LEARNING OBJECTIVES
After reading this article you will be able to:
• understand the challenges with regard to the diagnosis and conceptualisation of the schizophrenia syndrome
• describe developments in the psychopathology of schizophrenia at the level of both the brain and the mind
• understand the importance of integrating neuroscientific approaches into clinical formulations of the schizophrenia syndrome.
This article aims to introduce the mental health clinician to some of the major developments in the field of the psychopathology of schizophrenia. These developments are ready to be incorporated into clinical practice. Although it is beyond the scope of the article to comprehensively review all advances in the understanding of schizophrenia psychopathology, we aim to demonstrate that psychiatry now has sufficient evidence to begin to change its terminology and mindset to reflect brain and mind process rather than symptoms alone.
‘Cause’ in the context of mental illness is often used to describe factors that can be characterised as triggers or vulnerability (which interact to lead to abnormal experiences). In this article, however, cause refers to a process-based entity that provides a link between trigger/vulnerability factors and the patient's experiences. For instance, an individual with asthma is liable to suffer an asthma attack, which is experienced as difficulty breathing. An account might describe factors ‘causing’ the asthma as an atopic genetic vulnerability and a trigger such as air pollution. However, the causal process is the mast and basophil cell degranulation that induces bronchospasm. In the case of schizophrenia, we have hitherto often focused our concern with cause on vulnerability and trigger factors (e.g. stress, cannabis and an inherited vulnerability). However, recent advances in mental health research allow clinicians to think about an explanatory process-based mechanism in the way the physician does for asthma. It is process in this sense that needs to be at the centre of our formulations and explanations of psychopathology.
Schizophrenia: history, nosology, neuroscience and current conceptual challenges
Contemporary notions of schizophrenia and their historical context
Although psychosis spectrum symptoms present in multiple diagnostic syndromes, we are attending here to the schizophrenia spectrum syndrome only. Schizophrenia is typified by an apparent fundamental breakdown in reality-testing (psychosis). Notwithstanding differences between the diagnostic symptom lists, most notions of schizophrenia incorporate a common set of experiences that includes perceptions in the absence of an external correlate (hallucinations) and fixed false beliefs (delusions). Its present-day conceptualisation is often traced back to the mid-19th century, and most notably to the influential Kraepelinian paradigm – the notion that schizophrenia is a brain-based condition with a pathognomonic trajectory. Bleuler, on the other hand (who was influenced by psychoanalytic thinking), emphasised the process of loosening of associations of psychic functions (Semple Reference Semple and Smyth2013).
The evolution from these earlier constructs to the current notion of schizophrenia has not been informed by a process of validation whereby the symptomatic description has been refined to better identify a recognised and identifiable underlying entity. Schneider made efforts to operationalise the diagnosis of schizophrenia by describing symptoms of first rank, which he thought should only occur in schizophrenia, and symptoms of second rank, which might also occur in other psychoses (Semple Reference Semple and Smyth2013). Later on, in the second half of the 20th century, psychosis psychopathology underwent a manualisation process with important attempts to improve reliability – the work of Robert Spitzer leading to the publication of DSM-III in 1980 being a prime example (Liebermann Reference Liebermann2015). While these efforts may have indeed improved reliability of diagnosis, the validity of diagnosis in terms of it being an accurate reflection of mental experiences and an accurate representation of brain and mind processes has improved very little.
Challenges relating to nosology and current conceptualisations of schizophrenia
The process of improving diagnostic reliability via a ‘manualisation’ process involving diagnostic rules (ICD and DSM) has come at a cost. Not only has it attracted the criticism that psychiatry has, on occasion, been reduced to a brief symptom checklist approach (Andreasen Reference Andreasen2006); it has also resulted in an emphasis (without empirical justification) on certain types of experience at the expense of others.
The assumption that there is something fundamentally pathological about the experience of hearing a voice without a corresponding auditory stimulus can lead to relative neglect of other anomalous experiences that do not meet the symptomatic definitions in ICD and DSM. Similarly, clinicians may adopt a ProcrusteanFootnote a approach of adapting a patient's experience to fit an existing psychopathological framework of limited empirical provenance. To take the example of voice-hearing phenomena, the diagnostic manuals tend to elevate those experiences that fit the description of hallucinations as worthy of clinical interest, but discourage the clinician from investing effort in understanding related experiences – unless it is to demonstrate that they are in fact not hallucinations.
In medicine it is often necessary to apply ‘cut-offs’ to dimensional expressions of pathology (e.g. in deciding when elevated blood pressure becomes clinically significant hypertension). The difference in psychiatry is that there is no clear rational for the boundaries applied to the definition of psychotic psychopathology such as hallucinations. Indeed, over-investment in the legitimacy of the boundary may interfere with understanding the patient's experience, which may in turn be experienced by the patient as invalidating. (We wish to point out that we are certainly not ‘anti-psychiatry’ or indeed ‘anti-diagnosis’, but support evidence-based change in practice to align our specialty closer to neuroscientific research.)
The current psychopathological framework is unlikely to reflect the underlying brain and mind pathology it aims to represent. When a patient is asked whether they are experiencing voice-hearing phenomena, they are often uncertain whether what they are experiencing is an auditory phenomenon, or a thought phenomenon or something in between. It might be that there are ‘spectra’ of experiences with varying degrees of agency and ownership, with ‘silent and internal own thoughts’ at one extreme and ‘fully external and clearly audible voices’ in the absence of a speaker at the other (Humpston Reference Humpston and Broome2016).
The boundary between perception and belief, and as such, hallucination and delusion, may not be as clear cut as we once thought (Fletcher Reference Fletcher and Frith2009). If a person experiences their arm movement as being controlled by an external agent, it can be unclear whether this is a somatosensory experience akin to a hallucination or whether it is primarily a belief. Indeed, it may be both at the same time, or may in fact fall into neither category. The experiential status of passivity symptoms can often shift and merge between what is usually conceived as a hallucinatory sensation and what is a delusion of control. The format of the standard mental state examination (MSE) has remained the same for many decades, but developments in phenomenology and the neurosciences are showing us that a revised and updated MSE is required. For example, we could shift from distinct categories of thought process and thought content to a broader category covering subjective alterations in the patient's experience of self and world. This could involve greater appreciation of subtle changes that are not captured by the current MSE. Furthermore, the hard boundary between traditional categories of thought content and perception may also need to be softened.
The neurobiology of schizophrenia: current evidence for brain dysfunction
Schizophrenia can be approached through a mind- or brain-based frame of reference. The adoption of a mind-based perspective encouraged by phenomenology should not be taken to diminish the importance of the brain-based biological view of schizophrenia. When symptoms of psychosis are triggered, the biology of the brain has an impact on the psychology of the mind and vice versa. One's perspective regarding the relative weighting of these components will be guided by which level of analysis is focused on, from the genetic, to the molecular, to the process level in the brain, to a subjective mind-based phenomenological expression (Humpston Reference Humpston2017: p. 180).
Evidence of a biological basis for schizophrenia is summed up succinctly by Fletcher & Frith (Fletcher Reference Fletcher and Frith2009). From a genetic point of view, liability to schizophrenia is highly heritable (approximately 0.81) and concordance between identical twins is almost 50%. Approximately 150 genes have been robustly linked with an increased risk for the disorder (Pardiñas Reference Pardiñas, Holmans and Pocklington2018). Neuropathologically, imaging studies reveal enlarged ventricles and reduced cortical volume – especially in the medial temporal lobe. Finally, to date, all drugs with antipsychotic properties block dopamine D2-like receptors; and exposure to amphetamine (a dopamine agonist) can result in schizophrenia-like symptoms (Fletcher Reference Fletcher and Frith2009).
Understanding of the schizophrenia syndrome has advanced sufficiently that we are now able to shift our clinical thinking from symptoms to brain and mind processes. Importantly, this should be accompanied by the clinician devoting more attention to a patient's subjective experience rather than less (as is often feared might be the case with this sort of approach).
Recent developments in schizophrenia psychopathology
Expanding the scope of the clinician's interest in patients’ subjectivity
Adopting a broader approach to assessment that does not constrain the assessor (in the way the conventional MSE does) has been explored in both clinical and research settings. The at-risk mental state concept and Comprehensive Assessment of At-Risk Mental States (CAARMS; Yung Reference Yung, Yuen and McGorry2005) are widely used by early intervention in psychosis teams and they provide a wider field of view than diagnostic manuals. As they are commonly used in UK clinical practice, and may well be known to our readers, we will focus on other developments here.
Basic symptoms and the BSABS
Subtle disturbances of experience hypothesised to be the proximal manifestations of neurobiological processes have been labelled ‘basic symptoms’ (Schultze-Lutter Reference Schultze-Lutter and Theodoridou2017). They comprise complaints that have been seen as subclinical in the areas of volition, affect, thinking and language (speech), (body) perception, memory, motor action, central vegetative functions, control of automatic cognitive processes, and stress tolerance. Examples include an interference of clear thinking due to the intrusion of objectively trivial thoughts, difficulties distinguishing between perceptions and ideas, and a sense of disconnectedness from one's surroundings (Schultze-Lutter Reference Schultze-Lutter2009). Experiences are grouped into three levels, which are potentially reversible and may demonstrate the existence of a continuum at a psychopathological level. Thus, a particular somatic hallucination (level 3) could revert to a cenesthetic feeling (level 2) and this, in turn, to a non-specific somatic feeling (level 1).
This conceptualisation of experience has been manualised in the Bonn Scale for the Assessment of Basic Symptoms (BSABS; Gross Reference Gross, Huber and Klosterkotter2008), which is a standardised procedure for inquiry into psychopathological and phenomenological data and has coverage of schizophrenia, schizotypal and delusional disorders as well as mood disorders.
Examples of experiences that fall outside the traditional diagnostically focused assessment include hypersensitivity to sound (which may be mistaken for a delusion regarding special powers of hearing), metachromopsia (a change in the perception of colour intensity), dysmegalopsia (objects being perceived in a distorted way) and disturbances of proprioception (i.e. cenesthesias).
Disturbance of ipseity and the EASE
Another approach to the assessment of subjective psychosis spectrum experiences has been based on an explanatory model of psychosis that emphasises a core disturbance of self-awareness (ipseity). The Examination of Anomalous Self Experience (EASE) (Parnas Reference Parnas, Møller and Kircher2005) lists an extensive array of anomalous experiences within the domain self-awareness and provides descriptions and prototypical examples. The EASE refers to ‘spatialization of experience’ – a scenario in which thoughts and experiences might be ‘localized to a particular part of the head or brain’. This struck a chord with us, because we had recent recollections of a patient reporting thoughts not of his agency ‘moving in a circle round my head’, while the thoughts he identified as belonging to him were experienced ‘at the back of my head’. Another such example from the EASE is a description of the situation when a patient ‘may become excessively intrigued or pre-occupied by semantic issues’. This can result in curiosity, amazement and intense reflection on everyday events and goings on. We had also previously observed ‘mirror-related phenomena’ on the wards (also referred to in the EASE) – where patients look in the mirror intensely to observe facial change. Other experiences within the EASE which resonated with us relate to a ‘feeling of centrality’, as if being at the centre of the universe, and ‘existential’ change, with themes relating to philosophy, the supernatural and psychology. As a final illustration relating to the EASE, we found reference to ‘cenesthetic experiences’ enlightening. Here, a patient may experience unusual bodily experiences – one that we have often heard in clinical interviews concerns vibrations moving through the body and head.
Anomalous experience of the world and the EAWE
An alternative assessment approach, the Examination of Anomalous World Experience (EAWE) (Sass Reference Sass, Pienkos and Skodlar2017) provides a very fine-grained list of subjective disturbances grouped into six domains: (a) space and objects; (b) time and events; (c) other persons; (d) language; (e) atmosphere; and (f) existential orientation. The EAWE is similar to the EASE in that it aims to elicit description of a person's subjective experience; but it focuses on the lived world, rather than focusing on the self as in the EASE.
The reach of the EAWE beyond conventional clinical approaches to the assessment of psychosis is illustrated by the exploration of the patient's experience of colour and image intensity, of time (e.g. movements being slowed down or speeded up) and of ‘difficulties with the gaze’ (e.g. feeling exposed through their own eyes or even feeling that their own gaze is penetrating for others).
Summary
Despite their breadth of concern, the BSABS, EASE and EAWE (summarised in Box 1) still leave phenomenological gaps between the experiences they list, and these tools do not fully address the criticism of the checklist approach to psychiatric assessment. Nevertheless, although we are not suggesting their routine use in clinical practice, by studying these tools clinicians interested in adopting a phenomenological approach are likely to benefit from a familiarity with the types of experience that occur alongside the apparently typical ones of hallucinations and delusions. Of further relevance to the clinician is the style of assessment encouraged by these assessment tools. All three instruments promote a style of open and exploratory conversation rather than a more formal interview. Not only does this facilitate a discussion about the full extent of the patient's experiences, but it is also likely to avoid the potentially invalidating effect of discarding much of the patient's subjectivity in their search for narrow psychopathological objects that have been afforded greater (possibly unmerited) status through the current approach to psychopathology and diagnosis.
BOX 1 Tools assessing subjective experience in psychosis: the BSABS, EASE and EAWE
The Bonn Scale for the Assessment of Basic Symptoms (BSABS) (Gross Reference Gross, Huber and Klosterkotter2008): a semi-structured interview for inquiry into psychopathological and phenomenological data in relation to schizophrenia, schizotypal and delusional disorders as well as mood disorders.
Examination of Anomalous Self Experience (EASE) (Parnas Reference Parnas, Møller and Kircher2005): a symptom checklist for semi-structured exploration of experiential or subjective disturbances of self-awareness (ipseity).
Examination of Anomalous World Experience (EAWE) (Sass Reference Sass, Pienkos and Skodlar2017): a semi-structured interview to explore the individual's subjective experiences of the world (rather than the self). The EAWE is primarily directed towards experiences thought to be common in schizophrenia spectrum conditions.
A more refined picture of the differences between different patients’ experience is also likely to lead to greater understanding of the heterogeneity that is recognised to be present in psychotic syndromes such as schizophrenia. If it is accepted that the specific nature of a subjective experience is the product of an underlying mental process, then it follows that the more we appreciate the detail of that experience, the greater our chances of identifying those brain and mind processes that are the key causal entities.
Mind-based process models
At the outset we wish to make clear that the subdivision of mind- and cognitive-based process models is for explanatory purposes only and that these are not mutually exclusive, as there is a theoretical and evidence-based overlap. Also, it is not possible, owing to the requirement of brevity, to cover all mind and cognitive process models here and we have therefore selected only a small number (summarised in Box 2) to draw attention to.
BOX 2 Mind based models of self disturbance:
• the ipseity model: schizophrenia is in part a disorder of the self or self-awareness – a disorder of ipseity
• the perceptual anomalies model: automatic unconscious processes lead to the self acting as a non-participatory bystander
Cognitive process-based models
Differences in attention, perception and action:
• aberrant salience: an attenuation of the process of filtering out the mundane
• reality-monitoring deficit (internal–external source-monitoring deficit): impaired ability to distinguish internally generated experiences from those generated by the outside world
Models of self-disturbance
One formulation of a mind-based process disturbance is that schizophrenia is in part a disorder of the self or self-awareness – a disorder of ipseity (Sass Reference Sass and Parnas2003). Broadly speaking, this involves two principal concepts – hyper-reflexivity and diminished self-affection – and a third related concept involving a disturbed ‘grip’ or ‘hold’, which pertains to the so-called ‘commonsensical’ world. Hyper-reflexivity involves an exaggerated self-consciousness and an inward-facing focus of immense introspection. The notion of diminished self-affection describes a reduction in the experience of being-in-the-world as a subject (Humpston Reference Humpston and Broome2020). The third component – ‘grip’ – which has received somewhat less research focus, relates disturbances in the self to those of the world. The external environment feels alien and threatening to the patient, yet at the same time the world is full of intangible meaning and perplexity. In combination, these concepts highlight the paradoxical nature of subjectivity in schizophrenia. In this paradigm the self is never able to fully detach from subjectivity, but neither is it able to fully participate in mental processes – it is stuck in an ‘in-between’ state that is not sustainable. The theory suggests that to resolve this state an urgent explanation is called for, mostly in the form of a delusional elaboration.
Many clinicians will have had experience of their patients intensely examining their own thoughts and mind as they seek to reassert a sense of control. There can even be a sense that patients are philosophising, as their own mind, and thus the world, appear unfamiliar. As the introspective process develops, thoughts become increasingly alien and detached from the self. This may be the crucial step by which the pathology of self-disturbance subsequently generates florid psychotic experiences such as thought insertion and auditory verbal hallucinations.
Another often neglected model of self-disturbance comes from accounts by the early Heidelberg school of psychiatrists. In contrast with the ipseity model, this ‘perceptual anomalies’ approach focuses on implicit and unconscious processing rather than conscious self-acquaintance or introspection. Here, it is the automatic processes that lead to the self acting as a non-participatory bystander who is unable to fully detach from certain experiences. It is theorised that these experiences might drive the self away from volitional control and towards passivity (Kaminski Reference Kaminski, Sterzer and Mishara2019).
Cognitive process-based models
Although much vital empirical work has been done to demonstrate cognitive differences in schizophrenia (Bora Reference Bora, Yucel and Pantelis2009), the notion first arose through detailed clinical interviews. Differences in attention, perception and action were identified over 60 years ago (McGhie Reference McGhie and Chapman1961) but have not yet been incorporated into diagnostic criteria.
Aberrant salience
Delusional mood or atmosphere is a recognised prodromal feature of schizophrenia. It has been defined as the ‘first subjective phenomenological experience of something radically new, or alien’ (Mishara Reference Mishara and Fusar-Poli2013). The process of aberrant salience has been identified as critical in explaining delusional mood. This dysfunctional process arises owing to a variation in the way we ordinarily manage a potentially overwhelming volume of stimuli with which we are faced. For example, only one hundred millionth of incoming raw visual data is used to guide behaviour (Pitkow Reference Pitkow, Mesiter, Gazzaniga and Mangun2014). Within about a tenth of a second the remainder is sifted out. By automatically ignoring the routine and over-familiar, normal functioning can continue. Attention is activated in response to stimuli that are new, unexpected or threatening. If the process of filtering out the mundane is attenuated, then there is a general sense of inexplicable significance, which has been described as delusional mood. Identifying a process underpinning this – aberrant salience – introduces the notion of cause in a way that is more proximal to the experience (or symptom) than the conventional psychiatric causal factor (e.g. predisposing risk factors).
Dopamine has a vital role in attributing salience to stimuli, and dopaminergic dysfunction may involve both reward and aversive signalling (Bromberg-Martin Reference Bromberg-Martin, Matsumoto and Hikosaka2010), which could lead to the world seeming ‘pregnant with significance’ (Howes Reference Howes and Nour2016). Jaspers referred to this as the delusional atmosphere in which ‘there is some change which envelops everything with a subtle, pervasive and strangely uncertain light’ (Jaspers Reference Jaspers, Hoenig and Hamilton1913).
Staying with existing terminology for the time being, however, it is easy to forget that when a patient presents with either a delusional mood or fully fledged delusions, this is an abnormality in their information processing ability that may affect other decisions and behaviour. Indeed, some experiments suggest that patients with delusions demonstrate what is termed ‘jumping to conclusions’ (JTC) bias. Here, a study found that participants displaying delusional psychopathology reach their conclusion on the basis of less evidence than control participants (Henquet Reference Henquet, van Os and Pries2020). Other recent research suggests that the JTC reasoning bias in psychosis might not be a specific cognitive deficit but rather a manifestation, or consequence, of general cognitive impairment (Tripoli Reference Tripoli, Quattrone and Ferraro2020). This notion of patients with a delusional thought process having other more widespread abnormalities in information processing and decision-making is important because a patient's cognitive deficits may be more pervasive than their delusion(s). This may have an impact on their cognitive processing of the discussions in ward round, and their decision-making as regards taking medication (or not) or remaining on the ward (or not) may be similarly affected.
Use of a process term such as aberrant salience, which links the presentation of the illness with the neurochemistry, pushes us clinicians towards a better understanding of our patients. Accounts that link levels of explanation from the neurochemical to the cognitive to the phenomenological demystify the frightening nature of psychotic illness for patients and their carers (Fletcher Reference Fletcher2017). Furthermore, a more secure neurobiological understanding may enhance the patient–doctor therapeutic relationship and promote psychotherapeutic approaches rather than diminish them (Bullmore Reference Bullmore, Fletcher and Jones2009). Thus, as a small first step, when a patient sees coincidence and connection where there is none, we need to start writing ‘aberrant salience’ in the case notes.
Reality-monitoring deficits
The term ‘reality-monitoring deficit’, or internal–external source-monitoring deficit (Johnson Reference Johnson, Hashtroudi and Lindsay1993), describes a difficulty in being able to distinguish internally generated experiences from those generated by the outside world. It is the process underpinning phenomena such as auditory hallucinations and passivity experiences of motor control. Reality-monitoring ability in healthy individuals is associated with activity in the medial anterior prefrontal cortex as well as with the structural morphology of the paracingulate sulcus (Garrison Reference Garrison, Moseley and Alderson-Day2017). People with schizophrenia show impairments in reality-monitoring ability that are associated with dysfunction in the same areas (Garrison Reference Garrison, Moseley and Alderson-Day2017).
We are not alarmed by our internal thoughts or internal voice because we recognise them as coming from our own mind. However, if I were to develop a reality-monitoring deficit and mistakenly confuse internal and external stimuli, I might be alarmed that a voice in my head which did not seem to be mine knew my most private thoughts. Furthermore, if it did not ‘feel’ like my own internal speech – how did it get there? Did someone ‘insert’ these thoughts and voices into my head? And what if I logically assumed that, because the voice does not belong to me, it is coming from outside my mind and I ‘respond’ as is the customary thing to do. In a similar vein, if a patient's experience of the sensory consequences of their own actions is not attenuated, then when they make an active movement, it would feel like a passive movement that someone else had controlled. This relates to the ‘comparator model’ of motor action: signals that are copies of motor commands (corollary discharge) are used to predict the consequences of motor action (e.g. a sensation) such that the predicted and experienced sensations can be compared. If these two signals match, then the sensory consequences are attenuated and the action is regarded as self-generated (Poletti Reference Poletti, Gebhardt and Raballo2017). If not, and my mind and brain were generating signals that my bodily actions were not under my control, it would be a logical next step if I were to assume that someone or something else was controlling them.
Support for the notion that auditory hallucinations might arise from the misperception of inner speech is that they are associated with activity in areas related to speech, including the auditory cortex. It is suggested that disruptions in the connectivity of the brain might lead to inefficient motor–sensory communication, a failure in prediction-based attenuation (see below) and, ultimately, difficulties in distinguishing internally from externally generated stimuli (Fletcher Reference Fletcher and Frith2009).
Computational models and predictive processing – linking the brain with the mind
There is thus a new phenomenology that affords us a wider and richer understanding of our patients’ experiences and subjectivity. There has also been the development of an understanding of causal process mechanisms in the separate but connected realms of the brain and mind. But how to link these developments with the neurochemistry – in particular dopamine and glutamate – is another challenge. The notion of ‘predictive processing’ may well provide a framework to link these different (yet equally valid) levels of analysis via computational processes (Sterzer Reference Sterzer, Adams and Fletcher2018). Psychiatry and psychology are broad and varied disciplines that have for too long been constrained by turf wars that somewhat miss the point. The predictive processing framework is a useful paradigm serving to link the biological with the psychological, the brain with the mind, via connecting differing levels of analysis.
It is underpinned by Bayes’ theorem: that is, the idea that incoming information is interpreted in the light of our prior expectations and beliefs (Corlett Reference Corlett, Frith and Fletcher2009). This is illustrated by the notion of illusions and Mooney images (distorted or inverted images that usually consist of faces in black and white with low resolution). With illusions, there is a deliberately manufactured deviation between prediction and actuality, such that the perception that emerges more strongly reflects what the observer predicts rather than what the raw sense data actually represent. Conversely, phenomena such as Mooney images are difficult to see and may appear ambiguous, but become clear if a person is equipped with the correct prior information that allows them to predict the contents of the image.
Predictive processing – a step-by-step guide
The brain needs to uncover the associative and causal structure of the world but is reliant on noisy and ambiguous sensory information as its guide. It cannot deal with this problem adequately by relying on its inputs and so must make use of prediction-based prior knowledge.
The brain is therefore engaged in the process of predictive inference: incoming information is interpreted in the light of our prior expectations and beliefs (Bayes’ theorem). We infer the probability that the cause for an experience or event is correct (or not) given the sensory evidence we are presented with.
• If sensory data do not fit the current model and are unexpected (i.e. there is a discrepancy between the expected experience and the actual experience) this will generate a so-called ‘prediction error’. A key signal in this computation relates to the brain's unsuccessful predictions. When there is a mismatch between the expected and actual signal (i.e. a prediction error) this must be dealt with. A central function of the brain therefore is to minimise surprise. It strives for a model of the world that is as accurate as possible, so that expectations fit with incoming sensory data: the old adage – ‘You see what you expect and expect what you see’.
• The brain will update its model of the world on the basis of incoming sensory data that does not match the current model and of expectations intrinsic to the current model.
• The prediction error may be resolved at a lower processing level, but if this cannot be achieved it will be propagated to a higher level for resolution.
• Sometimes the balance of this prediction system can go awry and result in faulty inferences, leading to false beliefs and false perceptions.
Beliefs and percepts emerge from the interaction of bottom-up and top-down processes (Corlett Reference Corlett, Frith and Fletcher2009) (Fig. 1). Bottom-up often refers to a signal that comes from sensory information (from peripheral to central). Top-down can refer to signals that are driven by cognition and prediction (from central to peripheral). Perception itself emerges as a consequence of the integration of these two signals (i.e., in Bayesian terms, it is the posterior). That said, it is useful to acknowledge that not all predictions are top-down (Teufel Reference Teufel and Fletcher2020).
• Increased weighting towards bottom-up signalling can lead to the construction of a delusional belief (especially if there is a weakened top-down prior) (Corlett Reference Corlett, Frith and Fletcher2009). Consider the concept of delusional mood referred to above. The kind of uncanny experience involved calls for the model to be updated. Here, delusion formation may act as a means of explaining away the strange experience and thus minimising surprise. However, if the sensory experience continues to be present, the precision weighting might shift to the top-down prior, which becomes more resistant to updating over time and results in maintenance of the delusion. That is, imbalance of processing in favour of top-down signalling can lead to hallucinations and the maintenance of delusional beliefs (Corlett Reference Corlett, Frith and Fletcher2009).
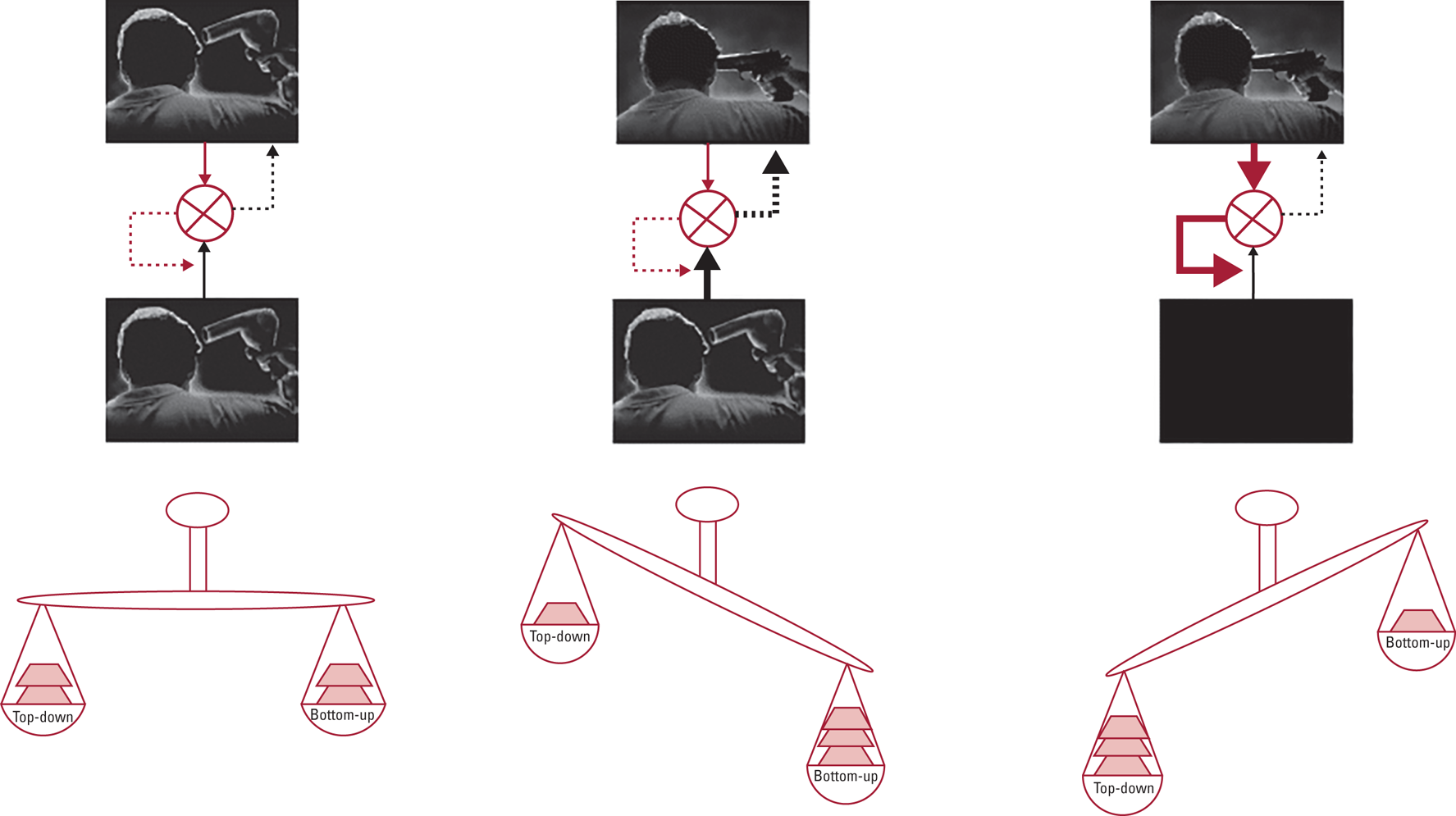
FIG 1 A schematic representation of the effects of a shift in balance between bottom-up and top-down processing. Bottom-up signals are represented by black arrows and top-down signals (‘priors’) by red arrows. Discrepancies between these signals are presented by differences in the thickness of the arrows and by the cartoon scales. Under normal circumstances (left panel), the match between a bottom-up signal and prior knowledge means that there is no requirement to change prior beliefs and perception is normal. If, however, there is persistent bottom-up firing (prediction error), prior beliefs will continually fail to match the incoming signal and will need to be changed to accommodate the signal and minimise the persistent prediction error. Corlett et al (Reference Corlett, Frith and Fletcher2009) suggest that this is a basis for changed beliefs characteristic of delusions (middle panel). If, on the other hand (right panel), strong priors exist in the absence of a strong reliable bottom-up signal, they suggest that these priors may be sufficient to create a percept, a basis, for hallucinations. Figure and caption reproduced, with small amendments, by kind permission of Corlett et al (Reference Corlett, Frith and Fletcher2009).
There is some evidence that dysregulation in top-down and bottom-up firing relate to imbalances in N-methyl-d-aspartate (NMDA) receptor functioning and dopamine (Sterzer Reference Sterzer, Adams and Fletcher2018). Prediction signals are sent to lower levels by NMDA receptors, and a proposed mechanism for a weak prior is hypofunction of these receptors (Sterzer Reference Sterzer, Adams and Fletcher2018). Glutamate may mediate top-down signals at NMDA receptors and bottom-up signals at α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors. It is postulated that this integration might be mediated by dopamine.
The language of predictive processing
Anticipated predictions and existing beliefs (priors) in the higher centres of the brain are combined with observed sensory data (likelihood) to calculate a posterior probability (posterior). The posterior corresponds to the percept that is most likely, given the prior and the likelihood (Fletcher Reference Fletcher and Frith2009).
If there is a mismatch between the prior and the likelihood, then a prediction error is generated. This error signal drives the need to update the brain's model for its current state and thus change its prior. In formal terms, a prediction error is the difference between the means of the distributions of the prior and the likelihood weighted by their respective precisions (inverse variance).
Linking predictive processing, phenomenology and neurochemistry
In psychosis, it is proposed that the balance between predictions and sensory data (priors and likelihood) is disrupted, with a decreased precision weighting in the representation of priors and increased precision weighting of the likelihood. This imbalance biases the Bayesian inference process towards the likelihood and away from the prior, resulting in the abnormally strong weighting of prediction error. The consequence of this is that it calls for an urgent restructuring of the current model of the world, sometimes in the form of a delusional elaboration. Candidate mechanisms for decreased prior and increased likelihood precisions are hypofunction of glutamatergic NMDA receptors and increased dopamine activity respectively. Some psychotic phenomena may be explained by a compensatory increase in feedback signalling at higher levels of the hierarchy (Sterzer Reference Sterzer, Adams and Fletcher2018).
Dopamine is thought to balance bottom-up sensory information and top-down prior beliefs when making predictions and is considered to play a crucial role in the precision weighting of prediction error signals through the cortex (Haarsma Reference Haarsma, Fletcher and Griffin2019). Depending on the level of the cortical hierarchy, an abnormally precise prediction error may lead to the destabilisation of prior beliefs (excessively favouring sensory information, for example in some hallucinations) or the discounting of sensory input (excessively favouring very strong prior beliefs, for example in some persistent delusions). The current consensus is that it is highly unlikely that a unifying role of strong or weak priors in psychosis exists; rather, it is a constant balancing act and interplay involving different types of prior expectations at various levels of the brain's cortical hierarchy (Haarsma Reference Haarsma, Knolle and Griffin2018). Priors from higher areas with more abstract representations (cognitive priors) are communicated downwards to lower sensory areas, which also bear their own expectations (perceptual priors).
A good way to link this with phenomenology is the case of delusional mood/delusional perception. The kind of uncanny experience involved in the very beginning stages of a psychotic illness calls for the brain's model to be updated and delusion formation acts as a means to explain away the strange experience and thus minimise prediction error. However, if the sensory experience continues to be present, the precision weighting might shift to the top-down prior, which becomes more resistant to updating over time (and may result in maintenance of the delusion). It is important to bear in mind that, despite the abnormal processing of error signals, the resulting inferences still approximate Bayesian optimality. In other words, the delusions are the best inferences a person's brain can generate given their neurochemical and neuroanatomical circumstances, which are of course embedded in their personal, societal and cultural backgrounds (Box 3). The stage of the psychotic illness may also be a factor: for example, in the early stages (including the at-risk mental state) of psychosis such as the above case of delusional mood, excessive glutamate signalling through NMDA hypofunction may lead to the weakening of perceptual priors. Once the delusion fully forms, cognitive priors may be strengthened, indicating a later stage of the illness. Nevertheless, there is significant interaction between perceptual and cognitive priors at different levels of the hierarchy, and again it may be too simplistic to generally classify priors as being only weak or strong.
BOX 3 Clinical vignette elucidating some of the principles of the predictive processing (PP) framework
This vignette is based on a real clinical presentation which has been anonymised. A simplified view of the predictive processing framework has been taken for illustrative purposes.
A is a 19-year-old who presented to the accident and emergency department following an episode of severe self-harm (cutting). They recounted that over the past few weeks they had experienced a strange sense that the world was in some way different and ‘not quite right’. PP account: an initial sense of salience set in train a process whereby existing priors (i.e the existing model and explanation of the world) feel wrong and there is a feeling that there is something new to be explained or accounted for. There is prediction error signalling linked to an aberrant salience process, leading to an experience of delusional mood.
A described having then seen some spilled red paint near a building site (observed sensory data) and coming to believe that there are thoughts within their blood. They considered that they must release the thoughts from their blood because otherwise other people's thoughts might dissolve into them from the surrounding air. When the on-call psychiatrist asked how it was that they are aware of the thoughts in their blood, they replied that it came to them ‘like a revelation.’ PP acount: in a quest to reduce the persistent prediction error, A has a new way of sampling evidence. A consequence of this is that a normally neutral stimulus or association (spilled paint) is more closely attended to and acquires new significance (blood), leading to it being incorporated into the search for explanation (or prediction error reduction).
A described the act of cutting themself as resulting in an experience of relief from irreconcilable ‘existential tensions’ and in a lessening of the feeling that ‘something isn't quite right’. PP account: there is thus a high-level prior profoundly affecting how sensory evidence is incorporated into comprehension. This in turn provides further evidence that the original prior (the world has changed) is correct. After all, how could it not be if one is seeing spilled blood on the street? Prediction error also acts as a catalyst for driving associations – and the connection between thoughts and blood, which might otherwise be ignored, takes on an added strength and leads to the further belief about other peoples’ thoughts dissolving into their own body. A's evolving priors are integrated with a dynamic change in how they attends to and processes sensory signals from the outside world.
Conclusions
Over the past 70 years there have been significant developments in the understanding of how schizophrenia-related psychopathology is generated in the brain and mind. These developments are clinically useful and urgently need to be integrated into psychiatric practice on the wards and in the clinics. As a medical specialty, psychiatry needs to align itself closer to neuroscientific research advances in order to further the field and to do patients justice (Bullmore Reference Bullmore, Fletcher and Jones2009). It is time to make the shift to a process-based psychopathology, as an additional step following phenomenological investigation of patient experience, and to move away from the 19th-century symptom-based approach, which lacks this vital step. This paradigm will improve the validity of diagnosis through linking it with brain and mind mechanisms rather than solely with symptomatology (as with the current system). We understand that the symptoms reported by patients may not alter despite a potential conceptual shift in the field of psychiatry; indeed, by a ‘process-based approach’ we are refocusing clinicians’ observations from what the checklist dictates to what the patients are really experiencing – and we suggest that this may well lead the clinician to a next step involving the consideration of brain and mind processes. (That said, the point could be made that patients can sometimes learn to interpret their experiences in the light of their encounters with clinicians, i.e. if asked about ‘voices’, patients are more likely to describe an experience in these terms.) Examinations that determine what is defined as a ‘symptom’ and those that contribute to making diagnoses ought to be based on our developing understanding of atypical experiences, which would in turn enrich history-taking according to phenomenological principles and allow clinicians to better access mind and brain mechanisms.
This approach will allow stigmatising and frightening experiences to be explained to patients and their families in a meaningful way. We have moved past the old stock exam question answer of ‘chemical imbalance’. For too long practitioners have debated whether psychotic mental illness is biological or psychological. The solution to this disagreement is that it is both. Advances in psychopathology take account of differing levels of explanation covering both the brain and the mind. (We are aware that some might consider this distinction of brain and mind problematic in that it raises issues around dualism.) Multiple levels of analysis provide different targets for varying modalities of treatment – dopamine blockade at the molecular level, and psychological therapy and social interventions at the level of the mind. We now better understand the two-way nature of the relationship between the brain and mind (and the relationship may well be a three-way one when we factor in societal influences); each able to trigger disturbance in the other. Crucially, a shift to a process-based model of mental illness would certainly not equate to a diminishment in the importance of subjective patient-focused experience; instead, it is likely to enhance this, with patients and their families gaining an improved understanding of their experiences. Similarly, a process-based approach would see psychological treatment and social therapy on a par with psychopharmacological treatments – each acting at their appropriate target level.
The transition to psychiatric and psychological process-based practice can be kick-started by clinicians obtaining a rich description of subjective experiences in their interviews and incorporating mind and brain process terms in the case notes where possible. Medical students and trainees should be taught to document aberrant salience and source-monitoring deficits in the case notes and the predictive processing concept should be one of the process-based paradigms taught routinely in medical schools.
Acknowledgements
We thank Professor Paul Fletcher for his comments on the manuscript and Dr Lauren Roberts (Foundation Doctor) for allowing us to test the clinical applicability of our ideas and the readability of the article.
Author contributions
All authors contributed significantly to this article.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
None.
ICMJE forms are in the supplementary material, available online at https://doi.org/10.1192/bja.2021.3.
MCQs
Select the single best option for each question stem
1 Which of the following is not a feature of the Bonn Scale for the Assessment of Basic Symptoms?
a it relies exclusively on patients’ first-person experience
b it gives DSM diagnoses
c it can be used with patients with prodromal symptoms
d it covers cenesthesia-related feelings
e symptoms assessed are fluid and can revert between one another.
2 One major difference between the ipseity model and the perceptual anomalies approach is that:
a only one posits that self-disturbances form the core of psychopathological experiences in schizophrenia
b only one may be considered, broadly speaking, a phenomenological approach
c one focuses on conscious self-acquaintance, the other on unconscious processing
d only one of them has helped to develop clinical assessment tools
e only one of them has relevance to clinical practice.
3 Regarding aberrant salience:
a both dopamine and serotonin are thought to play equally important roles
b it cannot be observed in people with psychosis
c it is considered central to delusion formation
d it is considered a central part of post-psychotic depression
e it has no biological basis.
4 Predictive processing is broadly based on the principles of:
a Bayesian statistics
b the dopamine hypothesis
c the brain–behaviour interface
d the biopsychosocial model
e the ipseity model.
5 Regarding priors:
a they are fixed, false beliefs
b they are encoded in the amygdala
c they do not have precision weighting
d they play very little role in hallucination formation
e they can be found in multiple cortical hierarchies.
MCQ answers
1 b 2 c 3 c 4 a 5 e





eLetters
No eLetters have been published for this article.