Introduction
Gait problems are a core feature of multiple sclerosis (MS), with 85% of patients reporting gait disturbances as their main complaint (Scheinberg, Holland & LaRocca, Reference Scheinberg, Holland and LaRocca1980) and 60% reporting falls in any 3-month period (Nilsagård et al., Reference Nilsagård, Gunn, Freeman, Hoang, Lord, Mazumder and Cameron2015). Half of these falls result in injuries (Matsuda et al., Reference Matsuda, Shumway-Cook, Bamer, Johnson, Amtmann and Kraft2011), 23% of which require medical attention (Peterson, Cho, von Koch & Finlayson, Reference Peterson, Cho, von Koch and Finlayson2008) that contribute to escalating health care costs. Impaired mobility is a major risk factor for falls in people with MS (pwMS) (Finlayson, Peterson & Cho, Reference Finlayson, Peterson and Cho2006), who typically walk with a reduced stride/step length, velocity and increased mediolateral (ML) base of support and double-limb support time, relative to age-matched healthy adults (Givon, Zeilig & Achiron, Reference Givon, Zeilig and Achiron2009; Kalron, Dvir & Achiron, Reference Kalron, Dvir and Achiron2010; Martin et al., Reference Martin, Phillips, Kilpatrick, Butzkueven, Tubridy, McDonald and Galea2006). Altered spatiotemporal gait patterns in pwMS are indicative of compromised stability and can be exacerbated by concomitant sensory deficits, such as reduced foot sensation (Rougier, Thoumie, Cantalloube & Lamotte, Reference Rougier, Thoumie, Cantalloube and Lamotte2007). Existing interventions reported to improve gait in pwMS involve short-term exercise programmes and largely address motor deficits (Davies et al., Reference Davies, Arpin, Liu, Reelfs, Volkman, Healey and Kurz2016; DeBolt & McCubbin, Reference DeBolt and McCubbin2004; Garrett et al., Reference Garrett, Hogan, Larkin, Saunders, Jakeman and Coote2013; Learmonth, Paul, Miller, Mattison & McFadyen, Reference Learmonth, Paul, Miller, Mattison and McFadyen2012; Pearson, Dieberg & Smart, Reference Pearson, Dieberg and Smart2015). However, the benefits of structured exercise on walking ability appear to be short-lived (Wiles et al., Reference Wiles, Newcombe, Fuller, Shaw, Furnival-Doran, Pickersgill and Morgan2001). New treatments to complement exercise by addressing MS sensory deficits are needed to achieve longer-term gains in activity, participation and independent living (Khan & Amatya, Reference Khan and Amatya2017).
Novel shoe insoles, designed to provide sensory input to the feet using textured materials, have been investigated as a new technique to optimise gait in healthy young (Collings, Paton, Chockalingam, Gorst & Marsden, Reference Collings, Paton, Chockalingam, Gorst and Marsden2015; Nurse, Hulliger, Wakeling, Nigg & Stefanyshyn, Reference Nurse, Hulliger, Wakeling, Nigg and Stefanyshyn2005) and older (Perry, Radtke, McIlroy, Fernie & Maki, Reference Perry, Radtke, McIlroy, Fernie and Maki2008) adults, fallers (Hatton, Dixon, Rome, Newton & Martin, Reference Hatton, Dixon, Rome, Newton and Martin2012), stroke survivors (Aries, Pomeroy, Sim, Read & Hunter, Reference Aries, Pomeroy, Sim, Read and Hunter2021; Aruin & Rao, Reference Aruin and Rao2018; Ma, Rao, Muthukrishnan & Aruin, Reference Ma, Rao, Muthukrishnan and Aruin2018), neurodegenerative (Jenkins et al., Reference Jenkins, Almeida, Spaulding, van Oostveen, Holmes, Johnson and Perry2009; Lirani-Silva et al., Reference Lirani-Silva, Vitório, Barbieri, Orcioli-Silva, Simieli and Gobbi2017) and neuromuscular (Baron et al., Reference Baron, Hatton, Robinson, Hodgson, McKeon, Rome and Dixon2016b; Dixon et al., Reference Dixon, Hatton, Robinson, Gamesby-Iyayi, Hodgson, Rome and Martin2014; Kalron, Pasitselsky, Greenberg-Abrahami & Achiron, Reference Kalron, Pasitselsky, Greenberg-Abrahami and Achiron2015; Kelleher, Spence, Solomonidis & Apatsidis, Reference Kelleher, Spence, Solomonidis and Apatsidis2010) disease populations. Evidence suggests that tactile stimulation of cutaneous receptors on the plantar surface of the foot can provide the brain with ‘amplified’ cues about the supporting surface, position and acceleration of the body, to inform balance and movement control (Roll, Kavounoudias & Roll, Reference Roll, Kavounoudias and Roll2002; Viseux et al., Reference Viseux, Lemaire, Barbier, Charpentier, Leteneur and Villeneuve2019). Indeed, recent evidence in healthy and athletic populations support the theory that textured insoles can enhance lower limb sensory feedback to augment dynamic movement control (Hasan, Davids, Chow & Kerr, Reference Hasan, Davids, Chow and Kerr2017; Jamali, Forghany, Bapirzadeh & Nester, Reference Jamali, Forghany, Bapirzadeh and Nester2019; Steinberg et al., Reference Steinberg, Waddington, Adams, Karin, Begg and Tirosh2016; Wilkinson et al., Reference Wilkinson, Ewen, Caplan, O'leary, Smith, Stoneham and Saxby2018). Similar effects of textured insoles could also occur in neurological disease populations, including pwMS, and underpin improvements in gait performance.
Exploratory studies have shown that textured insoles may have potential to improve spatiotemporal gait measures (Dixon et al., Reference Dixon, Hatton, Robinson, Gamesby-Iyayi, Hodgson, Rome and Martin2014), gait kinetics and kinematics (Kelleher et al., Reference Kelleher, Spence, Solomonidis and Apatsidis2010), self-perceived walking ability (Baron et al., Reference Baron, Hatton, Robinson, Hodgson, McKeon, Rome and Dixon2016a) and lower limb proprioception (Baron et al., Reference Baron, Robinson, Gamesby-Iyayi, Hodgson, Hatton, Warnett and Martin2014), in pwMS. A pilot randomised controlled trial in pwMS demonstrated that short-term wear (2 weeks) of textured insoles led to increased stride and step length, and reduced ML base of support, during level-ground walking (Dixon et al., Reference Dixon, Hatton, Robinson, Gamesby-Iyayi, Hodgson, Rome and Martin2014). Importantly, improvements in gait were observed when the textured insoles were not in situ, pointing to a possible sensory learning effect (Dixon et al., Reference Dixon, Hatton, Robinson, Gamesby-Iyayi, Hodgson, Rome and Martin2014). However, further work in pwMS has reported no significant changes in spatiotemporal gait measures during treadmill walking, or foot sensation, after wearing textured insoles for 4 weeks (Kalron et al., Reference Kalron, Pasitselsky, Greenberg-Abrahami and Achiron2015). To date, studies exploring textured insoles for pwMS have been limited to the evaluation of level-ground walking; overlooking irregular, uneven terrain encountered in everyday life that can perturb balance to a greater extent and which may provide valuable insight into any insole effects under conditions where falls commonly occur (Hollander, Petersen, Zech & Hamacher, Reference Hollander, Petersen, Zech and Hamacher2022; Menant, Steele, Menz, Munro & Lord, Reference Menant, Steele, Menz, Munro and Lord2009). Furthermore, few studies report the effects of long-term wear of textured insoles on gait in pwMS. This is a critical area to research, as the benefits of textured insoles may accrue (or decline) with prolonged wear, allowing pwMS sufficient time to become familiar with (or habituate to) a new source of sensory stimuli.
Innovative thinking towards the therapeutic capabilities of shoe insoles for pwMS (e.g., providing substitute plantar sensory input) challenges the traditional physiological basis for insole/orthotic prescription in neurological diseases, which has centred on the management of neuromotor control during walking (Young & Moss, Reference Young and Moss2019). Recent evidence suggests that textured insoles may also influence perceptual aspects of movement control in MS, which manifest as greater walking confidence and awareness of foot position (Baron et al., Reference Baron, Hatton, Robinson, Hodgson, McKeon, Rome and Dixon2016a; Baron et al., Reference Baron, Robinson, Gamesby-Iyayi, Hodgson, Hatton, Warnett and Martin2014). Whilst textured insoles can improve objective (and self-reported) measures of gait in pwMS, we do not understand their underlying mechanisms. Only one study in pwMS has explored the effect of textured insoles on measures of foot sensation, reporting no significant change in light-touch pressure sense (Kalron et al., Reference Kalron, Pasitselsky, Greenberg-Abrahami and Achiron2015). However, alterations may occur in other dimensions of sensory function, such as vibration perception, spatial discrimination, or joint proprioception.
Therefore, the objective of this study was to determine whether wearing textured insoles for 12 weeks can improve spatiotemporal gait patterns and foot sensory function in pwMS. The primary aim was to explore if prolonged wear of textured insoles alters the size of the ML base of support (a measure of gait stability) in pwMS, when walking over even and uneven surfaces – relative to smooth (control) insoles. We hypothesised that wearing textured insoles for 12 weeks would lead to reductions in stride/step width during walking. Secondary aims were to investigate if prolonged wear of textured insoles alters other gait measures (stride time, double-limb support time, stride length and velocity), foot sensory function (light-touch, vibration, two-point discrimination and joint position sense) and patient-reported outcomes (walking ability, MS symptoms, falls, quality of life). We hypothesised that wearing textured insoles would decrease stride time and double support time and increase stride length and velocity and lead to improvements in foot sensory function and patient-reported outcomes.
Methods
Design
A prospective, parallel group, single-blinded, randomised controlled trial of pwMS was conducted. Recruitment occurred from March 2016 to November 2017; and post-intervention assessments until March 2018. Ethical approval was obtained from The University of Queensland (#2014000871) and Queensland University of Technology (#1500000615) Human Research Ethics Committees. All participants provided written informed consent. The trial was conducted in accordance with the Declaration of Helsinki, conformed to the Consolidated Standards of Reporting Trials guidelines (Schulz, Aman & Moher, Reference Schulz, Altman and Moher2010) and was registered with the Australian and New Zealand Clinical Trials Registry (ACTRN12615000421538). The methods employed are described within the published protocol (Hatton et al., Reference Hatton, Dixon, Rome, Brauer, Williams and Kerr2016).
Sample size
A priori calculation was performed to determine sample size; following publication of protocol, the sample size calculation was updated resulting in a slightly smaller sample size. Based on preliminary work in pwMS (Dixon et al., Reference Dixon, Hatton, Robinson, Gamesby-Iyayi, Hodgson, Rome and Martin2014), a mean (SD) reduction of 1.7 (3.0) cm in ML base of support during level-ground walking, after wearing textured insoles for 2 weeks, was estimated. With a power of 90% to detect a difference between groups of 1.7 cm, significance of 0.05 and accounting for a 15% dropout rate, 83 participants were required per group.
Participants
Men and women with MS were recruited via volunteer databases maintained at The University of Queensland and MS Queensland, and through advertisements to local MS health care providers and support groups, across South East Queensland, Australia. Participants were eligible to take part if they met the following criteria: aged ≥18 years; diagnosis of MS; ambulant over 100 m (with/without use of an assistive device); and Disease Step rating 1–4 (clinician-rated) (Hohol, Orav & Weiner, Reference Hohol, Orav and Weiner1995). Exclusion criteria were: neurological disease other than MS; peripheral neuropathy; current use of foot insoles/orthoses; cardiovascular or orthopaedic conditions that limit ambulation; unstable psychiatric condition or cognitive impairment (Short Form Mini Mental State Examination score < 24; Folstein, Folstein & McHugh, Reference Folstein, Folstein and McHugh1975)). Participants who experienced an exacerbation of MS symptoms (persisting >24 h), 4 weeks prior to, or during, the intervention period were excluded. Volunteers were screened for eligibility by telephone and thereafter invited to attend a clinical examination (conducted by a physiotherapist, KW), which involved the assessment of disease stage (Disease Steps; Hohol et al., Reference Hohol, Orav and Weiner1995), spasticity (Tardieu Scale; Tardieu, Shentoub & Delarue, Reference Tardieu, Shentoub and Delarue1954), ataxia (Brief Ataxia Rating Scale; Schmahmann, Gardner, MacMore & Vangel, Reference Schmahmann, Gardner, MacMore and Vangel2009) and foot sensation (ability to detect a Semmes–Weinstein 10 g monofilament at ≥4 sites/ft; Armstrong, Lavery, Vela, Quebedeaux & Fleischli, Reference Armstrong, Lavery, Vela, Quebedeaux and Fleischli1998).
Intervention
Both groups continued to receive their usual care during the study; participants were asked to notify the investigators of any change to their usual care during their involvement in the study. The intervention group was fitted with a pair of textured insoles (Evalite Pyramid ethyl vinyl acetate, 3 mm thick, Shore A50; Algeos, VIC, Australia) comprising raised pyramidal peaks (2.5 mm peak-to-peak distances) (Fig. 1). The control group received a pair of smooth insoles (medium-density ethyl vinyl acetate, 3 mm thick, Shore A50; Algeos, VIC, Australia), comprising a flat surface (Fig 1). Insoles were tailored to each individuals’ shoe size and fitted by a podiatrist (SH, JNM), who also provided advice on frequency of wear, completion of insole wear (to monitor hours of insole wear per day) and falls diaries and contact details for podiatry care. Over the 12-week intervention period, participants were instructed to wear their allocated insoles in their own shoes, as much as possible (when indoors and outdoors), and to gradually increase wear time after first being issued the insoles. During laboratory gait tests, the insoles were worn in standard shoes (Volley International Canvas, Volley, China), to control for any confounding shoe/insole interactions. Upon wearing the shoes for the first time, participants walked for 5-min to allow for familiarisation.

Figure 1. Smooth (A) and textured (B) shoe insoles.
Randomization and blinding
The computer-generated randomisation schedule was maintained by an independent investigator. Participants were randomly allocated to one of two groups (Textured insoles; Smooth insoles), using permuted blocks of 4 (1:1 ratio). Consecutively numbered, opaque envelopes containing group allocation were opened after Baseline 2 assessment by the study podiatrists who were only responsible for issuing the insoles. All other investigators involved in participant enrolment and assessments were blinded to group allocation. Participants could not be blinded to their group, as those allocated to the intervention would likely perceive the textured material under their feet. The full study aims were concealed from participants until debriefing, upon completion of the study.
Laboratory assessments
Participants attended three assessments (2–3 h/assessment) within the Gait Laboratory at Queensland University of Technology: Baseline 1 (Week 0); Baseline 2 (Week 4); Post-Intervention (Week 16). Two baseline assessments were conducted to establish participants’ usual rate of disease progression over a 4-week period, prior to issuing the insoles upon completion of Baseline 2.
Baseline 1
Demographic details were collected including age, gender, body mass. Participants completed questionnaires addressing medical history, MS diagnosis and symptoms (MS Impact Scale; Hobart, Lamping, Fitzpatrick, Riazi & Thompson, Reference Hobart, Lamping, Fitzpatrick, Riazi and Thompson2001), and perceived walking ability (MS Walking Scale; Hobart, Riazi, Lamping, Fitzpatrick & Thompson, Reference Hobart, Riazi, Lamping, Fitzpatrick and Thompson2003). Self-report questionnaires were used to assess quality of life (MS Quality of Life Instrument; Vickrey, Hays, Harooni, Myers & Ellison, Reference Vickrey, Hays, Harooni, Myers and Ellison1995), the impact of fatigue (Modified Fatigue Impact Scale; Fisk et al., Reference Fisk, Pontefract, Ritvo, Archibald and Murray1992) and pain (Medical Outcomes Study Pain Effects Scale; Archibald et al., Reference Archibald, McGrath, Ritvo, Fisk, Bhan, Maxner and Murray1994), perceived disability (Perceived Deficits Questionnaire; Sullivan, Edgley & Dehoux, Reference Sullivan, Edgley and Dehoux1990) and fear of falling (Falls Efficacy Scale-International; Yardley et al., Reference Yardley, Beyer, Hauer, Kempen, Piot-Ziegler and Todd2005). Participants also reported the number of falls experienced in the previous 12 months.
Foot sensory function was assessed bilaterally, as described in the study protocol (Hatton et al., Reference Hatton, Dixon, Rome, Brauer, Williams and Kerr2016). Light-touch pressure sense was measured using Semmes–Weinstein monofilaments (1.65–6.65 gauges), applied to the great toe, first and fifth metatarsal heads, heel and dorsum of the foot (Citaker et al., Reference Citaker, Gunduz, Guclu, Nazliel, Irkec and Kaya2011; Hatton et al., Reference Hatton, Dixon, Rome, Brauer, Williams and Kerr2016). Vibration sense was measured using a 128-Hz tuning fork applied to the first metatarsal head and medial malleoli (Citaker et al., Reference Citaker, Gunduz, Guclu, Nazliel, Irkec and Kaya2011; Hatton et al., Reference Hatton, Dixon, Rome, Brauer, Williams and Kerr2016). The two-point discrimination test was performed using an aesthesiometer, to determine tactile spatial acuity at the great toe, first to second metatarsal interspace and fifth metatarsal head (Citaker et al., Reference Citaker, Gunduz, Guclu, Nazliel, Irkec and Kaya2011; Hatton et al., Reference Hatton, Dixon, Rome, Brauer, Williams and Kerr2016). Proprioception was assessed via the ankle joint angle reproduction test (Riskowski, Mikesky, Bahamonde, Alvey & Burr, Reference Riskowski, Mikesky, Bahamonde, Alvey and Burr2005), with an internet-based goniometer used to measure accuracy in joint positioning (Russell, Jull & Wootton, Reference Russell, Jull and Wootton2003).
Gait was assessed whilst walking at a comfortable, self-selected pace over a 12 m even and uneven surface. The even surface comprised the vinyl top cover of a GaitRite® walkway (CIR Systems Inc., Havertown, USA). The uneven surface, designed to simulate outdoor terrain, was created from layers of foam, wood blocks and artificial grass (Menant et al., Reference Menant, Steele, Menz, Munro and Lord2009). Start and finish lines were taped two metres in front and behind the walkways to allow for acceleration and deceleration (Batey, Rome, Finch & Hanchard, Reference Batey, Rome, Finn and Hanchard2003). PwMS completed five walking trials (or as many trials as tolerated) along the even and uneven surfaces, under four different footwear conditions: (i) barefoot, (ii) standard shoes only, (iii) textured insoles and (iv) smooth insoles (order randomised). Prior to testing, reflective markers were attached to participants (Vicon Plug-In-Gait full body model). Spatiotemporal gait patterns were measured using the GaitRite® (sampling rate 80 Hz) during even surface walking trials, and an 11-camera Vicon® system (sampled at 200 Hz), for the uneven surface walking trials. It was not possible to collect data using Vicon®, for both surfaces, due to the size of the camera capture area, relative to the layout of the walkways within the laboratory.
Upon completion of Baseline 1, a wireless activity monitor (ActivPALTM, Glasgow, Scotland), was fitted to each participant’s right thigh using adhesive tape. The monitor was worn for seven consecutive days to characterise participants’ habitual activity levels (total number of steps, counts/day; total time spent sitting, standing, walking, h/day) (Edwardson et al., Reference Edwardson, Winkler, Bodicoat, Yates, Davies, Dunstan and Healy2017).
Baseline 2
Four weeks after their initial assessment, participants returned to the laboratory to perform tests of foot sensory function and gait, as per Baseline 1. This waiting period enabled observation of participants’ natural rate of MS disease progression, and any changes in the outcome measures, prior to issuing the intervention. Participants’ allocated insoles were fitted by the podiatrist at the end of the Baseline 2 assessment (the investigators left the laboratory to ensure assessor blinding).
Post-intervention
Participants completed a final assessment of foot sensory function and gait, after wearing their allocated insoles for 12 weeks. Questionnaires completed at Baseline 1 were re-administered for a second time. Participants also rated how comfortable their insoles were to wear using a 100 mm visual analogue scale (VAS, 0 = extremely uncomfortable; 100 = extremely comfortable) (Mills, Blanch & Vicenzino, Reference Mills, Blanch and Vicenzino2010). Insole wear (Supplementary Material 1) and falls (Supplementary Material 2) diaries, completed over the 12-week intervention period, were returned at this time.
Outcome measures
The primary outcome was the change in size of the ML base of support, when walking over the even and uneven surface, with a reduction in stride/step width interpreted to indicate greater stability. Secondary spatiotemporal gait measures included stride time, double-limb support time, stride length and gait velocity. Secondary foot sensation and proprioception measures were light-touch pressure sense (smallest monofilament perceived ≥2/3 applications, at each of the five foot sites) (Citaker et al., Reference Citaker, Gunduz, Guclu, Nazliel, Irkec and Kaya2011; Hatton et al., Reference Hatton, Dixon, Rome, Brauer, Williams and Kerr2016), vibration sense (duration of vibration, seconds) (Citaker et al., Reference Citaker, Gunduz, Guclu, Nazliel, Irkec and Kaya2011; Hatton et al., Reference Hatton, Dixon, Rome, Brauer, Williams and Kerr2016), two-point discrimination (smallest distance perceived, mm) (Citaker et al., Reference Citaker, Gunduz, Guclu, Nazliel, Irkec and Kaya2011; Hatton et al., Reference Hatton, Dixon, Rome, Brauer, Williams and Kerr2016) and ankle joint position sense (accuracy in joint angle re-positioning, degrees error) (Riskowski et al., Reference Riskowski, Mikesky, Bahamonde, Alvey and Burr2005). Secondary patient-reported outcomes included the MS Impact Scale (Hobart et al., Reference Hobart, Lamping, Fitzpatrick, Riazi and Thompson2001), MS Walking Scale (Hobart et al., Reference Hobart, Riazi, Lamping, Fitzpatrick and Thompson2003), MS Quality of Life Instrument (Vickrey et al., Reference Vickrey, Hays, Harooni, Myers and Ellison1995), Modified Fatigue Impact Scale (Fisk et al., Reference Fisk, Pontefract, Ritvo, Archibald and Murray1992), Medical Outcomes Study Pain Effects Scale (Archibald et al., Reference Archibald, McGrath, Ritvo, Fisk, Bhan, Maxner and Murray1994), Perceived Deficits Questionnaire (Sullivan et al., Reference Sullivan, Edgley and Dehoux1990) and Falls Efficacy Scale-International (Yardley et al., Reference Yardley, Beyer, Hauer, Kempen, Piot-Ziegler and Todd2005).
Data analysis
Statistical analyses were performed in a blinded manner, on an intention-to-treat basis, using Stata 16.0 (StataCorp. 2019). Data were assessed for normality. Outcomes that were skewed, were transformed onto the 100 log(e) scale, to enable reporting of symmetric percentage differences (Cole, Reference Cole2000). Gait and foot sensory measures were averaged across the left and right leg/foot. To determine any between-group differences in outcomes, independent t-tests were performed on change from baseline (average of Baseline 1 and Baseline 2 measures) to post-intervention. The alpha level was 0.05, with no adjustments for multiple testing.
Results
A total of 202 pwMS were screened for eligibility. Of these, 51 pwMS underwent a clinical examination, and 41 pwMS were enrolled into the study and completed Baseline 1 assessment (Fig. 2). Recruitment ceased prior to reaching the estimated sample size (n = 166), and before any data analysis had taken place, due to the exhaustion of funding and resources. Eighteen pwMS were allocated to the smooth insole group and 20 pwMS to the textured insole group. The attrition rate was 7% at 4 weeks and 27% at 16 weeks. Thirty participants successfully completed the trial (Control group, N = 15; Intervention group, N = 15). Baseline demographic and clinical characteristics were similar between groups (Table 1).

Figure 2. Flow of participants through the study.
Table 1. Demographics and Clinical Characteristics for Participants Who Were Allocated to the Control Group (Smooth Insoles) and Intervention (Textured Insoles) Group and Successfully Completed the Trial
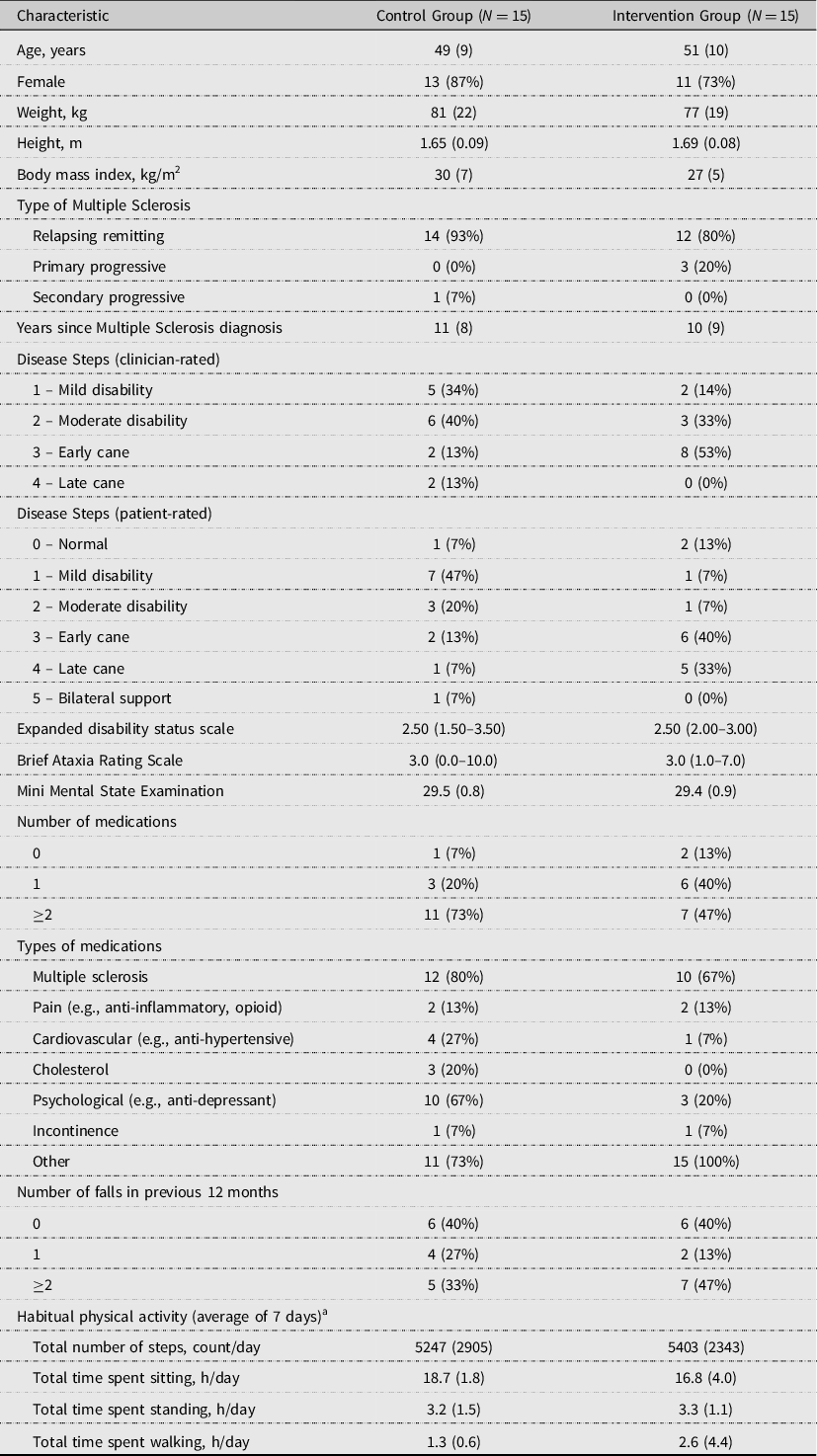
Data are presented as mean (SD) or median (IQR) for continuous measures, and n (%) for categorical measures.
a Physical activity data for the Control Group represents N = 14, due to technical problems with the ActivPalTM monitor.
Insole adherence and comfort
Participants in both groups reported wearing their insole for a similar number of (mean ± SD) hours/day over the intervention period (Smooth insole: 5.5 ± 3.5 h/day; Textured insole: 6.4 ± 3.0 h/day; P = 0.47). Perceived comfort when wearing the insoles (VAS, mean ± SD) did not significantly differ between groups (Smooth insole: 64 ± 32; Textured insole: 77 ± 27; P = 0.25).
Adverse events
Over the intervention period, five pwMS (18%) reported a non-injurious fall. Of these, four participants (29%) were in the control group, and one participant (7%) was in the intervention group. The rate of falls did not significantly differ between the groups (P = 0.33). PwMS who experienced a fall during the trial were known to be recurrent fallers and, therefore, wearing the insoles did not increase their usual rate of falls. The insole wear diaries indicated that foot pain and discomfort were experienced by some participants in the smooth (N = 7, 47%) and textured (N = 5, 36%) insole groups, but this was not significantly different (P = 0.71). Nine participants noted minor skin irritation to the soles of their feet, whilst wearing the smooth (N = 2, 13%) and textured (N = 7, 47%) insoles (P = 0.11).
Primary outcome measure
At post-intervention, there were no significant between-group differences in change in stride width, when walking over the even surface (all P values ≥ 0.20) in each of the four footwear conditions (Fig. 3 and Table 2).
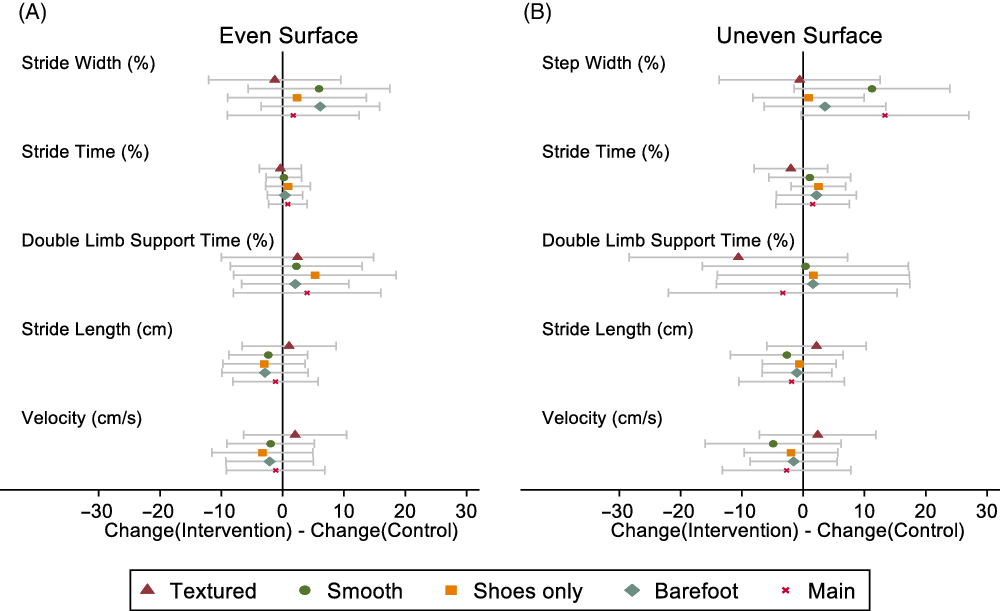
Figure 3. Effect of intervention (versus control) with 95% confidence interval for change in Stride Length and Velocity, and symmetric percentage change in Stride/Step Width, Stride Time, and Double-Limb Support Time, when walking over even (A) and uneven (B) surfaces. ‘Main’ denotes a comparison between baseline gait assessments completed in the ‘Shoes only’ condition (i.e., no insoles), and post-intervention gait assessments performed with participants wearing the insoles allocated to them over the intervention period (i.e., textured insole gait assessments for the intervention group; smooth insole gait assessments for the control group).
Table 2. Changes in Spatiotemporal Gait Measures (Averaged Across Right/Left Legs) from Baseline to Post-Intervention for the Control (Smooth Insole) and Intervention (Textured Insole) Groups, When Walking Over Even and Uneven Surfaces in Four Footwear Conditions

a Walking over the even surface, data represents N = 14 (Control Group) and N = 12 (Intervention Group), due to technical problems with the GaitRite® system during testing.
b Percent difference (rather than absolute difference).
c ‘Main’ represents a comparison between gait assessments completed at baseline whilst wearing shoes only (i.e., no insoles) to gait assessments completed at post-intervention when participants wore the insoles allocated to them over the intervention period (i.e., textured insole assessments for the intervention group; smooth insole assessments for the control group).
d Walking over the uneven surface, data represents N = 12 (Control Group), with the exception of the barefoot condition where N = 11, and N = 13 (Intervention Group). Three participants were not physically able to perform uneven surface walking tests due to fatigue or the use of an assistive device that could not be used safely over the irregular terrain. Technical problems were encountered during data processing for N = 3.
Secondary outcome measures
There were no significant between-group differences for changes in the secondary gait parameters when walking over the even or uneven surface, after wearing textured insoles for 12 weeks (all P values > 0.23) (Fig. 3 and Table 2). We observed no significant changes in measures of foot sensory function between groups (all P values ≥ 0.08) (Fig. 4 and Table 3). Data from the insole wear diaries indicated that a proportion of participants in the control (N = 7, 47%) and intervention (N = 9, 60%) groups, reported experiencing changes in foot sensation, but this was not significantly different (P = 0.72). There were no significant between-group differences for any patient-reported outcomes (all P values ≥ 0.23) (Table 4).
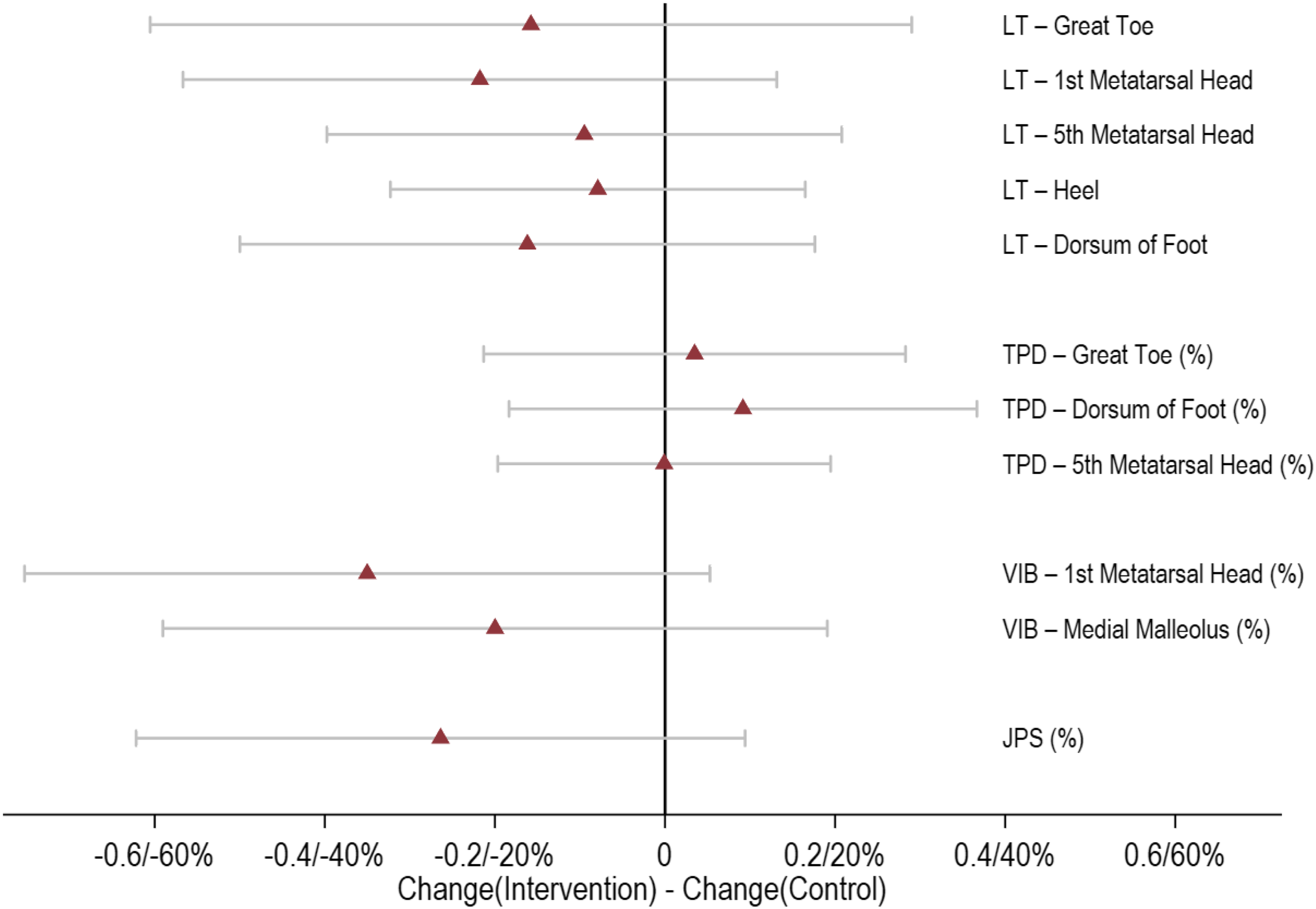
Figure 4. Effect of intervention (versus control) with 95% confidence interval for change in light-touch pressure sense measures, and symmetric percentage change in two-point discrimination, vibration sense, and joint position sense measures. LT, light-touch pressure sense; TPD, two-point discrimination; VIB, vibration sense; JPS, joint position sense.
Table 3. Changes in Foot Sensation and Proprioception Measures (Averaged Across Right and Left Legs) from Baseline to Post-intervention for the Control (Smooth Insole, N = 15) and Intervention (Textured Insole, N = 15) Groups

a Percent difference (rather than absolute difference).
Table 4. Changes in Patient-Reported Outcome Measures from Baseline to Post-intervention for the Control (Smooth Insole, N = 15) and Intervention (Textured Insole, N = 15) Groups

a Percentage change (for MS Impact Scale, scores of 0 first recoded as 1).
b Data is N = 11 (Control) and N = 13 (Intervention), as six participants preferred not to complete questionnaire items addressing sexual function.
Discussion
This study investigated whether prolonged wear of textured shoe insoles alters spatiotemporal walking patterns and foot sensory function in pwMS. Contrary to our hypotheses, there were no differences in gait patterns, foot sensory measures, or patient-reported outcomes in pwMS after wearing textured insoles for 12 weeks. Similar results were found for the pwMS allocated to the control group, who wore smooth insoles for 12 weeks.
Our study was the first to explore the effects of wearing textured insoles over an extended period (>4 weeks). Several studies have reported the positive effect of textured insoles on balance and walking in neurological disease groups, upon wearing the insoles for the first time (immediate effects) (Jenkins et al., Reference Jenkins, Almeida, Spaulding, van Oostveen, Holmes, Johnson and Perry2009; Kalron et al., Reference Kalron, Pasitselsky, Greenberg-Abrahami and Achiron2015; Kelleher et al., Reference Kelleher, Spence, Solomonidis and Apatsidis2010; Qiu et al., Reference Qiu, Cole, Davids, Hennig, Silburn, Netscher and Kerr2013) and after short-term wear (up to 4 weeks) (Dixon et al., Reference Dixon, Hatton, Robinson, Gamesby-Iyayi, Hodgson, Rome and Martin2014; Kalron et al., Reference Kalron, Pasitselsky, Greenberg-Abrahami and Achiron2015; Lirani-Silva et al., Reference Lirani-Silva, Vitório, Barbieri, Orcioli-Silva, Simieli and Gobbi2017). Our previous pilot study in pwMS reported improvements in stride length, ML base of support and double-limb support time during level-ground walking, after wearing textured insoles for 2 weeks (Dixon et al., Reference Dixon, Hatton, Robinson, Gamesby-Iyayi, Hodgson, Rome and Martin2014), however, no significant immediate effects were observed. Subsequent work by Kalron et al. (Reference Kalron, Pasitselsky, Greenberg-Abrahami and Achiron2015) demonstrated that textured insoles had no immediate or short-term wear (4 weeks) effects on spatiotemporal gait or plantar sensory measures in pwMS. Rather, the therapeutic benefits of textured insoles were observed for standing balance only, with improvements in centre of pressure measures immediately after inserting the insoles (vs shoes only), which were maintained at 4-week follow-up (Kalron et al., Reference Kalron, Pasitselsky, Greenberg-Abrahami and Achiron2015). Evidence in other neurological disease groups, specifically Parkinson’s disease, supports the theory that immediate and short-term exposure to textured footwear interventions has the capacity to improve single-limb support time (Jenkins et al., Reference Jenkins, Almeida, Spaulding, van Oostveen, Holmes, Johnson and Perry2009), stride length (Lirani-Silva et al., Reference Lirani-Silva, Vitório, Barbieri, Orcioli-Silva, Simieli and Gobbi2017) and plantar sensation (Lirani-Silva et al., Reference Lirani-Silva, Vitório, Barbieri, Orcioli-Silva, Simieli and Gobbi2017). However, conflicting findings from a systematic review report that sensory-stimulating insoles (e.g., texture) do not improve balance or gait in pwMS or Parkinson’s disease (Alfuth, Reference Alfuth2017). Importantly, the findings from Alfuth (Reference Alfuth2017) should be interpreted with caution due to the methodological approach and analyses undertaken.
In the current study, we observed no significant changes in gait or foot sensory measures after wearing textured insoles for 12 weeks. It is possible that during this longer intervention period participants may have habituated to the sensory stimulus, which negated any beneficial insole effects that accrued in the short term. Furthermore, there may be a dose–response relationship with regard to the therapeutic effects of textured insoles, whereby the physical properties of the textured stimuli may need to be modulated (e.g., increasingly larger protrusions), once a user has acclimatised to the stimuli, to ensure any benefits continue to accrue. There is convincing evidence that an individuals’ response to footwear devices, designed to improve balance and walking, can fluctuate over time. Ramdharry, Marsden, Day and Thompson (Reference Ramdharry, Marsden, Day and Thompson2006) reported that wearing foot orthoses for 4 weeks led to an initial de-stabilisation effect in pwMS that was superseded by improvements in balance. Taken together, this evidence suggests that we do not clearly understand the optimal treatment duration for wearing textured insoles, to elicit sustained improvements in gait and foot sensation.
A secondary aim was to explore if wearing textured insoles alters foot sensory function, as an underlying mechanism of action. Contrary to our hypothesis, we reported no between-group differences in any of the foot sensory measures, at post-intervention. This result supports work by other groups (Kalron et al., Reference Kalron, Pasitselsky, Greenberg-Abrahami and Achiron2015), who similarly observed no change in plantar light-touch pressure sense in 25 pwMS, following short-term wear (4 weeks) of textured insoles. One possible explanation for this finding is that pwMS who had severe foot sensory loss were excluded from the current study. This was based on the rationale that it was important for participants to be able to perceive the textured stimuli for the insoles to be effective. However, our systematic review indicated that people with reduced foot sensation may benefit most from textured insoles, through the provision of ‘substitute’ sensory information (Paton, Hatton, Rome & Kent, Reference Paton, Hatton, Rome and Kent2016).
Limitations
There were several study limitations. First, our small sample size could mean the study was underpowered to detect effects of a plausible magnitude of textured insoles on gait and foot sensation, and thus, the results should be interpreted with caution. Second, pwMS who had severe loss of foot sensation were excluded. Emerging evidence proposes that individuals with reduced foot sensation may benefit most from textured insoles (Paton et al., Reference Paton, Hatton, Rome and Kent2016). Therefore, our participant selection criteria may have limited the ability to observe the true potential of textured insoles. Third, wearing textured insoles could lead to beneficial changes in measures that were not assessed in this work, e.g., gait kinetics, neuromuscular function, physical activity levels.
Conclusions
Wearing textured insoles for 12 weeks did not appear to alter walking patterns or foot sensation in pwMS who have limited foot sensory loss. However, textured insoles may be an effective gait rehabilitation strategy for pwMS who have significant loss of foot sensation: this area is yet to be explored. It remains unclear if wearing textured insoles for an extended period leads a user to habituate to the sensory stimuli, and thus any immediate or short-term improvements in gait become redundant over time. Further research is warranted to investigate the effects of textured insoles in pwMS with neuropathy and to explore different textured insole design features, by way of larger studies.
Supplementary materials
For supplementary material for this article, please visit https://doi.org/10.1017/BrImp.2022.33
Acknowledgements
The authors would like to acknowledge Sarah Robins and Jessica Thompson for their contribution to completing the blinded assessments; and Robyn Lamont for maintaining the randomisation schedule. The authors would also like to thank Nampech Wuthapanich and Jessica Thompson for their assistance with data processing. In particular, the authors would like to acknowledge Multiple Sclerosis Queensland for their involvement with participant recruitment.
Financial support
This work was supported by a Multiple Sclerosis Research Australia Project Grant (Grant ID: 13-006) awarded to ALH, KW, JD, KR, GK and SGB.
Conflicts of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.










