Background
So-called ‘street triage’ services were first piloted in the UK several years ago in order to support police officers responding to mental health crises. Rates of use of section 136 of the Mental Health Act had been causing concern and the police service had reported an increasing number of contacts with a mental health component, with estimates ranging from 2 to 50%,1,Reference Kirubarajan, Puntis, Perfect, Tarbit, Buckman and Molodynski2 alongside a perceived lack of skills to manage such situations among officers.Reference Wells and Schafer3 There were also growing concerns regarding the experience and rights of individuals,Reference Riley, Freeman, Laidlaw and Pugh4 with several cases of vulnerable individuals spending long periods in police cells, including children.5
Although the introduction of street triage services was considered a logical and positive response to these issues, it was not based upon empirical evidence. It is extremely difficult to rigorously examine the effectiveness of such complicated interventions once they have been widely introduced, and traditional methods of gathering high-level evidence, such as randomised controlled trials, are very challenging indeed. This has been seen in previous studies of mental health law.Reference Burns, Rugkåsa, Molodynski, Dawson, Yeeles and Vazquez-Montes6
Triage services vary significantly, both between and within areas. All offer a co-response model in which police and health staff work together to manage mental health crises. In some services this involves the mental health worker (usually a nurse or social worker) attending incidents with the police, in others there is real-time telephone advice, and in some both are available.
There remains scarce evidence for processes and outcomes in street triage services despite some high-quality local evaluations.Reference Irvine, Allen and Webber7–Reference Jenkins, Dye, Obeng-Asare, Nguyen and Wright9 A recent systematic review concluded that there is a lack of evidence for the effectiveness of street triage services and regarding the characteristics, experiences and outcomes of those who use them. It also concluded that there is substantial variation in the services offered.Reference Puntis, Perfect, Kirubarajan, Bolton, Davies and Hayes10 These gaps in knowledge need to be remedied to provide the most effective services for this vulnerable group. As the funding for many pilots comes towards an end, crucial questions remain about what these services should look like, who they should serve, what they achieve and who should fund them. This service evaluation aimed to provide data regarding the characteristics of street triage users and their outcomes in terms of service use over a 90 day period following initial contact.
Method
Setting, design and participants
We conducted a retrospective case note review of the co-response street triage service provided by Thames Valley Police and Oxford Health NHS Foundation Trust. This service covers the whole of Oxfordshire (680 000 population) and runs from 18.00 h to 04.00 h, 7 days a week. The team comprises one police officer and one mental health worker per shift and offers both a ride-along mobile unit (where police officer and mental health worker are dispatched in a marked police car) and a control-room-based telephone triage service located at the local police station. At the time of the evaluation, the mobile unit was only available within Oxford city. Potential cases are referred to the street triage team either through the police control room or directly from police officers who are attending incidents. The service has been in operation since August 2014.
We collected data retrospectively for individuals who had contact with the street triage team between the months of April and June 2017 (3 months in total). Records were examined for the 90 days following initial contact. Data was collected from both National Health Service (NHS) (carenotes) and street triage service records. Each contact made with the street triage team is logged by a trained mental health worker in a Microsoft Excel spreadsheet as part of routine clinical practice. The information captured includes the referral source, service user demographics, notes describing the reason for the call, the response of the street triage team, and the outcome of the response. This information was coded by one member of our team (D.P.), and the codes were then checked by another (S.P.).
We also collected data on any previous contact with mental health services in the past year, previous detention under the mental health act at any time of life, and any history of drug or alcohol misuse or dependence. This study was part of a commissioned service evaluation for Thames Valley Police and Oxford Health NHS Foundation Trust and therefore no ethical approval was needed.
Analysis
We used descriptive statistics to summarise data on demographic and clinical characteristics and service use in our sample. We categorised individuals as either ‘single’ or ‘multiple’ street triage users based on their number of triage events over the 90 day follow-up and used cross tabulations to examine the relationships within the data. We used t-tests for continuous data and χ2-tests or Fisher's exact tests for categorical variables to compare demographic and clinical characteristics and service use between single and multiple users of street triage. We did not make adjustments for multiple testing and so our findings assume significance at the P < 0.05 level.
Results
Characteristics
During the 3 month period analysed, there were 374 recorded incidents of street triage contact involving 307 different individuals. Of the 307 individuals, 244 (79%) had a mental health record with Oxford Health NHS Foundation Trust. Demographic and clinical details of our sample are given in Table 1.
Table 1 Demographic and clinical details of individuals seen by street triage (ST) team between April 2017 and June 2017 (n = 307)
a. Higher decile equals higher deprivation.
b. Previous mental health detention in Oxford Health only.
c. Previous ST contact on Oxford Health electronic health record only.
IMD, index of multiple deprivation; MH, mental health; MHA; Mental Health Act; TVP, Thames Valley Police.
The reasons recorded for the involvement of the street triage service are illustrated in Fig. 1.
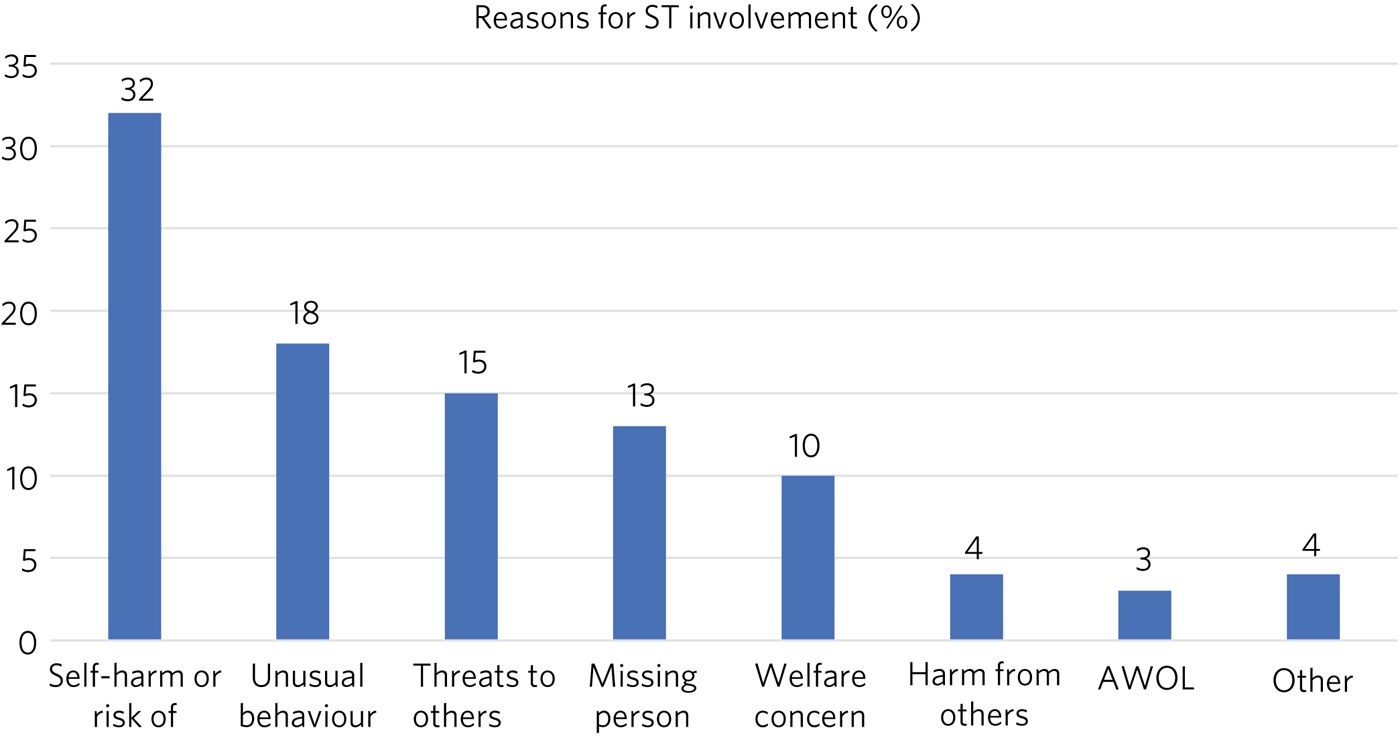
Figure 1. Documented reasons for street triage involvement.
ST, street triage; AWOL, absent without leave (from ward).
Outcome
In 284 episodes (91%), telephone advice was given either to the officer or the service user, with only 17 (6%) calls resulting in face-to-face contact. Only nine contacts (3%) resulted in section 136 use, with 199 (61%) resulting in signposting to other services or no action, 30 (10%) in accident and emergency department attendance, and 73 (24%) in police intervention regarding an alleged/ actual offence. Longer-term outcomes are shown in Table 2.
Table 2 Service users' outcomes within 90 days of index street triage (ST) incident, n = 307
a. Five (1.7%) participants were in-patients at time of street triage incident.
b. This metric only includes deaths recorded in Oxford Health's clinical records.
Although overall 45% of people accessed mental health services in the 90 days following their initial contact, this rate varied substantially by whether and when they had had previous contact. These variations are discussed below.
Single and repeat users
Within the follow-up period, 257 people (84%) only had one contact with street triage services, while 50 (16%) had two or more. Of the 50 multiple attenders, 33 had one further contact and 17 had two or more. The maximum number of street triage contacts was 11 in the time period, with three individuals having more than five contacts. The peak time for repeat contacts was within the first 2 weeks. Single and multiple users were similar demographically and in terms of the response they received. There was a non-significant trend towards differences in diagnosis between the two groups (χ2(4) = 8.39, P = 0.078), with non-affective psychoses (22 v. 14%) and personality disorders (31 v. 16%) being more common in repeat attenders. Repeat users also had significantly higher levels of service use in the prior 2 weeks (62 v. 34%; χ2(2) = 12.85, P < 0.001), in the past year (86 v. 58%; χ2(2) = 13.19, P < 0.001) and in their lifetime (96 v. 68%; χ2(2) = 15.36, P < 0.001). They were more likely to access mental health services following the street triage contact (70 v. 41%; χ2(2) = 13.39, P < 0.001) and to be admitted to a psychiatric hospital (22 v. 10%; χ2(2) = 5.77, P = 0.016).
Substance misuse
Amongst those referred to street triage services, 88 (36%) had a history of substance misuse (Table 3). In this group, 28 (32%) of people had a diagnosis of dependence in their NHS records and the remainder had symptoms of misuse. The number of health problems related to alcohol use disorder was high. Over half of substance misuse cases involved alcohol (58%), and 11 (13%) of the overall substance misuse sample (n = 88) had mixed disorders involving alcohol and another substance. Only 38 (43%) of individuals with a history of substance use disorder required street triage as a direct result of intoxication.
Table 3. Substance misuse in sample, n = 307
ST, street triage.
Limitations
This is a retrospective case note review within a short time frame and with a relatively short follow-up, so the results need to be examined with caution. However, our sample was large with few missing data on important indicators. Missing data were mostly due to the individual not having a mental health record with Oxford Health NHS Foundation Trust; therefore, the data were not missing at random as the two groups (those known to the mental health trust and those not known) were likely to be different in terms of demographics, clinical presentation, substance misuse and service use. We were not able to collect data from other services such as primary care or those for substance misuse.
Discussion
Street triage services are a major part of emergency care, with on average 100 contacts per month for a population of 680 000 people. The majority of people (84%) who use these services do so only once within a 90 day time period, with a minority using them repeatedly. Repeated use tended to be within 2 weeks, fitting with previous assumptions of a crisis-driven model of contact. Reasons for accessing triage services predominantly related to concerns for the individual's welfare due to self-harm, unusual behaviour or generalised concerns, with these making up three-quarters of contacts. The response in 94% of cases was by telephone, with a surprisingly small number of face-to-face contacts (this is a service resourced and set up for a mixed response as needed). As models vary significantly around the country and as a previous survey showed a clear preference among police officers for a face-to-face response,Reference Kirubarajan, Puntis, Perfect, Tarbit, Buckman and Molodynski2 there is a need to understand the reasons for and outcomes of differing response styles.
Multiple users were more likely to have a diagnosis of psychosis or personality disorder and were significantly more likely to have used services before, with 96% having documented previous use. They were also significantly more likely to use services afterwards, including in-patient care. This information could be useful in longer-term planning for this group, with repeat street triage use being an indicator of higher need and an automatic trigger for a response from mental health services. Such intervention might mitigate the risks and reduce rates of hospital admission in this clearly vulnerable group. Such vulnerability is shown by the eight deaths in our sample population. It is important to note, however, that the population using the triage service is not composed only of mental healthcare patients, with one in four users having had no previous contact with secondary mental health services (at least within Oxford Health NHS Foundation Trust).
Thirty-six per cent of incidents involved documented substance misuse, perhaps less than might be expected given the association between crisis situations and substance misuse. Most police officers (65%) are quite confident in determining intoxication most or all of the time,Reference Hollander, Lee, Tahtalian, Young and Kulkarni11 so underreporting seems unlikely to be a major issue. It remains important to recognise substance misuse, as many with these problems are not in specialised care and it is an added risk factor, whether the individual remains in the community or is detained in custody.Reference Norfolk12
While 45% of individuals accessed mental health services within 90 days, only 11% were admitted to hospital, and even fewer (7%) were detained under section 136. The very significant differences in subsequent access to mental healthcare between those who were already patients (75%) and those who were not (9%) are perhaps concerning as they suggest that street triage may not provide a fluid pathway into mainstream mental health services as hoped.
Conclusions
Street triage services are heavily used where available with a tendency to use a telephone model response by default in this area. Most referrals were made owing to concerns for individual welfare, and the majority of people used the service only once in 90 days.
The large differences in follow-up rates between current or recent patients and non-patients are concerning, as they suggest that triage services may not be adequately fulfilling one of their roles – as a pathway to mainstream services for this vulnerable group. Although one cannot draw causal conclusions from our data, they indicate a clear need for research studies that can more accurately determine access to services and patterns of care of those accessing triage services. This should in turn inform decision-making regarding these services. A crucial part of this is to directly ascertain the views and experience of the people who come into contact with such services at times of crisis alongside those of serving officers and the triage staff themselves. Do these services already, or will they, replace traditional crisis services, or will they wither as funding dries up? At present we simply do not know enough to take a view, let alone direct practice.
About the authors
Andrew Molodynski is a consultant psychiatrist at Oxford Health NHS Foundation Trust and Oxford University, and is BMA Consultant Committee Mental Health Lead, UK; Sarah Hollingsworth is a researcher at Oxford Health NHS Foundation Trust, UK; Louise Penzenstadler is a senior psychiatrist Geneva University Hospitals, Switzerland; Devon Perfect is a research assistant at Oxford Health NHS Foundation Trust; and Stephen Puntis is a postdoctoral researcher in the Department of Psychiatry at Oxford University, UK.







eLetters
No eLetters have been published for this article.