this kind of initiative would work with older adults is the Long Live the Elderly programme reported by Liotta et al. (Reference Liotta, Inzerilli, Palombi, Madaro, Orlando, Scarcella, Betti and Marazzi2018). The programme is aimed at strengthening social ties and community relations with those over 75 years and initial evaluations of the impact of the programme have been positive (Liotta et al., Reference Liotta, Inzerilli, Palombi, Madaro, Orlando, Scarcella, Betti and Marazzi2018). The authors of the study concluded that community-based programmes which aim to strengthen social capital among older adults should be promoted in any health intervention (Liotta et al., Reference Liotta, Inzerilli, Palombi, Madaro, Orlando, Scarcella, Betti and Marazzi2018). Drink Wise Age Well adopted this approach for older drinkers by creating self-help recovery groups which were led by volunteers who had lived experience of harmful alcohol use. The aim of this national demonstration project was to benefit both the members of the group and the group leads (Holley-Moore and Beach, Reference Holley-Moore and Beach2016).
The finding that females benefit more from higher levels of cognitive capital than men suggests a role for education and a publicity campaign to increase knowledge on alcohol risk in the general population and give extra attention to direct these messages towards men. These campaigns are expensive and beyond the budget of any community-based organisation. Thus, government action is required to design, implement and fund these campaigns.
We also think that further research is required to assess the feasibility of introducing these interventions to older drinkers and community-based services. To echo Wilkinson and Dare (Reference Wilkinson and Dare2014), this will need to be multi-disciplinary, participative and qualitative in nature to give understanding of what interventions will help to build older people's social engagement and reduce isolation, shame and stigma about reporting alcohol-drinking levels which make older drinkers an ‘invisible population’, (Alpert, Reference Alpert2014) and reluctant to seek help. The differential experiences and perspectives between men and women also need to be considered.
Strengths, limitations and implications for research
The key contribution of this research is the beneficial effect of social capital in reducing alcohol risks among older people and we believe the findings add to existing research. Furthermore, we sampled from a wide range of geographical and socio-economic areas across the UK, which strengthened the results. We also targeted GPs as gatekeepers, which facilitated access to a community-wide sample of people over 50. However, we experienced a 22 per cent response rate which is lower than that reported in other community-wide samples of albeit telephone-based research (50%) (Zhao et al., Reference Zhao, Stockwell and Macdonald2009). We compared the AUDIT-10 scores for our sample with those of a similar age from the Adult Psychiatric Morbidity Survey (APMS) (McManus et al., Reference McManus, Bebbington, Jenkins, Morgan, Brown, Collinson and Brugha2020) for England in 2014 (57% response rate). Approximately 80 per cent of our sample were classified as lower risk (AUDIT-10 score <8) which is similar to the 79 per cent in the APMS. Approximately 20 per cent in our survey were classified as higher risk (AUDIT-10 score ≥8) which is close to the 21 per cent in the APMS. A limitation of our study is that the findings are derived from a quantitative cross-sectional survey and thus causal pathways cannot be determined.
The study data were also derived from self-report questionnaires, which cannot guarantee accurate reports of alcohol risks. Self-reported surveys on alcohol consumption can suffer from impression bias (where the respondent wishes to present themselves in a good light) and self-deception (respondents not realising how much they drink) (Davis et al., Reference Davis, Thake and Vilhena2010). Both these measures lead to underreporting of consumption and Davis et al. (Reference Davis, Thake and Vilhena2010) found women were more likely to be associated with impression bias. Social stigma (Bradley et al., Reference Bradley, Boyd-Wickizer, Powell and Burman1998) associated with older women drinking might well reinforce the impression bias. Knibbe and Bloomfield (Reference Knibbe and Bloomfield2001) also draw attention to gender differences in reporting alcohol use, with women more likely to underreport. Perhaps more reliable self-reporting can occur if an IT platform in which a person's anonymity is assured is used to collect sensitive data of a stigmatised nature. Mitchell et al. (Reference Mitchell, Schwartz, Alvanzo, Weisman, Kyle, Turrigiano, Gibson, Perez, McClure, Clingerman and Froias2015) reported that such data collection systems were accepted by staff and service users in drug treatment interventions.
A further limitation is that the conceptualisation of relational and cognitive capital is imperfect, and work is needed to form agreed and accepted measures of these variables. Some of the variables are measured rather bluntly, notably religion; simply asking what religion the person identifies with does not convey the intensity of belief nor the degree of interaction with others of that religion, and perhaps it would be better to use the gender a person identifies with rather than sex. Similarly, ethnicity failed to give diverse information and the nationality someone considered themselves was not available. Also missing are variables to control for the respondent's history of drinking, financial status and location of residence.
As far as we know, there are no comprehensive measures of social capital for older people including, of course, those who consume alcohol. We think greater attention is required to better understand what those with lived experience of both understand by social capital and how these meanings change over time. This calls for more qualitative research and would contribute to the formulation of quantitative variables that enhance survey instruments for use in large population-based observational surveys. It may also help in the assessment of interventions designed to improve the social capital of older drinkers.
Conclusions
We have contributed to the evidence base on social capital by providing empirical analysis of relative impacts of relational and cognitive capital and on alcohol risks among men and women over 50. Results indicate that people will benefit from engagement in social networks which give access to relational and cognitive capital but, ultimately, there are no assurances that changes in social capital will bring about change in alcohol-related risks. Therefore, future research should consider evaluating the impact of social network interventions for older drinkers and how these might affect men and women. This research should include a qualitative component which seeks to understand why women and men may be affected differently. This research should be guided by social capital and social network theory.
Financial support
This work was supported by the Big Lottery Fund.
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
Ethical approval for this study was granted by the National Health Service Research Ethics Committee UK (reference 15/EM/0098).







